Abstract
Introduction
Monitoring of sanitation programs is often limited to sanitation access and coverage, with little emphasis on use of the facilities despite increasing evidence of widespread non-use.
Objectives
We assessed patterns and determinants of individual latrine use over 12 months in a low- income rural study population that had recently received latrines as part of the Government of India’s Total Sanitation Campaign (TSC) in coastal Puri district in Odisha, India.
Materials and methods
We surveyed 1938 individuals (>3 years) in 310 rural households with latrines from 25 villages over 12 months. Data collection rounds were timed to correspond with the seasons. The primary outcome was reported use by each member of the household over the prior 48 h. We classified use into three categories—“never”, “sometimes” and “always/usually”. We also assessed consistency of use over six days across the three seasons (dry cold, dry hot, rainy). We explored the association between individual and household-level variables and latrine use in any given season and longitudinally using multinomial logistic regression. We also inquired about reasons for non-use.
Results
Overall, latrine use was poor and inconsistent. The average response probability at any given round of never use was 43.5% (95% CI = 37.9, 49.1), sometimes use was 4.6% (95% CI = 3.8, 5.5), and always/usual use was 51.9% (95% CI = 46.2, 57.5). Only two-thirds of those who reported always/usually using a latrine in round one reported the same for all three rounds. Across all three rounds, the study population was about equally divided among those who reported never using the latrine (30.1%, 95% CI = 23.0, 37.2), sometimes using the latrine (33.2%, 95% CI = 28.3, 38.1) and always/usually using the latrine (36.8%, 95% CI = 31.8, 41.8). The reported likelihood of always/usually versus never using the latrine was significantly greater in the dry cold season (OR = 1.50, 95% CI = 1.18, 1.89, p = 0.001) and in the rainy season (OR = 1.34, 95% CI = 1.07, 1.69, p = 0.012), than in the dry hot season.
Across all three seasons, there was increased likelihood of always/usually and sometimes using the latrine versus never using it among females and where latrines had a door and roof. Older age groups, including those aged 41–59 years and 60+ years, and increase in household size were associated with a decreased likelihood of always/usually using the latrine versus never using it. The leading reason for non-use was a preference for open defecation.
Conclusion
Results highlight the low and inconsistent use of subsidized latrines built under the TSC in rural Odisha. This study identifies individual and household levels factors that may be used to target behavior change campaigns to drive consistent use of sanitation facilities by all.
Keywords: Sanitation, Rural, Latrine use, Consistent use, Patterns, Determinants
1. Introduction
Sanitation is considered to be fundamental to human health (WHO, 2014). Yet many people, especially those in low-resource settings, have no access to sanitation. Among an estimated 946 million who practice open defecation, nine in ten of those reside in rural settings (WHO-UNICEF, 2015a, WHO-UNICEF, 2015b). Almost 60% of the world’s open defecators live in India, most in rural settings (Planning Commission, 2013, WHO-UNICEF, 2014a).
By 2016, the Central Indian government’s sanitation programs have already been operational for more than three decades (Planning Commission, 2013). The Total Sanitation Campaign (TSC)—the version of the program which is investigated here—was launched in 1999 as part of a comprehensive program aimed to accelerate sanitation coverage in rural areas and make India open defecation free (ODF or ‘Nirmal Bharat’) by 2017. It focused primarily on the construction of individual household pit latrines. The TSC was designed as a “demand-driven, community-led”, “low to no subsidy” approach to total sanitation and was implemented by the state governments (DDWS, 2011).
In the decade of the TSC through March 2010, 64.3 million individual household latrines were reportedly constructed, including 34.8 million latrines in below poverty line households (WSP, 2011). However, a review of the TSC commissioned by the Government of India (GoI) suggested that as many as 72.63% households in rural India practice open defecation even though they have access to latrines (Planning Commission, 2013). This estimate, although higher than others (WHO-UNICEF, 2014a), reveals that latrine access does not always translate into use (National Sample Survey Office, December 2013; Sanan and Moulik, 2007, WSP, 2011). It offers insights into likely reasons for open defecation, even among households that have latrines, including that it is “an established age old practice” with little or no stigma attached to it (Coffey et al., 2014, Ghosh and Cairncross, 2014; Planning Commission, 2013), and generally low awareness of the benefits of hygiene (Banerjee and Mandal, 2011, Planning Commission, 2013). Finally, the scale of the problem reflects certain implementation and program service delivery issues that require strengthening (Ghosh and Cairncross, 2014, WSP, 2011). From a monitoring perspective, it implies that the focus should also be on latrine use rather than only on access and coverage.
Monitoring progress on sanitation has been greatly influenced by the approach adopted by the WHO-UNICEF Joint Monitoring Programme for Water Supply and Sanitation (JMP). JMP sanitation monitoring elicits data on coverage and household-level use, to a limited extent (WHO-UNICEF, 2015a, WHO-UNICEF, 2015b). It does not enable monitoring of individual latrine use. While suitable modifications to the monitoring parameters have been debated in connection with the development of the post-2015 Sustainable Development Goals (SDG), the SDG Target 6.2 remains largely unchanged in regard to latrine use monitoring (WHO-UNICEF, 2014b, October 2015).
Similarly, the Indian government’s routine monitoring system for the rural sanitation sector is limited to periodic tracking of inputs (budget spent) and outputs (latrines constructed). It does not track actual use of latrines (Ganguly, 2008, Planning Commission, 2013, WSP, 2013). Outcomes such as ODF communities are monitored to a limited extent through the “Nirmal Gram Puraskar” (NGP or Clean Village Prize) verification process but latrine use data is not available in the public domain and there is little effort to track sustainability in NGP-winning local governments (WSP, 2013). As a result, implementers are incentivized to prioritize latrine construction over use or sustainable behavior change (Wicken, 2008, WSP, 2013). The consequence, according to some experts, is that the program has been reduced to “a no-gain toilet construction scheme….where India built millions of toilets but people (did) not use them” (Jitendra et al., 16–31 January 2014).
Ensuring that populations with access to latrines actually use them requires an insight into the determinants of use (O’Reilly and Louis, 2014, Pattanayak et al., 2009). Research into the successful adoption and sustained use of latrines has revealed a range of factors that may potentially influence use, with health considerations only playing a minor role (Jenkins and Cairncross, 2010, Mara et al., 2010). Research suggests that latrine adoption may be motivated by a “prestige, well-being or situational drive”and that it may vary with gender, age, occupation, life-stage, travel experience, education, wealth and income, and the physical and social geography of the village environment with reference to the availability of good defecation sites around the home and/or villages (Jenkins and Cairncross, 2010, Jenkins and Curtis, 2005). Factors such as family size (O’Loughlin et al., 2006), privacy and safety for women and girls (Arnold et al., 2010), socio-economic status of the household and female literacy rates (Ghosh and Cairncross, 2014) may be associated with latrine use. Evidence also suggests that a preference for open defecation even among latrine owning households, especially those that received government subsidies for latrine construction versus those that did not (Coffey et al., 2014, Routray et al., 2015), may be a determinant of latrine use. Additional determinants of use may include social cohesion and peer influence (Crocker et al., 2016, Shakya et al., 2014) and access to water, supply-related and structural issues related to latrine construction (Barnard et al., 2013; ICRA, April 2011; Jenkins et al., 2014).
Measuring latrine use, at both household and individual levels, is challenging and a robust indicator for the same is not yet readily available for integration into large-scale household surveys (Bartram et al., 2014, Coffey and Spears, 2014). Despite certain limitations (Curtis et al., 1993, Schmidt and Cairncross, 2009, Zwane et al., 2011), self-report measures, such as a diary or survey, are popular measures of behavior assessment at both household and individual levels. Based on the results of a previously published study (Sinha et al., 2016), which compared various categories of reported latrine use and corresponding sensor-based latrine events, a reported latrine use measure of recall over the previous 48 h has been considered in this study.
The aim of this research is to assess patterns and determinants of individual latrine use over 12 months in a low income rural study population that had recently received latrines as part of the TSC in coastal Puri district in Odisha, India.
2. Materials and methods
2.1. Study context
We conducted the study among 25 villages in rural Puri, a coastal district of Odisha, India, that comprised part of the intervention arm of a randomized, controlled trial (the “Sanitation Trial”) to assess the health impact of rural sanitation under the Indian TSC (Clasen et al., 2012, Clasen et al., 2014). WaterAid and its partner NGOs conducted community mobilization and constructed pour-flush latrines among eligible “below the poverty line” households between January 2010 and March 2011.
2.2. Study design
The study followed a longitudinal design, with repeated follow up of the same population over a period of 12 months. This study design allowed us to explore the patterns of latrine use – the extent to which latrine use varied over seasons (dry hot, dry cold and rainy season), whether use was consistent – and the determinants of use.
2.3. Village and household selection
The sampling frame comprised 50 villages, spread across seven Blocks (district sub-divisions comprising several villages), which were part of the intervention arm in the Sanitation Trial. Villages were eligible for inclusion if they had at least one household that was enrolled in the Sanitation Trial surveillance (had a child under four years and/or a pregnant woman at baseline) with a constructed latrine as a result of the intervention. Of the 46 villages that were found to be eligible, 25 were randomly selected for this latrine use study using Block-level stratification and a computer-generated sequence. All surveillance households in the selected villages were eligible for inclusion in the study provided they had latrines. Eligible households were enrolled if they gave informed consent to participate in the study.
2.4. Measuring use
Our primary measure of individual latrine use was reported use by each member of the household over the prior 48 h. Our use of 48-h recall is based on our previous work suggesting that it may be the most reliable measure of assessing use via surveys (Sinha et al., 2016). We used a comprehensive survey-based tool that asked about place of defecation and latrine use for each household member listed in the household roster (Coffey and Spears, 2014). The survey was developed after extensive pilot testing in the field in 2011 and 2012. All the survey-based instruments used in this research were translated into the local language and the fieldwork was carried out by trained enumerators in 2012–2013. Reported latrine use data was gathered for each household member (ascribed a code) in all enrolled households in each of the three seasons, that is, dry cold, dry hot and rainy season. Individual members, if present and able to comprehend and respond to the questions, were directly queried about their latrine use behavior. If a household member was absent but still currently living in the household or was unable to respond to the questions, the primary household respondent, that is, the consenting female head of household or the eldest daughter-in-law, was asked to respond on his/her behalf.
The 48-h data was gathered by asking about latrine use “yesterday” and the “day-before yesterday”. Each reported 24 h period was also divided into four segments (Sunrise/Morning; Pre-Noon/Afternoon; Evening/Sunset; Night). Reported events were queried during each segment for each household member to aid more accurate recall. A recording of whether the response was reported or self-reported was made for each household member.
In order to provide information that may be more useful for programmatic and policy purposes, we classified latrine use into three categories—“never”, “sometimes” and “always/usually”—based on the previous 48 h reported use measure. Based on the results of a previously published study of defecation frequency in this region (Manas Kumar et al., 2013) and an analysis of pilot data collected during the Sanitation Trial, a conservative assumption was made that in this rural context, each person per household is likely to defecate at least once per day and at least two or more total events over the prior 48 h. Individuals that did not use the latrine on both days were considered “never” or non-users. To qualify as a “sometimes” user, the individual must have used the latrine at least once on either of the two days. To be included in the “always/usually” use category, individuals were expected to have used the latrine at least once on both days.
In order to examine the consistency of latrine use over time, we constructed a longitudinal measure of latrine use from participants’ responses to the 48 h recall measure at each study round. The longitudinal use measure was defined by the following criteria: “never use” included those with 0 events on both days per round resulting in 0 events over all 6 days; “always/usually use” was defined as ≥1 event per day per round resulting in ≥6 events over all 6 days; and “sometimes use” was defined as <1 event per day per round in any of the 3 rounds with total events >0 but <6 across the 6 days of queried use.
The survey also gathered additional household and individual level reported latrine use data, including the reasons given by the primary household respondent or non-using household members themselves, if present, for not using the latrine despite having access to one. Survey items regarding non-use of latrines were drawn from previous research (Banda et al., 2007; ICRA, April 2011; WSP, 2011) and a pilot study conducted in the early stages of research. Respondents were permitted to report multiple reasons for non-use, as applicable.
2.5. Predictor variables
The aforementioned survey also gathered data on covariates that may be associated with latrine use, including individual and contextual predictors, such as, age, gender, educational attainment, household size, demographic and socio-economic status (SES) of the household; and latrine construction and functionality status.
The gender and age of each member currently living in the household was recorded in each round of data collection. Based on evidence from previous research (WSP, March 2015) and a pilot study, which suggests that individuals of age three and below are not likely to use the latrine, we excluded this age group from our model. Age, modelled as a categorical variable, was grouped into the following quartiles: 4–12 years, 13–20 years, 21–40 years, 41–59 years, 60+ years. The ranges were chosen to capture potential variations in latrine use habits and practices, the ability to use the latrine and whether they were ambulatory or not (Routray et al., 2015). In this survey, we assessed household size in each round of data collection. Information on specific socio-economic variables was gathered only once for each study household. Educational attainment of the head of household and the primary care provider was modelled as a categorical variable (dichotomized as not completed primary school versus completed primary school). Data was gathered on the status of the household as a scheduled caste or scheduled tribe (SC/ST) and was dichotomized as yes or no. Asset ownership was recorded for each household. An asset index including watch/clock, pressure cooker, telephone, refrigerator, chair, mattress, cot, table, electric fan, sewing machine, water pump, scooter, animal drawn cart, thresher and tractor was constructed by calculating the tetrachoric correlation coefficients for the binary variables and then applying PCA analysis to the resulting correlation matrix (Howe et al., 2012, Vyas and Kumaranayake, 2006) The first component, explaining 57.7% variance of the items was used in the analysis. Study households were divided into five wealth quintiles based on their asset index, where quintiles 1 and 5 corresponded to the lowest and highest levels respectively.
We assessed latrine construction and functionality for each household in each season or round of data collection by directly inspecting the latrine and documenting the status of features such as type of latrine, height and type of latrine enclosure, presence and type of latrine closure over entrance, presence and type of latrine roof, floor material around pan, pan condition, the number of pits per latrine, and for each pit, as relevant, the height of the pit, condition of the pit cover and the pan-pit pipe connection. If a household had more than one latrine, each latrine was examined following the same parameters. Latrines were considered to be minimally functional if they met all the following criteria: pan that is not broken/choked/blocked; latrine pit (shared or independent); pit covering; and a pan-pit connection that is functional. In the model, we considered structural variables, including latrine wall/enclosure of at least four feet or more, a door/closure over the entrance for privacy, and the presence of a roof, separately to assess the impact of each of these covariates on latrine use.
The latrine−house and latrine−water source distances were calculated based on the Global Position System (GPS) location of every house, their latrine(s) and the reported water source used by the given household for ablution. While data was gathered in each round of data collection, for the purpose of this study, we have only considered GPS-based distance data from one round.
Data was entered using EPIData 3.1 (EpiData Association, Odense Denmark).
2.6. Data analysis
We examined the association between individual and household-level variables and latrine use using multinomial logistic regression. The regression analysis was done in two stages. First, we regressed the categorical measure of latrine use in the prior 48 h on all hypothesized determinants of use. Because data collection rounds were timed to correspond with the seasons, this model contained a categorical indicator of the season in which the measurement occurred. Next, we assessed the determinants of consistent use over the 12 month study period by regressing the latrine use measure derived from reported use across all three rounds on the same group of covariates. Models were fit with never use specified as the reference category in order to examine covariate effects on sometimes versus never use and always versus never use. Additional contrasts between outcome categories (e.g. always use versus sometimes use) were derived from fitted models using the listcoef command available in the SPost13 package (Long and Freese, 2014). The coefficients from all models were exponentiated to yield multinomial odds ratios, which are interpreted as the effect of a unit increase in the covariate on the odds of being in the specified outcome category rather than the reference category. In addition, we used marginal standardization to calculate the population-averaged predicted probabilities of use at specified covariate values (Muller and MacLehose, 2014). We adjusted the standard errors and 95% confidence intervals of the coefficient estimates using robust standard errors to account for the clustered structure of the data. Consistent with current recommendations, we adjusted for the highest level (villages) of clustering (Bottomley et al., 2016). In order to assess for potential bias due to a small number of higher-level clusters, we conducted sensitivity analyses adjusting for the next level of clustering, household-level with more than 300 clusters, and obtained comparable results. All analyses were conducted using Stata 14 (StataCorp, 2015).
2.7. Ethics
The latrine use assessment research was a sub-study of the Sanitation Trial and was granted ethics approval by the Ethics Committee of the London School of Hygiene and Tropical Medicine (Approval #5561, as amended) and by the Institutional Ethics Committee of the Xavier University, Bhubaneswar (Approval 310510, as amended). The Sanitation Trial was registered with ClinicalTrials.gov (Registration No. NCT01214785). Surveys and observations were undertaken only after obtaining informed, written consent from the male/female head of the household.
3. Results
3.1. Sampled population
The sampled population included in this study comprised 25 villages in Puri district. Of a total of 323 eligible households, 13 were excluded from analysis, including three that did not consent to participate in the study, three that had incompletely constructed latrines through the duration of the study, four where the study tools were vandalized and three with missing data on one of the household level covariates across all rounds of data collection. The analysis is based on data from a total of 1938 individuals living in 310 households. The sample excluded 266 individuals aged three years and below. Table 1 provides information on the characteristics of the study households and latrines at baseline. The analysis for the longitudinal measure of latrine use included 1178 individuals who were present in all three rounds.
Table 1.
Baseline characteristics of the study households and latrines.
| Variable | Sample unit | N (%) | Mean (SD) |
|---|---|---|---|
| Total households/25 villages | Households | 310 | |
| Total persons | Persons | 2204 | |
| Persons ≤3 years for duration of study | Persons | 266 | |
| Persons >3 years included in study | Persons | 1938 | |
| Age | Persons | 1938 | 32.24 years (19.41) |
| Gender | Persons | ||
| Male | 962 (49.64) | ||
| Female | 976 (50.36) | ||
| Household size | Households | 6.06 (2.90) | |
| Head of household completed primary school | Households | ||
| No | 136 (43.87) | ||
| Yes | 174 (56.13) | ||
| Mother/Carer of child completed primary school | Households | ||
| No | 76 (24.52) | ||
| Yes | 234 (75.48) | ||
| Scheduled caste/tribe | Households | ||
| No | 251 (80.97) | ||
| Yes | 59 (19.03) | ||
| Number of latrines per household | Households | ||
| One latrine | 268 (86.45) | ||
| Two latrines | 35 (11.29) | ||
| Three latrines | 7 (2.26) | ||
| Latrine wall height of atleast four feet or more | Households | ||
| No | 37 (11.94) | ||
| Yes | 273 (88.06) | ||
| Presence of latrine door/closure over entry | Households | ||
| No | 38 (12.26) | ||
| Yes | 272 (87.74) | ||
| Presence of latrine roof | Households | ||
| No | 149 (48.06) | ||
| Yes | 161 (51.94) | ||
| Own atleast one minimally functional latrinea | Households | ||
| No | 23 (7.42) | ||
| Yes | 287 (92.58) | ||
| Latrine distance measures | Households | ||
| Distance from latrine to water, mean (SD) | 18.68 (21.99) | ||
| Distance from latrine to house, mean (SD) | 12.96 (15.21) | ||
Minimally functional latrine: Latrine with pan that is not broken/choked/blocked, pit (shared or independent), pit covered, pan-pit connection that is functional.
3.2. Patterns of latrine use
Individual reported use in the study population was classified into “always/usually”, “sometimes” and “never” use. Derived from the regression model, the average response probability at any given round of never use was 43.5% (95% CI = 37.9, 49.1), sometimes use was 4.6% (95% CI = 3.8, 5.5), and always/usual use was 51.9% (95% CI = 46.2, 57.5). The model with the outcome defined as a longitudinal consistency of use measure (considering all three rounds/seasons) estimated the average response probability of never use as 30.1% (95% CI = 23.0, 37.2), sometimes use as 33.2% (95% CI = 28.3, 38.1), and always/usual use as 36.8% (95% CI = 31.8, 41.8). Descriptive statistics comparing the outcome measure in round one with that across all three rounds revealed that of those who reported that they always/usually used the latrine in round one, 66.6% were found to also report always/usually using it across all three rounds while 33.4% reported sometimes using it. Similarly, of those who reported never using the latrine in round one, 73.4% remained in the never use category and 26.6% reported sometimes using it when all three rounds were considered.
The results of the multinomial regression (Table 2) indicate a seasonal variation in reported individual latrine use behavior. Latrine use in the dry hot season was considered the reference group. In the dry cold season, the reported likelihood of always/usually versus never using the latrine was significantly greater than in the dry hot season (OR = 1.50, 95% CI = 1.18, 1.89, p = 0.001). The predicted probability of always/usual latrine use was 55.6% in the dry cold season and 47.4% in the dry hot season, an absolute increase of 8.2% (95% CI = 3.4, 13.0, p = 0.001). Conversely, we observed an absolute reduction of 7.1% (95% CI = 2.8, 12.6, p = 0.001) in the probability of never using a latrine during the dry cold season (40.5%) compared to the dry hot season (47.7%). The evidence also indicates that in the rainy season individuals were significantly more likely to report always/usually using the latrine versus never using it in comparison to the dry hot season (OR = 1.34, 95% CI = 1.07, 1.69, p = 0.012). The predicted probability of always/usual latrine use in the rainy season was 52.8%, an absolute increase of 5.6% (95% CI = 1.0, 9.7, p = 0.016), while the probability of never use during the rainy season (42.1%) was decreased by 5.4% (95% CI = 1.2, 10.1, p = 0.014) compared to the dry hot season. There were no observed seasonal differences in the probability of sometimes use.
Table 2.
The average response probability of the categories of latrine use – “always/usually”, “sometimes” and “never” use – in any given season or round and across all three seasons or rounds.
| Models | Never use (95% CI) | Sometimes use (95% CI) | Always/Usually use (95% CI) |
|---|---|---|---|
| At any given season/round (Pr) | 43.5 (37.9, 49.1) | 4.6 (3.8, 5.5) | 51.9 (46.2, 57.5) |
| Across all three season/round (Pr) | 30.1 (23.0, 37.2) | 33.2 (28.3, 38.1) | 36.8 (31.8, 41.8) |
3.3. Determinants of latrine use
3.3.1. Determinants of latrine use in any given season
Table 2 presents the results of multinomial logistic regression models of the association between reported individual latrine use (classified as “always/usually”, “sometimes” and “never”) in any given season and hypothesized predictors of use.
3.3.2. Gender
In the analysis, females were significantly more likely than males to report always or usually using the latrine versus never using it (OR = 2.24, 95% CI = 1.87, 2.68, p < 0.001). They were also significantly more likely than males to report sometimes using the latrine versus never using it (OR = 1.99, 95% CI = 1.48, 2.70, p < 0.001).
3.3.3. Age
While exploring the effect of age on latrine use, the reference group was age group 21 − 40 years. There was some evidence to suggest that the age group 4–12 years had a 58% increased likelihood of sometimes versus never using the latrine (OR = 1.58, 95% CI = 1.10, 2.27, p = 0.014) but a 43% decreased likelihood of always/usually using the latrine versus sometimes using it (OR = 0.57, 95% CI = 0.41, 0.78, p < 0.001). The age group 41–59 years was found to be significantly less likely than the reference group to always/usually use the latrine versus never using it (OR = 0.68, 95% CI = 0.53, 0.89, p = 0.004) and also always/usually use the latrine versus sometimes using it (OR = 0.66, 95% CI = 0.44, 0.97, p = 0.036). The oldest age group, comprising individuals who were 60+ years, were significantly less likely to both always/usually use the latrine versus never using it (OR = 0.56, 95% CI = 0.43, 0.73, p < 0.001) and sometimes use the latrine versus never using it (OR = 0.53, 95% CI = 0.30, 0.93, p = 0.028) when compared to the reference group.
3.3.4. Household size
There was evidence that members living in larger sized households were significantly less likely to report always/usually using the latrine versus never using it (OR = 0.92, 95% CI = 0.87, 0.97, p = 0.003). Persons in larger sized households were also significantly less likely to report sometimes using the latrine versus never using it (OR = 0.87, 95% CI = 0.83, 0.91, p < 0.001). There was no evidence of an association between always/usual use of the latrine versus sometimes and household size (p = 0.069).
3.3.5. Latrine construction
There was no evidence that latrine wall height or an enclosure of at least four feet or more was associated with any of the categories of reported latrine use. By contrast, the presence of a latrine door/closure significantly increased the likelihood of household members reporting always/usually using the latrine versus never using it (OR = 3.08, 95% CI = 1.80, 5.28, p < 0.001) and also sometimes versus never using it (OR = 2.92, 95% CI = 1.30, 6.58, p < 0.010). There was also evidence that the presence of a latrine roof significantly increased reported always/usual use of the latrine versus never use (OR = 2.00, 95% CI = 1.30, 3.09, p < 0.002) and also sometimes versus never using it (OR = 2.92, 95% CI = 1.77, 4.83, p < 0.001).
3.3.6. Latrine functionality
Latrines were considered minimally functional if the latrine met all the criteria of an un-broken and un-blocked pan, the presence of a pit (shared or independent), a pit covering and a functional pan-pit connection. Individuals that did not have even one minimally functional latrine were found to be significantly less likely to report always/usually versus never using the latrine (OR = 0.28, 95% CI = 0.13, 0.61, p < 0.001) or even sometimes using the latrine versus never using it (OR = 0.27, 95% CI = 0.08, 0.92, p = 0.037) when compared to individuals in households that had access to at least one minimally functional latrine. There was also some evidence that those who had two minimally functional latrines were significantly more likely to report both always/usually using the latrine versus never using it (OR = 2.35, 95% CI = 1.34, 4.13, p = 0.003) and sometimes using the latrine versus never using it (OR = 2.10, 95% CI = 1.03, 4.28, p = 0.041) in comparison to the reference group.
There was no evidence of an association between scheduled caste/tribe, educational attainment of the head of the household, household wealth quintile, distance to water supply and house with the reported latrine use categories (Table 2).
3.4. Determinants of consistent latrine use (across all three seasons)
Table 3 shows the association between the a priori selected co-variates and consistent individual latrine use.
Table 3.
Model showing the effect of individual and household-level predictors on individual latrine use based on prior 48 h recall (in any given season or round).
| Variable | Always/Usually vs. Never |
Sometimes vs. Never |
Always/Usually vs. Sometimes |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Multinomial Odds Ratio | 95% CI | p-value | Multinomial Odds Ratio | 95% CI | p-value | Multinomial Odds Ratio | 95% CI | p-value | |
| Female | 2.24 | 1.87, 2.68 | <0.001* | 1.99 | 1.48, 2.70 | <0.001* | 1.12 | 0.82, 1.53 | 0.470 |
| Age | |||||||||
| Age 4–12 years | 0.90 | 0.71, 1.14 | 0.365 | 1.58 | 1.10, 2.27 | 0.014* | 0.57 | 0.41, 0.78 | <0.001* |
| Age 13–20 years | 0.71 | 0.51, 1.01 | 0.056 | 0.84 | 0.45, 1.57 | 0.583 | 0.85 | 0.47, 1.54 | 0.597 |
| Age 21–40 years | Ref. | Ref. | Ref. | ||||||
| Age 41–59 years | 0.68 | 0.53, 0.89 | 0.004* | 1.04 | 0.72, 1.52 | 0.828 | 0.66 | 0.44, 0.97 | 0.036* |
| Age 60+ years | 0.56 | 0.43, 0.73 | <0.001* | 0.53 | 0.30, 0.93 | 0.028* | 1.05 | 0.62, 1.78 | 0.860 |
| Scheduled caste/tribe | 0.55 | 0.25, 1.22 | 0.143 | 0.58 | 0.39, 0.88 | 0.010* | 0.94 | 0.48, 1.86 | 0.864 |
| Head of household completed primary school | 1.34 | 0.89, 2.03 | 0.164 | 1.21 | 0.88, 1.68 | 0.245 | 1.11 | 0.76, 1.61 | 0.598 |
| Primary care giver completed primary school | 1.29 | 0.96, 1.73 | 0.095 | 1.01 | 0.63, 1.63 | 0.965 | 1.27 | 0.85, 1.91 | 0.248 |
| SES | |||||||||
| Wealth quintile 1 | Ref. | Ref. | Ref. | ||||||
| Wealth quintile 2 | 1.06 | 0.60, 1.91 | 0.821 | 1.32 | 0.65, 2.65 | 0.440 | 0.81 | 0.43, 1.52 | 0.513 |
| Wealth quintile 3 | 1.11 | 0.72, 1.70 | 0.650 | 1.13 | 0.52, 2.48 | 0.755 | 0.98 | 0.51, 1.86 | 0.940 |
| Wealth quintile 4 | 1.30 | 0.77, 2.19 | 0.326 | 1.04 | 0.59, 1.84 | 0.881 | 1.24 | 0.70, 2.21 | 0.457 |
| Wealth quintile 5 | 1.49 | 0.69, 3.19 | 0.309 | 0.92 | 0.45, 1.88 | 0.822 | 1.61 | 0.85, 3.05 | 0.141 |
| Household size | 0.92 | 0.87, 0.97 | 0.003* | 0.87 | 0.83, 0.91 | <0.001* | 1.05 | 0.99, 1.11 | 0.069 |
| Distance between latrine−latrine water source | 0.99 | 0.99, 1.00 | 0.312 | 0.99 | 0.99, 1.01 | 0.741 | 0.99 | 0.99, 1.00 | 0.493 |
| Distance between latrine−house | 0.99 | 0.99, 1.01 | 0.860 | 0.99 | 0.98, 1.01 | 0.324 | 1.00 | 0.99, 1.02 | 0.578 |
| Latrine wall ≥4 ft | 1.10 | 0.66, 1.84 | 0.703 | 0.88 | 0.45, 1.72 | 0.712 | 1.25 | 0.70, 2.26 | 0.453 |
| Latrine door | 3.08 | 1.80, 5.28 | <0.001* | 2.92 | 1.30, 6.58 | 0.010* | 1.05 | 0.51, 2.16 | 0.884 |
| Latrine roof | 2.00 | 1.30, 3.09 | 0.002* | 2.92 | 1.77, 4.83 | <0.001* | 0.68 | 0.43, 1.09 | 0.108 |
| Latrine functionality | |||||||||
| No minimally functional latrine | 0.28 | 0.13, 0.61 | 0.001* | 0.27 | 0.08, 0.92 | 0.037* | 1.04 | 0.46, 2.35 | 0.929 |
| One minimally functional latrine | Ref. | Ref. | Ref. | ||||||
| Two minimally functional latrines | 2.35 | 1.34, 4.13 | 0.003* | 2.10 | 1.03, 4.28 | 0.041* | 1.12 | 0.67, 1.88 | 0.673 |
| Season | |||||||||
| Dry hot | Ref. | Ref. | Ref. | ||||||
| Dry cold | 1.50 | 1.18, 1.89 | 0.001* | 1.00 | 0.67, 1.49 | 0.995 | 1.5 | 0.97, 2.31 | 0.071 |
| Rainy | 1.34 | 1.07, 1.69 | 0.012* | 1.26 | 0.88, 1.82 | 0.213 | 1.06 | 0.77, 1.46 | 0.704 |
p < 0.05.
The evidence suggests that gender remains a significant predictor of the categories of consistent latrine use where females were significantly more likely than males to report always/usual use of the latrine versus never use, sometimes use of the latrine versus never use, and also always/usual use of the latrine versus sometimes use. It may be inferred that the two oldest age groups, that is, individuals aged 41–59 years and individuals who were 60+ years, were significantly less likely to report always/usually using the latrine consistently versus never using it and always/usually using the latrine consistently versus sometimes using it in comparison to the age group 21–40 years. The results indicate that an increase in household size was significantly associated with a decreased likelihood of reported consistent always/usual use of the latrine versus never use. The evidence also suggests that the presence of a latrine door/closure significantly increased the likelihood of household members reporting consistent always/usual use of the latrine versus never use and also consistent sometimes versus never use. There was also evidence that the presence of a latrine roof significantly increased reported consistent always/usual use of the latrine versus never use and also consistent sometimes versus never use Table 4.
Table 4.
Model showing the effect of individual and household-level predictors on consistent individual latrine use (across all three seasons or rounds).
| Variable | Always/Usually vs. Never |
Sometimes vs. Never |
Always/Usually vs. Sometimes |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Multinomial Odds Ratio | 95% CI | p-value | Multinomial Odds Ratio | 95% CI | p-value | Multinomial Odds Ratio | 95% CI | p-value | |
| Female | 3.53 | 2.55, 4.89 | <0.001* | 1.83 | 1.53, 2.18 | <0.001* | 1.93 | 1.48, 2.52 | <0.001* |
| Age | |||||||||
| Age 4–12 years | 0.88 | 0.55, 1.40 | 0.592 | 1.48 | 0.93, 2.37 | 0.099 | 0.59 | 0.42, 0.84 | 0.004* |
| Age 13–20 years | 0.63 | 0.30, 1.31 | 0.216 | 0.75 | 0.38, 1.50 | 0.420 | 0.83 | 0.40, 1.74 | 0.630 |
| Age 21–40 years | Ref. | Ref. | Ref. | ||||||
| Age 41–59 years | 0.45 | 0.30, 0.67 | <0.001* | 0.68 | 0.43, 1.05 | 0.080 | 0.67 | 0.49, 0.91 | 0.011* |
| Age 60+ years | 0.34 | 0.19, 0.58 | <0.001* | 0.57 | 0.32, 1.01 | 0.054 | 0.59 | 0.40, 0.88 | 0.009* |
| Scheduled caste/tribe | 0.43 | 0.15, 1.24 | 0.117 | 0.42 | 0.24, 0.75 | 0.003* | 1.01 | 0.48, 2.17 | 0.971 |
| Head of household completed primary school | 1.10 | 0.54, 2.22 | 0.797 | 0.93 | 0.55, 1.59 | 0.796 | 1.18 | 0.75, 1.84 | 0.478 |
| Primary care giver completed primary school | 1.02 | 0.58, 1.76 | 0.957 | 0.83 | 0.42, 1.65 | 0.597 | 1.22 | 0.66, 2.28 | 0.529 |
| SES | |||||||||
| Wealth quintile 1 | Ref. | Ref. | Ref. | ||||||
| Wealth quintile 2 | 1.00 | 0.32, 3.11 | 1.000 | 1.06 | 0.44, 2.56 | 0.900 | 0.95 | 0.51, 1.75 | 0.856 |
| Wealth quintile 3 | 2.03 | 0.82, 5.04 | 0.125 | 2.73 | 1.20, 6.22 | 0.017* | 0.74 | 0.43, 1.28 | 0.289 |
| Wealth quintile 4 | 1.38 | 0.59, 3.25 | 0.458 | 1.21 | 0.57, 2.54 | 0.618 | 1.14 | 0.56, 2.32 | 0.711 |
| Wealth quintile 5 | 2.04 | 0.58, 7.17 | 0.266 | 1.15 | 0.37, 3.63 | 0.809 | 1.77 | 0.94, 3.35 | 0.079 |
| Household size | 0.92 | 0.86, 0.99 | 0.018* | 0.96 | 0.90, 1.03 | 0.256 | 0.96 | 0.89, 1.03 | 0.276 |
| Distance between latrine−latrine water source | 0.99 | 0.98, 1.01 | 0.497 | 1.00 | 0.99, 1.02 | 0.501 | 0.99 | 0.98, 1.00 | 0.029 |
| Distance between latrine−house | 0.99 | 0.97, 1.02 | 0.511 | 1.01 | 0.99, 1.02 | 0.196 | 0.98 | 0.96, 1.01 | 0.249 |
| Latrine wall ≥4 ft | 1.03 | 0.40, 2.69 | 0.946 | 0.85 | 0.36, 2.01 | 0.708 | 1.22 | 0.54, 2.77 | 0.635 |
| Latrine door | 7.29 | 1.60, 33.22 | 0.010* | 3.13 | 1.02, 9.59 | 0.046* | 2.33 | 0.92, 5.91 | 0.075 |
| Latrine roof | 4.73 | 2.23, 10.04 | <0.001* | 3.91 | 1.72, 8.90 | 0.001* | 1.21 | 0.89, 1.64 | 0.217 |
| Latrine functionality | |||||||||
| No minimally functional latrine | 0.34 | 0.08, 1.54 | 0.162 | 0.28 | 0.06, 1.40 | 0.121 | 1.22 | 0.27, 5.60 | 0.796 |
| One minimally functional latrine | Ref. | Ref. | Ref. | ||||||
| Two minimally functional latrines | 2.35 | 0.90, 6.12 | 0.081 | 1.27 | 0.38, 4.26 | 0.699 | 1.85 | 1.07, 3.17 | 0.025* |
p < 0.05.
There was no evidence of an association between SC/ST, education, SES, distance between latrine and house, distance between latrine and water source, latrine wall, the number of minimally functional latrines and reported consistent always/usually versus never use of the latrine.
3.5. Reported reasons for non-use of latrines
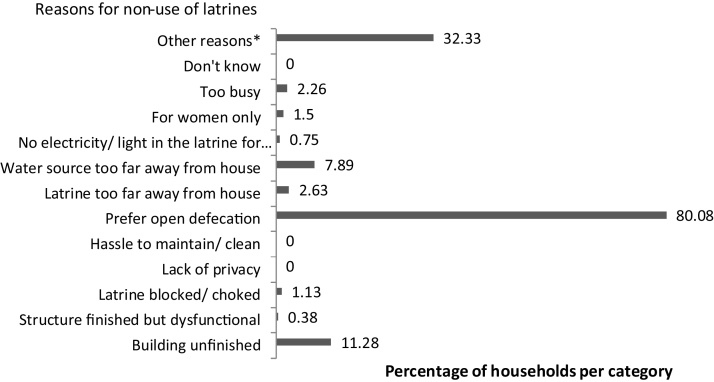
When households (N = 266) were queried on the likely reasons for non-use of latrines despite having access to facilities (Fig. 1), respondents from 80.1% households suggested that they preferred open defecation; 32.3% cited other reasons that were not among those listed in the survey; 11.3% felt that an un-finished latrine building prevented them from using it; and 7.9% and 2.6% gave distance of latrine from water source and distance between the latrine and house respectively as their main reasons for not using it. Furthermore, respondents from 2.3% of households reported that the latrine getting busy during peak use hours was among their reasons for not using the facility. Respondents from only 1.5% of households attributed non-use of the latrine to the perception that it is a facility to be exclusively used by women. Many of the reasons for open defecation referenced from other studies in this paper, including, for example, the hassle of cleaning and maintaining the facility as well as lack of privacy were not reported as likely reasons for non-use of latrines.
Fig. 1.
Reported reasons for non-use of latrines among latrine owning households in sample (N = 266).
4. Discussion
A few major observations emerged from monitoring individual latrine use in a rural coastal population in Odisha, India. First, individuals living in households with access to latrines do not all use the facilities, suggesting that latrine coverage does not necessarily translate into use. Second, we observed seasonal variation in latrine use in the study sample, implying that individuals do not consistently use the facilities throughout the year. Third, based on our data, we found that certain individual and household-level variables were significant predictors of individual latrine use, both when assessed in any given season or longitudinally. Fourth, among the cited reasons for non-use of household latrines, we found that a preference for open defecation was the predominant stated reason for not using the facility.
If the ideal may be assumed to be the use of a sanitation facility by all members of a household (including men and women, boys and girls, elderly, people with disabilities) whenever needed (WHO-UNICEF, 2014b; October 2015), we found evidence to suggest that latrine use is low in the study population. The study findings revealed that the average response probability of never using the latrine in the prior 48 h was 43.5% when assessed in any given season. The probability decreased to 30.1% when a longitudinal latrine use measure was considered. The latter individual level estimate is similar to the 37% reported in another study conducted in the same region (Barnard et al., 2013) but is greater than seen elsewhere in India (Coffey et al., 2014). Strikingly, our data also suggests a decrease in the average response probability of individuals who report always/usually using the latrine from 51.9%, when assessed in any given season, to 36.8%, when assessed longitudinally. This finding underscores the challenge in ensuring latrine use, which is also consistent and sustained, regardless of widespread subsidized latrine construction efforts spearheaded by the government in the region. Our findings resonate with messaging from other studies (Clasen et al., 2014, Coffey et al., 2014, Patil et al., 2014) that latrine coverage and access does not always translate into latrine use or meaningful reductions in open defecation. This issue presents a key challenge to the Government’s sanitation program and merits strategic and immediate action if sanitation targets are to be met.
Our analysis revealed that season was significantly related to latrine use. After adjusting for socio-demographic and latrine characteristics, the odds and average probability of always/usually using a latrine versus never were greater in the winter and rainy season than in the summer. Increased latrine use in the winter months may be attributed to various reasons including, the early morning and late evening winter chill that acts as a deterrent to open defecation; longer nights in winter and related concerns about safety in venturing too far from the house; the fields are inaccessible during the rice growing season (approximately September–January) (Routray et al., 2015). Previous research also points to the seasonal availability (or lack thereof) of open defecation sites as a partial explanation for the observed variations in latrine use. It has been suggested that open defecation is typically most challenging in the rainy season as fields and low-lying land are inundated with water, there are fears of insect and snake bites, and defecating on raised land along the road is inconvenient (ICRA, April 2011; Routray et al., 2015). In contrast, the summer months, particularly the initial months, tend to be more conducive to open defecation as crop harvesting is complete and the fields are once again clear; the weather is pleasant both early in the morning and late in the evening (Routray et al., 2015).
Gender, age, household size, latrine door and latrine roof were associated with both the 48 h recall measure and the longitudinal or consistent measure of latrine use, while level of education was not.
Among the non-health issues that act as drivers for the adoption and use of sanitation facilities at the household-level, gender plays an important role (Arnold et al., 2010, Coffey et al., 2014). This view is corroborated by our study findings where gender was found to be a strong predictor of individual latrine use. Access to sanitation facilities, particularly individual household latrines, has been found to lower the risk of violence and sexual abuse among women and enables them to deal with defecation, menstrual hygiene and pregnancy safely and discreetly (Arnold et al., 2010, Fisher, 2006). It permits women to defecate when the need arises as opposed to following a “schedule” of early morning or late evening/night visits to the fields (Routray et al., 2015). The resulting time and energy savings from using a household latrine is thought to free up more time that may be spent on “child care, domestic hygiene, increased rest time and community development work” (Pearson and Mcphedran, 2008).
Broadly, our findings suggest that the likelihood of reportedly never (compared to always) using the latrine (and presumably, defecating in the open) increases with age, with the most notable rise among the 60+ year age group. These results mirror those from another north-Indian study where open defecation rates increased sharply among individuals who were about 60 years or above (Coffey et al., 2014). It may be because this generation belongs to a cohort where open defecation in India was even more wide-spread than it is today and they are un-willing to re-habituate themselves to use a latrine (O’Reilly and Louis, 2014, Routray et al., 2015). Further, this age-group has a relatively higher social status with fewer inhibitions about enacting their preferences (Coffey et al., 2014, Routray et al., 2015).
As expected, structural features of the latrine, such as a door/closure over entry and a roof appear to be significant predictors of individual latrine use. This finding is consistent with previous evidence that suggests that latrine structures that are functional, perceived to be more durable and robust are also more likely to be used (Barnard et al., 2013; ICRA, April 2011; Planning Commission, 2013).
Among the predictors that were not significantly associated with individual latrine use, educational attainment of the household head and the carer appears to be counter-intuitive. Despite previous evidence to the contrary (Ghosh and Cairncross, 2014, O’Loughlin et al., 2006), a plausible explanation for this finding may be that until the intervention was introduced, less than 10% households had access to a latrine (Clasen et al., 2012). It may be inferred that the normative behavior in this region was open defecation. Since un-learning an “established age-old practice” that has little or no stigma attached to it (Banda et al., 2007, Coffey et al., 2014, Ghosh and Cairncross, 2014, Planning Commission, 2013) is likely to be challenging, there may be a time lag before awareness levels increase and educational attainment begins to effect sanitation behavior. Other predictors that were not significantly associated with individual latrine use were the distances between the latrine and house and the latrine and water source. It is often asserted that the post defecation practice of washing in India and flushing deems access to water as an important pre-condition to latrine use (ICRA, April 2011; O’Reilly and Louis, 2014). However, other evidence (Coffey et al., 2014, Desai and Vanneman, 2010) also supports our finding that convenient access to water may not be a predictor of individual latrine use.
Regardless of the intensity and scale of the government-led sanitation intervention, which aims to reduce open defecation rates in rural India, people persist with the practice. This preference for open defecation, even among those with access to a latrine, has been revealed in this study and also resonates with findings from other studies (Coffey et al., 2014, Planning Commission, 2013). It has been suggested that this challenge may be addressed through intensive and targeted behavior change campaigns, which may be slow initially but once “adopted by a critical mass of people…become self-sustaining” (Sinha, 4 July 2016).
A number of limitations should be considered in the interpretation of these results. First, the observational nature of the study limits our ability to draw causal inferences, although we have attempted to account for temporality between predictor and outcome variables to gain better insight into likely associations, if any. Second, the population of households from which the sample was drawn was not representative of all households that received the intervention in a village as only those with a child under four years and/or a pregnant woman at baseline were included in the sampling frame. Third, reported use in the previous 48 h was considered the primary measure for latrine use in this study based on empirical evidence from comparisons with instrumented monitoring. However, there is the potential of reporting bias and resulting imprecision in the latrine use measure. Fourth, the classification criteria for the categories of latrine use based on prior 48 h recall may not be adequate to characterize consistency of use or intra-personal use. We have, therefore, also derived a longitudinal measure of use based on all three seasons, in an attempt to address this issue. However, the model with the longitudinal measure cannot incorporate time-variant co-variates. Fifth, the possibility that the observed relationship between individual latrine use and the predictors of use may be due to the omission of certain unidentified variables might still be a concern in the interpretation of our results. However, an attempt has been made to include a reasonably comprehensive set of predictor variables that are likely to be associated with the outcome − individual latrine use. Finally, the study does not attempt to examine the extent to which latrine use may be associated with certain health outcomes of interest, for example, diarrhea, stunting or intestinal nematode infection, which were addressed in the Sanitation Trial. No attempt was made in this regard as evidence from the Sanitation Trial indicated that the intervention had no effect on the health outcomes of interest (Clasen et al., 2014).
5. Conclusions
To conclude, our study considers the methodological benefit in assessing longitudinal or consistent latrine use relative to use at a given time. It also suggests that the construction of subsidized latrines by the government in rural Odisha is insufficient to adequately address the “human development emergency” (Coffey et al., 2014) resulting from open defecation. Government policies and implementation practices that emphasize a strategic shift from building latrines to effectively triggering behavior change in the population may increase the demand for latrine use (MoDWS, 22 August 2014). This may be achieved through targeted interventions focused on an understanding of individual and household-level factors that presumably drive use of sanitation facilities.
Disclosures
The authors have declared that no competing interests exist.
Financial support
This work was supported by the Bill & Melinda Gates Foundation, International Initiative for Impact Evaluation (3ie), and Department for International Development-backed SHARE Research Consortium at the London School of Hygiene and Tropical Medicine. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Acknowledgements
The authors thank all the study participants who contributed to this study. We also thank the field team for supporting data collection, the rest of the team based in Bhubaneswar, Odisha, India, for providing administrative and logistical support, and Matthew Freeman for assistance with the sampling strategy and other aspects of the study.
References
- Arnold B.F., Khush R.S., Ramaswamy P., London A.G., Rajkumar P., Ramaprabha P., Durairaj N., Hubbard A.E., Balakrishnan K., Colford J.M.J. Causal inference methods to study non-randomized, pre-existing development interventions. Proc. Natl. Acad. Sci. U. S. A. 2010;107:22605–22610. doi: 10.1073/pnas.1008944107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banda K., Sarkar R., Gopal S., Govindarajan J., Harijan B.B., Jeyakumar M.B., Mitta P., Sadanala M.E., Selwyn T., Suresh C.R., Thomas V.A., Devadason P., Kumar R., Selvapandian D., Kang G., Balraj V. Water handling, sanitation and defecation practices in rural southern India: a knowledge, attitudes and practices study. Trans. R. Soc. Trop. Med. Hyg. 2007;101:1124–1130. doi: 10.1016/j.trstmh.2007.05.004. [DOI] [PubMed] [Google Scholar]
- Banerjee T., Mandal K. 2011. Revisiting the Midnapore Model After Ten Years of Total Sanitation Campaign in India. (Available at SSRN 1768687) [Google Scholar]
- Barnard S., Routray P., Majorin F., Peletz R., Boisson S., Sinha A., Clasen T. Impact of Indian total sanitation campaign on latrine coverage and use: a cross-sectional study in Orissa three years following programme implementation. PLoS One. 2013;8:e71438. doi: 10.1371/journal.pone.0071438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartram J., Brocklehurst C., Fisher M.B., Luyendijk R., Hossain R., Wardlaw T., Gordon B. Global monitoring of water supply and sanitation: history, methods and future challenges. Int. J. Environ. Res. Public Health. 2014;11:8137–8165. doi: 10.3390/ijerph110808137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bottomley C., Kirby M.J., Lindsay S.W., Alexander N. Can the buck always be passed to the highest level of clustering? BMC Med. Res. Methodol. 2016;16:1. doi: 10.1186/s12874-016-0127-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clasen T., Boisson S., Routray P., Cumming O., Jenkins M., Ensink J.H., Bell M., Freeman M.C., Peppin S., Schmidt W.-P. The effect of improved rural sanitation on diarrhoea and helminth infection: design of a cluster-randomized trial in Orissa, India. Emerg. Themes Epidemiol. 2012;9:7. doi: 10.1186/1742-7622-9-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clasen T., Boisson S., Routray P., Torondel B., Bell M., Cumming O., Ensink J., Freeman M., Jenkins M., Odagiri M., Ray S., Sinha A., Suar M., Schmidt W.-P. Effectiveness of a rural sanitation programme on diarrhoea, soil-transmitted helminth infection, and child malnutrition in Odisha, India: a cluster-randomised trial. Lancet Glob. Health. 2014;2:e645–e653. doi: 10.1016/S2214-109X(14)70307-9. [DOI] [PubMed] [Google Scholar]
- Coffey D., Spears D. Research Institute for Compassionate Economics; 2014. How can a Large Sample Survey Monitor Open Defecation in Rural India for the Swatch Bharat Abhiyan? Working Paper.www.susana.org/_resources/documents/default/3-2176-7-1424791330 (Available at Accessed 12 April 2015) [Google Scholar]
- Coffey D., Gupta A., Hathi P., Khurana N., Spears D., Srivastav N., Vyas S. Revealed preference for open defecation. Econ. Pol. Wkly. 2014;49:43. [Google Scholar]
- Crocker J., Abodoo E., Asamani D., Domapielle W., Gyapong B., Bartram J. Impact evaluation of training natural leaders during a community-led total sanitation intervention: a cluster-randomized field trial in Ghana. Environ. Sci. Technol. 2016;50:8867. doi: 10.1021/acs.est.6b01557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtis V., Cousens S., Mertens T., Traore E., Kanki B., Diallo I. Structured observations of hygiene behaviours in Burkina Faso: validity, variability, and utility. Bull. World Health Org. 1993;71:23–32. [PMC free article] [PubMed] [Google Scholar]
- DDWS . Guidelines: Central Rural Sanitation Programme, Total Sanitation Campaign (July 2011) In: G.o.I, editor. Department of Drinking Water and Sanitation; 2011. [Google Scholar]
- Desai S., Vanneman R. Inter-university Consortium for Political and Social Research [distributor]; Ann Arbor, MI: 2010. National Council of Applied Economic Research, New Delhi. India Human Development Survey (IHDS), 2005; pp. 06–29. (ICPSR 22626-v8) [Google Scholar]
- Fisher J. 2006. For Her Its the Big Issue Putting Women at the Centre of Water Supply Sanitation and Hygiene. [Google Scholar]
- Ganguly S.C. India’s national sanitation and hygiene programme: from experience to policy West Bengal and Maharashtra models provide keys to success. In: Wicken J., Verhagen J., Sijbesma C., Da Silva C., Ryan P., editors. Beyond Construction: Use by All. WaterAid; London: 2008. [Google Scholar]
- Ghosh A., Cairncross S. The uneven progress of sanitation in India. J. Water Sanit. Hyg. Dev. 2014;4:15–22. [Google Scholar]
- Howe L.D., Galobardes B., Matijasevich A., Gordon D., Johnston D., Onwujekwe O., Patel R., Webb E.A., Lawlor D.A., Hargreaves J.R. Measuring socio-economic position for epidemiological studies in low-and middle-income countries: a methods of measurement in epidemiology paper. Int. J. Epidemiol. 2012:s037. doi: 10.1093/ije/dys037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ICRA . UNICEF; 2011. Study to Assess Gaps Responsible for Low Utilization of TSC Among Tribal Population of Orissa: Final Report. (April) [Google Scholar]
- Jenkins M., Cairncross S. Modelling latrine diffusion in Benin: towards a community typology of demand for improved sanitation in developing countries. J. Water Health. 2010;8:166–183. doi: 10.2166/wh.2009.111. [DOI] [PubMed] [Google Scholar]
- Jenkins M.W., Curtis V. Achieving the ‘good life’: Why some people want latrines in rural Benin. Soc. Sci. Med. 2005;61:2446–2459. doi: 10.1016/j.socscimed.2005.04.036. [DOI] [PubMed] [Google Scholar]
- Jenkins M.W., Freeman M.C., Routray P. Measuring the safety of excreta disposal behavior in India with the new safe san index: reliability, validity and utility. Int. J. Environ. Res. Public Health. 2014;11:8319–8346. doi: 10.3390/ijerph110808319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jitendra, Gupta A., Bera S., Jacob N. India's Sanitation Programme: Mission Possible, Down to Earth. In: Narain S., editor. Society for Environmental Communications; New Delhi, India: 2014. pp. 30–37. (January 16–31) [Google Scholar]
- Long J.S., Freese J. third edition. Stata Press; College Station, TX: 2014. Regression Models for Categorical Dependent Variables Using Stata. [Google Scholar]
- Manas Kumar P., Sanjib Kumar K., Shivaram Prasad S. Defecation frequency and stool form in a coastal Eastern Indian population. J. Neurogastroenterol. Motil. 2013;19:374–380. doi: 10.5056/jnm.2013.19.3.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mara D., Lane J., Scott B., Trouba D. Sanitation and health. PLoS Med. 2010;7:e1000363. doi: 10.1371/journal.pmed.1000363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MoDWS G. Swachh Bharat Mission - action plan of the ministry of drinking water and sanitation, government of India. Draft of Note for Distribution to State Governments for Further Discussion on 25th August 2014 in Review Meeting. 2014 (Ministry of Drinking Water, Sanitation G.o.I., 22 August) [Google Scholar]
- Muller C.J., MacLehose R.F. Estimating predicted probabilities from logistic regression: different methods correspond to different target populations. Int. J. Epidemiol. 2014;43:962–970. doi: 10.1093/ije/dyu029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Sample Survey Office G.o.I . NSS 69th Round: July 2012 − December 2012? Ministry of Statistics & Programme Implementation, Government of India; 2013. Key indicators of drinking water, sanitation, hygiene and housing condition in India. (December) [Google Scholar]
- O'Loughlin R., Fentie G., Flannery B., Emerson P.M. Follow-up of a low cost latrine promotion programme in one district of Amhara, Ethiopia: characteristics of early adopters and non-adopters. Trop. Med. Int. Health. 2006;11:1406–1415. doi: 10.1111/j.1365-3156.2006.01689.x. [DOI] [PubMed] [Google Scholar]
- O’Reilly K., Louis E. The toilet tripod: understanding successful sanitation in rural India. Health Place. 2014;29:43–51. doi: 10.1016/j.healthplace.2014.05.007. [DOI] [PubMed] [Google Scholar]
- Patil S.R., Arnold B.F., Salvatore A.L., Briceno B., Ganguly S., Colford J.M., Jr., Gertler P.J. The effect of India's total sanitation campaign on defecation behaviors and child health in rural madhya pradesh: a cluster randomized controlled trial. PLoS Med. 2014;11:e1001709. doi: 10.1371/journal.pmed.1001709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pattanayak S.K., Yang J.-C., Dickinson K.L., Poulos C., Patil S.R., Mallick R.K., Blitstein J.L., Praharaj P. Shame or subsidy revisited: social mobilization for sanitation in Orissa, India. Bull. World Health Org. 2009;87:580–587. doi: 10.2471/BLT.08.057422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson J., Mcphedran K. A literature review of the non-health impacts of sanitation. Waterlines. 2008;27:48–61. [Google Scholar]
- Planning Commission, G.o.I . Government of India; 2013. Evaluation Study on Total Sanitation Campaign Planning Commission. [Google Scholar]
- Routray P., Schmidt W.-P., Boisson S., Clasen T., Jenkins M.W. Socio-cultural and behavioural factors constraining latrine adoption in rural coastal Odisha: an exploratory qualitative study. BMC Public Health. 2015;15:1. doi: 10.1186/s12889-015-2206-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanan D., Moulik S.G. The World Bank; New Delhi, India: 2007. Community-Led Total Sanitation in Rural Areas − An Approach That Works Water and Sanitation Program − South Asia. [Google Scholar]
- Schmidt W.-P., Cairncross S. Household water treatment in poor populations: is there enough evidence for scaling up now? Environ. Sci. Technol. 2009;43:986–992. doi: 10.1021/es802232w. [DOI] [PubMed] [Google Scholar]
- Shakya H.B., Christakis N.A., Fowler J.H. Association between social network communities and health behavior: an observational sociocentric network study of latrine ownership in rural India. Am. J. Public Health. 2014;104:930–937. doi: 10.2105/AJPH.2013.301811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha A., Nagel C.L., Thomas E., Schmidt W.P., Torondel B., Boisson S., Clasen T.F. Assessing latrine use in rural India: a cross-sectional study comparing reported use and passive latrine use monitors. Am. J. Trop. Med. Hyg. 2016:16–0102. doi: 10.4269/ajtmh.16-0102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha A. Indian Express Group; New Delhi: 2016. Tiolets Under Swachh Bharat Mission: Ready to Use, but Difficult to Flush Inhibitions, Indian Express. (4 July) [Google Scholar]
- StataCorp . StataCorp LP; College Station, TX: 2015. Stata Statistical Software: Release 14. [Google Scholar]
- Vyas S., Kumaranayake L. Constructing socio-economic status indices: how to use principal components analysis. Health Policy Plan. 2006;21:459–468. doi: 10.1093/heapol/czl029. [DOI] [PubMed] [Google Scholar]
- WHO . World Health Organization; 2014. UN-water Global Analysis and Assessment of Sanitation and Drinking-water (GLAAS) 2014 Report: Investing in Water and Sanitation: Increasing Access, Reducing Inequalities. [Google Scholar]
- WHO-UNICEF . World Health Organization; Geneva: 2014. Progress on Drinking Water and Sanitation: 2014 Update. [Google Scholar]
- WHO-UNICEF . 2014. WASH POST-2015: Proposed Targets and Indicators for Drinking-water, Sanitation and Hygiene. [Google Scholar]
- WHO-UNICEF . World Health Organization and United Nations Children’s Fund Monitoring Programme for Water Supply and Sanitation (JMP); 2015. Progress on Sanitation and Drinking-Water: 2015 Update and MDG Assessment WHO. [Google Scholar]
- WHO-UNICEF . WHO UNICEF Joint Monitoring Programme for Water Supply and Sanitation; 2015. The JMP Green Paper: Global Monitoring of Water, Sanitation and Hygiene Post-2015. (October) [Google Scholar]
- WSP . World Bank; 2011. A Decade of the Total Sanitation Campaign: Rapid Assessment of Processes and Outcomes. Water and Sanitation Program. [Google Scholar]
- WSP . World Bank; New Delhi, India: 2013. Linking Service Delivery Processes and Outcomes in Rural Sanitation: Findings from 56 Districts in India. Water and Sanitation Program. [Google Scholar]
- WSP . WSP-UNICEF; 2015. Child Feces Disposal in India. (March) [Google Scholar]
- Wicken J. WaterAid; London: 2008. Meauring Sanitation: Outcomes as Well as Outputs. [Google Scholar]
- Zwane A.P., Zinman J., Van Dusen E., Pariente W., Null C., Miguel E., Kremer M., Karlan D.S., Hornbeck R., Giné X. Being surveyed can change later behavior and related parameter estimates. Proc. Natl. Acad. Sci. 2011;108:1821–1826. doi: 10.1073/pnas.1000776108. [DOI] [PMC free article] [PubMed] [Google Scholar]