Abstract
Rationale:
Ectopic splenic autotransplantation refers to the heterotopic autotransplantation of splenic tissue and no treatment is necessary for it when patient is asymptomatic. Its incidence rate is reported up to 67% among patients with a history of splenic trauma and splenic surgery. The diagnosis of it before operation is really difficult, and it is easy to mimic as other tumors.
Patient concerns:
We reported a 42-year-old man with hepatic splenosis, with history of splenectomy for traumatic splenic rupture 16 years ago and hepatitis B&C. The patient was enrolled with recurrent low back pain for more than 1 month without any treatment.
Diagnoses:
Radiological imaging revealed a subcapsular hepatic nodule, showing “fast-in and fast-out” enhancement. Surgery was performed, and the result of histological diagnosis was hepatic splenosis.
Interventions:
No intervention before segmentectomy of the liver.
Lessons:
When imaging of a patient with history of traumatic splenic rupture or splenectomy shows1 or few well circumscribed hepatic nodules with enhancement in dynamic study, we should suspect hepatic splenosis, for the purpose of avoiding unnecessary surgery.
Keywords: computed tomography, hepatic carcinoma, intrahepatic splenosis, magnetic resonance imaging
1. Introduction
Ectopic splenic autotransplantation (ESAT) refers to the heterotopic autotransplantation of splenic tissue which is a benign condition and is frequently secondary to traumatic splenic rupture or splenectomy.[1] Its incidence rate is reported up to 67% among patients with a history of splenic trauma and splenic surgery.[2] ESAT is asymptomatic even without any surgical procedure and often incidentally diagnosed during imageological examinations.[3] ESAT can occur in any location of peritoneal cavity, thoracic cavity, pelvic cavity, skin incision, and so on.[4]
Hepatic splenosis refers to a heterotropic implantation of splenic fragments in the liver. Even though the actual mechanism of occurrence remains unresolved, there are 2 suspected possibilities: spleen cells may directly grow on the surface of the liver and then subside into the depths, or spleen cells may hematogenously spread through the splenic vein and are subsequently implanted in the liver.[3,5] Around 18 cases of hepatic splenosis have been reported in the literature during the last 10 years. Nineteen lesions in 10 cases (Table 1) with computed tomography (CT) or magnetic resonance imaging (MRI) were reviewed here, including solitary lesions in 5 cases[2,4,6–8] and multiple lesions in the rest.[1,3,5,9,10] Eighteen lesions among them were located along the capsule of the liver parenchyma, only 1 lesion was observed within the liver parenchyma but still closed to the liver capsule.[8] In these cases, 11 lesions were located in the left lobe, whereas 8 were located in the right lobe. Furthermore, the size of these nodules ranged from 0.6 to 5 cm.
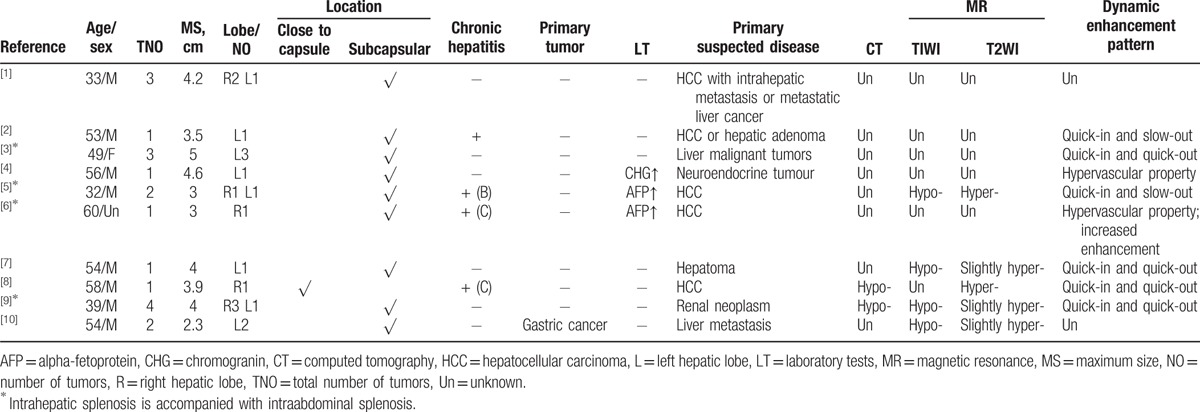
Table 1.
Review of the clinical and radiological characteristics of literatures about intrahepatic splenosis.
2. Case report
A 42-year-old man was enrolled with recurrent low back pain for more than 1 month without any treatment. He underwent splenectomy for traumatic splenic rupture 16 years ago. Physical examination was negative. Alpha-fetoprotein was 1.53 IU/mL. Serology analysis was positive for Hepatitis B virus antibody (Ab), antigen (Ag), pre-SI Ag, hepatitis B Core Antibody Immunoglobulin G, and hepatitis C virus antibody. CT of upper abdomen revealed a 23 × 18 mm sized isodense subcapsular hepatic nodule with CT value 52.9 HU in segment IV (SIV) of fatty liver (Fig. 1A). Dynamic enhanced CT imaging showed that the lesion had marked homogeneous enhancement in the arterial and portal venous phase with CT value 78.05 and 98.52 HU, respectively, and diminished enhancement in the equilibrium phase with CT value 68.56 HU (Fig. 1B–D). MRI showed a nodule hypointense on T1 weighted imaging (T1WI) and hyperintense on T2 weighted imaging (T2WI) (Fig. 2A–C). On MR dynamic enhanced images, this nodule showed moderate homogenous enhancement with marked delayed ring enhancement mimicking a pseudocapsule similar to hepatocellular carcinoma (HCC) in equilibrium phase (Fig. 2D–F). On the basis of image features and laboratory test findings, HCC could not be ruled out, resulting in segmentectomy of the liver.
Figure 1.
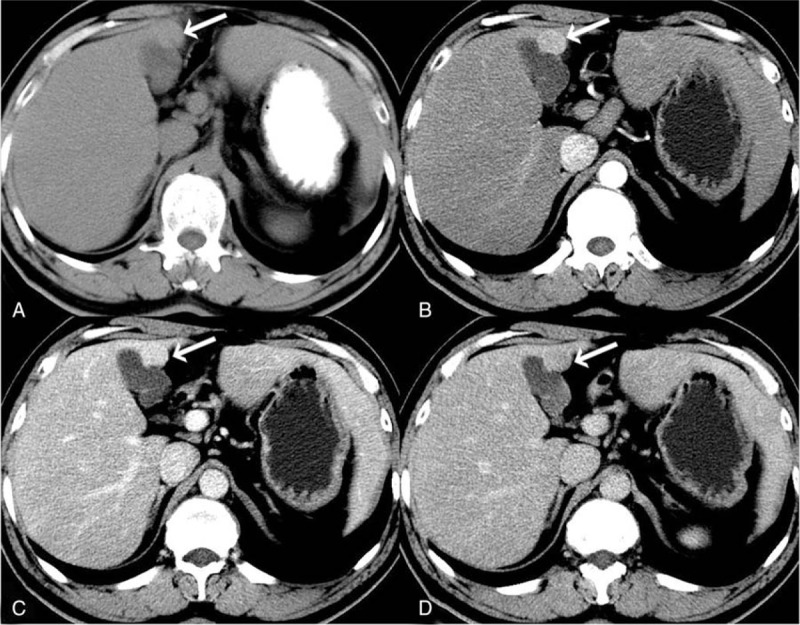
Computed tomography (CT) images of implanted hepatic splenosis. Noncontrast CT revealed a hypodense nodule in SIV of fatty liver (A). A dynamic study showed moderate homogenous enhancement in arterial (B), portal venous phase (C), and hypodensity in equilibrium phase with delayed rim enhancement (D). SIV = segment IV.
Figure 2.
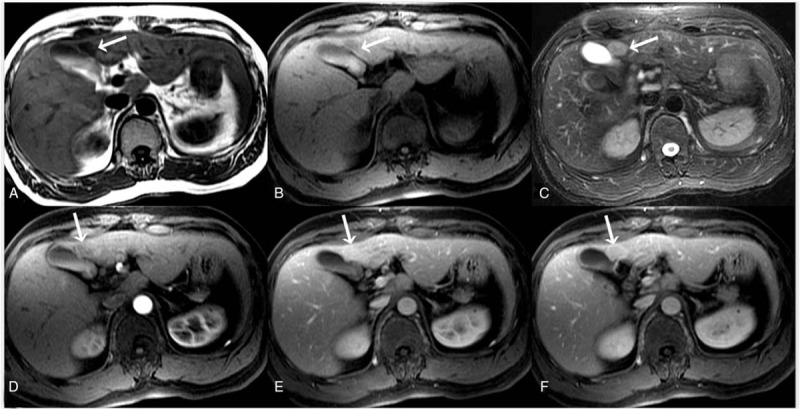
Magnetic resonance images of implanted hepatic splenosis. Magnetic resonance imaging showed a nodule in SIV which was homogenous hypointense on T1WI (A and B) and hyper-intensity on T2WI (C). On the gadolinium-diethylenetriamine pentaacetic acid dynamic-enhanced images, this nodule showed marked enhancement in the arterial phase (D) and portal venous phase (E) and appeared a hypointense lesion compared with the surrounding liver parenchyma in the equilibrium phase (F). In addition, its rim had obvious circular delayed enhancement during the enhancing process. SIV = segment IV, T1WI = T1 weighted imaging, T2WI = T2 weighted imaging.
During laparotomy, a pliablecrater-like reddish-brown nodule protruding from the surface of the liver was revealed in SIV, measuring 3 × 3 cm and having intact capsule. The subsequent histopathology of the resected lesion demonstrated redundant lymphocytes, scattered lymphoid follicles, and class trabecular structures, including fibrovascular tissues between hepatocytes and fatty infiltration (Fig. 3A and B). The histological findings confirmed hepatic splenosis.
Figure 3.
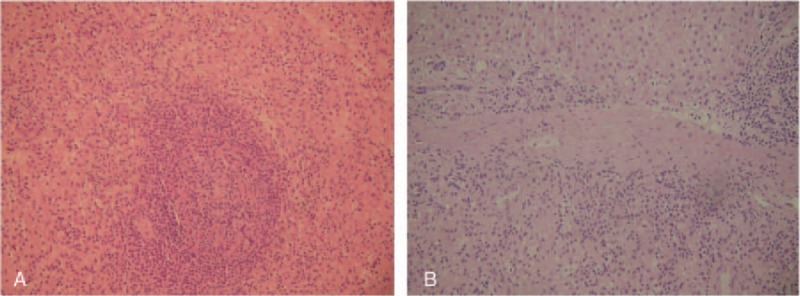
Hematoxylin and eosin staining (A × 100; B × 200) of the lesion demonstrated redundant lymphocytes, scattered lymphoid follicles, and class trabecular structures consisting of fibrovascular tissues between hepatocytes and also including fatty infiltration (A and B). The histological findings confirmed hepatic splenosis.
3. Discussion
According to the previous literature about hepatic splenosis, it is mostly found incidentally in the ultrasound examination of the liver as a hypoechoic mass, featuring clear margins and hyperechoic envelope which required further additional evaluation for definite diagnosis.
Generally, noncontrast CT reveals a well circumscribed iso- or hypodense mass in the liver, while noncontrast MRI demonstrates mild-to-moderate hyperintensity on T2-weighted image and hypointensity on the T1-weighted image. A dynamic study on CT and MRI shows a slight to intense enhancement, which may be homogeneous or heterogeneous during the arterial phase but enhancement is diversely during the portal venous and equilibrium phases in different cases. Compared with the surrounding hepatic parenchyma, the lesion could reveal hypodensity and hypointensity,[9] or hyperdensity[2] in the arterial phase. Or it can demonstrate diminished enhancement,[7,8] slight enhancement,[5] or increased enhancement[6] during the following phases. Also notable is that there is a case report[3] described the mass with fast-in and fast-out contrast enhancement on contrast enhanced CT imaging, which shows the feature of malignant tumors. Back on our case, against the background of fatty liver, the lesion was isodense on noncontrast CT images, meanwhile, showed hypointensity on the T1WI and hyperintensity on T2WI. A dynamic study both on CT and MRI showed marked homogeneous enhancement in the arterial and portal venous phase, whereas diminished enhancement in the equilibrium phase. Thus, it can be perceived that hepatic splenosis have no sufficient strong features on radiographic examination, leading to the confusion of differentiating hepatic splenosis from other hepatic diseases.
In the previous 10 cases, hepatic slpenosis was suspected as HCC in 6 cases (with history of chronic hepatitis in 3 cases,[5,7,8] fatty liver in 1 case,[2] and without any other associated disease in 2 cases[1,6]), as liver metastasis with the presence of gastric cancer in 1 case,[10] as malignant tumor in 1 case, and even mimicked a renal neoplasm in 1 case.[9] In our case, it was first misdiagnosed as HCC with the significant history of hepatitis B&C. Finally, all cases underwent surgical resection and the histological examination confirmed it to be splenic tissue.
As a matter of fact, hepatic splenosis in absence of any symptoms do not require clinical treatment. Hence, the differential diagnosis of the hepatic splenosis is particularly important.
Differential diagnoses in radiological diagnosis of splenosis include HCC, metastasis, cavernous hemangioma, and focal nodular hyperplasia (FNH). HCC has the characteristic fast-in and fast-out enhancement pattern, and it becomes hypointense on superparamagnetic iron oxide (SPIO) enhanced image relative to the liver parenchyma, while intrahepatic splenic nodes remain hyperintense. Furthermore, HCC's images sometimes could demonstrate vascular invasion or tumor thrombosis, biliary system invasion, adjacent lymph node swelling, and distant metastasis. Hepatic metastasis have typical features of multiple, variable sized, and low-density masses, which mostly have central degeneration and necrosis zone and contrast enhanced feature of “bull's-eye” which presents as the ring-like enhancement on portal venous phase. Hepatic cavernous hemangioma has a progressive centripetal enhancement and the lesion eventually merges with the background parenchyma. On MRI, it has uniform high signal intensity on T2WI, and the “bulb sign” appears with the extension of the echo time, which means it becomes significantly hyperintense. Typically, FNH is iso- or hypointense on T1WI, slightly hyper- or isointense on T2WI and has a hyperintense central scar on T2WI. Furthermore, it reveals intense homogeneous enhancement during the arterial phase and enhancement of the central scar during later phases.[11]
4. Conclusion
When liver imaging of a patient with history of traumatic splenic rupture or splenectomy shows 1 or few well circumscribed nodules with enhancement in the arterial phase, especially in the subcapsular area, we should suspect hepatic splenosis. MR SPIO enhancement and follow-up are recommended especially when the tumor markers are negative with nonspecific clinical symptoms, for the purpose of avoiding unnecessary surgery.
Footnotes
Abbreviations: Ab = antibody, Ag = antigen, CT = computed tomography, ESAT = ectopic splenic autotransplantation, FNH = focal nodular hyperplasia, HCC = hepatocellular carcinoma, MRI = magnetic resonance imaging, SPIO = superparamagnetic iron oxide.
Authors’ contribution: Images interpretation: M-YW, A-LL, and M-YS; drafting of the manuscript: M-YW; images collection: BL; histopathology images interpretation: DC; English writing revision: SQ.
Ethical approval: The present article does not contain any studies with human participants performed by any of the authors.
All of us certify that this manuscript a unique submission and is not being considered for publication by any other source in any medium.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Liu C, Liu J, Wang F. Intrahepatic splenosis mimicking liver cancer: report of a case and review of literature. Int J Clin Exp Pathol 2015;8:1031–5. [PMC free article] [PubMed] [Google Scholar]
- [2].Inchingolo R, Peddu P, Karani J. Hepatic splenosis presenting as arterialised liver lesion in a patient with NASH. Eur Rev Med Pharmacol Sci 2013;17:2853–6. [PubMed] [Google Scholar]
- [3].Liu Y, Ji B, Wang G, et al. Abdominal multiple splenosis mimicking liver and colon tumors: a case report and review of the literature. Int J Med Sci 2012;9:174–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Leong CW, Menon T, Rao S. Post-traumatic intrahepatic splenosis mimicking a neuroendocrine tumour. BMJ Case Rep 2013;2013:bcr2012007885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Choi GH, Ju MK, Kim JY, et al. Hepatic splenosis preoperatively diagnosed as hepatocellular carcinoma in a patient with chronic hepatitis B: a case report. J Korean Med Sci 2008;23:336–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Abu Hilal M, Harb A, ZeidanF B, et al. Hepatic splenosis mimicking HCC in a patient with hepatitis C liver cirrhosis and mildly raised alpha fetoprotein; the important role of explorative laparoscopy. World J Surg Oncol 2009;7:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Yu H, Xia L, Li T, et al. Intrahepatic splenosis mimicking hepatoma. BMJ Case Rep 2009;2009:bcr06.2008.0230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Sato N, Abe T, Suzuki N, et al. Intrahepatic splenosis in a chronic hepatitis C patient with no history of splenic trauma mimicking hepatocellular carcinoma. Am J Case Rep 2014;15:416–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Imbriaco M, Camera L, Manciuria A, et al. A case of multiple intra-abdominal splenosis with computed tomography and magnetic resonance imaging correlative findings. World J Gastroenterol 2008;14:1453–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Kang KC, Cho GS, Chung GA, et al. Intrahepatic splenosis mimicking liver metastasis in a patient with gastric cancer. J Gastric Cancer 2011;11:64–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Hussain SM, Terkivatan T, Zondervan PE, et al. Focal nodular hyperplasia: findings at state-of-the-art MR imaging, US, CT, and pathologic analysis. Radiographics 2004;24:3–19. [DOI] [PubMed] [Google Scholar]


