Abstract
This study reports the clinical emergency treatment of 68 critical patients with severe organophosphorus poisoning, and analyzes the prognosis after rescue.
The general data of 68 patients with severe organophosphorus poisoning treated in our hospital were retrospectively analyzed. These patients were divided into 2 groups: treatment group, and control group. Patients in the control group received routine emergency treatment, while patients in the treatment group additionally received hemoperfusion plus hemodialysis on the basis of routine emergency treatment. The curative effects in these 2 groups and the prognosis after rescue were compared.
Compared with the control group, atropinization time, recovery time of cholinesterase activity, recovery time of consciousness, extubation time, and length of hospital stay were shorter (P < .05); the total usage of atropine was significantly lower (P < .05); Glasgow Coma Score was significantly higher (P < .05); acute physiology and chronic health score (APACHE II) was significantly lower (P < .05); and mortality and poisoning rebound rate was significantly lower (P < .05) in the treatment group.
Hemoperfusion and hemodialysis on the basis of routine emergency treatment for critical patients with organophosphorus poisoning can improve rescue outcomes and improve the prognosis of patients, which should be popularized.
Keywords: critically ill organophosphate poisoning, first aid, prognosis
1. Introduction
Organophosphorus pesticide is an agricultural pesticide that is widely used in China, and its dosage reaches the maximum among other pesticides. It is estimated by the World Health Organization that approximately 200,000 persons die of organophosphorus pesticide poisoning per year.[1]
Critical organophosphorus poisoning is a common emergency disease. The method of poisoning is usually through oral use, followed by respiratory tract and skin contact. The oral use of organophosphorus pesticides results in the inhibition of cholinesterase activity and the aggregation of a large number of acetylcholine (ACh), causing clinical syndrome induced by failure after cholinergic nerve cord excitation. Patients develop vascular spasm and tissue hypoxia and ischemia induced by a large amount of ACh, which result in the release of a large number of inflammatory mediators, and leads to multiple organ dysfunction syndrome and microcirculation disorder.
The conditions of patients with severe organophosphorus poisoning are unstable with a high fatality rate, and immediate rescue and appropriate therapy are very vital for them. In order to improve the success rate of clinical treatment, a retrospective analysis is made of clinical treatment approaches of 68 patients with severe and acute organophosphorus poisoning admitted by the hospital as well as their prognosis.
2. Materials and methods
This study was conducted with approval from the Ethics Committee of Beijing Luhe Hospital Affiliated to Capital Medical University. Written informed consent was obtained from all participants.
2.1. Materials
From April 2013 to April 2014, 68 critical patients with severe organophosphorus poisoning treated in our hospital were enrolled into this study. All patients were in accordance with the criteria of the diagnosis and classification of the “diagnosis and treatment principles of occupational acute organophosphorus poisoning.”[2] Whole blood acetylcholinesterase activity was <30% in all patients. Informed consents are obtained from all patients’ families. Patients who received hemoperfusion and hemodialysis were included into the observation group, whereas patients who refused these treatments were included into the control group. These 68 patients were divided into 2 groups: treatment group and control group.
2.2. Methods
Patients in the control group received routine emergency treatment, including gastrolavage, catharsis, rehydration, maintenance of water-electrolyte balance, and anti-infection treatment. Atropine combined with pralidoxime treatment was additionally given: 1.2 to 1.6 g of pralidoxime was intravenously injected, this intravenous injection was performed once again after half an hour, and intravenous injection was maintained at .6 g/h for at least 1 day thereafter. Hereafter, this dose was halved day by day. The duration of use of pralidoxime was 2 to 3 days. The dose of atropine and injection interval were adjusted according to changes in the patient's condition, and these were adjusted every 5 to 20 minutes, to reach the atropinization status in the shortest possible time and to maintain atropinization. Mechanical ventilation was immediately given if ventilation-related indications appeared. For example, patients who develop acute respiratory failure, arterial partial pressure of oxygen (PaO2) <8.00 kPa (60 mm Hg), PaO2 > 6.0 kPa (45 mm Hg), acute respiratory distress syndrome caused by pulmonary edema, and progressive inspiratory dyspnea with hypoxia, oxygen, tracheal intubation, tracheotomy, and mechanical ventilation should be given. The vital signs of patients were closely monitored during the course of treatment. For patients with severe arrhythmia, toxic encephalopathy, cerebral edema, and cerebral hernia, symptomatic treatments should be given and life support should be strengthened.
Patients in the treatment group additionally received hemoperfusion and hemodialysis on the basis of routine emergency treatment. Direct puncture of the femoral vein and median cubital vein, or dual-lumen femoral vein catheterization were performed to establish an effective temporary vascular access. The hemoperfusion apparatus and blood dialyzer were connected in series, in which the hemoperfusion apparatus is set before the dialyzer. Anticoagulation was conducted with sodium heparin. The initial dose was 110 to 210 mg/kg, followed by 8 to 10 mg for every half an hour for maintenance. Bicarbonate dialysate was used. Blood flow was set at 100 to 160 mL/min, and dialysis fluid flow was set at 500 mL/min. Ultrafiltration started at 2000 mL/h. If the patient has a significant improvement in pulmonary edema, it was changed into 500 mL/h. Dialysis duration was 2 to 3 hours. The instruments used include a disposable HA230 hemoperfusion apparatus and single-pump hemodialysis machine (Japan).
2.3. Observation indexes
From hospitalization on, atropinization time, recovery time of cholinesterase activity, recovery time of consciousness, extubation time, length of hospital stay, mortality, poisoning rebound rate, and the success rate of rescue were recorded in detail.
Acute organophosphorus pesticide poisoning can cause consciousness disorders. Previous studies revealed that Glasgow Coma Score (GCS) can reflect the severity of illness, and acute physiology and chronic health score (APACHE-II) can precisely predict mortality risks and severity of patients with organophosphorus pesticide poisoning.[3–5] Hence, in this study, the above indicator was used to evaluate patients’ conditions and prognosis.
GCS: 13 to 14 points indicate mild coma, 9 to 12 points indicate moderate coma, and 3 to 8 points indicate severe coma. APACHE II: the score range within 0 to 71 points; the higher the score, the more serious the condition becomes.
2.4. Statistics processing
Data were analyzed using SPSS 19.0 statistics software. Measurement data were expressed as mean ± standard deviation (±SD), and were evaluated using t test. Count data were evaluated using Chi-square test. P < .05 was considered statistically significant.
3. Results
3.1. General information
The treatment group comprised 34 patients, including 18 male and 16 female patients. The age of these patients ranged within 19 to 66 years, with an average age of 46.6 ± 5.8 years. The amount of poison was 123.6 ± 45.3 mL. Visit times ranged from 10 minutes to 3 hours. Types of poisoning include the following: Dipterex poisoning in 13 patients, methyl parathion poisoning in 12 patients, methamidophos poisoning in 6 patients, and dichlorvos poisoning in 3 patients. The control group comprised 34 patients, including 17 male and 17 female patients. The age of these patients ranged within 18 to 66 years, with an average age of 45.9 ± 5.5 years. The amount of poison was 124.3 ± 41.2 mL. Visit times ranged within 10 minutes to 3 hours. Types of poisoning include Dipterex poisoning in 14 patients, methyl parathion poisoning in 10 patients, methamidophos poisoning in 5 patients, and dichlorvos poisoning in 5 patients. The difference in sex, age, visiting time, amount of poison, and types of poisoning between these 2 groups were not statistically significant (P > .05).
3.2. Frequency of post-treatment complications of both groups
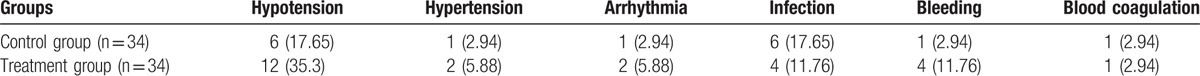
Thirty-four patients received hemodialysis and hemoperfusion for 345 times, and 25 patients had complications. According to the frequency of complications, it is estimated that 12 patients presented with hypotension, in addition with 4 patients with hemorrhage of digestive tract, 4 patients with infections, 2 patients with resistant hypertension, 1 patient with coagulation, 1 patient with arrhythmia, and 4 patients with bleeding (Table 1).
Table 1.
The frequency of complications for the 2 groups of patients after treatment (n [%]).
3.3. Incidence rate of organ failure in both groups
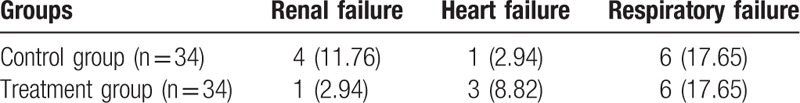
Among the 34 patients in the control group, there are 4 cases with renal failure (11.76%), 1 case with heart failure (2.94%), and 6 cases with respiratory failure (17.65%). Among the 34 patients in the treatment group, there is 1 case with renal failure (2.94%), 3 cases with heart failure (8.82%), and 6 cases with respiratory failure (17.65%) (Table 2).
Table 2.
The frequency of both groups having organ failure (n [%]).
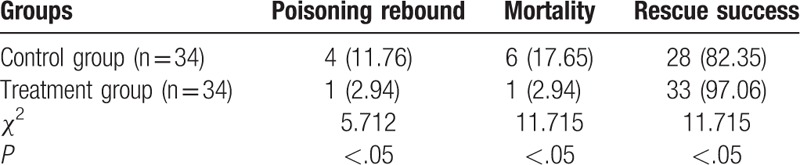
3.4. Comparison of rescue outcomes
As shown in Table 3, compared with the control group, rescue success rate was significantly higher in the treatment group (P < .05), whereas poisoning rebound rate and mortality were significantly lower in the treatment group (P < .05). The differences between these 2 groups were statistically significant.
Table 3.
Comparison of rescue outcomes.
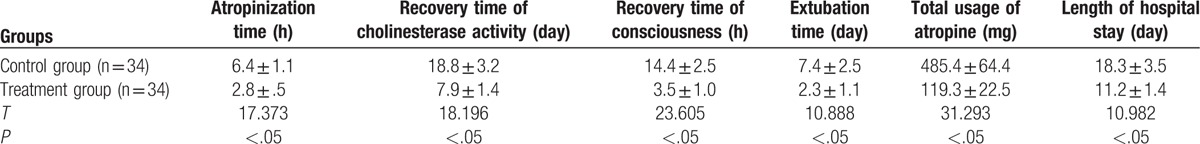
3.5. Comparison of the clinical effect and length of hospital stay
As shown in Table 4, compared with the control group, atropinization time, recovery time of cholinesterase activity, recovery time of consciousness, extubation time, and length of hospital stay were shorter in the treatment group (P < .05). Furthermore, the total usage of atropine was significantly lower (P < .05), and the differences between these 2 groups were statistically significant.
Table 4.
Comparison of the clinical effect and length of hospital stay.
3.6. Comparison of prognostic indicators
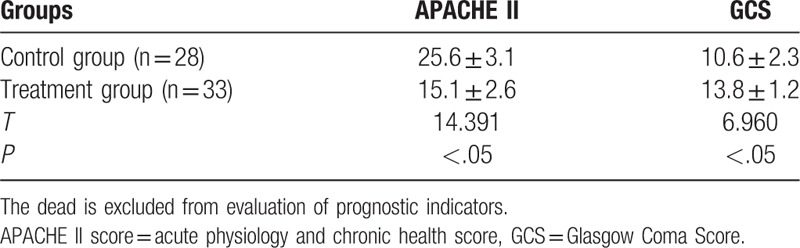
As shown in Table 5, after the success of the rescue, APACHE II score and GSC were significantly better in the treatment group than in the control group (P < .05); and the differences between these 2 groups were statistically significant.
Table 5.
Comparison of prognostic indicators.
4. Discussion
Studies[6,7] have reported that hemoperfusion and hemodialysis on the basis of routine treatment for organophosphorus pesticide poisoning could increase the success rate of rescue, and improve the prognosis of patients. The results of this study revealed the following: compared with the control group, the rescue success rate in patients who received hemoperfusion and hemodialysis based on routine treatment was significantly higher (P < .05); poisoning rebound rate and mortality were significantly lower (P < .05); and indicators related to clinical treatment effects, APACHE II score, and GCS were significantly better (P < .05), which were consistent with those reported in literature.
As shown in Table 1, compared with the observation group, hypotension and bleeding in the control group were increased. In the hemodialysis, patients’ heart rate and blood pressure change, and excessive ultrafiltration and ultrafiltration failure impact the body's blood volume; damage kalium and sodium balance; and disturb cardiac systole and diastolic functions.[8] Some studies showed that patients with loss of weight by >5% after hemodialysis were contracted with symptomatic hypotension; Excessive hemodialysis ultrafiltration volume and quick dehydration can reduce patients’ weight and cause hypotension.[9] The application of anticoagulation can aggravate hemorrhage of digestive tract.
Organ failure induced by severe organophosphorus poisoning may be related to the following factors: direct actions of organophosphorus pesticide and indirect actions causing secondary damages. Because of the early respiratory failure, cephaledema, and hypoxia, the body generates damage effect and then emits endotoxin and inflammatory mediums, and thus damaging body organs.[10] Early hemoperfusion and hemodialysis promote the elimination of endotoxin and the adsorption of inflammatory medium, reduce systematic inflammatory reaction, and quickly restore cholinesterase activity.[11] Hemodialysis and hemoperfusion reduce kidney burdens, so the incidence rate of renal failure is lower than that of the control group. In the hemodialysis process, patients’ heart rate and blood pressure change, and excessive ultrafiltration and ultrafiltration failure impact the body's blood volume; damage kalium and sodium balance; and disturb cardiac systole and diastolic functions. Hence, heart failure occurs, and consequently the proportion of heart failure increases. However, there are some limitations about hemoperfusion and hemodialysis treatment: increasing the fee and not applicable to the patients with severe heart failure and low blood pressure.
The routine use of specific antidote anticholinergic drug atropine can relieve the muscarinic symptoms of patients and resist central respiratory depression. The early, adequate and proper use of anticholinergic drugs is an important influence factor for the success of rescue.[12,13] However, if Atropine is used repeatedly in large dosage, many side effects occur; and Atropine does not well act on nicotinic symptoms and is unable to revive aged phosphorus acylation cholinesterase and pralidoxime iodide. Furthermore, regular drugs are unable to effectively eliminate inflammatory medium formed in the poisoning process, metabolites caused by organ damage or organophosphorus pesticide in the body. Meanwhile, organic pesticide has a strong lipid solubility, which leads to central respiratory failure through blood–brain barrier. Cholinesterase reactivators cannot pass through blood–brain barrier, so pralidoxime iodide combined with atropine is restricted in the treatment.
To date, blood purification technique is used for severe and acute organophosphorus poisoning, including continuous blood purification, hemodialysis, and hemoperfusion. However, in this study, the observation group adopts hemoperfusion combined with hemodialysis treatment. Hemoperfusion can sufficiently eliminate lipid-soluble poisons or poisons bonded with plasma proteins, especially lipid-soluble organophosphorus pesticide. It can remove poisons in blood as many as possible and reduce the incidence rate of complications caused by poisoning. Notwithstanding, hemoperfusion can only get rid of poisons, but it cannot filter excessive water. Therefore, it is unable to correct water and electrolyte disturbance and acid–base imbalance. If patients are combined with acute renal failure, pulmonary edema, heart failure, and cephaledema, its effects are unsatisfactory. In addition, hemoperfusion cannot guarantee blood temperature of extracorporeal circulation, so blood coagulation often occurs in the perfusion device. Hemodialysis technique can fully eliminate poisons with small molecular weight, low lipid solubility, and bonding rate with proteins depending on diffusion and ultrafiltration effects. This case is inapplicable to poisons with a high lipid solubility or binding rate with proteins. Therefore, hemoperfusion combined with hemodialysis is often used in clinical practices to treat patients with organophosphorus pesticide poisoning. Some studies[14,15] in China reported that hemoperfusion and hemodialysis can act on each other in the treatment of patients with severe organophosphorus pesticide poisoning, which not only improves the clearance rate of poisons, but keeps internal circulation in stable status. Furthermore, they can protect organs and reduces or even avoids multiple organ failure.
In summary, this study verifies that hemoperfusion and hemodialysis on the basis of routine treatment can improve the success rate of clinical rescue, and improve the prognosis of patients, which is worthy of clinical popularization and application for treating organophosphorus pesticides poisoning patients with renal insufficiency.
Footnotes
Abbreviations: ACh = acetylcholine, APACHE II score = acute physiology and chronic health score, ARDS = acute respiratory distress syndrome, GCS = Glasgow Coma Score, OP = organophosphate, PaO2 = partial pressure of oxygen, SD = standard deviation.
The authors have no conflicts of interest to disclose.
References
- [1].Eddleston M, Phillips MR. Self poisoning with pesticides. BMJ 2004;328:42–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Qian XX. Analysis of relationship between changes of cholinesterase and clinical poisoning degree: 60 cases. Chin Crit Care Med 2001;4:237–9. [Google Scholar]
- [3].Davies JO, Eddleston M, Buckley NA. Predicting outcome in acute organophosphorus poisoning with a poison severity score or the Glasgow coma scale. QJM 2008;101:371–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Lee P, Tai DY. Clinical features of patients with acute organophosphate poisoning requiring intensive care. Intensive Care Med 2001;27:694–9. [DOI] [PubMed] [Google Scholar]
- [5].Kang EJ, Seok SJ, Lee KH, et al. Factors for determining survival in acute organophosphate poisoning. Korean J Intern Med 2009;24:362–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Zhang X, Zhao W, Jing R, et al. Work-related pesticide poisoning among farmers in two villages of Southern China: a cross-sectional survey. BMC Public Health 2011;11:429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Lee KJ, Shin JW, Moon J, et al. An illustrative case of mixed pesticide poisoning with remarkable improvement: a case report. J Neurol Sci 2014;344:232–3. [DOI] [PubMed] [Google Scholar]
- [8].Du JH. Observation and treatment of acute complications during the hemodialysis. Baotou Yi Xue 2013;37:29–30. [Google Scholar]
- [9].Gao HB. Reason analysis and coping strategy of hemodialysis and its complication in the aging. J Clin Med Lit 2015;4:1825–6. [Google Scholar]
- [10].Qian HB, Zheng ZQ, Lu JH, et al. Analysis of the prognosis of 30 cases with multiple organ dysfunction syndrome (MODS) caused by acute organophosphorus poisoning. J Intern Intensive Med 2016;12:32. [Google Scholar]
- [11].Zhang HF, Zhang JS, Zhou HL. Clinical observation of 110 case with multiple organ dysfunction syndrome (MODS) caused by acute organophosphorus poisoning. Intern Med China 2006;12:130. [Google Scholar]
- [12].Yan YJ. Follow-up study of delayed damage caused by acute organophosphorus pesticide poisoning. Master Thesis: Shandong University; 2007. [Google Scholar]
- [13].Nan JY, Gao XY, Li HL, et al. Clinical observation of acute organophosphorus pesticide poisoning treated by Tuoning. J Xi’an Jiaotong Univ (Med Sci) 2006;6:622–4. [Google Scholar]
- [14].Zeng WJ. A clinical research of curing heavily organophosphorus pesticide toxicosis by hemoperfusion combined with discount. Guide China Med 2014. 4–5. [Google Scholar]
- [15].Du BH, Qiu YP, Song RR. Effective observation of plasma exchange combined with blood perfusion technique treating severe organophosphorus poisoning. J Clin Exp Med 2013. 1686–7. [Google Scholar]


