Abstract
Rationale:
Although some cases of recurrent bacteremia due to Campylobacter jejuni have been reported in immunocompromised patients, antibiotic treatment strategies to eradicate C. jejuni and prevent recurrent infections in immunocompromised patients have not been established. Authors’ experience of such rare cases should be shared for improving patients’ outcomes.
Patient concerns:
An 18-year-old boy with hypogammaglobulinemia, who received intravenous immunoglobulin replacement therapy every 3 weeks, was admitted to hospital repeatedly due to recurrent diarrhea and cellulitis of the leg.
Diagnoses:
The patient was admitted 6 times, and among them, C. jejuni was isolated from blood cultures 4 times and stool cultures 2 times.
Interventions:
The patient experienced recurrent C. jejuni enteritis and bacteremia 5 times despite macrolide therapy. Doxycycline was administered for 3 months after the fifth admission.
Outcomes:
Ten months after the completion of doxycycline therapy for 3 months, C. jejuni enteritis relapsed; however, since then, recurrent infection has not occurred for 10 months.
Lessons:
Immunocompromised patients can experience recurrent C. jejuni infection despite prolonged antibiotic therapy. Further studies to establish appropriate antibiotic therapy for eradicating colonized C. jejuni and preventing recurrent infection are needed.
Keywords: agammaglobulinemia, bacteremia, Campylobacter jejuni, recurrence
1. Introduction
Campylobacter spp. is one of the most common pathogens causing infectious enterocolitis.[1] In humans, most cases of Campylobacter infections are caused by Campylobacter jejuni, manifested as a self-limiting enterocolitis.[1] Patients with human immunodeficiency virus (HIV) infections and immunocompromised patients, including those with hypogammaglobulinemia, are especially susceptible to Campylobacter infections.[2] Infections in these patients were reported to be severe, prolonged, and recurrent.[2]Campylobacter spp. is the most common cause of infectious diarrhea in patients with hypogammaglobulinemia,[3] and cases of recurrent bacteremia associated with C. coli and C. lari, as well as C. jejuni have been reported in patients with hypogammaglobulinemia.[4–6] In spite of this, an antibiotic treatment strategy for immunocompromised patients experiencing recurrent Campylobacter infections has not been established, and no study on the prevention of recurrent Campylobacter infections has been implemented.
We report a case of an 18-year-old boy with underlying hypogammaglobulinemia, who experienced recurrent C. jejuni bacteremia 4 times in a period of 8 months. His diarrhea resolved with doxycycline administration for 3 months; however, C. jejuni enteritis recurred 10 months after the completion of doxycycline therapy. Future studies should be performed to determine appropriate antibiotic therapy for immunocompromised patients experiencing recurrent Campylobacter infections. This report was approved by the Institutional Review Board of Seoul St. Mary's Hospital (Approval number: KC16ZISE0757).
2. Case presentation
An 18-year-old boy was admitted to the hospital complaining of persistent cough and painful swelling with focal redness on the left shin. The patient had been diagnosed with hypogammaglobulinemia at 1 year of age, and subsequently received intravenous immunoglobulin (IVIG) replacement therapy every 3 weeks. Due to the parents’ opposition, genetic studies for X-linked agammaglobulinemia had never been performed. On admission, a chest radiography showed a pneumonic consolidation on the left lower lobe. Blood tests revealed a white blood cell (WBC) count of 7120/mm3 (neutrophils, 80.8%; lymphocytes, 12.4%; and monocytes, 6.6%), hemoglobin level of 8.4 g/dL, and a platelet count of 22,000/mm3. Blood chemistry tests showed no abnormalities. The last IVIG was administered 1 week before this admission, and the serum IgG level was 418 mg/dL on admission. He was diagnosed with pneumonia and cellulitis of the left leg based on his presenting symptoms and X-ray findings. Intravenous cefazolin and amikacin were administered for cellulitis of the leg, and oral roxithromycin was administered for pneumonia. He developed a fever on hospital day (HD) 2, which resolved on HD 5. Diarrhea occurred only on HD 3. The stool culture grew no pathogens, and occult blood and WBC were negative. C. jejuni was identified on the blood culture that was performed on admission; however, the blood culture performed on HD 4 was negative for C. jejuni. Antibiotic susceptibility tests for the identified C. jejuni were not performed. The patient was discharged from the hospital after intravenous antibiotic therapy for 10 days, and oral roxithromycin was administered for a total of 15 days. Serum immunoglobulin levels on discharge were as follows: IgG, 352 mg/dL; IgA, <1.0 mg/dL; IgM, <1.0 mg/dL; and IgE, <1.0 mg/dL. Lymphocyte subset tests on discharge showed the following results: CD3+ cells, 97.2%; CD4+ cells, 59.6%; CD8+ cells, 34.3%; CD19+ cells, <0.1%; and CD3–56+ cells, 2.4%. The patient developed diarrhea 2 weeks after discharge and this persisted. Two months after discharge, he was readmitted with continued weight loss and poor oral intake due to oral mucositis. Blood culture on admission grew C. jejuni, and he was discharged from the hospital after intravenous amoxicillin/clavulanate, amikacin, and acyclovir therapy for 8 days. One month later, he was readmitted due to persistent diarrhea and left shin cellulitis that had recurred. Blood culture on admission again grew C. jejuni, and he received oral roxithromycin for 10 days. Although C. jejuni was reported as a cause of cellulitis in patients with hypogammaglobulinemia, we could not ignore the fact that Gram-positive cocci are the most common cause of cellulitis. Therefore, the patient also received intravenous cefazolin and arbekacin therapy for 6 days. After that time, diarrhea waxed and waned. Two months later, the left shin cellulitis recurred. Stool culture grew C. jejuni, although blood was sterile. Intravenous cefazolin and arbekacin was given for 14 days along with oral clarithromycin for 10 days. He was readmitted with fever and left shin cellulitis 1 month later. Intravenous cefazolin and amikacin, and oral clarithromycin therapy was begun as recurrent C. jejuni infection was suspected. Blood cultures were negative on admission; however, a repeat blood culture on HD 5 was positive for C. jejuni. On HD 8, the antibiotic susceptibility test revealed resistance against ciprofloxacin and erythromycin and susceptibility to tetracycline. Intravenous cefazolin and oral clarithromycin were switched to intravenous meropenem and oral doxycycline. The patient's fever disappeared on HD 9, and a repeat blood culture on HD 10 was negative. Stool culture revealed no pathogens, and the diarrhea resolved on HD 27. After the administration of meropenem and doxycycline for 3 weeks and amikacin for 4 weeks, the patient was discharged from the hospital. Oral doxycycline therapy was continued for an additional 3 months after discharge. Ten months after the completion of the doxycycline therapy, the patient again experienced fever and diarrhea. The stool culture was positive for C. jejuni; but blood cultures were negative. The patient received doxycycline, with resolution of his symptoms before the report of the antibiotic susceptibility test; therefore, doxycycline was continued for 10 days, even though the report showed resistance to tetracycline. Figure 1 shows the clinical course of recurrent C. jejuni infection in our patient.
Figure 1.
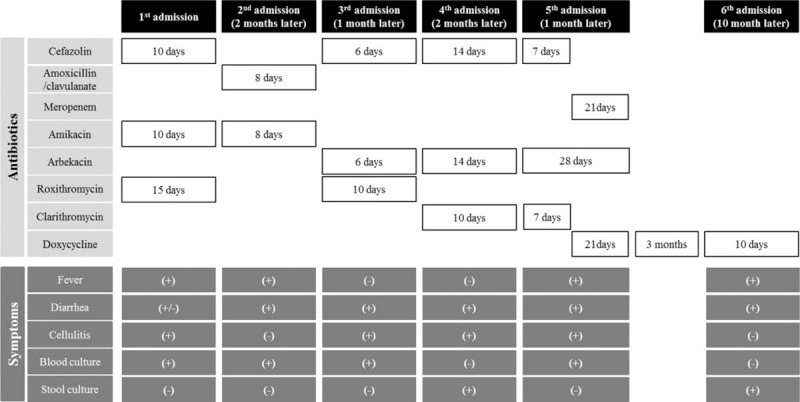
The clinical course of recurrent Campylobacter jejuni infection.
3. Discussion
There are numerous reports about Campylobacter bacteremia in patients with chronic illnesses, such as chronic hepatitis, liver cirrhosis, diabetes, chronic lung diseases and cardiovascular disorders, HIV-infected patients, and immunocompromised patients.[7–12] In the past, it was believed that C. fetus was the cause of most systemic campylobacteriosis. Recent studies show, however, that both bacteremia and enterocolitis are caused mainly by C. jejuni.[8–13] Bacteremia due to Campylobacter spp. is very rarely, comprising only 0.2% to 0.4% of all Campylobacter infections.[10,12] Also, recurrent bacteremia occurs in 2% to 5% of all bacteremia cases.[11–13]
Most cases of recurrent Campylobacter bacteremia were reported in patients with hypogammaglobulinemia.[4–6,13] In accordance with these findings, humoral immunity seems to play a role in immunity against and eradication of Campylobacter spp.[5] Secretory IgA in the intestinal mucosa may act as an important local immune defense; however, there was no significant increase in Campylobacter infections in patients with selective IgA deficiency.[2] Therefore, other immune mechanisms against Campylobacter spp. should be considered. Serum IgM is thought to be important because it promotes complement-mediated phagocytosis by increasing opsonization of pathogens.[2] Consequently, lack of IgA in the intestinal mucosa and IgM in the serum makes hypogammaglobulinemia patients more susceptible to Campylobacter infections, and prevents the eradication of colonized Campylobacter spp.[2] Although hypogammaglobulinemia patients receive IVIG regularly, IVIG consist mainly of IgG. Our patient's serum IgM and IgA levels could not be detected. It appears that the patient could not eradicate C. jejuni after the primary infection, and the colonized C. jejuni caused prolonged diarrhea and recurrent bacteremia.
Previously, C. jejuni was reported to be susceptible to macrolides and fluoroquinolones, and azithromycin was the recommended drug of choice.[1] However, Campylobacter strains isolated from patients with bacteremia showed resistance rates of 26% to 70% for fluoroquinolones and 6% to 79% for erythromycin. Resistance rates were 1% to 8% for amoxicillin/clavulanate, 0% to 6% for gentamicin, and 0% for carbapenems.[9–11,13,14] Therefore, amoxicillin/clavulanate, carbapenems, or aminoglycosides are recommended for patients with Campylobacter bacteremia.[9–11,13,14] Previously, recurrence of C. jejuni bacteremia was reported in spite of amoxicillin/clavulanate, erythromycin, or gentamicin therapy.[5,15,16] However, bacteremia did not recur with prolonged antibiotic therapy (e.g., imipenem for 2–6 weeks, ciprofloxacin for 6 weeks, or doxycycline for 4 months).[5,15,16] One patient showed persistent positive stool cultures for C. jejuni following imipenem therapy that was eradicated by ciprofloxacin and maternal plasma infusion therapy.[17] Other examples include erythromycin given for 6 weeks to eradicate Campylobacters,[5] clarithromycin given for 3 weeks in a patient with C. jejuni bacteremia,[18] and oral kanamycin in patients with recurrent C. coli bacteremia.[6,19] Our patient received aminoglycosides at the time of each admission. First-generation cephalosporins, which almost all C. jejuni strains are resistant to,[11,20] were concomitantly administered, and the duration of antibiotic therapy in each bacteremia episode was less than 2 weeks. Therefore, C. jejuni could not be eradicated from our patient. Antibiotic susceptibility tests for Campylobacter spp. are not routinely performed in our hospital, and therefore, the susceptibility test was performed with the authors’ requirement, at the fifth recurrence of bacteremia. The strain isolated from our patient was susceptible to tetracycline, and the patient did not experience recurrent fever and diarrhea after 3 months of doxycycline therapy. However, his symptoms recurred 10 months after the completion of doxycycline therapy, and the isolated strain became resistant to tetracycline. In the future, if the patient experiences repeated episode of C. jejuni infection, oral aminoglycosides should be considered to eradicate intestinal colonization.
In conclusion, recurrent Campylobacter infections can occur in immunocompromised patients, especially in patients with a humoral immune deficiency. Further studies to establish appropriate antibiotic therapy for eradicating colonized Campylobacter spp. and preventing recurrent infections should be conducted.
Footnotes
Abbreviations: HD = hospital day, HIV = human immunodeficiency virus, IVIG = intravenous immunoglobulin, WBC = white blood cell.
The authors have no conflicts of interest to disclose.
References
- [1].Zakhour R, Heresi GP, Murphy JR. Cherry JD, Demmler-Harrison GJ, Kaplan SL, Hotez P, Steinbach WJ. Campylobacter jejuni. Fiegin and Cherry's Pediatric Infectious Diseases. Philadelphia, PA: Saunders: 2014;1644–57. [Google Scholar]
- [2].Janssen R, Krogfelt KA, Cawthraw SA, et al. Host-pathogen interactions in Campylobacter infections: the host perspective. Clin Microbiol Rev 2008;21:505–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Van der Hilst JC, Smits BW, van der Meer JW. Hypogammaglobulinaemia: cumulative experience in 49 patients in a tertiary care institution. Neth J Med 2002;60:140–7. [PubMed] [Google Scholar]
- [4].Jirapongsananuruk O, Wanotayan K, Phongsamart W, et al. Recurrent Campylobacter lari bacteremia in X-linked agammaglobulinemia: a case report and review. Asian Pac J Allergy Immunol 2006;24:171–4. [PubMed] [Google Scholar]
- [5].Kerstens PJ, Endtz HP, Meis JF, et al. Erysipelas-like skin lesions associated with Campylobacter jejuni septicemia in patients with hypogammaglobulinemia. Eur J Clin Microbiol Infect Dis 1992;11:842–7. [DOI] [PubMed] [Google Scholar]
- [6].Okada H, Kitazawa T, Harada S, et al. Combined treatment with oral kanamycin and parenteral antibiotics for a case of persistent bacteremia and intestinal carriage with Campylobacter coli. Intern Med 2008;47:1363–6. [DOI] [PubMed] [Google Scholar]
- [7].Mori T, Hasegawa N, Sugita K, et al. Clinical features of bacteremia due to Campylobacter jejuni. Intern Med 2014;53:1941–4. [DOI] [PubMed] [Google Scholar]
- [8].Feodoroff B, Lauhio A, Ellstrom P, et al. A nationwide study of Campylobacter jejuni and Campylobacter coli bacteremia in Finland over a 10-year period, 1998–2007, with special reference to clinical characteristics and antimicrobial susceptibility. Clin Infect Dis 2011;53:e99–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Liao CH, Chuang CY, Huang YT, et al. Bacteremia caused by antimicrobial resistant Campylobacter species at a medical center in Taiwan, 1998–2008. J Infect 2012;65:392–9. [DOI] [PubMed] [Google Scholar]
- [10].Nielsen H, Hansen KK, Gradel KO, et al. Bacteraemia as a result of Campylobacter species: a population-based study of epidemiology and clinical risk factors. Clin Microbiol Infect 2010;16:57–61. [DOI] [PubMed] [Google Scholar]
- [11].Pigrau C, Bartolome R, Almirante B, et al. Bacteremia due to Campylobacter species: clinical findings and antimicrobial susceptibility patterns. Clin Infect Dis 1997;25:1414–20. [DOI] [PubMed] [Google Scholar]
- [12].Skirrow MB, Jones DM, Sutcliffe E, et al. Campylobacter bacteraemia in England and Wales, 1981–91. Epidemiol Infect 1993;110:567–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Fernandez-Cruz A, Munoz P, Mohedano R, et al. Campylobacter bacteremia: clinical characteristics, incidence, and outcome over 23 years. Medicine (Baltimore) 2010;89:319–30. [DOI] [PubMed] [Google Scholar]
- [14].Pacanowski J, Lalande V, Lacombe K, et al. Campylobacter bacteremia: clinical features and factors associated with fatal outcome. Clin Infect Dis 2008;47:790–6. [DOI] [PubMed] [Google Scholar]
- [15].Hopkins S, Abuzakouk M, Brannigan E, et al. Campylobacter jejuni cellulitis in a patient with pan-hypogammaglobulinaemia. BMJ Case Rep 2011;Feb 2. DOI: 10.1136/bcr.02.2010.2741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Johnson RJ, Nolan C, Wang SP, et al. Persistent Campylobacter jejuni infection in an immunocompromised patient. Ann Intern Med 1984;100:832–4. [DOI] [PubMed] [Google Scholar]
- [17].Autenrieth IB, Schuster V, Ewald J, et al. An unusual case of refractory Campylobacter jejuni infection in a patient with X-linked agammaglobulinemia: successful combined therapy with maternal plasma and ciprofloxacin. Clin Infect Dis 1996;23:526–31. [DOI] [PubMed] [Google Scholar]
- [18].Ariganello P, Angelino G, Scarselli A, et al. Relapsing Campylobacter jejuni systemic infections in a child with X-linked agammaglobulinemia. Case Rep Pediatr 2013;2013:735108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Tokuda K, Nishi J, Miyanohara H, et al. Relapsing cellulitis associated with Campylobacter coli bacteremia in an agammaglobulinemic patient. Pediatr Infect Dis J 2004;23:577–9. [DOI] [PubMed] [Google Scholar]
- [20].Sjogren E, Kaijser B, Werner M. Antimicrobial susceptibilities of Campylobacter jejuni and Campylobacter coli isolated in Sweden: a 10-year follow-up report. Antimicrob Agents Chemother 1992;36:2847–9. [DOI] [PMC free article] [PubMed] [Google Scholar]


