Abstract
Rationale:
Plasma cell neoplasms are categorized by neoplastic proliferation of a single clone of plasma cells which produce a monoclonal immunoglobulin. Plasma cell neoplasms can present as a solitary plasmacytoma or as multiple myeloma. Both of them can progress to multiple myeloma. Once a diagnosis of plasmacytoma has been made, thorough examinations should be carried out for identifying the disease entity.
Patient concerns and diagnoses:
Herein, we describe an extraordinary rare case of multiple myeloma with initial presentation of a left sphenoid neoplasm resulting in left-sided headache and rapid deterioration of visual acuity. Histo-pathologic analysis revealed a plasma cell neoplasm with positive immunostaining for cluster of differentiation (CD)138, CD79a, and kappa light chain of immunoglobulin. A bone marrow aspiration was then performed, and the diagnosis of multiple myeloma was then confirmed.
Interventions and outcomes:
After investigative workup, our patient received chemotherapy, localized radiotherapy, and autologous stem cell transplantation. Her visual acuity recovered to the baseline and she sustained a partial response without subjective discomfort.
Lessons:
Extramedullary plasmacytoma is an interesting but infrequent presentation of multiple myeloma. Moreover, involvement of the sphenoid sinus in multiple myeloma resulting in extrinsic optic nerve compression is extremely rare. Clinicians should consider plasmacytoma as a diagnostic possibility when presented with cases of solitary sphenoid neoplasm and rapid progression of clinical course.
Keywords: multiple myeloma, plasmacytoma, sphenoid sinus, vision loss
1. Introduction
Plasma cell neoplasms are characterized by neoplastic proliferation of a single clone of plasma cells which produce a monoclonal immunoglobulin.[1] The clinical presentations of plasma cell neoplasm are diverse. They can present as a single lesion (solitary plasmacytoma) with single bone or extramedullary organ being involved, or as multiple lesions (multiple myeloma) with many organs being affected.[2] Both of solitary plasmacytoma of the bone and extramedullary plasmacytoma can progress to multiple myeloma.[1] Plasmacytoma in the head and neck region is rare, and it mainly affects mucosal and submucosal tissue of the nasal cavity, nasopharynx, oropharynx, and larynx.[3] Once a diagnosis of plasmacytoma has been made, a bone marrow biopsy, whole body skeletal survey, and thorough laboratory tests are essential for identifying the disease entity. If the bone marrow biopsy shows a clonal bone marrow plasma cell percentage ≥60%, or >1 focal lesions on magnetic resonance imaging (MRI) studies, or evidence of end organ damage that can be attributed to the underlying plasma cell proliferative disorder, a diagnosis of multiple myeloma can be made.[4]
2. Case report
A 59-year-old woman presented to our emergent department with sudden vision loss in the left eye. She had a 1-month history of worsening headache, ptosis, and diplopia on the left side. She had no history of nasal obstruction, purulent rhinorrhea, epistaxis, or facial pressure. She had a history of hypertension, but she was otherwise healthy.
Endoscopic examination of the nasal cavity revealed a vascular soft-tissue mass that bled easily on touching in the left sphenoethmoidal recess. MRI confirmed the presence of a mass lesion in the body of the sphenoid and clivus that was isointense on T2-weighted images (Fig. 1) and hypointense on T1-weighted images with moderate gadolinium enhancement (Fig. 2). Laboratory tests yielded insignificant findings, except moderate anemia (hemoglobin 9.3 g/dL). There was no anterior hypophyseal hormonal imbalance.
Figure 1.
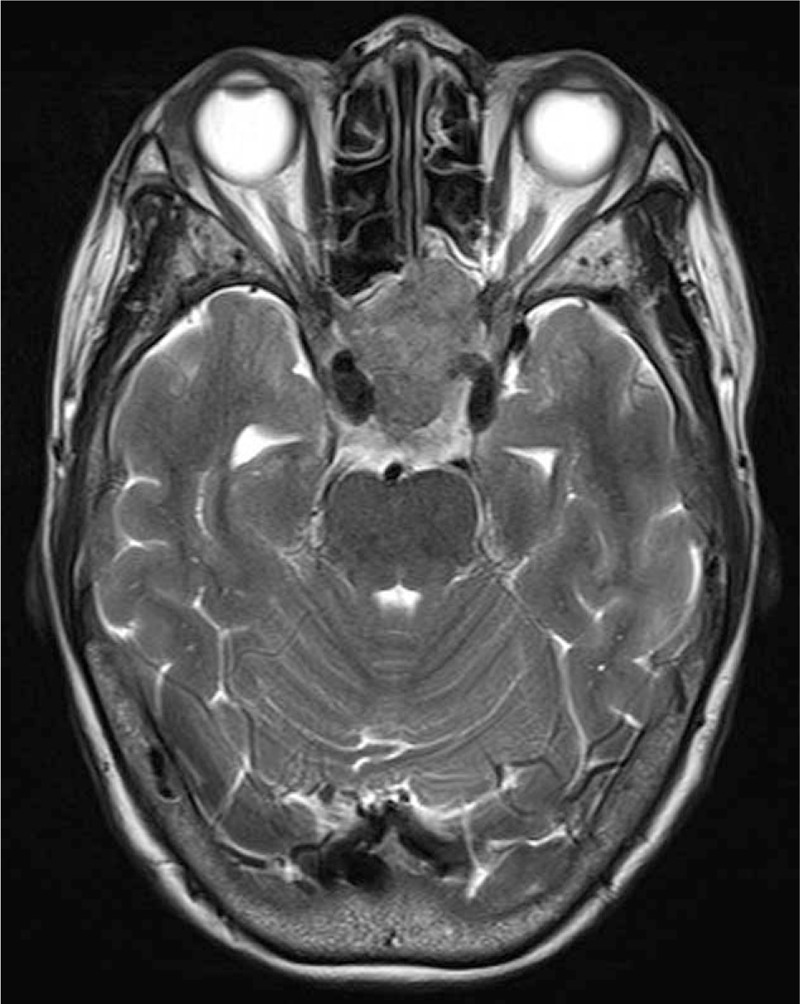
A mass lesion in the body of the sphenoid that was isointense on T2-weighted image result in extrinsic optic nerve compression on the left side.
Figure 2.
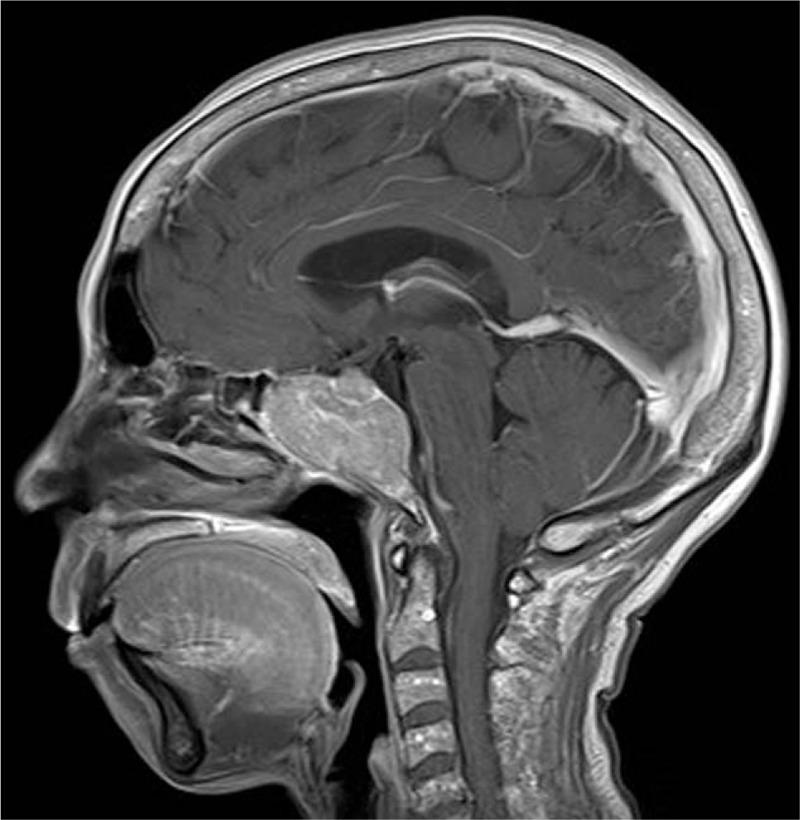
The sphenoid mass lesion was hypodense on T1-weighted images with moderate gadolinium enhancement.
Biopsy via a transnasal endoscopic approach was performed under general anesthesia. Considerable bleeding was encountered during the procedure, which required the placement of dissolvable nasal packing. Histo-pathologic analysis revealed diffuse infiltrative plasma cells with mildly pleomorphic round nuclei with fine chromatin and high mitoses favoring a plasma cell neoplasm (Fig. 3). The diagnosis of extramedullary plasmacytoma was determined by positive immunostaining for cluster of differentiation (CD)138, a plasma cell marker (Fig. 4); CD79a, a B-cell marker; and kappa light chain of immunoglobulin. A bone marrow aspiration was then performed and it identified diffuse infiltrate of plasma cells with prominent nucleoli positive for CD138 staining on approximately 80% of all nucleated cells. There was also kappa light chain restriction among the plasma cells. The diagnosis of multiple myeloma was then confirmed. After investigative workup, our patient received induction chemotherapy with 4 cycles of velcade-thalidomide-dexamethasone followed by high-dose melphalan (200 mg/m2) and autologous stem cell transplantation. External beam radiation therapy 4920 centigray administered in 26 fractions was also prescribed for the sphenoid plasmacytoma. Her visual acuity recovered soon. To date, 18 months after the diagnosis, she sustained a partial response with disappearance of the sphenoid plasmacytomas.
Figure 3.
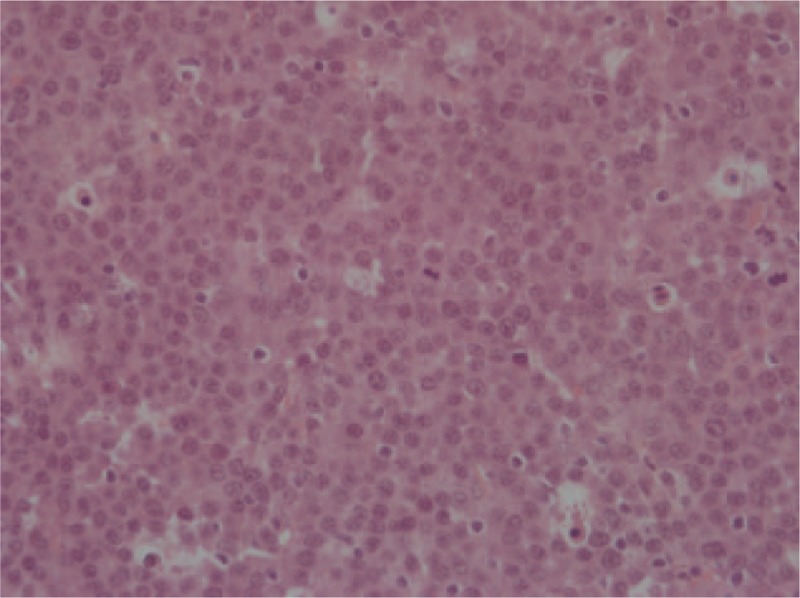
Hematoxylin and eosin stain. Histo-pathologic analysis revealed diffuse infiltrative plasma cells with mildly pleomorphic round nuclei with fine chromatin and high mitoses favoring a plasma cell neoplasm. Magnification 400×.
Figure 4.

Cluster of differentiation (CD)138 stain. The tumor cells showed positive immunostaining for CD138, a plasma cell marker. Magnification 400×.
3. Discussion
Herein, we describe an extraordinary rare case of multiple myeloma with initial presentation of a left sphenoidal mass resulting in left-sided headache and rapid deterioration of visual acuity. Extramedullary plasmacytoma is an interesting but infrequent presentation of multiple myeloma at diagnosis. In a series of 822 patients with plasma cell neoplasm, only 3% had extramedullary plasmacytomas as their initial presentation.[5] Moreover, involvement of the sphenoid sinus in multiple myeloma resulting in extrinsic optic nerve compression is extremely rare.
The sphenoid sinus is surrounded by critical structures such as the optic nerves, abducent nerves, ophthalmic and maxillary division of the trigeminal nerves, and carotid arteries. The anatomic localization accounts in large part for the difficulty of diagnosing a pathologic process when it is confined to the sphenoid and for the wide diversity of presenting findings when the mass extends out of the sphenoid or arises in adjacent structures.[6] Unlike other paranasal sinus lesions that usually present with nasal obstruction, epistaxis, and nasal discharge, headache and II, III, IV, VI cranial nerve palsies are the most frequent symptoms of isolated sphenoid sinus diseases. However, these symptoms are usually vague and nonspecific, until the tumor grows and expands to the sinus wall. Thus, by the time of diagnosis, the disease advances in most patients.
The sphenoid sinus can be affected by numerous pathologic entities including inflammatory lesions (sphenoiditis, fungal ball, mucocele, and sphenochoanal polyps), skull base defects with cerebrospinal fluid leakage or meningo (encephalo)cele, neoplasms, and vascular lesions. Because of the anatomic complexity, thorough image studies such as computed tomography and/or MRI are recommended before tumor biopsy for histologic examination and definite diagnosis, especially in cases of suspicious meningo (encephalo)cele or vascular lesions. During transnasal endoscopic surgery, even when only performing a simple biopsy procedure, we should consider the possibility of bony dehiscence caused by tumor expansion and take great care to prevent injury to the vital structures, such as the carotid arteries and optic nerves surrounding the sphenoid sinus.
The current treatment of multiple myeloma varies considerably across institutions and across countries. Multimodality treatment, encompassing chemotherapy, biological therapy, radiation, and stem cell transplantation, has been recognized as important approaches for improving overall survival. The overall prognosis of multiple myeloma depends on a variety of host- and disease-related factors, included the patient's performance status, the patient's renal function, the tumor burden, and the tumor biology.[7] Based on data from surveillance, epidemiology, and end results (2006–2012), the 5-year survival rate of multiple myeloma is around 48.5%.[8]
4. Conclusion
In summary, extramedullary plasmacytoma is an interesting but infrequent presentation of multiple myeloma. Moreover, involvement of the sphenoid sinus in multiple myeloma resulting in extrinsic optic nerve compression is extremely rare. Clinicians should consider plasmacytoma as a diagnostic possibility when presented with cases of solitary sphenoid neoplasm and rapid progression of clinical course.
Footnotes
Abbreviations: CD = cluster of differentiation, MRI = magnetic resonance imaging.
Ethics Approval: This study was approved by the Institutional Review Board of Chang Gung Medical Foundation (IRB number: 201601067B0).
The authors have no funding and conflicts of interest to disclose.
References
- [1].Dores GM, Landgren O, McGlynn KA, et al. Plasmacytoma of bone, extramedullary plasmacytoma, and multiple myeloma: incidence and survival in the United States, 1992–2004. Br J Haematol 2009;144:86–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Ravikishore H, Ashwini S Doddamani, Narendranath A, et al. Extramedullary plasmacytoma of the nasal cavity: a rare case report. MedPulse – Int Med J 2015;2:456–8. [Google Scholar]
- [3].Castro EB, Lewis JS, Strong EW. Plasmacytoma of paranasal sinuses and nasal cavity. Arch Otolaryngol 1973;97:326–9. [DOI] [PubMed] [Google Scholar]
- [4].Rajkumar SV, Dimopoulos MA, Palumbo A, et al. International Myeloma Working Group updated criteria for the diagnosis of multiple myeloma. Lancet Oncol 2014;15:e538–48. [DOI] [PubMed] [Google Scholar]
- [5].Knowling MA, Harwood AR, Bergsagel DE. Comparison of extramedullary plasmacytomas with solitary and multiple plasma cell tumors of bone. J Clin Oncol 1983;1:255–62. [DOI] [PubMed] [Google Scholar]
- [6].Bachmeyer C1, Levy V, Carteret M, et al. Sphenoid sinus localization of multiple myeloma revealing evolution from benign gammopathy. Head Neck 1997;19:347–50. [DOI] [PubMed] [Google Scholar]
- [7].Rajkumar SV, Gahrton G, Bergsagel PL. Approach to the treatment of multiple myeloma: a clash of philosophies. Blood 2011;118:3205–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].National Cancer Institute. Surveillance, Epidemiology, and End Results Program. Stat Fact Sheets: Myeloma. http://seer.cancer.gov/statfacts/html/mulmy.html [Accessed October 30, 2016]. [Google Scholar]


