Abstract
Background:
Red blood cell (RBC) transfusions are commonly used in surgical patients, but accompanied by many risks such as metabolic derangement, and allergic and febrile reactions. Indications for transfusion in patients after hip or knee surgery have not been definitively evaluated and remain controversial. We performed a meta-analysis to compare the benefits and harms of restrictive versus liberal transfusion strategies in patients after hip or knee surgery.
Methods:
The PubMed, EMBASE, and Cochrane Library databases were searched for relevant studies through September 2015. The main clinical outcomes reported in randomized controlled trials (RCTs) included 30-day mortality, infection rate, cardiogenic complications, and length of hospital stay. The meta-analysis program of the Cochrane Collaboration (RevMan version 5.3.0) was used for data analysis. Statistical heterogeneity was assessed by both Cochran chi-squared test (Q test) and I2 test. Begg and Egger test were used to assess potential publication bias.
Results:
We identified 10 eligible RCTs, involving 3788 patients in total. In patients undergoing hip or knee surgery, we found no differences in mortality, or the incidence rates of pneumonia, wound infection, myocardial infarction, or congestive heart failure, between restrictive and liberal thresholds for RBC transfusion (P > .05).
Conclusion:
Restrictive transfusion has no advantage over the liberal strategy. However, considerably less patients received blood transfusion via the restrictive strategy than with the liberal counterpart. Due to variations in the included studies, additional larger scale and well-designed studies are required to validate these conclusions.
Keywords: blood transfusion, hip, knee, liberal transfusion, randomized, restrictive transfusion
1. Introduction
Postoperative bleeding is one of the major complications in joint arthroplasty, and can significantly influence morbidity and mortality. there Considerable blood loss can occur during hip surgery, and up to half of hip surgery patients receive an average of 2 units of blood postoperatively.[1] Several studies have suggested that the risk of postoperative morbidity is higher in patients with cardiovascular disease or anemia after surgery.[2,3] For many years, the widely used red blood cell (RBC) transfusion threshold was hemoglobin levels of 10 g/dL, which is largely credited to Adams and Lundy.[4] However, allogeneic blood transfusion harbors the well-recognized risk of complications, including allergic reactions, bacterial or viral infections, and metabolic imbalance.[5]
To prevent these complications of blood transfusion, many recent studies have proposed that lower, more restrictive thresholds may be acceptable in certain groups of patients. Vuille-Lessard et al[6] suggested that anemia resulting from a restrictive transfusion strategy does not affect the functional outcome or quality of life in patients after hip or knee surgery. Clinically, there has been a trend to lower the blood transfusion threshold from 10 to 8 g/dL, or to administer blood transfusion only when the patient develops anemia symptoms. At present, there are 2 major types of RBC transfusion, including restrictive and liberal transfusion strategies. The liberal transfusion threshold is hemoglobin amounts of 10 g/dL. Meanwhile, the restrictive transfusion threshold is a lower hemoglobin concentration of 8 g/dL or even until the patient develops anemia symptoms.[7–9] Many recent meta-analyses of randomized controlled trials (RCTs) showed that the restrictive transfusion approach is as safe as the liberal transfusion strategy.[7–10] Nevertheless, contemporary knowledge from published reviews should be considered cautiously because the majority of published reviews combine data from studies that were conducted in different clinical disorders.
The threshold for allogeneic transfusion remains controversial, and no clear consensus to guide clinical practice has yet appeared. Multiple studies have been criticized for poor design, low statistical power, inconclusive results, and short duration of follow-up. Given newly emerging evidences, we conducted a meta-analysis of RCTs to examine whether the restrictive transfusion strategy is more effective and safer than the liberal counterpart in patients after hip or knee surgery.
2. Methods
This meta-analysis was carried out in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses reporting guidelines for the meta-analysis of intervention trials.[11] Ethics committee approval for this study was unnecessary as a review of existing literature and not involving handling of individual patient data.
2.1. Search strategy
This meta-analysis was planned, conducted, and reported based on the Cochrane methodology.[12] A PubMed database search through September 2015 was performed to identify relevant studies. The following search terms were used for the initial literature search: “blood transfusion,” “hip,” “knee,” “lower limb,” and “randomized.” Selection of relevant studies was then independently performed by 2 authors (GFQ and MTL), and any discrepancies were resolved through discussion. Additionally, the results were cross-checked with other databases, namely EMBASE, Medline, and Google Scholar, for trials investigating blood transfusion and lower limb surgery. We also reviewed the reference lists of the retrieved articles and recent reviews. However, we did not contact the authors of the original studies for additional information.
2.2. Inclusion criteria and study selection
The following inclusion criteria were considered: study design as RCT; enrolled patients undergoing hip or knee surgery; selected patients above 18 years of age; and RBC transfusion with liberal transfusion strategy in 1 group and restrictive transfusion approach in the other. The threshold for the liberal transfusion strategy was hemoglobin levels of 10 g/dL and above; in contrast, the threshold for the restrictive transfusion strategy was lower than 10 g/dL.[7–9] Conference abstracts were also included if they provided sufficient data. Animal studies, narrative reviews, systematic reviews, and nonrandomized controlled studies were excluded from the current meta-analysis.
2.3. Data extraction and quality assessment
The following data were extracted from the included studies: first author's last name, publication year, study population, age, male to female ratio, number of cases and participants, transfusion thresholds, 30-day mortality, incidence of infections, incidence of myocardial infarction, incidence of congestive heart failure, length of hospital stay, and number of patients who underwent blood transfusion. The methodological quality of each component study was assessed using the Jadad composite scale.[13] The quality scale ranged from 0 (very poor) to 5 (rigorous) points. A score above 2 was considered to reflect a high quality study. Data extraction and quality assessment were independently performed by 2 authors (GFQ and MTL). In case of disagreement, all the authors discussed the matter until a consensus was reached.
2.4. Statistical analyses
The meta-analysis program of the Cochrane Collaboration (RevMan version 5.3.0) was used for data analysis. Statistical heterogeneity was assessed by both Cochran chi-squared test (Q test) and I2 test. P < .1 and I2 > 50% were considered suggestive of statistical heterogeneity, and a random effects model was used to estimate binary and continuous variables. Otherwise, a fixed effects model was used, and the inverse variance statistical method was used for binary and continuous variables. Binary variables were presented as risk ratio (RR) and 95% confidence interval (95%CI). Continuous variables were expressed as mean and standard deviation (SD), and assessed using weighted mean differences and respective 95%CIs. Begg test[14] and Egger test[15] were used to assess potential publication bias.
3. Results
The electronic search originally identified 1018 studies as potentially relevant. However, 970 were excluded after scrutiny of their titles or abstracts, for not meeting the inclusion criteria, leaving 48 potentially relevant studies. The full publications were then obtained and evaluated. Of these 48 relevant studies, 38 were excluded for nonrandomization (n = 13), nonadequate data (n = 11), ineligible comparators (n = 7), untouched transfusion strategy (n = 6), and no hip or knee surgery (n = 1). There were 10 eligible RCTs in the final analysis (Fig. 1). The majority of the included trials reported an appropriate method of randomization. All 10 trials documented some concealment of allocation. In 9 of the 10 studies, the double-blinding technique was not feasible due to the nature of the interventions. However, 7 trials attempted to blind data collection. The basic demographic characteristics of patients assessed by the included studies are listed in Table 1.
Figure 1.
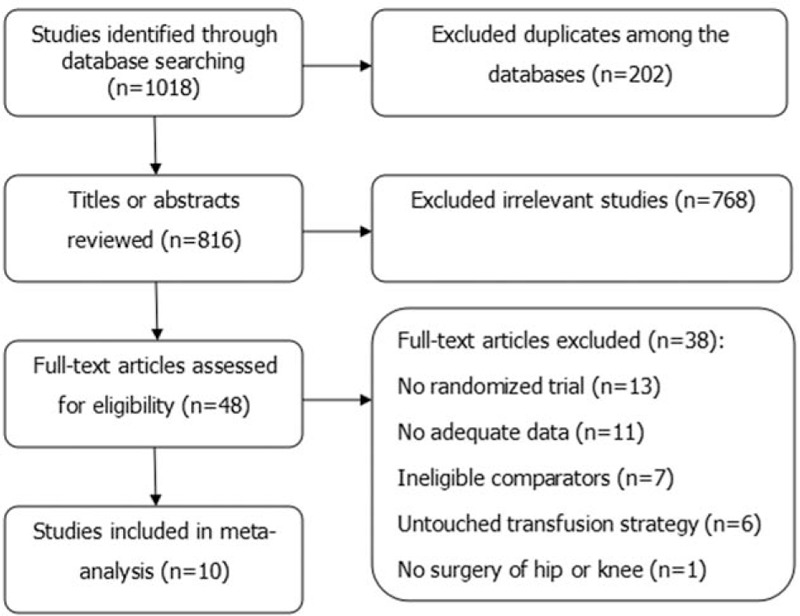
Flowchart of the study selection.
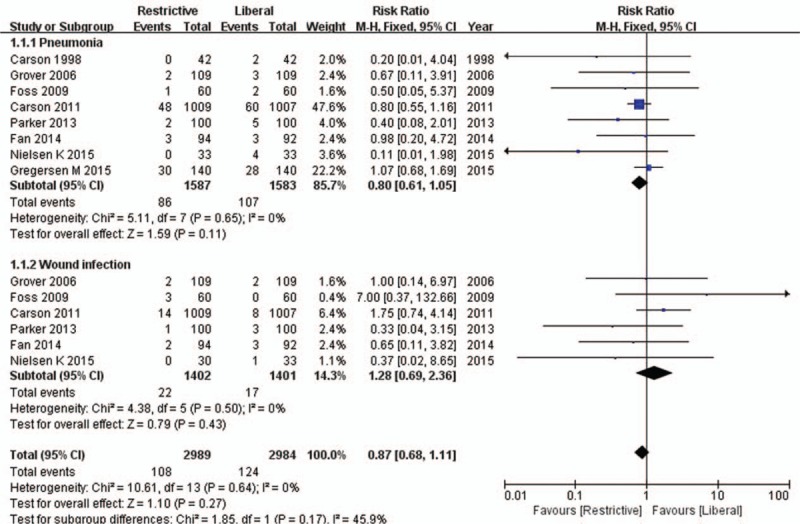
Table 1.
Demographic characteristics of component studies.
3.1. Study quality
The quality score of each of the 10 included studies consisted of the average value of individual scores given by 2 authors. Eight studies[16,18–21,23–25] were scored with higher than 2 points, and considered to be of high quality. In contrast, the remaining 2 studies[17,22] had 2 points, and therefore considered to be of low quality (Table 1).
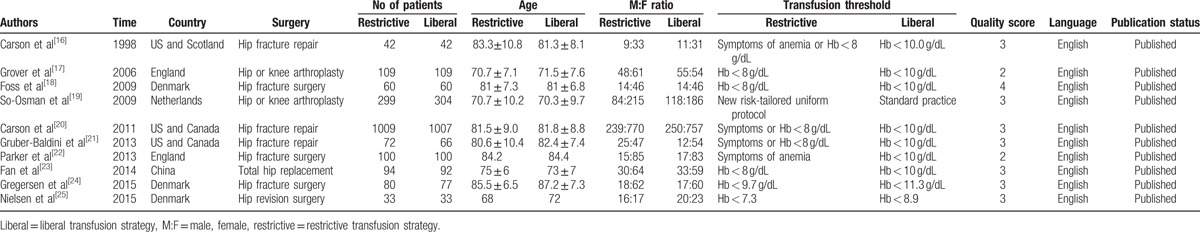
3.2. 30-day mortality
The 30-day mortality outcome was described in 7 of the 10 articles[16–20,22,24] which included 1763 and 1762 patients in restrictive and liberal transfusion threshold groups, respectively. There was no difference in mortality at 30 days postsurgery between the 2 groups (RR = 1.06, 95%CI 0.78–1.45; P = .71), and no statistically significant heterogeneity (χ2 = 7.28; P = .30; I2 = 18%; Fig. 2). Publication bias was not evident in any of the included studies according to Begg test (P = 1.00) or Egger test (P = .52; 95%CI −1.24–2.14).
Figure 2.
Forest plot of 30-day mortality. 95% CI = 95% confidence interval, df = degrees of freedom, Fixed = fixed effects model, IV = inverse variance, SD = standard deviation.
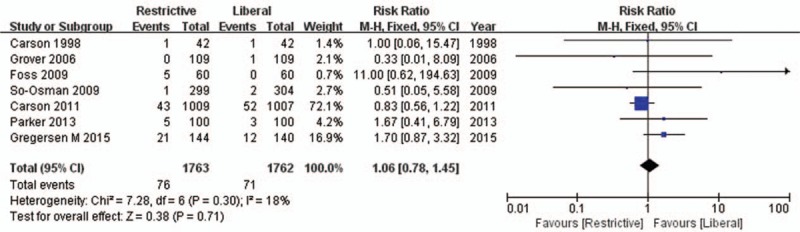
3.3. Infection rates
Relevant data about pneumonia and wound infection incidence rates were obtained from 8 of the included studies.[16–19,21,22–25] A fixed effects model was used for data analysis. The summarized estimates of effect size indicated that the incidence of pneumonia did not differ significantly between the restrictive and liberal transfusion threshold groups (RR = 0.80, 95%CI 0.61–1.05; P = .11). Similarly, there was little difference in wound infection incidence between the liberal and restrictive transfusion threshold groups (RR = 1.28, 95%CI 0.69–2.36; P = .43). The pooled estimates of effect size for pneumonia and wound infection incidence rates showed that these infections did not differ significantly in incidence between the 2 groups (RR = 0.87, 95%CI 0.68–1.11; P = .27; Fig. 3). No publication bias was found in any of the included studies according to Begg test (P = .23) or Egger test (P = .27; 95%CI −1.19–0.37).
Figure 3.
Forest plot of infections. 95% CI = 95% confidence interval, df = degrees of freedom, Fixed = fixed effects model, IV = inverse variance, SD = standard deviation.
3.4. Transfusion requirements
Seven of the included component studies provided relevant data on transfusion rates,[16–20,24,25] with a total of 1696 and 1695 patients in the restrictive and liberal transfusion threshold groups, respectively. A random effects model was used for data analysis. The pooled estimates of effect size for transfusion rate showed that the restrictive transfusion threshold group had a significantly lower transfusion rate than the liberal counterpart (RR = 0.61, 95%CI 0.47–0.80; P = .0004), with a significant level of heterogeneity between the included trials (χ2 = 38.22; df = 6; P < .00001; I2 = 84%; Fig. 4). Publication bias was found according to Begg test (P = .03), but this finding was not supported by Egger test (P = .06; 95%CI −0.08–4.58).
Figure 4.
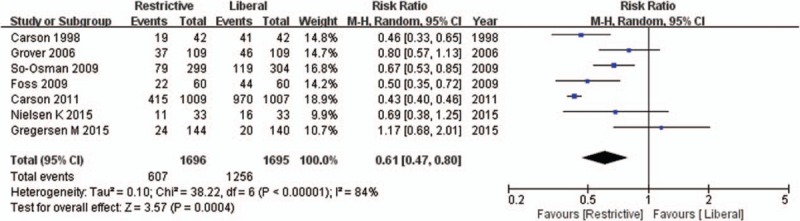
Forest plot of transfusion requirements. 95% CI = 95% confidence interval, df = degrees of freedom, Random = random effects model, IV = inverse variance, SD = standard deviation.
3.5. Myocardial infarction rate
The incidence of myocardial infarction was described in 5 of the included reports,[15–18,20,23] which assessed a total of 1313 and 1308 patients in the restrictive and liberal transfusion threshold groups, respectively. The summarized estimates of effect size indicated that myocardial infarction incidence did not differ significantly between the restrictive and liberal transfusion threshold groups (RR = 1.55, 95%CI 0.96–2.50; P = .07), and no statistical heterogeneity was found (χ2 = 2.20; P = .70; I2 = 0%; Fig. 5). Publication bias was not found according to Begg test (P = .08) or Egger test (P = .51; 95%CI −1.93–1.19).
Figure 5.
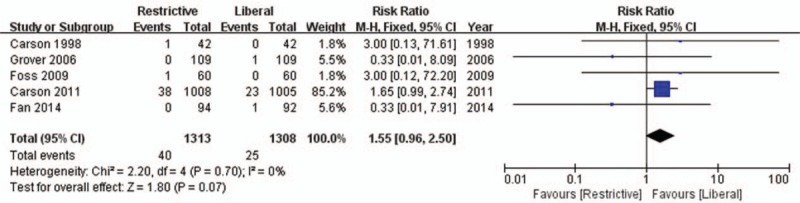
Forest plot of myocardial infarction. 95% CI = 95% confidence interval, df = degrees of freedom, Fixed = fixed effects model, IV = inverse variance, SD = standard deviation.
3.6. Congestive heart failure rate
Five of the included papers[18,20–23] described the incidence of congestive heart failure, with a total of 1333 and 1323 patients in the restrictive and liberal transfusion threshold group. There was no significant difference in the rate of congestive heart failure between the liberal and restrictive transfusion threshold groups (RR = 1.32, 95%CI 0.83–2.11; P = .25), and no statistically significant heterogeneity was found (χ2 = 1.52; P = .82; I2 = 0%; Fig. 6). Publication bias was not evident according to Begg test (P = .81) or Egger test (P = .89; 95%CI −1.40–1.56).
Figure 6.
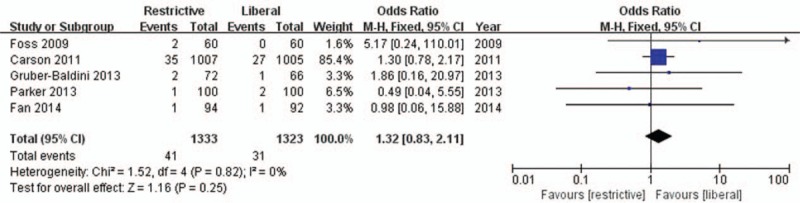
Forest plot of congestive heart failure. 95% CI = 95% confidence interval, df = degrees of freedom, Fixed = fixed effects model, IV = inverse variance, SD = standard deviation.
3.7. Length of hospitalization
The length of hospitalization was assessed by 6 of the included papers,[15,18–21,23] with a total of 3157 patients, including 1576 and 1581 patients in the restrictive and liberal transfusion threshold groups, respectively. A fixed effects model was used for data analysis. The length of hospital stay did not differ significantly between the 2 groups (mean difference = 0.14, 95%CI −0.13–0.42, P = .31), and no statistically significant heterogeneity was found (χ2 = 5.45, df = 5, P = .36, I2 = 8%; Fig. 7). Publication bias was not found according to Begg test (P = 1.00) or Egger test (P = .07; 95%CI −2.53–0.16).
Figure 7.
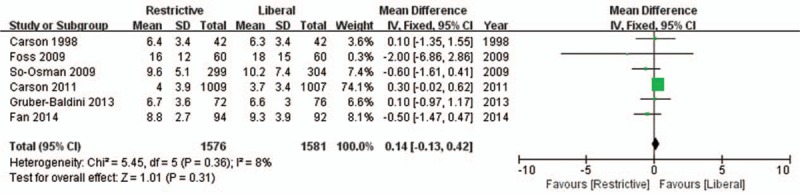
Forest plot of length of hospitalization. 95% CI = 95% confidence interval, df = degrees of freedom, Fixed = fixed effects model, IV = inverse variance, SD = standard deviation.
3.8. Sensitivity analyses
Sensitivity analyses investigating the influence of each single study on the overall outcome estimate were conducted by omitting 1 study at a time. The results of each sensitivity analysis were not materially different from the original data.
4. Discussion
Study selection and the homogeneity of selected studies play important roles in the quality of meta-analyses. Only RCTs were assessed in this meta-analysis because they can optimize follow-up and data quality, while minimizing selection bias and other confounding factors.[24] All 10 RCTs included in this meta-analysis were of sufficient methodological quality, with most of high quality. We conducted a sensitivity analysis to explore the impact of each trial on the pooled effect estimates for each outcome, and found that omitting any one of the studies did not have a significant effect on the overall results. Additionally, we did not observe any obvious publication bias in the current meta-analysis according to Begg and Egger test.
This meta-analysis of RCTs demonstrated that there was no significant difference in 30-day mortality between the restrictive and liberal transfusion strategy groups. These findings are consistent with most previously published meta-analyses.[6,8,26,27] However, unlike the latter reports, we pooled data only from randomized trials assessing adult hip or knee surgery patients that compared restrictive and liberal transfusion thresholds. The clinical settings and thresholds for blood transfusion were similar in all the trials included in the current meta-analysis. Carson et al[20] evaluated 2016 patients who underwent hip fracture surgery. The rate of in-hospital mortality was not significantly different between the 2 groups, with 2.0% and 1.4% mortality recorded for the liberal and restrictive transfusion threshold groups, respectively. A retrospective study of 919 individuals in an elderly population undergoing surgery for hip fracture found that receiving an RBC transfusion is not associated with changes in mortality.[28] Parker et al[22] reported that a restrictive transfusion policy is not associated with any statistically significant difference in 90-, 120-, or 365-day mortality.
We found no significant difference in pneumonia or wound infection rates in orthopedic patients when comparing the restrictive transfusion strategy with the liberal counterpart. A recent meta-analysis that included 8 RCTs showed that restrictive transfusion strategies are associated with a 35% decrease in infection risk in orthopedic patients.[7] However, in the latter review, only some of the included studies reported the overall number of patients with infection precisely. Therefore, this finding should be interpreted with caution in that it derived from incomplete data in terms of infection rates for the whole trial population. Claridge et al[29] demonstrated that undergoing blood transfusion is associated with an increased susceptibility to infection and transfusion-related lung injury, suggesting that liberal transfusion would increase the risk of these negative outcomes. To verify this report, we added 2 additional RCTs to our analysis. However, we did not find significantly decreased rates of pneumonia or wound infection in the restrictive transfusion threshold group.
The results of the current meta-analysis indicated that there were no significant differences in the myocardial infarction incidence, congestive heart failure incidence, or length of hospital stay between hip or knee surgery patients treated with restrictive and liberal transfusion thresholds, respectively. A previous systematic review[10] reported a lower incidence of myocardial infarction in patients treated with the liberal transfusion strategy than in those treated with a restrictive transfusion approach. This meta-analysis included 2 additional studies, and although a similar trend was observed, it did not reach statistical significance. Carson et al[30] proposed that for patients presenting with acute myocardial infarction or heart failure, clinicians should opt for a more liberal transfusion strategy to maintain oxygenation. Additional large scale and well-designed RCTs are required before definitive conclusions can be made.
Furthermore, this study also examined the impact of the restrictive transfusion strategy on transfusion frequency in patients undergoing lower limb surgery. The results suggested that the restrictive transfusion strategy served its purpose of reducing the number of RBC transfusions performed in the postoperative period, with 39% less patients receiving blood transfusion after lower limb surgery. The variations in anesthesia methods and operation modes between trials may explain the significant heterogeneity observed in this analysis. So-Osman et al[19] reported that hip surgery patients have blood transfusion significantly more often (11%) than knee surgery patients (4.1%).
Several studies have suggested that blood transfusions are associated with adverse outcomes and high costs.[31,32] According to surgeons, reduction of complications related to blood transfusion could speed the postoperative rehabilitation of patients and avoid the huge medical expenses. This study demonstrated that there were no significant differences in terms of mortality, and the incidence rates of pneumonia, wound infection, myocardial infarction, and congestive heart failure between the restrictive and liberal transfusion thresholds for RBC transfusion, suggesting that restrictive transfusion strategies could potentially reduce the number of transfusions and relieve the economic burden of using liberal transfusion strategies, without increasing the risk of adverse events. Finally, compared with previous similar studies,[33] this analysis updates the results of restrictive versus liberal transfusion strategies for red blood cell transfusion in adult participants with lower limb surgery.
This study had several limitations that should be considered. First, the current analyses were based on a limited number of studies. Notably, the study by Carson et al[20] had the largest number of participants, so its weight was much larger than those of the remaining included studies. Second, the thresholds of restrictive and liberal transfusion strategies varied among the included studies. Third, the aggregate data of patients undergoing hip or knee replacement surgery were reported in only 2 of all included studies,[17,19] which limited our ability to conduct meaningful subgroup analyses comparing hip and knee surgeries. Fourth, variations in anesthesia methods, operation modes, and prosthesis types in the included studies may have resulted in bias. Finally, any uncontrolled confounding factors inherited from the original studies might have influenced these results, although we found no evidence for statistically significant heterogeneity in most results.
5. Conclusion
This updated meta-analysis found no difference in 30-day mortality, length of hospitalization, or incidence rates of infections, myocardial infarction, and congestive heart failure, between patients who underwent lower limb surgery with restrictive versus liberal transfusion strategies. However, our meta-analysis was based on a limited number of studies. Additional large-scale RCTs would be of value to confirm these findings.
Acknowledgments
The authors thank National Natural Science Foundation of China (81372013, 81672236), Beijing Natural Science Foundation (7174346), and the Research Fund of China-Japan Friendship Hospital (2014–4-QN-29); China–Japan Friendship Hospital Youth Science and technology excellence project (2014-QNYC-A-06) for the support. The authors also thank the members of the Department of Epidemiology and Bio-statistics, School of Public Health, Peking University for help with the statistical analysis, and Fan Meng (experienced nurse) for helpful discussions.
Footnotes
Abbreviations: RBC = red blood cell, RCT = randomized controlled trial, RR = risk ratio.
TM, FG, and JH are the first coauthors.
Funding/support: This study was funded by the National Natural Science Foundation of China (81372013, 81672236), Beijing Natural Science Foundation (7174346), and the Research Fund of China-Japan Friendship Hospital (2014–4-QN-29); China–Japan Friendship Hospital Youth Science and technology excellence project (2014-QNYC-A-06).
The authors have no conflicts of interest to disclose.
References
- [1].Ferraris VA, Bown JR, Despotis GJ, et al. Update to the society of thoracic surgeons and the society of cardiovascular anesthesiologists blood conservation clinical practice guidelines. Ann Thorac Surg 2011;91:944–8. [DOI] [PubMed] [Google Scholar]
- [2].Carson JL, Duff A, Poses RM. Effect of anemia and cardiovascular disease on surgical mortality and morbidity. Lancet 1996;348:1055–60. [DOI] [PubMed] [Google Scholar]
- [3].Hebert PC, Wells G, Tweeddale M, et al. Does transfusion practice affect mortality in critically ill patients? Transfusion Requirements in Critical Care (TRICC) Investigators and the Canadian Critical Care Trials Group. Am J Respir Crit Care Med 1997;155:1618–23. [DOI] [PubMed] [Google Scholar]
- [4].Adams RC, Lundy JS. Anesthesia in cases of poor surgical risk: some suggestions for decreasing the risk. Surg Gynecol Obstet 1942;74:1011–9. [Google Scholar]
- [5].Borghi B, Casati A. Incidence and risk factors for allogenic blood transfusion during major joint replacement using an integrated auto-transfusion regimen. The Rizzoli Study Group on Orthopaedic Anaesthesia. Eur J Anaesthesiol 2000;17:411–7. [DOI] [PubMed] [Google Scholar]
- [6].Vuille-Lessard E, Boudreault D, Girard F, et al. Postoperative anemia does not impede functional outcome and quality of life early after hip and knee arthroplasties. Transfusion 2012;52:261–70. [DOI] [PubMed] [Google Scholar]
- [7].Holst LB, Petersen MW, Haase N, et al. Restrictive versus liberal transfusion strategy for red blood cell transfusion: systematic review of randomised trials with meta-analysis and trial sequential analysis. Br Med J 2015;350:1354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Teng ZW, Zhu Y, Liu YG, et al. Restrictive blood transfusion strategies and associated infection in orthopedic patients: a meta-analysis of 8 randomized controlled trials. Sci Rep 2015;5:13421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Salpeter SR, Buckley JS, Chatterjee S. Impact of more restrictive blood transfusion strategies on clinical outcomes: a meta-analysis and systematic review. Am J Med 2014;127:124–31. [DOI] [PubMed] [Google Scholar]
- [10].Brunskill SJ, Millette SL, Shokoohi A, et al. Red blood cell transfusion for people undergoing hip fracture surgery. Cochrane Database Syst Rev 2015;21:CD009699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Moher D, Liberati A, Tetzlaff J, et al. PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009;10:1006–12. [DOI] [PubMed] [Google Scholar]
- [12].Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Version 4.2.5 (2005). The Atrium, Southem Gate, Chichester, West Sussex POI98SQ, England: John Wiley & Sons Ltd; 2005. [Google Scholar]
- [13].Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 1996;17:1–2. [DOI] [PubMed] [Google Scholar]
- [14].Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994;50:1088–101. [PubMed] [Google Scholar]
- [15].Egger M, David SG, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Carson JL, Terrin ML, Barton FB, et al. A pilot randomized trial comparing symptomatic vs. hemoglobin-level-driven red blood cell transfusions following hip fracture. Transfusion 1998;38:522–9. [DOI] [PubMed] [Google Scholar]
- [17].Grover M, Talwalkar S, Casbard A, et al. Silent myocardial ischaemia and haemoglobin concentration: a randomized controlled trial of transfusion strategy in lower limb arthroplasty. Vox Sang 2006;90:105–12. [DOI] [PubMed] [Google Scholar]
- [18].Foss NB, Kristensen MT, Jensen PS, et al. The effects of liberal versus restrictive transfusion thresholds on ambulation after hip fracture surgery. Transfusion 2009;49:227–34. [DOI] [PubMed] [Google Scholar]
- [19].So-Osman C, Nelissen R, Te Slaa R, et al. A randomized comparison of transfusion triggers in elective orthopaedic surgery using leucocyte-depleted red blood cells. Vox Sang 2010;98:56–64. [DOI] [PubMed] [Google Scholar]
- [20].Carson JL, Terrin ML, Noveck H, et al. Liberal or restrictive transfusion in high-risk patients after hip surgery. N Engl J Med 2011;365:2453–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Gruber-Baldini AL, et al. Delirium outcomes in a randomized trial of blood transfusion thresholds in hospitalized older adults with hip fracture. J Am Geriatr Soc 2013;61:1286–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Parker MJ, et al. Randomised trial of blood transfusion versus a restrictive transfusion policy after hip fracture surgery. Injury 2013;44:1916–8. [DOI] [PubMed] [Google Scholar]
- [23].Fan YX, Liu FF, Jia M, et al. Comparison of restrictive and liberal transfusion strategy on postoperative delirium in aged patients following total hip replacement: a preliminary study. Arch Gerontol Geriatr 2014;59:181–5. [DOI] [PubMed] [Google Scholar]
- [24].Gregersen M, Borris LC, Damsgaard EM. Postoperative blood transfusion strategy in frail, anemic elderly patients with hip fracture. Acta Orthop 2015;86:363–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Nielsen K, Johansson PI, Dahl B, et al. Perioperative transfusion threshold and ambulation after hip revision surgery- a randomized trial. BMC Anesthesiol 2014;14:89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Ibrahim M, Ho SK, Yeo CL. Restrictive versus liberal red blood cell transfusion thresholds in very low birth weight infants: a systematic review and meta-analysis. J Paediatr Child Health 2014;50:122–30. [DOI] [PubMed] [Google Scholar]
- [27].Wang J, Bao YX, Bai M, et al. Restrictive vs liberal transfusion for upper gastrointestinal bleeding: a meta-analysis of randomized controlled trials. World J Gastroenterol 2013;19:6919–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Shokoohi A, Stanworth S, Mistry D, et al. The risks of red cell transfusion for hip fracture surgery in the elderly. Vox Sang 2012;103:223–30. [DOI] [PubMed] [Google Scholar]
- [29].Claridge JA, Sawyer RG, Schulman AM, et al. Blood transfusions correlate with infections intrauma patients in a dose-dependent manner. Am Surg 2002;68:566–72. [PubMed] [Google Scholar]
- [30].Carson JL, Carless PA, Hebert PC. Transfusion thresholds and other strategies for guiding allogeneic red blood cell transfusion. Cochrane Database Syst Rev 2012;4:CD002042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Corwin HL, Gettinger A, Pearl RG, et al. The CRIT Study: anemia and blood transfusion in the critically ill-current clinical practice in the United States. Crit Care Med 2004;32:39–52. [DOI] [PubMed] [Google Scholar]
- [32].Blumberg N, Kirkley SA, Heal JM. A cost analysis of autologous and allogeneic transfusions in hip-replacement surgery. Am J Surg 1996;171:324–30. [DOI] [PubMed] [Google Scholar]
- [33].Holst Lars B, Petersen Marie W, Haase Nicolai, et al. Restrictive versus liberal transfusion strategy for red blood cell transfusion: systematic review of randomised trials with meta-analysis and trial sequential analysis. BMJ 2015;350:h1354. [DOI] [PMC free article] [PubMed] [Google Scholar]


