Abstract
Objective
Soft tissue (ST) dehiscence with graft exposure is a frequent complication of vertical augmentation. Flap dehiscence is caused by failure to achieve tension‐free primary wound closure and by the impairment of flap microcirculation due to surgical trauma.
Soft tissue expansion (STE) increases ST quality and quantity prior to reconstructive surgery. We hypothesized that flap preconditioning using STE would reduce the incidence of ST complications after bone augmentation and that optimized ST healing would improve the outcome of bone regeneration.
Materials and methods
Self‐filling tissue expanders were implanted in mandibular bone defects in ten beagle dogs. After expansion, alloplastic scaffolds were placed for vertical bone augmentation in STE sites and in control sites without STE pre‐treatment. ST flap microcirculation was analysed using laser Doppler flowmetry. The incidence of graft exposures was evaluated after 2 weeks. Bone formation was assessed after 2 months, using histomorphometry and immunohistochemistry.
Results
Test sites showed significantly less impairment of perfusion and faster recovery of microcirculation after bone augmentation. Furthermore, no flap dehiscences occurred in STE sites. Bone regeneration was found in both groups; however, significantly greater formation of new bone was detected in test sites with preceding STE.
Conclusions
Preconditioning using STE improved ST healing and bone formation after vertical augmentation. The combination of STE and the subsequent placement of alloplastic scaffolds may facilitate the reconstruction of severe bone defects.
Keywords: animal experiments, biomaterials, bone regeneration, guided tissue regeneration, surgical techniques, wound healing
Placement of endosseous dental implants often requires the reconstruction of lost bone. The principles of guided bone regeneration (GBR) include the maintenance of regenerative space and the stabilization of a blood clot due to the placement of scaffolds consisting of granular material and covering barrier membranes on the local bone. The membrane secludes the scaffold from the periosteum and other soft tissues, and angiogenic and osteogenic cells proliferate from the local bone marrow into the membrane‐protected area, with the result of intramembranous ossification (Buser et al. 1996; Kostopoulos & Karring 1995; Kostopoulos et al. 1994; Schenk et al. 1994).
As yet, the routine use of GBR is limited to self‐containing defects, where remaining bony walls exert mechanical support and protect the scaffold against macro‐motion caused by soft tissue movement (Dahlin et al. 1988); that is, GBR may be primarily used for the regeneration of defects within the contour of residual bone (Esposito et al. 2009; McAllister & Haghighat 2007). In contrast, the outcomes of extra‐skeletal osseous reconstructions appear dubious. Sparse clinical and histological data support the feasibility of extra‐skeletal augmentation especially with autogenous bone used as block grafts or with reinforced scaffolding constructs (Esposito et al. 2009; Rocchietta et al. 2008). Clinical data show a high incidence of soft tissue wound dehiscences with the subsequent exposure of bone grafts or scaffolds (up to 50%), which may cause complete failure of the reconstructive treatment (Jensen & Terheyden 2009; Kaner & Friedmann 2011). Primary wound closure after placement of grafts or scaffolds for vertical augmentation requires large‐scale mobilization and advancement of soft tissues in order to cover the reconstructed area (Greenstein et al. 2009). Dehiscences occur mainly after difficulties in attaining primary wound closure, and due to high strain on the margins of the covering mucoperiosteal flaps (Burkhardt & Lang 2010). Further, flap surgery affects perfusion and induces ischaemia, while ample blood flow is essential for the survival of tissue (Nakayama et al. 1982). Correspondingly, traumatic surgery massively reduces blood supply and causes ischaemia/reperfusion injury, leading to tissue damage and necrosis of the operated tissue (Carroll & Esclamado 2000). Indeed, the extent of surgical trauma and the resultant impairment of soft tissue microcirculation are correlated (Retzepi et al. 2007), while the maintenance of sufficient blood supply to the soft tissues is one of the prerequisites for bone healing (Stegen et al. 2015). Therefore, quality and quantity of soft tissue and its resilience against surgical trauma may be crucial for successful bone regeneration. Preservation of reconstructed bone is another matter of importance, as up to 70% of grafted bone may be resorbed throughout healing (McAllister & Haghighat 2007; Simon et al. 2000). Again, compromised vascularization and soft tissue deficiencies causing the mechanical instability of the augmented area may contribute to these negative outcomes of bone regeneration (Lundgren et al. 2008; Rothamel et al. 2009).
Soft tissue expansion (STE) improves tissue quantity and quality in order to facilitate the subsequent reconstructive surgery; that is, STE provides a tissue surplus for easier primary closure and improves flap vascularity and viability (Asa'ad et al. 2015; Bascom & Wax 2002; Cherry et al. 1983). Pre‐treatment by STE prior to vertical augmentation with autogenous bone leads to high gain of new bone, minimizes graft resorption, and results in a very low incidence of wound dehiscences (Abrahamsson et al. 2012; Kaner & Friedmann 2011; Mertens et al. 2013; for review, see Asa'ad et al. 2015). As yet, the effects of STE on the outcome of vertical augmentation have only been investigated using autogenous grafts. Many clinicians prefer autogenous bone over alloplastic materials for complex osseous reconstructions because of its combined osteoconductive and osteoinductive properties (Miron & Zhang 2012). However, harvesting of bone causes significant morbidity and costs, and poses additional risks (Nkenke & Neukam 2014). While alternatives to autogenous bone appear desirable, data on vertical augmentation using GBR with alloplastic scaffolds alone after preconditioning with STE have not yet been published. Here, we report on the effects of STE on GBR using alloplastic scaffolds in an animal model of vertical augmentation.
The hypothesis was that preconditioning with STE would reduce the impairment of perfusion and improve the healing of soft tissues after vertical augmentation; finally, the better preconditions would improve the outcome in terms of an increased formation of new bone.
Material and methods
The study protocol was in accordance with the European Communities Council Directive of 24 November 1986 (86/609/EEC) and local laws and regulations. It was approved by the Food Safety and Animal Health Protection Board of the Regional Council of Pest/Hungary. The study was carried out at the Research Institute for Animal Breeding and Nutrition, Herceghalom/Hungary, which provided ten male beagle dogs (mean age 8.1 ± 0.9 months, mean weight 12.2 ± 1.3 kg). The dogs were kept in pairs in kennels of five sqm with straw bedding and elevated wooden resting places and were walked twice daily for at least 30 min. They were fed commercially available dog food (Bonafarm, Nagyigmánd/Hungary), and water was provided ad libitum. Surgeries were carried out in general anaesthesia; ketamine hydrochloride (2.5 ml/10 kg; Ketavet 10%, Pfizer, Berlin/Germany) and xylazine hydrochloride (1 ml/10 kg; Xylavet 2%, Sanofi‐Aventis, Budapest/Hungary) were administered intravenously every 15 min. For pain control, intramuscular injections of metamizole (1 ml/10 kg; Algopyrin, Sanofi, ‐Aventis, Budapest/Hungary) were administered for 3 days. Amoxicillin hydrochloride (150 mg, 1 ml/10 kg, Pfizer, Berlin/Germany) was injected intramuscularly for prophylaxis of infections.
Bone defects and STE
The surgical procedures have been specified earlier in detail (Kaner et al. 2014). Briefly, all premolars were extracted and the tooth‐supporting bone was additionally reduced in order to create supra‐alveolar critical‐size defects on both sides of the mandible (Wikesjo et al. 2006). Six weeks later, tissue expanders (cylinder 0.7 ml; Osmed, Ilmenau/Germany) were placed in submucosal pouches in randomly allocated mandibular test sites for a 5‐week expansion phase; according to a split‐mouth design, opposing mandibular sides were used as controls (Fig. 1a, b).
Figure 1.
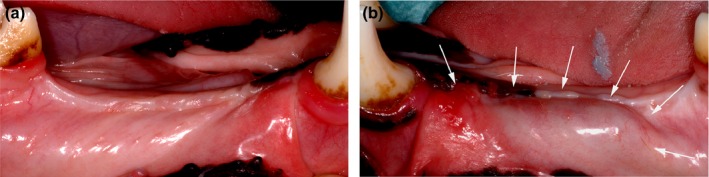
(a) Control site prior to vertical bone augmentation. Note the vertical and horizontal loss of tissue. (b) STE test site prior to vertical bone augmentation with tissue expander in place (arrows), after 5 weeks of expansion.
Vertical augmentation
0.5 ml of a local anaesthetic (articaine 4% with 1 : 100 000 epinephrine; UDS forte, Sanofi‐Aventis, Frankfurt/Germany) was injected each buccally and lingually. At STE sites, the tissue expanders were removed after placement of a mid‐crestal incision without releasing incisions. The tissue below the expander was cut in mesiodistal direction, buccal and lingual flaps were elevated, and the bone was exposed.
A similar incision was placed at control sites. Additional releasing incisions were extended from the canine and the first molar into the mucosa. Buccal and lingual flaps were raised, and the bone was exposed.
The recipient bone at test and control sites was perforated to provoke bleeding, and the defect was augmented with a scaffold consisting of granular biphasic calcium phosphate soaked with blood, and a resorbable polyethylene glycol membrane (BCP/PEG; Institut Straumann AG, Basel/Switzerland; Fig. 2a, b). Length, width and height were measured in millimetres, and the volume of the semioval scaffold was calculated in mm3 (ScVol). Wound closure at test sites was attained without additional flap advancement. At control sites, periosteum and submucosa were stripped and dissected until the flaps covered the scaffold passively, as recommended (Greenstein et al. 2009). Flaps were closed with vertical mattress sutures and fine continuous sutures (Vicryl 3.0 and Monocryl 6.0, Ethicon, Norderstedt/Germany).
Figure 2.
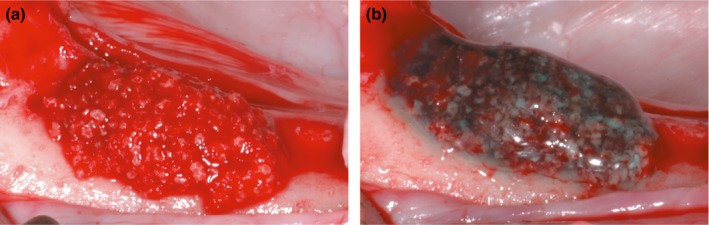
(a) BCP mixed with blood and applied on the residual bone ridge. (b) Completed scaffold after application of the PEG membrane gel onto the BCP granules.
Microcirculation and soft tissue healing
Results on microcirculation and soft tissue healing have been reported previously in detail (Kaner et al. 2015). The primary outcome, soft tissue dehiscence (yes/no), was evaluated after 2 weeks. Flap microcirculation was measured at augmentation surgery before local anaesthesia (baseline), 2 min later, immediately after surgery, and after 3 days, using laser Doppler flowmetry (LDF; Periflux 5010, PF 416 probe, outside diameter 1.0 mm, fibre separation 0.25 mm, wavelength 780 nm; Perimed AB, Jarfalla/Sweden).
Preparation of specimens
After 8 weeks, all animals were killed with pentobarbital. The mandibles were dissected and snap‐frozen at −80°C. Later, the samples were thawed in buffered 4% formalin for 22 h. The specimens were dehydrated in graded ethanol and xylene, and infiltrated and embedded in resin (Technovit 9100, Heraeus Kulzer, Wehrheim/Germany) at −15°C. All specimens were sectioned in buccolingual direction into slides of 80 μm thickness, using a saw microtome (SP1600, Leica, Bensheim/Germany), and stained (Masson Goldner trichrome). Digital images were obtained using a light microscope equipped with a digital camera with 5‐megapixel CCD (Leitz DMRB and Leica DFC 425 C, Leica, Wetzlar/Germany).
Histomorphometry
The total augmented area (TA) in each specimen was determined by agreement between three investigators (AF, HZ and WA). Single images of the augmented area under 32‐fold magnification were stitched to an overview image, using image‐processing software (Adobe Photoshop CS6, Adobe, Dublin/Ireland). One investigator (HZ) calculated areas for new bone (NB), osteoid (O), connective tissue (CT) and residual particles (RP), and their proportions (%) of TA, using AutoCAD 2011 software (Autodesk, Munich/Germany).
Immunohistochemistry
The sections were treated with 2‐methoxyethyl acetate for 4 min to dissolve the resin and were rehydrated in graded alcohol and washed in PBS for 10 min. Endogenous peroxidase was blocked with peroxidase block (Dako, Hamburg/Germany) for 5 min. Antigens were unmasked using trypsin (TG‐II: Abcam, Cambridge/UK) and proteinase K (OC: Abcam, Cambridge/UK), respectively, for 10 min. Non‐specific binding was blocked by incubation with blocking solution (Danko, Hamburg/Germany) for 15 min. The sections were incubated with primary antibodies (TG‐II: anti‐transglutaminase‐II AB‐1, mouse antibody, Lab Vision Corporation, Fremont/CA, USA; OC: anti‐osteocalcin, mouse antibody, Abcam, Cambridge/UK), respectively, for 50 min. Then, the slides were washed in PBS for 10 min and incubated with streptavidin–peroxidase solution (Dako, Hamburg/Germany) for 45 min. 3‐Amino‐9‐ethylcarbazole (Dako, Hamburg/Germany) was used as chromogen. A semiquantitative evaluation of staining intensity (negative/weak/strong) was independently carried out by three investigators (WA, AF and DK).
Statistical analysis
One investigator (DK) carried out all statistical analyses. Sample size was calculated for the primary endpoint (soft tissue dehiscence, binary outcome yes/no) with the animal as the unit of analysis (Rosner 2010). The assumption that the proportions of dehiscences would be 50% in control sites and 0% in test sites resulted in a sample size of nine animals in a split‐mouth design (two‐sided test, α = 0.05, β = 0.8). In order to compensate for potential dropouts, ten dogs were used.
Medians and quartiles were calculated for ScVol, changes in LDF measurements and histomorphometric parameters and their proportions of TA. Mann–Whitney U‐test and Fisher's exact test were used for comparisons between test and control groups. Wilcoxon's signed‐rank test was used for longitudinal comparisons within groups. Correlations between histomorphometric parameters were analysed using Spearman's correlation coefficient. Levels of TG‐II and OC were compared using the chi‐squared test. The level of significance was α = 0.05. All histomorphometric and immunohistochemical evaluations and the statistical analyses were carried out blinded to the group allocation.
Results
Expander surgery and initial healing were without complications. Later, three expanders were lost before augmentation, as reported previously in detail (Kaner et al. 2015). At augmentation surgery, similar‐sized scaffolds were applied in both groups (test: median ScVol = 141 mm3 (IQ 110; 191), control: median ScVol = 130 mm3 (IQ 108; 161), P = 0.529).
Microcirculation and soft tissue healing
Detailed results for microcirculation and soft tissue healing have been reported previously (Kaner et al. 2015). Uneventful healing in test sites contrasted with the finding of eight dehiscences in control sites (P = 0.002).
Comparable LDF measurements before augmentation and similar declines caused by local anaesthesia were found in both groups (data not shown). However, perfusion dropped significantly after augmentation surgery in control sites (P < 0.001), whereas test site perfusion remained stable (P = 0.627). Accordingly, microcirculation after augmentation was significantly better in STE sites (P = 0.012).
From the termination of augmentation surgery to the third post‐surgical day, no change was found in test sites, while control sites showed significant increases in perfusion (P = 0.001). Nevertheless, microcirculation measurements at control sites were – contrasting to test sites – still significantly lower after 3 days, when compared to baseline (P = 0.005).
Histomorphometry
Total augmented area
Figure 3 depicts representative sections after 2 months of healing. Test sites and control sites showed similar median values for TA (test: 9.49 mm2; IQ 4.62; 14.85/control: 5.26 mm2; IQ 3.35; 6.97; P = 0.105; Table 1).
Figure 3.
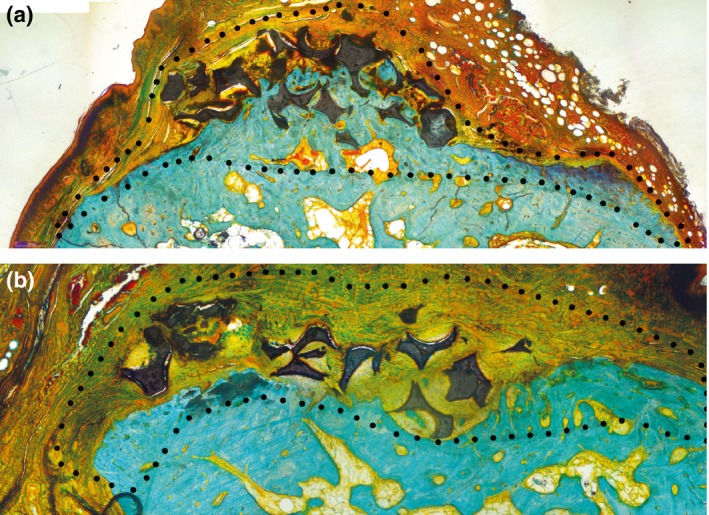
(a) Representative histological section of a test group specimen with highlighted total augmented area (Masson Goldner trichrome staining). (b) Representative histological section of a control group specimen with highlighted total augmented area (Masson Goldner trichrome staining).
Table 1.
Histomorphometric parameters for test and control groups (medians and interquartiles)
| TA (mm2) | NB (mm2) | CT (% of TA) | |
|---|---|---|---|
| Test | 9.49 | 3.81 a | 19.80 b |
| IQ | (4.62, 14.85) | (1.33, 5.35) | (15.43, 27.60) |
| Range | 2.28–18.64 | 0.21–8.63 | 2.8–11.7 |
| Control | 5.26 | 1.06 a | 42.27 b |
| IQ | (3.35, 6.97) | (0.43, 1.39) | (30.18, 61.48) |
| Range | 2.75–8.23 | 0–4.11 | 4.32–23.35 |
Significant difference in favour of the test group, P = 0.023.
Significant difference in favour of the test group, P = 0.009 (Mann–Whitney U‐test).
TA: total augmented area; NB: new bone; CT: connective tissue.
New bone area
New bone was found in all ten test sites, whereas two of ten control specimens showed no NB formation at all. Test sites showed greater areas of NB than control sites (Table 1). NB covered 3.81 mm2 (median, IQ 1.33; 5.35) in test sites, whereas control sites showed a NB area of 1.06 mm2 (median, IQ 0.43; 1.39). The difference was statistically significant (P = 0.023) favouring the test group.
Proportion of connective tissue
CT covered 19.80% (median, IQ 10.98%; 46.95%) of TA in test sites, whereas control sites showed a CT proportion of 42.27% (median, IQ 17.29%; 93.39%) of TA (significant difference favouring the test group, P = 0.009, Table 1).
Other parameters
For NB%, CT, O, O%, RP and RP%, no significant differences were found between both groups (data not shown).
Correlations between histomorphometric parameters
The correlation between the area covered with osteoid and TA was significant in both groups (test: r = 0.794, P = 0.006; control: r = 0.927, P < 0.001). Both groups showed similar correlations between TA and the amount of RP (test: r = 0.818, P = 0.004; control: r = 0.830, P = 0.003).
However, NB was correlated with TA in test specimens only (r = 0.794, P = 0.006, Fig. 4a). In contrast, control specimens showed no significant correlation between NB and TA (P = 0.059, Fig. 4b).
Figure 4.
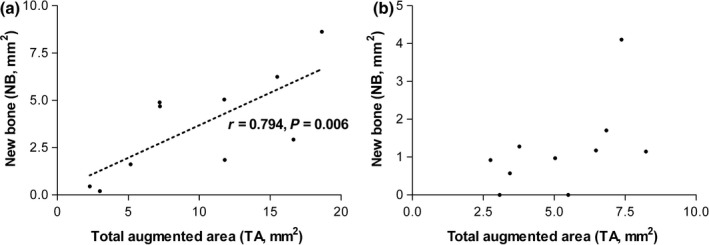
(a) Significant correlation between the total area of interest (TA) and new bone (NB) in test sites (Spearman's correlation coefficient, r = 0.794, P = 0.006). (b) Lack of significant correlation between the total area of interest (TA) and new bone (NB) in control sites (Spearman's correlation coefficient, r = 0.614, P > 0.05). Two specimens showed no bone formation at all.
Osteocalcin
In the test group, five specimens were negative for OC. One specimen showed a weak staining only, while four specimens showed a strong reaction for OC (Fig. 5a).
Figure 5.
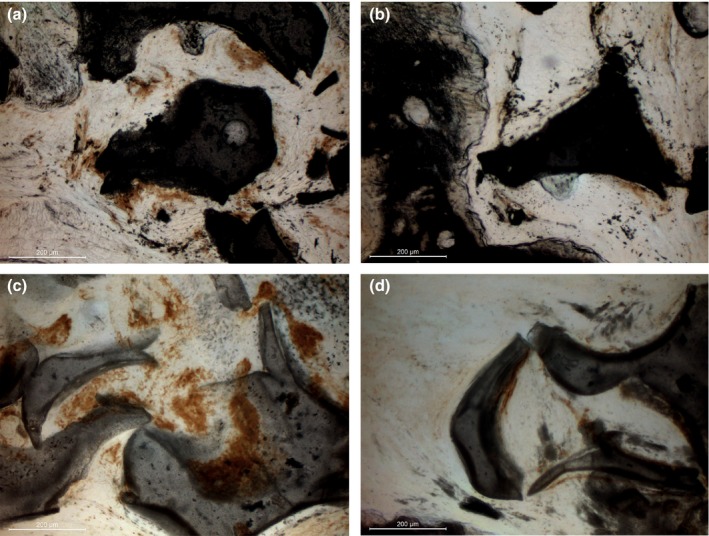
a, b. Immunohistochemical stainings for OC with strong staining intensity scattered around BCP particles in test specimens (a). As well, positive staining is found in small zones around the BCP particles in control specimens (b). No statistically significant difference between groups (Table 2). c, d. Immunohistochemical stainings for TG‐II with very strong staining intensity around BCP particles in test specimens (c). Some positive staining is found in small zones around the BCP particles in control specimens (d). The difference between both groups is statistically significant (Table 3).
Six control specimens were OC negative. Three specimens showed a weak staining only (Fig. 5b), while one specimen showed a strong reactivity for OC. No significant difference was found (P = 0.236, chi‐squared test, Table 2).
Table 2.
Immunohistochemical reactivity for osteocalcin (the number of specimens)
| Osteocalcin staining intensity | |||
|---|---|---|---|
| Negative | Weak | Strong | |
| Test | 5 | 1 | 4 |
| Control | 6 | 3 | 1 |
No significant difference between the groups (P = 0.236, chi‐squared test).
Transglutaminase II
In the test group, three specimens were TG‐II negative. Two specimens showed weak staining only, while five specimens showed a strong TG‐II reactivity (Fig. 5c). In the control group, six specimens were TG‐II negative and four specimens showed a weak staining (Fig. 5d). No control specimen showed a strong TG‐II reactivity. The difference between the groups was statistically significant (P = 0.036, chi‐squared test, Table 3).
Table 3.
Immunohistochemical reactivity for transglutaminase II (the number of specimens)
| Transglutaminase II staining intensity | |||
|---|---|---|---|
| Negative | Weak | Strong | |
| Test | 3 | 2 | 5 |
| Control | 6 | 4 | 0 |
Significant difference favouring the test group (P = 0.03, chi‐squared test).
Discussion
We compared the outcomes of vertical augmentation using GBR between sites with or without preceding STE in a critical‐size defect model that has been designed for rigorous testing of techniques and materials aimed at supra‐alveolar bone regeneration (Wikesjo et al. 2006). The volume of the BCP/PEG scaffolds placed on the residual bone was similar in both groups. Histomorphometric calculations showed no difference between test and control sites with regard to the total augmented area after 8 weeks of healing. Obvious bone formation and similar amounts of osteoid and residual BCP particles in both test and control sites indicate bone regeneration according to the GBR principle regardless of group allocation, and corroborate the results for these materials obtained in less critical situations such as grafting of the maxillary sinus or of other self‐containing defects. In these favourable conditions, osteogenesis around BCP granules resembles intramembranous bone formation, passing the stages of osteoid formation, mineralization, the generation of fibrous bone and remodelling (Friedmann et al. 2009, 2015; Thoma et al. 2012). Likewise, both groups showed a similar immunohistochemical reactivity for the mineralization marker osteocalcin, as found previously in studies that demonstrated the osteoconductivity of BCP in straightforward dehiscence‐type defects around implants (Sager et al. 2012; Schwarz et al. 2010).
Nevertheless, test sites with preceding STE showed significantly greater areas of new bone formation. Consistently, significantly higher proportions of connective tissue were found in control sites, and two of ten control sites failed to show any bone formation at all. The significantly stronger immunohistochemical reactivity for TG‐II, a marker substance for a maturating bone matrix and ongoing calcification (Nurminskaya & Kaartinen 2006), observed in the bone matrix around residual particles in test sites, matches the histomorphometric outcomes and emphasizes the different outcomes of osteogenesis in both groups.
Inferior bone formation in sites without STE was preceded by poor soft tissue healing after augmentation surgery, when test and control sites are compared. In all STE sites, soft tissues healed primarily and without complications. Conversely, exposure of the BCP/PEG scaffold to the oral cavity was the consequence of soft tissue dehiscence in eight control sites. Premature degradation of membranes, bacterial infection of the surgical site, exfoliation of scaffold material and secondary healing are consequences of graft exposure. Inflammatory infiltrates are common around scaffolding materials in sites after secondary healing, and as found in compromised control sites in our study, bone regeneration may either be limited or fail completely (Moses et al. 2005; Friedmann et al. 2015).
Linear correlations between the total augmented area (TA) and other histomorphometric parameters are to be expected as outcome of GBR (von Arx et al. 2001); that is, a given scaffold volume should predictably generate a certain amount of new bone. In both groups, TA was indeed positively correlated with the areas covered with osteoid and with residual particles, respectively. Interestingly, a highly significant and strong correlation between TA and the amount of new bone was solely found in STE sites (r = 0.794, P = 0.006), indicating that a reliable and predictable relation between the scaffold volume and the amount of newly formed bone existed in test sites only. Obviously, the positive effects of STE on soft tissue healing proved beneficial on the outcome of GBR applied for vertical augmentation.
Besides complications, a scaffold's resilience against deformation and displacement and its capability in maintaining space affect bone healing (Babis & Soucacos 2005; Moses et al. 2005). Mechanical stability is a prerequisite for vascularization and angiogenesis during bone formation and is necessary to allow incorporation and remodelling of implanted scaffolds (Babis & Soucacos 2005; Dimitriou et al. 2011). Likewise, mechanical instability affects the proliferation and differentiation of regenerating tissues: while direct bone formation occurs in regions exposed to neither compressive stress nor tensile strain, high tensile strain and increased macro‐mobility increase the formation of fibrous tissues and inhibit osteoneogenesis (Carter et al. 1998; Hiltunen et al. 1993). In our study, the tissue surplus created by STE may have increased the resilience of the BCP/PEG scaffolds against deformation and displacement, as illustrated by higher amounts of new bone and the strong correlation between NB and TA.
In order to place a scaffold, a mucoperiosteal flap has to be elevated, and the resultant surgical trauma disturbs perfusion and induces ischaemia (McLean et al. 1995). The extent of the subsequent microvascular damage can be monitored by LDF (Retzepi et al. 2007). LDF measurements taken directly after augmentation surgery and after 3 days, respectively, showed distinct differences between sites with and without preceding STE. Augmentation surgery caused a significant additional decrease in microcirculation in control sites, whereas no further reduction in perfusion beyond the effect of local anaesthesia was observed in STE test sites. Accordingly, microcirculation was significantly better in test sites after the conclusion of augmentation surgery, and perfusion had fully recovered after 3 days. In contrast, a significant disturbance of microcirculation was still present in control sites 3 days after surgery. LDF has been used previously to evaluate the effects of differing surgical invasiveness. Minimally invasive surgeries lead to earlier recovery of perfusion than conventional techniques (Retzepi et al. 2007). Furthermore, arteries traverse obliquely from posterior in canine and human mandibles (Jeffcoat et al. 1982; Kleinheinz et al. 2005), and releasing incisions in mucosa and periosteum basically affect the revascularization of mucoperiosteal flaps (Mörmann & Ciancio 1977). This is in strong agreement with our findings, which clearly attribute the negative impact of augmentation surgery on microcirculation and wound healing to the standard technique for wound closure applied in control sites without STE: in order to close the flap above the BCP/PEG scaffold, long releasing incisions and incisions into the submucosa were placed, and repeated stripping of the periosteum had to be carried out. Sufficient vascularization in order to allow the influx of stem cells is a precondition for bone healing (Stegen et al. 2015). Therefore, angiogenesis is essential for successful bone regeneration (Glowacki 1998; Kanczler & Oreffo 2008). However, non‐pedicled grafts initially obtain nutrients and oxygen through diffusion from surrounding tissues only (Alberius et al. 1996; Winet 1996). Hence, impairment of perfusion critically affects bone healing (Glowacki 1998; Kanczler & Oreffo 2008). Periosteal vessels are important for osseous blood supply, and mobilization and stripping of the periosteum do not only decrease the blood flow in the mucosa, but also reduce perfusion of the outer cortical bone itself (Kowalski et al. 1996).
The effects of STE exceed sole increases in tissue volume and thickness; hence, the good outcomes of reconstructive surgery after STE are not only attributed to the surplus of tissue, but also to its mechanic, vascular and angiogenic properties as well (Bascom & Wax 2002). Regardless of whether expanders are implanted above or below the periosteum, a dense and mechanically stable connective tissue capsule forms around the device after a retention time of several weeks (Abrahamsson et al. 2009, 2012; Kaner & Friedmann 2011; Tominaga et al. 1993). The capsule is highly vascularized and improves flap viability (Johnson et al. 1993). Higher microvessel capacity and blood flow were found in soft tissue above block grafts, when STE had been carried out in advance. In contrast, perfusion of the overlying tissues stops for 10 days, when grafts are placed without preceding STE (von See et al. 2010). In addition, expanded skin has even been found to express vascular endothelial growth factor (VEGF) (Lantieri et al. 1998). Further, implantation of silicone expanders or resins like polymethylmethacrylate (PMMA) induces a foreign body reaction that depends on expansion speed, surface properties and retention time (Anwander et al. 2007; Wiese 1993; Wiese et al. 2001). Implantation of a non‐expanding PMMA spacer has been shown to induce the formation of a pseudosynovial membrane that could subsequently be used to enclose bone grafts in continuity defects of long bones. Interestingly, the stimulated membrane did not only express VEGF, but other growth factors and osteoinductive factors such as TGF‐ß, vWF and BMP‐2 as well (Christou et al. 2014; Pelissier et al. 2004). Following the principle that therapies that improve tissue vascularization likewise improve healing and formation of bone (Stegen et al. 2015), the connective tissue capsule induced by the implanted expander material may have led to additional beneficial effects on the integration of the osteoconductive BCP/PEG scaffolds.
Conclusions
Preconditioning with STE improved microcirculation and soft tissue healing and optimized the mechanical and biological conditions for bone formation in the applied animal model of vertical augmentation using GBR with alloplastic scaffolds. The good outcome of bone regeneration using the combination of STE and GBR may reduce the need for harvesting of autogenous bone in complex augmentation procedures.
Acknowledgements
We are grateful to Dr. Endre Felszhegy, Semmelweis University, Budapest, Hungary, for supervision of animal care and general anaesthesia, and to Dr. Aart Molenberg, Institut Straumann AG, for the preparation of the PEG membrane. We also thank Mrs. Susanne Haussmann, Witten/Herdecke University, for sectioning the specimens and for the histological and immunohistochemical stainings.
The study was supported by the ITI Foundation for the Promotion of Oral Implantology, Switzerland (Grant 687‐2010), and by Institut Straumann AG, Basel, Switzerland. Institut Straumann AG and Osmed GmbH, Ilmenau, Germany, donated clinical materials. A. F. and D. K. have received lecture and consultancy fees from Osmed. All authors report no conflict of interest. The funding sources were not involved in designing the study protocol; in the collection, analysis and interpretation of data; in the writing of the manuscript; and in the decision to submit the manuscript for publication.
Kaner D, Zhao H, Arnold W, Terheyden H, Friedmann A. Pre‐augmentation soft tissue expansion improves scaffold‐based vertical bone regeneration – a randomized study in dogs. Clin. Oral Impl. Res. 28, 2017, 640–647.
References
- Abrahamsson, P. , Isaksson, S. , Gordh, M. & Andersson, G. (2009) Periosteal expansion of rabbit mandible with an osmotic self‐inflatable expander. Scandinavian Journal of Plastic and Reconstructive Surgery and Hand Surgery 43: 121–125. [DOI] [PubMed] [Google Scholar]
- Abrahamsson, P. , Walivaara, D.A. , Isaksson, S. & Andersson, G. (2012) Periosteal expansion before local bone reconstruction using a new technique for measuring soft tissue profile stability: a clinical study. Journal of Oral and Maxillofacial Surgery 70: e521–e530. [DOI] [PubMed] [Google Scholar]
- Alberius, P. , Gordh, M. , Lindberg, L. & Johnell, O. (1996) Influence of surrounding soft tissues on onlay bone graft incorporation. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontics 82: 22–33. [DOI] [PubMed] [Google Scholar]
- Anwander, T. , Schneider, M. , Gloger, W. , Reich, R.H. , Appel, T. , Martini, M. , Wenghoefer, M. , Merkx, M. & Berge, S. (2007) Investigation of the expansion properties of osmotic expanders with and without silicone shell in animals. Plastic and Reconstructive Surgery 120: 590–595. [DOI] [PubMed] [Google Scholar]
- von Arx, T. , Cochran, D.L. , Hermann, J.S. , Schenk, R.K. & Buser, D. (2001) Lateral ridge augmentation using different bone fillers and barrier membrane application. A histologic and histomorphometric pilot study in the canine mandible. Clinical Oral Implants Research 12: 260–269. [DOI] [PubMed] [Google Scholar]
- Asa'ad, F. , Rasperini, G. , Pagni, G. , Rios, H. F. & Gianni, A. B. (2015) Pre‐augmentation soft tissue expansion: an overview. Clinical Oral Implants Research 3: 12617. [DOI] [PubMed] [Google Scholar]
- Babis, G.C. & Soucacos, P.N. (2005) Bone scaffolds: the role of mechanical stability and instrumentation. Injury 36(Suppl 4): S38–S44. [DOI] [PubMed] [Google Scholar]
- Bascom, D.A. & Wax, K.A. (2002) Tissue expansion in the head and neck: current state of the art. Current Opinion in Otolaryngology Head and Neck Surgery 10: 273–277. [Google Scholar]
- Burkhardt, R. & Lang, N.P. (2010) Role of flap tension in primary wound closure of mucoperiosteal flaps: a prospective cohort study. Clinical Oral Implants Research 21: 50–54. [DOI] [PubMed] [Google Scholar]
- Buser, D. , Dula, K. , Hirt, H. P. & Schenk, R. K. (1996) Lateral ridge augmentation using autografts and barrier membranes: a clinical study with 40 partially edentulous patients. Journal of Oral and Maxillofacial Surgery 54: 420–432 discussion 432‐423. [DOI] [PubMed] [Google Scholar]
- Carroll, W.R. & Esclamado, R.M. (2000) Ischemia/reperfusion injury in microvascular surgery. Head and Neck 22: 700–713. [DOI] [PubMed] [Google Scholar]
- Carter, D.R. , Beaupre, G.S. , Giori, N.J. & Helms, J.A. (1998) Mechanobiology of skeletal regeneration. Clinical Orthopaedics and Related Research 355: S41–S55. [DOI] [PubMed] [Google Scholar]
- Cherry, G.W. , Austad, E. , Pasyk, K. , McClatchey, K. & Rohrich, R.J. (1983) Increased survival and vascularity of random‐pattern skin flaps elevated in controlled, expanded skin. Plastic and Reconstructive Surgery 72: 680–687. [DOI] [PubMed] [Google Scholar]
- Christou, C. , Oliver, R.A. , Yu, Y. & Walsh, W.R. (2014) The masquelet technique for membrane induction and the healing of ovine critical sized segmental defects. PLoS ONE 9: e114122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahlin, C. , Linde, A. , Gottlow, J. & Nyman, S. (1988) Healing of bone defects by guided tissue regeneration. Plastic and Reconstructive Surgery 81: 672–676. [DOI] [PubMed] [Google Scholar]
- Dimitriou, R. , Jones, E. , McGonagle, D. & Giannoudis, P.V. (2011) Bone regeneration: current concepts and future directions. BMC Medicine 9: 66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esposito, M. , Grusovin, M. G. , Felice, P. , Karatzopoulos, G. , Worthington, H. V. & Coulthard, P. (2009) Interventions for replacing missing teeth: horizontal and vertical bone augmentation techniques for dental implant treatment. Cochrane Database Systematic Review 7: CD003607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedmann, A. , Dard, M. , Kleber, B.M. , Bernimoulin, J.P. & Bosshardt, D.D. (2009) Ridge augmentation and maxillary sinus grafting with a biphasic calcium phosphate: histologic and histomorphometric observations. Clinical Oral Implants Research 20: 708–714. [DOI] [PubMed] [Google Scholar]
- Friedmann, A. , Gissel, K. , Konermann, A. & Götz, W. (2015) Tissue reactions after simultaneous alveolar ridge augmentation with biphasic calcium phosphate and implant insertion‐histological and immunohistochemical evaluation in humans. Clinical Oral Investigations 19: 1595–1603. [DOI] [PubMed] [Google Scholar]
- Glowacki, J. (1998) Angiogenesis in fracture repair. Clinical Orthopaedics and Related Research 355: S82–S89. [DOI] [PubMed] [Google Scholar]
- Greenstein, G. , Greenstein, B. , Cavallaro, J. , Elian, N. & Tarnow, D. (2009) Flap advancement: practical techniques to attain tension‐free primary closure. Journal of Periodontology 80: 4–15. [DOI] [PubMed] [Google Scholar]
- Hiltunen, A. , Vuorio, E. & Aro, H.T. (1993) A standardized experimental fracture in the mouse tibia. Journal of Orthopaedic Research 11: 305–312. [DOI] [PubMed] [Google Scholar]
- Jeffcoat, M.K. , Kaplan, M.L. , Rumbaugh, C.L. & Goldhaber, P. (1982) Magnification angiography in beagles with periodontal disease. Journal of Periodontal Research 17: 294–299. [DOI] [PubMed] [Google Scholar]
- Jensen, S.S. & Terheyden, H. (2009) Bone augmentation procedures in localized defects in the alveolar ridge: clinical results with different bone grafts and bone‐substitute materials. International Journal of Oral & Maxillofacial Implants 24(Suppl): 218–236. [PubMed] [Google Scholar]
- Johnson, T.M. , Lowe, L. , Brown, M.D. , Sullivan, M.J. & Nelson, B.R. (1993) Histology and physiology of tissue expansion. The Journal of Dermatologic Surgery and Oncology 19: 1074–1078. [DOI] [PubMed] [Google Scholar]
- Kanczler, J.M. & Oreffo, R.O. (2008) Osteogenesis and angiogenesis: the potential for engineering bone. European Cells and Materials 15: 100–114. [DOI] [PubMed] [Google Scholar]
- Kaner, D. & Friedmann, A. (2011) Soft tissue expansion with self‐filling osmotic tissue expanders before vertical ridge augmentation: a proof of principle study. Journal of Clinical Periodontology 38: 95–101. [DOI] [PubMed] [Google Scholar]
- Kaner, D. , Zhao, H. , Terheyden, H. & Friedmann, A. (2014) Submucosal implantation of soft tissue expanders does not affect microcirculation. Clinical Oral Implants Research 25: 867–870. [DOI] [PubMed] [Google Scholar]
- Kaner, D. , Zhao, H. , Terheyden, H. & Friedmann, A. (2015) Improvement of microcirculation and wound healing in vertical ridge augmentation after pre‐treatment with self‐inflating soft tissue expanders – a randomized study in dogs. Clinical Oral Implants Research 26: 720–724. [DOI] [PubMed] [Google Scholar]
- Kleinheinz, J. , Büchter, A. , Kruse‐Lösler, B. , Weingart, D. & Joos, U. (2005) Incision design in implant dentistry based on vascularization of the mucosa. Clinical Oral Implants Research 16: 518–523. [DOI] [PubMed] [Google Scholar]
- Kostopoulos, L. & Karring, T. (1995) Role of periosteum in the formation of jaw bone. An experiment in the rat. Journal of Clinical Periodontology 22: 247–254. [DOI] [PubMed] [Google Scholar]
- Kostopoulos, L. , Karring, T. & Uraguchi, R. (1994) Formation of jawbone tuberosities by guided tissue regeneration. An experimental study in the rat. Clinical Oral Implants Research 5: 245–253. [DOI] [PubMed] [Google Scholar]
- Kowalski, M.J. , Schemitsch, E.H. , Kregor, P.J. , Senft, D. & Swiontkowski, M.F. (1996) Effect of periosteal stripping on cortical bone perfusion: a laser doppler study in sheep. Calcified Tissue International 59: 24–26. [DOI] [PubMed] [Google Scholar]
- Lantieri, L.A. , Martin‐Garcia, N. , Wechsler, J. , Mitrofanoff, M. , Raulo, Y. & Baruch, J.P. (1998) Vascular endothelial growth factor expression in expanded tissue: a possible mechanism of angiogenesis in tissue expansion. Plastic and Reconstructive Surgery 101: 392–398. [DOI] [PubMed] [Google Scholar]
- Lundgren, S. , Sjostrom, M. , Nystrom, E. & Sennerby, L. (2008) Strategies in reconstruction of the atrophic maxilla with autogenous bone grafts and endosseous implants. Periodontology 2000 47: 143–161. [DOI] [PubMed] [Google Scholar]
- McAllister, B.S. & Haghighat, K. (2007) Bone augmentation techniques. Journal of Periodontology 78: 377–396. [DOI] [PubMed] [Google Scholar]
- McLean, T.N. , Smith, B.A. , Morrison, E.C. , Nasjleti, C.E. & Caffesse, R.G. (1995) Vascular changes following mucoperiosteal flap surgery: a fluorescein angiography study in dogs. Journal of Periodontology 66: 205–210. [DOI] [PubMed] [Google Scholar]
- Mertens, C. , Thiele, O. , Engel, M. , Seeberger, R. , Hoffmann, J. & Freier, K. (2013) The use of self‐inflating soft tissue expanders prior to bone augmentation of atrophied alveolar ridges. Clinical Implant Dentistry & Related Research 28: 12093. [DOI] [PubMed] [Google Scholar]
- Miron, R.J. & Zhang, Y.F. (2012) Osteoinduction: a review of old concepts with new standards. Journal of Dental Research 91: 736–744. [DOI] [PubMed] [Google Scholar]
- Mörmann, W. & Ciancio, S.G. (1977) Blood supply of human gingiva following periodontal surgery. A fluorescein angiographic study. Journal of Periodontology 48: 681–692. [DOI] [PubMed] [Google Scholar]
- Moses, O. , Pitaru, S. , Artzi, Z. & Nemcovsky, C.E. (2005) Healing of dehiscence‐type defects in implants placed together with different barrier membranes: a comparative clinical study. Clinical Oral Implants Res 16: 210–219. [DOI] [PubMed] [Google Scholar]
- Nakayama, Y. , Soeda, S. & Kasai, Y. (1982) The importance of arterial inflow in the distal side of a flap: an experimental investigation. Plastic & Reconstructive Surgery 69: 61–67. [PubMed] [Google Scholar]
- Nkenke, E. & Neukam, F.W. (2014) Autogenous bone harvesting and grafting in advanced jaw resorption: morbidity, resorption and implant survival. European Journal of Oral Implantology 7(Suppl 2): S203–S217. [PubMed] [Google Scholar]
- Nurminskaya, M. & Kaartinen, M.T. (2006) Transglutaminases in mineralized tissues. Frontiers in Bioscience 11: 1591–1606. [DOI] [PubMed] [Google Scholar]
- Pelissier, P. , Masquelet, A.C. , Bareille, R. , Pelissier, S.M. & Amedee, J. (2004) Induced membranes secrete growth factors including vascular and osteoinductive factors and could stimulate bone regeneration. Journal of Orthopaedic Research 22: 73–79. [DOI] [PubMed] [Google Scholar]
- Retzepi, M. , Tonetti, M. & Donos, N. (2007) Comparison of gingival blood flow during healing of simplified papilla preservation and modified Widman flap surgery: a clinical trial using laser doppler flowmetry. Journal of Clinical Periodontology 34: 903–911. [DOI] [PubMed] [Google Scholar]
- Rocchietta, I. , Fontana, F. & Simion, M. (2008) Clinical outcomes of vertical bone augmentation to enable dental implant placement: a systematic review. Journal of Clinical Periodontology 35: 203–215. [DOI] [PubMed] [Google Scholar]
- Rosner, B. (2010) Estimation of sample size and power for comparing two binomial proportions Fundamentals of biostatistics, 381–389. Boston: Brooks/Cole. [Google Scholar]
- Rothamel, D. , Schwarz, F. , Herten, M. , Ferrari, D. , Mischkowski, R.A. , Sager, M. & Becker, J. (2009) Vertical ridge augmentation using xenogenous bone blocks: a histomorphometric study in dogs. International Journal of Oral and Maxillofacial Implants 24: 243–250. [PubMed] [Google Scholar]
- Sager, M. , Ferrari, D. , Wieland, M. , Dard, M. , Becker, J. & Schwarz, F. (2012) Immunohistochemical characterization of wound healing at two different bone graft substitutes. International Journal of Oral and Maxillofacial Surgery 41: 657–666. [DOI] [PubMed] [Google Scholar]
- Schenk, R.K. , Buser, D. , Hardwick, W.R. & Dahlin, C. (1994) Healing pattern of bone regeneration in membrane‐protected defects: a histologic study in the canine mandible. International Journal of Oral and Maxillofacial Implants 9: 13–29. [PubMed] [Google Scholar]
- Schwarz, F. , Jung, R.E. , Fienitz, T. , Wieland, M. , Becker, J. & Sager, M. (2010) Impact of guided bone regeneration and defect dimension on wound healing at chemically modified hydrophilic titanium implant surfaces: an experimental study in dogs. Journal of Clinical Periodontology 37: 474–485. [DOI] [PubMed] [Google Scholar]
- von See, C. , Gellrich, N.C. , Jachmann, U. , Laschke, M.W. , Bormann, K.H. & Rucker, M. (2010) Bone augmentation after soft‐tissue expansion using hydrogel expanders: effects on microcirculation and osseointegration. Clinical Oral Implants Research 21: 842–847. [DOI] [PubMed] [Google Scholar]
- Simon, B.I. , Von Hagen, S. , Deasy, M.J. , Faldu, M. & Resnansky, D. (2000) Changes in alveolar bone height and width following ridge augmentation using bone graft and membranes. Journal of Periodontology 71: 1774–1791. [DOI] [PubMed] [Google Scholar]
- Stegen, S. , van Gastel, N. & Carmeliet, G. (2015) Bringing new life to damaged bone: the importance of angiogenesis in bone repair and regeneration. Bone 70: 19–27. [DOI] [PubMed] [Google Scholar]
- Thoma, D.S. , Dard, M.M. , Halg, G.A. , Ramel, C.F. , Hammerle, C.H. & Jung, R.E. (2012) Evaluation of a biodegradable synthetic hydrogel used as a guided bone regeneration membrane: an experimental study in dogs. Clinical Oral Implants Research 23: 160–168. [DOI] [PubMed] [Google Scholar]
- Tominaga, K. , Matsuo, T. , Kuga, Y. & Mizuno, A. (1993) An animal model for subperiosteal tissue expansion. Journal of Oral and Maxillofacial Surgery 51: 1244–1249. [DOI] [PubMed] [Google Scholar]
- Wiese, K.G. (1993) Osmotically induced tissue expansion with hydrogels: a new dimension in tissue expansion? A preliminary report. Journal of Cranio‐Maxillo‐Facial Surgery 21: 309–313. [DOI] [PubMed] [Google Scholar]
- Wiese, K.G. , Heinemann, D.E. , Ostermeier, D. & Peters, J.H. (2001) Biomaterial properties and biocompatibility in cell culture of a novel self‐inflating hydrogel tissue expander. Journal of Biomedical Materials Research 54: 179–188. [DOI] [PubMed] [Google Scholar]
- Wikesjo, U.M. , Susin, C. , Qahash, M. , Polimeni, G. , Leknes, K.N. , Shanaman, R.H. , Prasad, H.S. , Rohrer, M.D. & Hall, J. (2006) The critical‐size supraalveolar peri‐implant defect model: characteristics and use. Journal of Clinical Periodontology 33: 846–854. [DOI] [PubMed] [Google Scholar]
- Winet, H. (1996) The role of microvasculature in normal and perturbed bone healing as revealed by intravital microscopy. Bone 19: 39S–57S. [DOI] [PubMed] [Google Scholar]


