Abstract
Mammography can be painful and unpleasant, but effective interventions to improve the experience remain scarce. As a first step towards more effective interventions, we aimed to achieve a thorough, contemporary understanding of thoughts, feelings and behaviours which affect and arise from mammography experiences. Research and professional experience suggest that the interaction between client and practitioner may be paramount in determining the quality of a client's experience. Therefore, this study aimed to capture the perspectives of clients and mammography staff from UK breast screening programmes. Thematic analysis of semi‐structured qualitative in‐depth interviews with 22 clients and 18 staff revealed that clients had positive attitudes to breast screening and mostly low knowledge about potential harms. Staff data indicated that some women attend for breast screening under pressure from others. Pain and coping with it were prominent themes, with wide variations in pain experiences. Clients recognised differences in mammographers’ abilities to put them at ease. Staff difficulties included empowering clients within the confines of a taxing technique, and maintaining compassionate care when under strain. Future intervention development should focus on the information and support needs of women prior to the appointment and on effectively training and supporting mammographers to deal with challenging encounters.
Keywords: breast, cancer, pain, patient satisfaction, radiography
1. Introduction
While many women tolerate mammography well (Myklebust, Seierstad, Stranden, & Lerdal, 2009), others find it a painful and unpleasant experience (Poulos & Llewellyn, 2005), to be avoided (Sarma, 2015), or to be tried but not repeated (Whelehan, Evans, Wells, & MacGillivray, 2013). This raises the question of how best to improve the experience, which in turn requires a thorough understanding of its nature and the factors affecting it.
Well‐conducted studies of interventions to improve experiences of the mammography examination are uncommon and tend to focus on pain (Miller, Livingstone, & Herbison, 2008). Recent studies have shown some promise in reducing pain through medical or mechanical means but modest sample and effect sizes and/or feasibility barriers have hampered implementation and impact (de Groot, Branderhorst, Grimbergen, Den Heeten, & Broeders, 2015; Lambertz, Johnson, Montgomery, & Maxwell, 2008). The study by Lambertz et al. produced a statistically significant but clinically small reduction in discomfort by the application of lidocaine gel but this involved application around an hour before mammography and covering with cling film in the interim so is a somewhat inconvenient intervention. The study by de Groot et al. investigated changing the way the amount of compression applied to the breast is calibrated. While the results for pain reduction were promising, the study was preliminary and further work would be needed before the intervention, which would involve equipment modification, could be implemented. Observational studies have identified non‐physical aspects of mammographic practice, largely concerning staff communication and caring skills, which can reduce reported pain and improve client satisfaction (Almog, Hagoel, Tamir, Barnett, & Rennert, 2008; van Goethem et al., 2003). However, while mammography training and culture may acknowledge these findings, they have not been translated into formal interventions.
Relatively few qualitative studies of the mammography experience have been performed in the UK and they have mostly involved specific population subgroups or focussed on particular aspects of the process (Mathers, McKenzie, & Robertson, 2013; Robinson, Hogg, & Newton‐Hughes, 2013; Truesdale‐Kennedy, Taggart, & McIlfatrick, 2011). An exception is a 2003 focus group study of breast screening experiences which highlighted the importance of physical pain and discomfort in mammography, and the need for high‐quality staff with good interpersonal skills (Hamilton, Wallis, Barlow, Cullen, & Wright, 2003). The study by Hamilton et al. provides only limited information on the nature of the mammographer interpersonal skills required to optimise client experience. Compared with other healthcare disciplines, such as nursing and medicine, communication skills and empathy in radiography and mammography have received far less attention in the academic literature. However, research findings indicating that higher levels of empathy demonstrated by healthcare professionals are associated with greater patient satisfaction (Goodchild, Skinner, & Parkin, 2005; Menendez, Chen, Mudgal, Jupiter, & Ring, 2015) may well be applicable in mammography. Definitions of the concept of empathy in healthcare encounters remain somewhat variable but tend to include the ability to detect and understand patients’ feelings and to convey to patients that they have been understood (Batt‐Rawden, Chisolm, Anton, & Flickinger, 2013; Mercer & Reynolds, 2002; Teding Van Berkhout & Malouff, 2016).
Given the continuing lack of effective interventions to improve mammography experiences, we wished to engender a thorough and current understanding of the experience as a first step towards identifying the best targets for intervention. We therefore conducted a qualitative study to explore experiences of mammography from the perspectives of both clients and radiographic staff within the UK breast screening programme. We aimed to examine clients’ and practitioners’ cognitive and emotional responses to the mammography experience, and identify factors which are important in determining good or bad experiences.
2. Methods
2.1. Methodological approach
Individual semi‐structured interviews were used to explore experiences and opinions about mammography in the context of breast screening. Clients and staff were included because the mammography examination is a close dyadic encounter where each partner may affect the responses of the other, and where the insights of staff are seldom captured and disseminated. Individual interviews were preferred over focus groups to reflect the intimacy of the mammography encounter and to access the individual rather than the collective experience.
2.2. Setting
The study took place in population‐based breast screening programmes in the UK. There were three centres in total. The first – local and therefore convenient to the research team in Scotland – serves a population from rural and semi‐rural areas, and a small city. Clients were recruited from this service. Staff members were not recruited from this service because the research interviewer was known to them and it was considered that this might risk inhibition within the interviews. A second Scottish centre with reasonably similar characteristics to the first was therefore included for staff sampling. An inner‐city London centre was added to increase the potential for demographic heterogeneity in the samples. Both clients and staff were recruited from here. Client interviews took place in the screening centre, in the clients’ homes, or in a clinical research facility at the screening location. All staff interviews took place in the screening centres.
2.3. Participants
2.3.1. Breast screening clients
Participants were recruited via the administration teams at two NHS breast screening centres. Study invitation letters were mailed to selected appointment lists of clients. The sampling strategy aimed to include a range of characteristics considered likely to influence perceptions of the experience of mammography: length of time between the mammogram and the research interview, screened on a mobile unit or at a static or hospital‐based site, past breast screening history, age, socio‐economic status and ethnicity. By using the centres’ databases, it was possible to target study invitations to fulfil some of the above sampling criteria. For example invitations were sent to lists of clients booked for screening at different locations. The London centre does not use any mobile screening units but clients were sampled from those attending static units in two different neighbourhoods. In the Scottish centre, the appointments system meant that sampling from women invited to the static centre would recruit those living in the city, whereas sampling from lists booked to the mobile units would recruit women living in the small town where the unit was sited at the time of the study, and from the surrounding villages and countryside. Thus it was straightforward to achieve a mixed sample on such characteristics. A reasonable degree of heterogeneity on factors such as age and socio‐economic status occurred naturally among those who opted into the study and recruitment was simply ceased when it was deemed that a sufficient range across most of the sampling criteria had been achieved.
Clients with abnormal results from the most recent screen were not included because the study aim was to concentrate specifically on standard mammography examinations, not on wider experiences of breast screening. Clients who had attended multiple screens, as identified from the breast screening databases, were included on the assumption that this may indicate that their experiences had been satisfactory. To access the opposite extreme case, specific attempts were made to invite clients whose records indicated they had not sustained their attendance, or who had complained to the service about their experience. Having been approached by the screening service, women opted into the study by returning a reply slip to the researcher with contact details. The researcher then telephoned respondents to arrange interview appointments.
Ethical approval was obtained from the London Bromley NHS Research Ethics Service, Reference 13/LO/1551. Further approval was obtained from the University of St Andrews Teaching and Research Ethics Committee. Local Research & Development office approval was obtained from each participating NHS organisation.
2.3.2. Mammography staff
There are two main subgroups of the radiography workforce carrying out mammography in the UK. The first group consists of radiographers who are registered with and regulated by the Health and Care Professions Council. They complete specialist mammography education at post‐graduate level and are responsible for episodes of patient and client care. Within this group some undertake advanced practice in breast imaging and/or act as trainers for staff wishing to specialise in mammography. Second, assistant radiography practitioners undertake at least 1 year of in‐service training and perform standard mammography under the indirect supervision of registered radiographers. Hereafter, these staff members will be collectively referred to as “mammographers.”
Study invitation letters were passed to staff by their managers. The researcher visited on pre‐arranged dates and all staff who were present in the centre on those dates, who wished to participate, and could be made available were interviewed. There was some purposive selection to achieve variance in age, length of mammography experience, whether or not the participant had had a mammogram herself, ethnicity and type of practitioner. The mechanisms for this were that rotas were lightly manipulated, and the last few recruits were selected, from among the available staff not already interviewed, on grounds of characteristics not already naturally occurring in the sample. For example there was a lack of fortuitous inclusion of mammographers in their 40s so these were then recruited in preference to those in age groups already covered. Despite this, the majority of the mammographers present in the centres on the days in question were recruited. This does not mean, however, that the majority of the workforce was recruited because some would have been working away on mobile or satellite static units on the days in question, as well as some being on leave.
2.4. Data collection
Individual interviews were conducted by a single researcher and were face‐to‐face except for one by telephone. The topic guides, designed in consultation with an experienced qualitative researcher, are available as Files S1 and S2. The researcher herself has a background in mammography, which was known to many of the staff participants but was not revealed to the clients. A minority of the mammographers were acquainted with the researcher, none closely. All participants were assured that the researcher, a university employee, was independent of the screening service and that their names would not be used. Written informed consent was taken before the start of each interview and each participant was allocated a pseudonym, which was then converted to a different, randomly generated number for the report, to achieve fully robust anonymisation. The interviews were digitally audio‐recorded and transcribed verbatim by a professional service. The transcripts were imported into NVivo10 (QSR International Proprietary Company Ltd).
The study was carried out after the introduction of the latest breast screening information leaflet (Forbes & Ramirez, 2014), entitled “NHS breast screening: helping you decide” (Informed Choice about Cancer Screening, 2013) in England, and entitled “Breast Screening: helping you decide” in Scotland (NHS Health Scotland, 2015). The two versions have only a few minor differences.
2.5. Analysis
Data were managed according to the “framework” method (Ritchie, Lewis, McNaughton, & Ormston, 2013). Initial coding, or “first cycle” coding of the transcripts, as defined by (Saldana, 2013) was carried out, using NVivo, by the same researcher who had conducted the interviews. An initial thematic framework (Spencer, Ritchie, Ormston, O'Connor, & Barnard, 2013) was developed in consultation with a second, more experienced, researcher. The initial thematic framework was then refined through data indexing and sorting. Material consisting of purely procedural accounts was left aside and the remaining content was exported to Microsoft Excel for further interpretation and development of the final thematic structure. The analysis was led by the client data with their themes then being explored further through the mammographer data. Additional themes were identified within the mammographer data which were very specific to the staff and therefore were not present in the client data, for example relating to professional career issues. These have not been included in the report because of their lesser direct relevance to the client experience. The analysis was initially inductive but became more deductive as themes started to emerge. In particular, where relevant, the analysis of the data on what women bring to the mammography and screening experience was informally underpinned by comparison with published models of informed choice and decisional conflict (Mullen et al., 2006).
3. Results
Forty transcripts were available for analysis – 22 clients and 18 staff. Mean length of the client interviews was 28 min (range 16–41), and of mammographer interviews was 44 min (range 28–56). There was no attempt to link a particular client to the individual mammographer who had examined her. The clients’ characteristics are shown in Table 1 and the mammographers’ in Table 2. For the mammographer sample, ages have been banded and ethnic classifications broadened to protect participants’ identities, given the small population. By purposively sampling from the available pools, we achieved heterogeneity across most of the sampling categories in both groups, including client socio‐economic status. Ethnic diversity in the client sample was low and more reflective of the Scottish than the London population, although the intent of our sampling was variety rather than representation. In addition to one non‐re‐attender, we recruited one client who had complained to the service of a poor standard of care.
Table 1.
Participant characteristics – clients (n = 22)
| Age | Years |
| Range | 50–72 |
| Mean | 59.45 |
| Standard deviation | 6.78 |
| Screening history | n |
| First attender | 7 |
| Second‐time attender | 3 |
| Multiple attender | 12 |
| Screen‐to‐interview interval | n |
| Minutes | 6 |
| Days | 7 |
| Weeks (after normal result) | 6 |
| More than 2 years (but before next invitation) | 2 |
| More than 3 years (non‐re‐attender) | 1 |
| Screening site | n |
| Mobile (associated with rural place of residence) | 5 |
| Static (associated with urban place of residence) | 17 |
| Index of multiple deprivation decile (1 = most deprived) | n |
| 1 | 5 |
| 2 | 4 |
| 5 | 1 |
| 6 | 2 |
| 7 | 3 |
| 8 | 2 |
| 9 | 3 |
| Missing data | 2 |
| Nationality/ethnicity | n |
| White British or White Scottish | 20 |
| African | 1 |
| Afro‐Caribbean | 1 |
Table 2.
Participant characteristics – staff (N = 18)
| Age | n |
| 26–30 | 3 |
| 31–35 | 2 |
| 36–40 | 1 |
| 41–45 | 2 |
| 46–50 | 3 |
| 51–55 | 1 |
| 56–60 | 6 |
| Years’ experience in mammography (associated with age), n = 16; two additional still in post‐graduate specialist training | Years |
| Range | 4–24 |
| Mean | 10.69 |
| Standard deviation | 6.16 |
| Practitioner type | n |
| Standard registered practitioner | 9 |
| Advanced practitioner | 4 |
| Clinical trainer | 3 |
| Assistant practitioner | 2 |
| Had undergone mammography herself | n |
| No | 8 |
| Yes | 10 |
| Nationality/ethnicity | n |
| White British | 11 |
| British mixed | 1 |
| Black (European, Caribbean or African) | 4 |
| Other non‐European | 2 |
Forty‐eight additional clients returned the study opt‐in slip but were not recruited, either because an interview appointment could not be arranged, or because the sampling criteria they would have fulfilled were already sufficiently saturated. In the case of the mammographers, the samples represented about one‐third to one quarter of the total staff.
At the broadest level, the data formed two themes – first concerning what the clients brought to the experience, and second how they responded to the experience. The main themes and subthemes are shown in Fig. 1. Participant identifiers in the text below are prefixed by C for client and M for mammographer.
Figure 1.
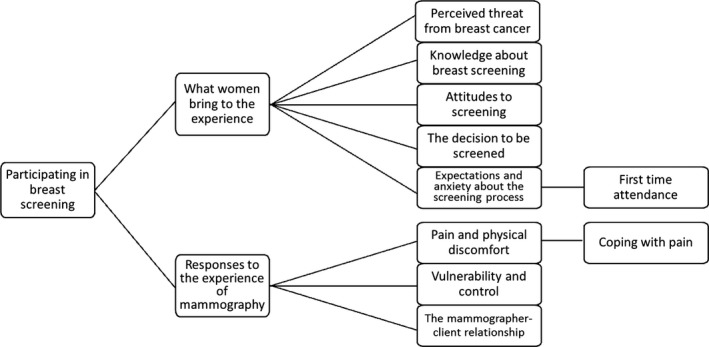
Thematic tree
3.1. What women bring to the experience of being screened
3.1.1. Knowledge about breast screening
There was considerable variation in participants’ knowledge about breast screening and in the use they had made of the information leaflet provided with their screening invitations. Most women understood that mammographic screening aims to detect breast cancer early to improve the chances of survival. Several women were aware of the possibility of false positive results and the potential risk of mammography inducing a cancer. Others could not name any risks of screening. Women had mostly either skimmed the information leaflet or not read it at all. Only one first‐time client said she had read it thoroughly and could provide an explanation of the concept of overdiagnosis.
C82: Do you know what, I didn't [read the leaflet].
C53: I don't sit line by line. I tend to skim all the different bits, I mean there's a lot of information you get and I get bored reading it all after a while.
C63: I know that there have – it has been questioned at times whether it's worth screening. I know that sometimes there's false positives and there might be – if you were screened a lot – is there the possibility that that actually may cause cancer?
C71: I did read in the literature that they can sometimes find little deposits that don't cause you – might not cause cancer but might cause cancer if they're in the milk ducts – this is the way I understood it. And they would call you in to discuss options at that time. There's a possibility that you might have to make decisions that you wouldn't otherwise have to make.
Mammographers tended to believe that few clients read and fully understand the information leaflet and while they recognised the importance of their own role in explaining breast screening and the mammography procedure, they felt that their capacity to rectify all suspected knowledge deficits was somewhat limited. This was not only because of the short screening appointment times but also because of difficulty knowing how well‐informed individual clients are.
M53: I would like to think that we give clear concise instructions but they don't read the letter.
M64: They don't ever say to you, I didn't really understand the information letter.
M81: Well we've looked at the leaflet we send out and I think it's a little bit better than it used to be but the only trouble is I'm quite certain a lot of women come, having read their appointment and not read the leaflet at all ….so it's the initial explanation ‐ it becomes very important, as it is anyway.
Staff also noted an awareness of negative news media coverage of breast screening but generally did not see this as a major issue for their clients. They did, however, sometimes feel affronted by some of the coverage, perhaps partly because it can call into question the worth of their work but also because of their own anticipated feelings in the event of being diagnosed with breast cancer.
M59: Every so often it rears its ugly head about having unnecessary operations and that does annoy me because if somebody turned round to me and said, “You have cells that might be cancerous, will we wait and see or will we take it out?,” what are you going to say, “No, no, I'll wait and see”? Yes, take it out, or take it off, I don't care. So to turn round, and assuming its males that write these articles, and say these are unnecessary operations, I think is outrageous.
3.1.2. Perceived threat from breast cancer
Most of the participants perceived the threat from breast cancer to be substantial, in terms of both its frequency and severity. This was largely fed by experience of friends or family members having breast or other cancers, as well as media coverage. Furthermore, confidence in their skills to detect breast abnormalities themselves was low.
C90: I've had five friends with breast cancer and two have died.
C84: You just never know; maybe there's something that you might not pick up at all, you know, if you're having a shower or anything.
Mammographers sometimes recognised clients’ perceived susceptibility to breast cancer as a factor in overcoming the barrier of aversion to the procedure:
M64: Obviously we get women who don't really want to be there but they come ‘cause a relative has been diagnosed with cancer and they think that maybe they should.
3.1.3. Attitudes to screening
Unsurprisingly for a sample of attenders, attitudes to screening were overwhelmingly positive, aside from the actual mammogram. Belief in the value of early detection and the effectiveness of the test was high and a “better safe than sorry” approach prevailed. Some participants felt grateful for the provision and felt that it would be churlish or irresponsible to refuse the opportunity to be screened.
C75: If they get it in reasonable time they can ‐ you won't live forever but they can prolong your life a few more years.
C60: If anything's developing inside me over the three years that it takes, the mammogram will show it.
C56: I just think it's better to be safe than sorry. …….. I just feel if there's anything that's going to help diagnose ‐ you know ‐ the first stages, you're better to go ahead and get that done.
C84: I think if somebody want [sic] to say, we'll come ‐ you know ‐ we want to check, to see if there might be anything, why wouldn't you want to turn up because, and it's time wasting as well; somebody else could be in your slot. If somebody's expecting you and you don't turn up and then it's sort of a snowball effect if you know what I'm saying.
There was a small amount of data from the mammographers pointing to variation in attitudes to screening, and to variable ability to withstand an unpleasant experience of screening, according to socio‐economic status or education level.
M80: They [meaning relatively affluent women] are used to screening, they're used to having things done and having that kind‐of healthy kind of lifestyle and promoting healthy attitudes and behaviours.
M88: Whereas you get women that come on that maybe don't know a lot about it, they haven't been before, they maybe think that if they get breast cancer they're gonna die next week and things. And if they have a bad experience they're probably not gonna come back.
3.1.4. The decision to be screened
There were signs that women had weighed up potential benefits of screening, such as early detection or reassurance, against the disadvantages, such as risk of inducing cancer or the unpleasantness of the procedure.
C65: What's worse, the fear of there being something and it not being found or the fear of it creating something?
C55: Even though it is uncomfortable I still would go, you know. It's just, I don't know, just as I say, for peace of mind, you know.
Some of the mammographer interviews, however, indicated that women were not always comfortable with their decisions to attend for mammography. Mammographers had experienced episodes, particularly with clients lacking good English language skills, or with learning disabilities, where women had seemed to be under pressure from others to attend. This was a source of strain for the mammographers as well as for the clients.
M73: When carers are bringing people along with physical disabilities, and mental disabilities, you know, is it an informed choice, have they actually consented to this?
M80: My worst experience was somebody with a language difficulty and it was clear to me that she definitely did not want to have a mammogram. She was new to the country, she didn't speak any English. However, her husband came and he was interpreting for her and his words were, ‘What's the problem? You're a woman, she's a woman, she has to have it done.’ And at the time, I didn't feel I had the skills necessary to be able to countermand that in any way, whereas nowadays I would deal with it differently. But at the time I ended up doing the mammos and felt very uncomfortable about it. It was……. I felt bullied into doing it.
M83: We've actually incurred lately quite a few situations where women came in and they said ‘My GP said to me that I have to have a mammogram or I can't belong to this practice any more’.
The above examples illustrate situations where mammographers have doubts about whether they really have informed consent from clients but feel they have no choice but to proceed. On other occasions, vulnerable clients show overt signs of withholding consent to the mammographic procedure itself and this provides a clear justification for mammographers to terminate the process without fear of being seen as infringing a woman's right to be screened:
M76: For a woman who's got a learning disability I always make sure that the trainees understand we have to talk to the woman and not to the carer and that we have to try and ascertain whether the woman understands or not and as long as she's compliant that's a kind of reasonable indication that she does understand and is willing to participate. If she says no and pulls away then she obviously doesn't want to have it done”.
3.2. Expectations and anxiety about the screening process
Some of the women stated that they did not experience any anxiety about attending. Where clients did mention feeling anxious, the perceived source of this was either the expected unpleasantness of the mammogram or the possibility of a cancer being present. The reputation of mammography as a painful procedure was articulated frequently. Some women said that they would play down the pain in order not to deter other women from attending.
C82: Practically everyone that you speak to who has previous experience of it finds it an unpleasant thing.
C73: A friend of mine from the village had come out and said, “That was bloody sore”.
C56: I wouldn't like to say pain to put them off. [This was from a participant who, in the interview, described the mammogram as quite painful.]
Mammographers were aware of an association between expected and actual pain but also that pain is not an inevitable consequence of expecting it, and that their own practice can be crucial in breaking this link.
M64: I think some ladies are expecting it to be painful and no matter what you do they will find it painful.
M53: Somebody can come in who is really nervous, really scared, been put off by others who have had it and then once I've explained the procedure and carried out the procedure the client then says, ‘Is that all it is?’.
3.2.1. First‐time attendance
A number of women identified that either they or others had not been well prepared for their first experience of mammography and some of the mammographers highlighted the same issue. Several of the clients and one of the mammographers directly suggested a possible intervention to address this, namely a face‐to‐face discussion prior to the mammography appointment to provide fuller information about the procedure.
C86: She came and got me after I got changed and said, ‘Right just put one breast under this machine’, and the machine got closed on it like a bit of a sandwich, a breast sandwich it was. And I thought, this is a bit sore. I wasn't expecting that. You know, I thought this is totally unlike what I've seen on the television, so it was totally what I was not expecting at all.
C68: I don't know whether there could ever be, you know, a personal one‐to‐one before you went. I mean, I know you can always go and get information but, you know, if that was the norm that the first thing was an interview with someone or just a friendly meeting with someone just to explain, then yes, that would've been quite welcome.
M64: Obviously the first timers are very anxious and nervous; they don't know what's gonna happen, and they're really uptight. You know, their shoulders are up and you just can't get them to relax into the machine.
3.3. Responses to the experience of mammography
3.3.1. Pain and physical discomfort
Women's descriptions of the level of pain from mammography were mostly related to the breast compression. The descriptions, elicited purely from open‐ended questions about the sensations experienced during mammography, ranged from not feeling pain at all to struggling to tolerate the pain during breast compression. Our two “extreme case” participants, one who had not re‐attended after her first screen and one who had complained to the service of a poor experience on various counts, both found the mammogram very painful, whereas pain was generally low or absent among the multiple attenders happy with the service. However, it is not appropriate to infer any reasons for the variation in pain level within this small sample, given the complex nature of pain in general and the wide range of technical, physiological and psychological factors thought to affect pain in mammography. Of the two participants who described the most extreme pain, only one was dissatisfied with the standard of care provided by the mammographer.
A few clients mentioned discomfort to various parts of the rib cage. Only two clients described pain persisting after the mammogram. One of them was interviewed immediately after the examination and could still feel pain in her breast and the other, interviewed the next day, felt tender over her sternum. The awkwardness of the position was mentioned several times but was a secondary concern among these clients, all of whom were able‐bodied apart from one requiring walking sticks and two with mild musculoskeletal problems. Several clients perceived that the mammographer was adjusting her technique to make them more comfortable, while the mammographers described barriers to successful and comfortable positioning.
C75: It wasn't horrendous; there was no pain ‐ a slight pinch, shall we say, that's all.
C81: I got to the point where I just thought, “I can't, you know I really can't take this anymore” because I know they have to compress the breast but I just thought, when is she going to stop this? It was really, really painful.
C66: The radiographer was very good at repositioning for height and for comfort, I think and you know when it was the sideways one and my arm was over and so on you know she placed it very carefully and then she actually went and she moved the positioning of the machine a little bit and I suppose the result of that is it made it more comfortable.
M62: Yes, if the shape is like a protruding chest, I know that when I do the oblique I will feel the ribs, I will come really close to the ribs and I have to say to the patient, “Sorry, I have to push at the back at the same time” and then I can feel [winces] that it is not comfortable.
Coping with pain
Women's coping mechanisms for the physical discomfort of the mammogram included stoicism, thinking of it as a means to an important end, and humour.
C82: Well I was quite anxious when she was setting me up for the first slide and I thought, ‘Right, okay, I'm just going to have to grit my teeth and get on with it,’ and I was determined just to sort of put up with it.
C84: You can put up with it if it's going to help.
C80: I said to her, ‘Men don't have to go through this sort of thing, I mean in any other way…. they don't get it squashed in the thing’. And we had a little laugh about that, so. Because it was painful, I was trying to take my mind off of it.
The mammographers recognised women's stoicism and related it to their motivation to be screened. Although they also acknowledged women's use of humour as a coping mechanism, that very humour, along oft‐repeated lines, can be a test of their own coping mechanisms.
M83: If they really want to do it they will grin and bear it.
M76: Some of my colleagues get really bugged with the women who always say it must have been a man that invented this, and, you see, early on I decided that I was not going to let that bug me, so I just say to them, ‘I can prove it wasn't. Do you know a man that can multi‐task? I'm asking you to do three things at once. Do you think a man could actually have invented that?’, you know, and that kind of makes them laugh and takes the sting out of it.
3.3.2. Vulnerability and control
Clients often expressed feelings of vulnerability or lack of control over the situation while mammographers expressed contradictory thoughts on the issue of power. They expressed the importance of allowing the client to feel in control but also recounted episodes when they had taken an authoritarian approach to get the job done. This exemplified the frequently encountered challenge of balancing the clinico‐technical demands of the examination, and the limited time available, with the emotional wellbeing of the client.
C81: You feel very vulnerable as well because you're standing there topless and I know it's another lady that you're with but you just sort of feel very vulnerable.
C55: They sort of more or less manipulate you into what position they want you to be in and whether you're comfortable with that or not you know that's the way that you have to be.
C90: I kind of wanted to help; it's a bit silly, and I said ‘Do I put it there?’ and she said ‘No, no, no I'll do it’, and I thought oh okay, so I'll just be completely passive and I felt vaguely foolish that I'd kind of, sort of intervened in the process about who's controlling what at that point
M64: (quoting herself) Don't try and help me, I'll just tell you what to do, don't help me because if you try and help me that makes it far more difficult for both of us.
M76: If they start talking about sore shoulders and stuff you say, ‘Right, okay, I've got a couple of tricks to deal with that but you need to keep me right’, and you need to remember to say to them, ‘Now is that okay on your shoulder?’ because they've got to trust you, that you're not going to hurt them.
3.3.3. The mammographer–client relationship
Clients placed considerable importance on whether the mammographer put them “at ease.” While some highlighted the value of procedural explanations, the mammographer's manner was a bigger issue for the clients than what was said, and was a key factor in making an unpleasant experience acceptable.
C56: Some of them put you at ease and some of them are quite clinical.……just, you know, they don't chat away to you. It's just a job ‐ do this, do that ‐ you know.
C56: You don't mind going through these kinds of things when someone's nice to you.
C81: Both of them introduced themselves, both of them told me what they were going to do, but the way that the second one did it was much kinder, maybe, if that's the right word.
Some clients, however, were comfortable with a cooler approach, and some of the mammographers described occasions when their attempts at friendliness had been rejected. They also highlighted the importance and the challenge of being able to recognise the best approach to take with an individual client.
M80: She actually might want me to just shut up but I think I'm doing a good thing because I'm telling her everything that's happening.
M76: Some people [mammographers] don't have, they just don't pick up the messages, the body languages from who they're talking to, or not as well as they could do perhaps.
M88: If there's a woman sat there, and you can tell she's really, really nervous, you reassure her……………………………. I kind of ask them if there's one particular thing that they are nervous about, or has there been an experience in the past, or something.
The effects of the clients’ behaviour on the feelings of the mammographer were sometimes at issue, as well as vice versa, and clashes between the emotions of the two were highlighted in some of the mammographer interviews.
M59: Somebody who….is so abrupt and rude and aggressive towards you, I find quite difficult to deal with. I feel myself getting defensive.
M70: Having the bad experience with a lady, say first thing in the morning, can throw you off the whole day and so you end up being on that defensiveness the rest of the day and so you don't know how many other ladies you've give a bad experience because of that.
The importance of empathy to both groups of participants was clear, although the word itself was seldom used.
4. Discussion
A substantial section of our findings concerns factors surrounding the decision to attend for breast screening. This was a more prominent theme than expected but is considered important because of the likely interaction between the attitudes and experiences women bring to the appointment and the way they experience the episode. In addition, if practitioners perceive that their clients are not necessarily making an informed choice to be screened, this can be professionally problematical and therefore stressful. Knowledge and attitudes, and whether behaviour is in line with these, are widely described as components of informed decision‐making (Hersch et al., 2014; Jepson, Hewison, Thompson, & Weller, 2005; Mullen et al., 2006; Reder & Kolip, 2015). Levels of knowledge about the potential harms of screening were mostly low among our participants but, unsurprisingly for a sample of attenders, they did not express dissatisfaction with their knowledge about screening. Considerable attention has been paid in recent years to presenting balanced and honest details about the potential for harm as well as benefit from breast screening in a way that is palatable to eligible women (Forbes et al., 2014) but the women in our study made limited use of the information leaflet provided. It has recently been shown that an information leaflet can increase knowledge and understanding of overdiagnosis in breast cancer screening but that study did not assess the extent to which women might read such a leaflet when not specifically required to do so for research purposes (Hersch et al., 2015). Women's satisfaction with their levels of knowledge about screening may be as important as levels of actual knowledge, because providing the information people want can help in reducing anxiety, as well as in making decisions (Jepson, Hewison, Thompson, & Weller, 2007). Furthermore, it may be burdensome to expect all invitees to consider detailed information on all aspects of breast screening (Entwistle et al., 2008). However, our data imply that more effective ways of imparting knowledge about screening are still needed and this is discussed further below.
The only wish for greater knowledge expressed by participants referred to the time of first attendance and was for more information about the mammography procedure itself. It was clear that the precise nature of the examination had caused a degree of shock to some, in line with previous qualitative findings (Hamilton et al., 2003). This may partially account for the higher screening drop‐out rate observed after first attendances (Maxwell et al., 2013). Screening mammography appointments are generally around 5 minutes long in the UK and although the importance of the practitioners explaining the procedure to the clients is well‐recognised (Shrestha & Poulos, 2001), this explanation usually takes place within the examination room itself and is severely time‐limited. There may be a place for more effective communication of the nature of the mammography procedure prior to attendance, both to prepare women better for what actually happens and to address anxieties arising from peer accounts of painful experiences. Intervention at this stage could also potentially help to support informed choice. Improved communication about the nature of mammography and the potential benefits and harms of screening might ideally be achieved through a one‐to‐one discussion with a suitably qualified person prior to the due date of the first screen. This would enable questions to be answered and difficult concepts to be explained in a tailored fashion. However, such an intervention would need careful development and testing, including an assessment of the resources required and the feasibility of providing them. A randomised controlled trial in Spain has shown that a nursing intervention involving additional support on arrival for the screening appointment and during the mammogram can reduce reported mammographic pain (Fernández‐Feito et al., 2015). However, the findings may not be generalisable to the UK because of differences in mammographer training. Also, the cost of the intervention, as tested, would be high.
Although the clients we interviewed were comfortable with their decisions to be screened, we found evidence from the mammographer interviews that some women, especially those with particular vulnerabilities such as linguistic challenges or cognitive disability, attend under pressure from others. This is concerning, causes strain for staff as well as clients, and requires attention. Women who feel coerced into attending for screening might be more likely to find the experience of the mammogram itself difficult to tolerate, because of their unease with the situation. Thus coercion may be relevant as a potential determinant of the examination experience, as well as being a problem in itself.
The question of pain in mammography has been much rehearsed in the literature over many years. Our findings support existing contentions that there is considerable variation in the pain experienced during mammography (Davey, 2007), and that pain can act as a deterrent to screening participation (Whelehan et al., 2013). One strategy shown to help reduce perceived pain and discomfort is for mammographers to enable women to feel that they are in control, as far as possible (van Goethem et al., 2003; Poulos & Llewellyn, 2005). While the mammographers believed that empowering clients was important, they sometimes experienced limitations in the extent to which it was feasible and found themselves taking a more authoritarian approach. Two recent papers based on a qualitative dataset from mammographer focus groups have explored beliefs, values and decision‐making by mammographers in applying compression to the breast (Murphy et al., 2015; Nightingale, Murphy, Robinson, Newton‐Hughes, & Hogg, 2014). In common with our study, both these analyses highlighted the tension between the technical and the caring demands of the mammography examination.
Our data support previous findings that the interpersonal skills of the mammographers are crucial in determining quality of client experience (Barr, Giannotti, van Hoof, Mongoven, & Curry, 2008; Baskin‐Smith, Miaskowski, Dibble, Weekes, & Nielsen, 1995; Engelman, Cizik, & Ellerbeck, 2005; Mathers et al., 2013). We have further identified that mammographers’ ability to care compassionately for clients may be impeded by their reactions to clients’ own behaviour. This reciprocity is unsurprising but it highlights the need for mammography staff to be effectively trained to manage their feelings when confronted with challenging behaviour. Methods for developing communication and relational skills in the radiography workforce are a neglected topic in the academic literature. Some of our results indicate that empathic communication is valued by clients and mammographers alike. In view of evidence that training programmes can be effective in enhancing empathic skills in healthcare professionals (Batt‐Rawden et al., 2013; Pehrson et al., 2016; Teding Van Berkhout & Malouff, 2016), consideration should perhaps be given to expanding this area within radiography and mammography education.
The main strengths of our study are that it involved a heterogeneous sample and included mammographers as well as clients. While there has been one previous qualitative study with participation from both mammography clients and staff (Morris, 2015), only two mammographers were interviewed for that study. Recently, a broad‐based sample of mammographers formed the basis of two analyses but the study differed from ours by using a focus‐group design, not including clients, and exploring compression behaviours specifically (Murphy et al., 2015; Nightingale et al., 2014). In our study, the inclusion of clients who had attended multiple screens provided data comparing different mammography episodes, helping to elucidate what is most important to clients in making the experience as good as it can be. The staff interviews provided indirect access to a wider range of client experiences, as well as exposing some of the challenges staff face in providing good experiences for their clients.
The researcher perspective was a significant potential limitation of this study because the interviews and the analysis were carried out by a single researcher with a background in mammography. Existing views and prejudices could be prone to confirmation bias while important themes could be missed because of seeming too obvious to the researcher. Conversely, unexpected data might make more of an impact on the researcher and therefore be overemphasised. The steps taken to address reflexivity and minimise bias were to use mostly open questions in the interviews, to discuss the analysis with a more experienced researcher with no experience of mammography, to keep a reflective diary to record and address reactions to the data, and simply to try to put preconceived ideas aside and keep as neutral a stance as possible, sometimes known as “bracketing” (Taylor, 2013).
5. Conclusions
Our study has reinforced the continuing need to address the lack of effective interventions to improve the wellbeing of women participating in mammographic screening. Novel approaches to conveying information in advance of the appointment are required, both to prepare women for the experience and to facilitate informed choice. Formal interventions which optimise the ability of staff to provide the best standards of supportive care during mammography and to cope effectively with emotionally charged encounters and with ethical dilemmas around consent should be developed. In the meantime, mammography educators, managers and practitioners must continue to strive for excellence in communication between staff and clients, to address informed choice and consent as well as physical and psychological wellbeing in relation to the examination.
Acknowledgements
We gratefully acknowledge advice on the study design from Professor Mary Wells, University of Stirling. We appreciate the support of the administrative and radiographic staff in the study centres and we particularly thank all the clients and mammographers who took part in the study. We are also grateful to the College of Radiographers Industrial Partnership Scheme (http://www.sor.org/about-us/awards/corips-research-grants) for funding the study. The funding body provided minor comments on the original proposal but took no other part in the design or conduct of the study. The reviewers’ thorough and constructive feedback on the initial manuscript is greatly appreciated.
Disclosure
The authors declare that they have no competing interests.
Author contributions
PW was responsible for conceiving and designing the study, collecting and analysing the data, and writing the manuscript. AE and GO contributed to the design of the study and edited the manuscript for important intellectual content. GO contributed to the data analysis. All authors have approved the final version of the manuscript.
Supporting information
Whelehan, P. , Evans, A. and Ozakinci, G. Client and practitioner perspectives on the screening mammography experience. European Journal of Cancer Care. 2017;26:e12580 https://doi.org/10.1111/ecc.12580
References
- Almog, R. , Hagoel, L. , Tamir, A. , Barnett, O. , & Rennert, G. (2008). Quality control in a national program for the early detection of breast cancer. Women's satisfaction with the mammography process. Womens Health Issues, 18, 110–117. [DOI] [PubMed] [Google Scholar]
- Barr, J. K. , Giannotti, T. E. , van Hoof, T. J. , Mongoven, J. , & Curry, M. (2008). Understanding barriers to participation in mammography by women with disabilities. American Journal of Health Promotion, 22, 381–385. [DOI] [PubMed] [Google Scholar]
- Baskin‐Smith, J. , Miaskowski, C. , Dibble, S. L. , Weekes, D. , & Nielsen, B. B. (1995). Perceptions of the mammography experience. Cancer Nursing, 18, 47–52. [PubMed] [Google Scholar]
- Batt‐Rawden, S. A. , Chisolm, M. S. , Anton, B. , & Flickinger, T. E . (2013) Teaching empathy to medical students: An updated, systematic review. Academic Medicine, 88, 1171–1177. [DOI] [PubMed] [Google Scholar]
- Davey, B. (2007). Pain during mammography: Possible risk factors and ways to alleviate pain. Radiography, 13, 229–234. [Google Scholar]
- Engelman, K. K. , Cizik, A. M. , & Ellerbeck, E. F. (2005). Women's satisfaction with their mammography experience: Results of a qualitative study. Women and Health, 42, 17–35. [DOI] [PubMed] [Google Scholar]
- Entwistle, V. A. , Carter, S. M. , Trevena, L. , Flitcroft, K. , Irwig, L. , McCaffery, K. , & Salkeld, G. (2008). Communicating about screening. BMJ, 337, 789–791. [DOI] [PubMed] [Google Scholar]
- Fernández‐Feito, A. , Lana, A. , Cabello‐Gutiérrez, L. , Franco‐Correia, S. , Baldonedo‐Cernuda, R. , & Mosteiro‐Díaz, P. (2015). Face‐to‐face information and emotional support from trained nurses reduce pain during screening mammography: Results from a randomized controlled trial. Pain Management Nursing, 16, 862–870. [DOI] [PubMed] [Google Scholar]
- Forbes, L. J. , & Ramirez, A.‐J ; The Expert Group on Information About Breast Screening (2014). Offering informed choice about breast screening. Journal of Medical Screening, 21, 194–200. [DOI] [PubMed] [Google Scholar]
- Forbes, L. J. L. , Ramirez, A. J. , Archer, M. , Cooke, J. , Coulter, A. , Dewar, J. A. , … & Wilson, R. M. (2014). Offering informed choice about breast screening. Journal of Medical Screening, 21, 194–200. [DOI] [PubMed] [Google Scholar]
- van Goethem, M. , Mortelmans, D. , Bruyninckx, E. , Verslegers, I. , Biltjes, I. , van Hove, E. , & de Schepper, A. (2003). Influence of the radiographer on the pain felt during mammography. European Radiology, 13, 2384–2389. [DOI] [PubMed] [Google Scholar]
- Goodchild, C. E. , Skinner, T. C. , & Parkin, T. (2005). The value of empathy in dietetic consultations. A pilot study to investigate its effect on satisfaction, autonomy and agreement. Journal of Human Nutrition and Dietetics, 18, 181–185. [DOI] [PubMed] [Google Scholar]
- de Groot, J. E. , Branderhorst, W. , Grimbergen, C. A. , Den Heeten, G. J. , & Broeders, M. J. M. (2015). Towards personalized compression in mammography: A comparison study between pressure‐ and force‐standardization. European Journal of Radiology, 84, 384–391. [DOI] [PubMed] [Google Scholar]
- Hamilton, E. L. , Wallis, M. G. , Barlow, J. , Cullen, L. , & Wright, C. (2003). Women's views of a breast screening service. Health Care for Women International, 24, 40–48. [DOI] [PubMed] [Google Scholar]
- Hersch, J. , Barratt, A. , Jansen, J. , Houssami, N. , Irwig, L. , Jacklyn, G. , … & McCaffery, K . (2014). The effect of information about overdetection of breast cancer on women's decision‐making about mammography screening: Study protocol for a randomised controlled trial. BMJ Open, 4 [Online] Available from: http://bmjopen.bmj.com/content/4/9/e006016.full [last accessed 14 September 2016]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hersch, J. , Barratt, A. , Jansen, J. , Irwig, L. , McGeechan, K. , Jacklyn, G. , Thornton, H. , Dhillon, H. , Houssami, N. , & McCaffery, K. (2015). Use of a decision aid including information on overdetection to support informed choice about breast cancer screening: A randomised controlled trial. The Lancet, 385, 1642–1652. [DOI] [PubMed] [Google Scholar]
- Informed Choice about Cancer Screening (2013). NHS breast screening: Helping you decide. Available from: https://www.gov.uk/government/publications/breast-screening-helping-women-decide [last accessed 25 January 2016].
- Jepson, R. G. , Hewison, J. , Thompson, A. G. H. , & Weller, D. (2005). How should we measure informed choice? The case of cancer screening. Journal of Medical Ethics, 31, 192–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jepson, R. G. , Hewison, J. , Thompson, A. , & Weller, D. (2007). Patient perspectives on information and choice in cancer screening: A qualitative study in the UK. Social Science and Medicine, 65, 890–899. [DOI] [PubMed] [Google Scholar]
- Lambertz, C. K. , Johnson, C. J. , Montgomery, P. G. , & Maxwell, J. R. (2008). Premedication to reduce discomfort during screening mammography. Radiology, 248, 765–772. [DOI] [PubMed] [Google Scholar]
- Mathers, S. A. , McKenzie, G. A. , & Robertson, E. M. (2013). ‘It was daunting’: Experience of women with a diagnosis of breast cancer attending for breast imaging. Radiography, 19, 156–163. [Google Scholar]
- Maxwell, A. J. , Beattie, C. , Lavelle, J. , Lyburn, I. , Sinnatamby, R. , Garnett, S. , & Herbert, A. (2013). The effect of false positive breast screening examinations on subsequent attendance: Retrospective cohort study. Journal of Medical Screening, 20, 91–98. [DOI] [PubMed] [Google Scholar]
- Menendez, M. E. , Chen, N. C. , Mudgal, C. S. , Jupiter, J. B. , & Ring, D. (2015). Physician empathy as a driver of hand surgery patient satisfaction. The Journal of Hand Surgery, 40, 1860–1865e2. [DOI] [PubMed] [Google Scholar]
- Mercer, S. W. , & Reynolds, W. J. (2002). Empathy and quality of care. British Journal of General Practice, 52, S9–S12. [PMC free article] [PubMed] [Google Scholar]
- Miller, D. , Livingstone, V. , & Herbison, P . (2008) Interventions for relieving the pain and discomfort of screening mammography. The Cochrane Database of Systematic Reviews, 1, CD002942 Available from: http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD002942.pub2/full [last accessed 14 September 2016]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris, N. (2015). When health means suffering: Mammograms, pain and compassionate care. European Journal of Cancer Care, 24, 483–492. [DOI] [PubMed] [Google Scholar]
- Mullen, P. D. , Allen, J. D. , Glanz, K. , Fernandez, M. E. , Bowen, D. J. , Pruitt, S. L. , … & Pignone, M. (2006). Measures used in studies of informed decision making about cancer screening: A systematic review. Annals of Behavioral Medicine, 32, 188–201. [DOI] [PubMed] [Google Scholar]
- Murphy, F. , Nightingale, J. , Hogg, P. , Robinson, L. , Seddon, D. , & Mackay, S. (2015). Compression force behaviours: An exploration of the beliefs and values influencing the application of breast compression during screening mammography. Radiography, 21, 30–35. [Google Scholar]
- Myklebust, A. M. , Seierstad, T. , Stranden, E. , & Lerdal, A. (2009). Level of satisfaction during mammography screening in relation to discomfort, service provided, level of pain and breast compression. European Journal of Radiography, 1, 66–72. [Google Scholar]
- NHS Health Scotland (2015). Breast screening: Helping you decide. Edinburgh: NHS Health Scotland Publications. [Google Scholar]
- Nightingale, J. M. , Murphy, F. J. , Robinson, L. , Newton‐Hughes, A. , & Hogg, P . (2014). Breast compression – An exploration of problem solving and decision‐making in mammography. Radiography, 21, 364–369. [Google Scholar]
- Pehrson, C. , Banerjee, S. C. , Manna, R. , Shen, M. J. , Hammonds, S. , Coyle, N. , … & Bylund, C. L. (2016). Responding empathically to patients: development, implementation, and evaluation of a communication skills training module for oncology nurses. Patient Education and Counseling, 99, 610–616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poulos, A. , & Llewellyn, G. (2005). Mammography discomfort: A holistic perspective derived from women's experiences. Radiography, 11, 17–25. [Google Scholar]
- Reder, M. , & Kolip, P . (2015). Does a decision aid improve informed choice in mammography screening? Study protocol for a randomized controlled trial. BMC Women's Health, 15 [Online] Available from: http://bmcwomenshealth.biomedcentral.com/articles/10.1186/s12905-015-0210-5 [last accessed 14 September 2016]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritchie J., Lewis J., McNaughton C., & Ormston R. (Eds.) (2013). Qualitative research practice (2nd ed.). London: Sage. [Google Scholar]
- Robinson, L. , Hogg, P. , & Newton‐Hughes, A. (2013). The power and the pain: Mammographic compression research from the service‐users’ perspective. Radiography, 19, 190–195. [Google Scholar]
- Saldana, J. (2013). First cycle coding methods. The coding manual for qualitative researchers (2nd edn.). London: Sage. [Google Scholar]
- Sarma, E. A. (2015). Barriers to screening mammography. Health Psychology Review, 9, 42–62. [DOI] [PubMed] [Google Scholar]
- Shrestha, S. , & Poulos, A. (2001). The effect of verbal information on the experience of discomfort in mammography. Radiography, 7, 271–277. [Google Scholar]
- Spencer, L. , Ritchie, J. , Ormston, R. , O'Connor, W. , & Barnard, M . (2013). Analysis: principles and processes In Ritchie J., Lewis J., McNaughton Nicholls C. & Ormston R. (Eds.), Qualitative research practice (pp. 269–293). London: Sage. [Google Scholar]
- Taylor, B. (2013). Phenomenology In Taylor B. & Francis K. (Eds.), Qualitative research in the health sciences. Abingdon: Routledge. [Google Scholar]
- Teding Van Berkhout, E. , & Malouff, J. M. (2016). The efficacy of empathy training: A meta‐analysis of randomized controlled trials. Journal of Counseling Psychology, 63, 32–41. [DOI] [PubMed] [Google Scholar]
- Truesdale‐Kennedy, M. , Taggart, L. , & McIlfatrick, S. (2011). Breast cancer knowledge among women with intellectual disabilities and their experiences of receiving breast mammography. Journal of Advanced Nursing, 67, 1294–1304. [DOI] [PubMed] [Google Scholar]
- Whelehan, P. , Evans, A. , Wells, M. , & MacGillivray, S. (2013). The effect of mammography pain on repeat participation in breast cancer screening: A systematic review. Breast, 22, 383–394. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


