Abstract
Accurate and timely diagnosis of intracranial vasculopathies is important owing to the significant risk of morbidity with delayed and/or incorrect diagnosis both from the disease process and inappropriate therapies. Conventional luminal imaging techniques for analysis of intracranial vasculopathies are limited to evaluation of changes in the vessel lumen. Vessel wall MRI techniques can allow direct characterization of pathologic changes of the vessel wall. These techniques may improve diagnostic accuracy and improve patient outcomes. Extracranial carotid vessel wall imaging has been extensively investigated in patients with atherosclerotic disease and has been shown to accurately assess plaque composition and identify vulnerable plaque characteristics that may predict stroke risk beyond luminal stenosis alone. This review provides a brief history of vessel wall MRI, an overview of the intracranial vessel wall MRI techniques, its applications, and imaging findings of various intracranial vasculopathies pertinent to the neurointerventionalist, neurologist, and neuroradiologist. We searched MEDLINE, PubMed, and Google for English publications containing any of the following terms: ‘intracranial vessel wall imaging’, ‘intracranial vessel wall’, and ‘intracranial vessel wall MRI’.
INTRODUCTION
Traditionally, intracranial vascular pathologies have been evaluated with angiography, whether conventional digital subtraction angiography (DSA) or non-invasive (MR angiography, CT angiography) techniques. Angiographic techniques are limited by evaluation of the vessel lumen, making differentiation between cerebral vasculopathies difficult or impossible.1 In recent years, high-resolution MR black-blood vessel wall imaging (VWI) techniques have been developed to subtract the signal of flowing blood in the vessel lumen. This allows direct visualization of the vessel wall enabling differentiation between various intracranial vasculopa-thies.1,2 VWI has been extensively used for evaluation and characterization of extracranial carotid atherosclerosis, shedding light on vulnerable plaque characteristics that can be used for risk stratification beyond the traditional evaluation using luminal imaging. Intracranial VWI (IVWI) has also shown early promise in detecting plaque characteristics associated with culprit features.
LIMITATIONS OF LUMINAL DATA
Luminal imaging has been the imaging standard for characterization and diagnosis of intracranial vasculopathies. However, luminal imaging findings of arterial stenoses are often non-specific for disease etiology. A number of vasculopathies can present with similar luminal patterns, such as vasculitis, reversible cerebral vasoconstriction syndrome (RCVS), intracranial atherosclerotic disease (ICAD), vasospasm, infection, and radiation-related vasculopathy.3,4 The sensitivity of DSA for primary central nervous system (CNS) angiitis is limited, primarily owing to its inability to detect small vessel vasculitides, thus limiting its reliability even in negative cases.4–6 It is even found that when DSA discloses findings classic for angiitis, an alternative diagnosis to vasculitis is often made at biopsy.7
Another drawback of luminal imaging is its limited ability to detect abnormalities in patients with non-stenotic disease. For example, ICAD can result in positive remodeling and may not result in luminal stenosis until advanced stages of disease.8–10 Occasionally, a signal from intraplaque hemorrhage (IPH) can blend imperceptibly with a lumen signal, thereby masking a stenotic lesion on time-of-flight MR angiography.
IVWI can serve as a complementary tool to luminal imaging techniques in disease detection and differentiation. This technique can improve diagnostic specificity based on its ability to characterize vessel wall changes. It can also potentially detect non-stenotic or small vessel disease that cannot be well visualized on luminal imaging.11 Campi et al11 indicated that five of six patients with biopsy-proven primary CNS angiitis who were evaluated with post-contrast MRI showed perivascular enhancement along the Virchow–Robin spaces within the basal ganglia, representing lenticulostriate involvement.
TECHNICAL ASPECTS OF VWI
IVWI is challenging owing to the small caliber and tortuous course of the intracranial arteries. For example, the middle cerebral artery diameter can range from 3 to 5 mm, with a vessel wall thickness of 0.5–0.7 mm.12 It is important to be able to depict the normal vessel wall in order to differentiate it from pathology, so the highest resolution is necessary, preferably at 3T. Although most published studies have used two-dimensional (2D) black-blood techniques, application of 3D IVWI techniques has increased recently. 3D acquisitions enable improved through-plane resolution, with increased brain coverage, and isotropic scans that can be reformatted in multiple planes, allowing for better inspection of the intracranial arteries. 3D variable refocusing flip angle (VRFA) sequences (VISTA, Philips Healthcare, Best, the Netherlands; SPACE, Siemens Healthcare, Erlangen, Germany; CUBE, GE Healthcare, Milwaukee, Wisconsin, USA) have been the most extensively used and studied 3D techniques to date. VRFA have been used with T1 and proton density (PD) weightings, both before and after contrast administration.
When 2D techniques are used, multiplanar imaging is beneficial for optimal wall/lesion assessment, using axial imaging and imaging in a plane perpendicular to the axis of the interrogated artery to better evaluate lesion morphology and effects on the lumen, and avoid volume averaging effects. Vessel obliquity, slice thickness, and in-plane resolution are all factors that will affect vessel wall measurements and the sharpness of the vessel wall borders. The parameters used at our institution for IVWI are listed in table 1.
Table 1.
High-resolution MRI sequences and parameters at 3.0T
| Parameters | 2D T2W | 2D T1W | 3D PD VISTA | 3D T2 VISTA |
|---|---|---|---|---|
| TE (ms) | 72 | 10 | 38 | 90 |
| TR (ms) | 3550 | 1000 | 2000 | 3000 |
| FOV (cm) | 18×18 | 18×15.8 | 18×16.5 | 25×19 |
| Matrix | 448×448 | 448×448 | 448×413 | 500×380 |
| Slice thickness (mm) | 1 | 2 | 0.4 | 0.5 |
| In-plane resolution (mm) | 0.4×0.4 | 0.4×0.35 | 0.4×0.4 | 0.5×0.5 |
| NA | 3 | 4 | 1 | 2 |
| Acquisition time per slice (s) | 10.4 | 45 | – | 60 |
| Oversampling factor | – | – | 1.2 | 4 |
| No of slices | 26 | 4–10 | 90 | – |
| Band width | 223 | 207 | 361.7 | 1.2 |
| TSE factor | 22 | 18 | 60 | 67 |
| Start-up echoes | – | – | 4 | 164 |
| Typical sequence time | 4:30 (26 slices) | 7:30 (10 slices) | 8:30 | 8:51 |
FOV, field of view; PD, proton density; TE, echo time; TR, repetition time; TSE, turbo spin echo; T1W/T2W, T1-/T2-weighted.
Multi-contrast imaging can be performed to evaluate differential signal wall characteristics.13 T1 pre-and post-contrast, PD-and T2-weighted sequences have all been used. This enables evaluation of multi-contrast lesion heterogeneity that can be advantageous for vasculopathy differentiation and evaluation of ICAD plaque composition.13,14
The ability to assess wall disease in peripheral branches depends on the resolution of the technique used and on the quality of cerebrospinal fluid (CSF) suppression.2,15 In our experience, with 3D IVWI techniques with resolution of 0.4–0.5 mm3 voxel size, third-order branches can be assessed accurately, whereas arteries out to second-order branches can be assessed with 2D IVWI techniques.
For intracranial VWI, it is important to consider blood suppression techniques to avoid artifacts that might be confused with vessel wall abnormalities, and CSF suppression techniques for better outer wall boundary evaluation. For 2D VWI a number of blood suppression techniques can be employed. Double inversion recovery techniques can be used for blood flow suppression,2 although a limitation of this technique is prolongation of scan time, the potential need for cardiac gating, and a need for accurate estimation of the time to inversion of blood after contrast administration. Quadruple inversion recovery techniques can be used, which negate the need to estimate the inversion time of blood or use of cardiac gating.16 Double and quadruple inversion recovery techniques, however, are not frequently employed for intracranial VWI owing to their time requirements. Spin-echo techniques will also generate dark blood; however, a major limitation is that with slow flow or in-plane flow, blood suppression will be lost. 3D VRFA techniques achieve dark blood imaging from gradient moment-induced intravoxel dephasing and stimulated echo-induced intravoxel dephasing.2 Additional blood suppression techniques can be employed with 3D imaging. One such technique is motion-sensitized driven equilibrium (MSDE), which uses flow-sensitive dephasing gradients to suppress flow17; however, this technique results in T2 signal decay and loss of signal. The delay alternating with nutation for tailored excitation (DANTE) pulse train is a series of low flip angle non-selective pulses interleaved with gradient pulses with short repetition times that can result in both optimized blood and CSF suppression, without any effects on tissue contrast.15 This allows for improved vessel wall assessment with PD-weighted 3D VRFA techniques while also minimizing artifacts from turbulent or slow flow.
MR VESSEL WALL IMAGING: HISTORICAL PERSPECTIVE
The first studies to evaluate the vessel wall using MRI were performed on surgically excised iliac artery atherosclerotic lesions. These studies provided correlation between plaque composition and MR signal characteristics.18,19 Subsequently, changes in vessel wall thickness in thoracic aortic pathology were studied using VWI.20 In 1990, Edelman et al21 compared the ability of bright and black-blood imaging techniques in carotid atherosclerotic disease and found that black-blood techniques were advantageous owing to more accurate estimation of luminal stenosis.
Since then, multiple studies have further characterized plaque components and their MR appearances, enabling atherosclerosis evaluation beyond luminal stenosis. With the introduction of the ‘vulnerable plaque’ model in 2003 by Naghavi et al,22,23 in which certain plaque characteristics can increase the likelihood of patient symptoms secondary to thrombus formation and embolization, carotid VWI with a focus on plaque characterization became an intense area of investigation.
In addition to the traditional luminal stenosis evaluation, plaque composition—specifically, the presence and status of the fibrous cap, IPH, presence and volume of lipid-rich necrotic core (LRNC), plaque neovascularity, ulceration, and fissuring, have been found to be markers of current and future cerebrovascular events.24–26 VWI has proved to be a valuable technique in the detection and follow-up also of early large artery vasculitides.27,28
INTRACRANIAL VWI
In 1995, the first study was performed assessing the intracranial vessel walls on MRI. The investigators examined the degree of intracranial carotid and vertebral arterial wall enhancement and its correlation with patient age. They found that with increased age, there was an associated significant increase in the presence and degree of wall enhancement, which was thought to correlate with ICAD.29 Thirteen years later, Küker et al,30 re-examined this technique and found that high-resolution T1 post-contrast IVWI detected wall enhancement and thickening associated with intracranial stenosis in cerebral vasculitis. The IVWI technique has increasingly been used to further characterize a range of intracranial vasculopathies, including cerebral vasculitis, ICAD, RCVS, aneurysms, arterial dissections, and moyamoya disease (MMD) and syndrome (MMS).
INTRACRANIAL VASCULOPATHIES AMENABLE TO INVESTIGATION WITH VWI
Intracranial atherosclerotic disease
ICAD causes significant morbidity and mortality, accounting for up to 50% of ischemic strokes in certain populations.31 Whereas previous approaches to ICAD assessment considered the degree of plaque-related stenosis, IVWI directly evaluates plaque characteristics, starting with the degree and pattern of wall thickening at the site of disease.32 Luminal imaging often underestimates the burden of ICAD and does not reliably detect non-stenotic lesions that can be symptomatic.8,9,33 IVWI studies have suggested that plaques with positive remodeling (outer wall remodeling) are more frequently symptomatic than negative remodeling plaques.32,34
Plaque signal characteristic evaluation is helpful in assessing plaque composition.14,34 The T2 hyperintense fibrous cap overlies the LRNC, which is isointense on T1-weighted imaging and hypointense on fat-saturated T2-weighted imaging.34,35 Increased volume of the LRNC has been associated with higher rates of rupture.34 IPH has proved to be an important risk factor for plaque vulnerability, with increased rates of plaque complications and stroke.14 IPH will appear as intraplaque T1 hyperintensity >150% of the signal intensity of internal reference muscle tissue.14 Additionally, ischemic infarcts are associated with upstream eccentric enhancing plaques within the first 4 weeks after the stroke, and over time, the degree of enhancement progressively diminishes.36 In patients with multifocal disease, culprit lesions enhance (figure 1A–D), and they do so more avidly than non-culprit lesions, which enhance inconsistently.37 The typical appearance of ICAD on IVWI is an eccentric, heterogeneous mild to moderate enhancing, outward remodeling lesion with heterogeneous T2 signal and juxtaluminal T2 hyperintensity that typically involves proximal intracranial branches or bifurcation points, which is distinctive in appearance from other vasculopathies described below.13 The radial location of plaques along the middle cerebral artery has been shown to be important for predicting symptoms and stroke type. For example, plaques along the superior wall of the middle cerebral artery have been associated with deep infarcts, presumably owing to ostial stenosis/occlusion at the origins of lenticulostriate perforators.9,38
Figure 1.
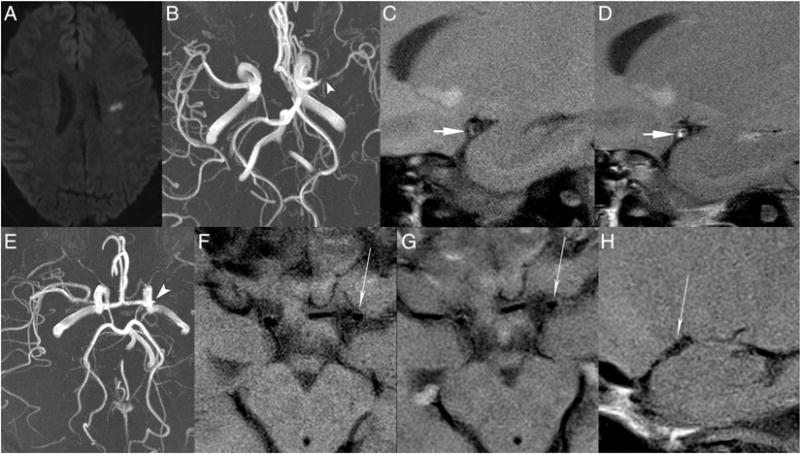
Atherosclerosis (A–D) and moyamoya disease (E–H). (A–D) A middle-aged homeless patient with 30 pack-year smoking history and IV drug abuse presented with a 4-day history of left middle cerebral artery (MCA) territory stroke. Axial diffusion-weighted imaging (A) shows multiple left MCA territory infarcts. Axial MR angiography (MRA) maximum intensity projection (MIP) (B) shows high-grade left MCA narrowing (arrowhead). Sagittal oblique T1 pre-contrast (C) and post-contrast (D) vessel wall sequences of the left MCA show an eccentric enhancing lesion with wall thickening and outward remodeling (short arrow), compatible with intracranial atherosclerotic disease. (E–H) A middle-aged patient without vascular risk factors, history of genetic syndromes, prior radiation, or evidence of central nervous system vasculitis presented with intermittent headaches and otherwise unremarkable clinical results. On axial MRA MIP (E) there is occlusion of the left carotid terminus (arrowhead) with attenuation of the right carotid terminus and proximal MCA. On axial T1 pre-contrast (F) and post-contrast (G) MRI of the carotid terminus and sagittal T1 post-contrast (H) MRI of the proximal MCA vessel wall there is no evidence of vessel wall enhancement, wall thickening, or outward remodeling (long arrows), most compatible with moyamoya disease.
IVWI is changing our understanding of the natural history of ICAD. As for cervical atherosclerotic disease, treatment algorithms for ICAD have been based on the degree of stenosis, with 70% stenosis being a cut-off point for endovascular treatment of refractory ICAD lesions following the Warfarin–Aspirin Symptomatic Intracranial Disease (WASID) trial.39 However, current IVWI techniques show that significant ICAD may not be associated with luminal stenosis. Initial vessel wall remodeling can maintain the lumen while the wall itself dramatically thickens, and such findings are associated with higher rates of atherosclerotic plaque rupture.32,34,40,41 With intracranial stenosis, some symptoms may result from hypoperfusion rather than thromboembolic phenomena, a corollary of late-stage constrictive remodeling in coronary atherosclerosis that causes stable angina rather than acute coronary syndrome.34,41,42 Prior investigations of ICAD therapies might not have been adequately targeting high-risk lesions most likely to cause future neurologic events. IVWI may provide a better imaging marker for selection of ICAD lesions in future trials.
Moyamoya disease/syndrome
MMD is an idiopathic disease causing progressive narrowing of the bilateral carotid termini, leading to development of compensatory collateral branches at the base of the brain.43 In MMS there is unilateral or bilateral supraclinoid internal carotid artery stenosis from one of several disease states, including ICAD, vasculitis, radiation therapy, neurofibromatosis type 1, or other processes.43 Distinguishing between these two processes is important because MMD typically requires treatment with external carotid to middle cerebral artery bypass, whereas some of the underlying processes causing MMS are potentially reversible.43 Angiography does not reliably distinguish between MMD and MMS as both may have a similar luminal imaging appearance. Some reports have shown concentric vessel wall thickening and enhancement of the distal internal carotid arteries in MMD, whereas others have indicated a lack of wall enhancement (figure 1E–H).1,44,45 The considerable genotypic heterogeneity found in MMD, and the variable phenotypic presentation of IVWI may represent varying pathophysiologic mechanisms of disease development.46,47 The difference in appearance might also be secondary to a transient inflammatory step, with corresponding enhancement in the longitudinal progression of MMD.48 In our experience, MMD shows minimal to no circumferential enhancement without outward remodeling. MMS caused by ICAD will show the findings described above, most notably with eccentric plaques often showing positive remodeling and enhancement, clearly discernible from MMD.1,44
CNS vasculitis
IVWI may provide another useful tool for differentiating intra-cranial vasculopathies that look similar on DSA, including vasculitis, RCVS, ICAD, vasospasm, infection, and radiation-related vasculopathy.3,4 The classic appearance of angiitis on DSA has a specificity as low as 30%.4 The sensitivity of catheter angiography for CNS vasculitis ranges from 27% to 90%.5,6 The limitation in sensitivity is primarily related to the difficulty of DSA in the detection of subtle changes or very distal small vessel involvement. Biopsy of cerebral vasculitis is associated with more risks than peripheral vessel biopsy, and its sensitivity for the diagnosis of CNS vasculitis may be <50%.49 Vasculitic enhancement on post-contrast MRI can extend beyond the vessel wall into the periadventitia, increasing the conspicuity of the affected segments and potentially enabling detection of microvascular involvement that is otherwise angiographically occult.5 IVWI directly visualizes vessel wall inflammation and edema, showing thickening and multifocal homogeneous, smooth, intense, concentric enhancement of the vessel wall (figure 2).1,30,50–52 IVWI can also help to track treatment response (figure 2A–F). This pattern is in contradistinction to that seen in ICAD, in which there is eccentric, expansive wall involvement and inconsistent and heterogeneous enhancement.1,34,37 With advances in IVWI, findings diagnostic for vasculitis may limit the need for biopsy, and in cases where biopsy is required, localization of active disease on IVWI can guide surgeons to increase diagnostic yield.30
Figure 2.
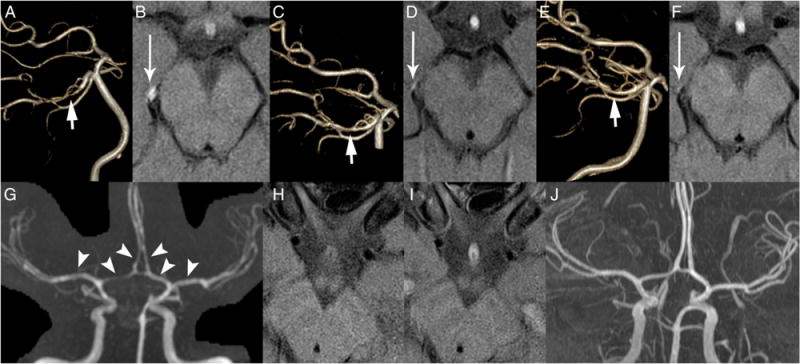
Vasculitis and reversible cerebral vasoconstriction syndrome. (A–F) Young patient who presented with aphasia and bilateral middle cerebral artery (MCA) territory infarcts. Cerebrospinal fluid analysis indicated the presence of anti-varicella zoster virus (anti-VZV) antibodies, confirming a diagnosis of VZV vasculitis. Three-dimensional reconstruction of the posterior circulation from time-of-flight (TOF) MR angiography (MRA) (A) shows high-grade stenosis of the right P2 posterior cerebral artery (short arrow). There were additional stenoses involving the inferior division of the bilateral M1 MCA and bilateral A2 anterior cerebral artery (not shown). On T1 post-contrast intracranial vessel wall imaging (IVWI) (B), there is a circumferential enhancing lesion involving the stenotic segment (long arrow), compatible with inflammatory vasculopathy. On follow-up IVWI and TOF MRA performed 2 months (C and D) and 4 months (E and F) later, there is progressive improved luminal patency (short arrow, C and E) and diminished wall enhancement (long arrow, D and F), which corresponded with clinical improvement. (G–J) A middle-aged patient with a history of depression and selective serotonin reuptake inhibitor use, who presented with severe headache and stroke symptoms, was found to have bilateral watershed distribution infarcts on diffusion-weighted imaging (not included). Coronal MRA maximum intensity projection of the intracranial arteries (G) shows diffuse intradural arterial stenosis (arrowheads). Axial T1-weighted black-blood pre-contrast (H) and post-contrast (I) sequences show no evidence of appreciable wall enhancement. Follow-up MRA (J) performed 1 month later shows significant improvement in the degree of diffuse luminal narrowing.
Reversible cerebral vasoconstriction syndrome
Patients with RCVS present with sudden, severe headaches, at times with concomitant neurological deficits.53 Possible complications of RCVS include infarction, subarachnoid hemorrhage, parenchymal edema, or intraparenchymal hemorrhage. IVWI studies show minimal smooth thickening of the vessel wall that is concentric with minimal to no enhancement (figure 2G–J).50,51 This is consistent with its pathophysiological process, specifically non-inflammatory vasospasm. There is near uniform resolution of luminal narrowing within 3 months of symptom onset (figure 2J).51,53 This is in contradistinction to cerebral vasculitis, which shows multifocal circumferential enhancement associated with the regions of stenosis with persistence of luminal narrowing on follow-up luminal imaging.50,51
Intracranial arterial dissection
Intracranial dissections, although relatively rare, are an important cause of ischemic stroke and subarachnoid hemorrhage, especially in younger patients.54 The etiology is unknown in most cases, but inflammatory vessel wall changes may also play a role in some cases. When blood collects between the media and internal elastic lamina via an intimal tear, this is termed a subintimal dissection; a subadventitial dissection occurs when the hematoma extends through the media.54 Subintimal dissections often lead to hypoperfusion or ostial occlusion and thromboemboli, resulting in ischemic symptoms.55 Intracranial subadventitial dissections frequently will result in subarachnoid hemorrhage and can often maintain luminal contours, making them difficult to detect on luminal imaging. Subadventitial dissections can also result in pseudoaneurysm or giant partially thrombosed aneurysm formation.54 T1-weighted imaging with fat saturation can demonstrate thrombus within the false lumen of a dissection, but IVWI techniques with improved resolution and improved blood signal suppression can improve characterization and detection.56 57 Additionally, dissections can be further evaluated with post-contrast imaging that may show eccentric dissection flap enhancement.58
Cerebral aneurysms
Cerebral aneurysms can be evaluated by IVWI, which is adding to our understanding of the factors that cause their growth. Vasa vasorum is not normally present in the cerebral vasculature until the development of pathology such as ICAD or aneurysms.58 The vasa vasorum may leak and cause hemorrhage into the wall of an aneurysm, inciting an inflammatory cascade that includes the release of growth factors, aneurysmal enlargement, and wall thinning, which may lead to rupture. IVWI can identify vasa vasorum, the aneurysm wall, and mural hematoma.58,59 IVWI can also more accurately measure wall thickness while mitigating the overestimation commonly seen with older techniques.60 In multiple aneurysms with acute subarachnoid hemorrhage, aneurysm wall enhancement helps to identify the culprit lesion.61 IVWI may help to identify an angiographically occult aneurysm as the source of hemorrhage.62 Figure 3 shows an example of IVWI used in a ruptured intracranial aneurysm. Early demonstrations of the feasibility of IVWI for aneurysms may now lead to further investigation to identify which characteristics are predictive of aneurysm rupture, providing neurointerventionalists/neurosurgeons with more information to determine when and what type of treatment is appropriate.58,59
Figure 3.
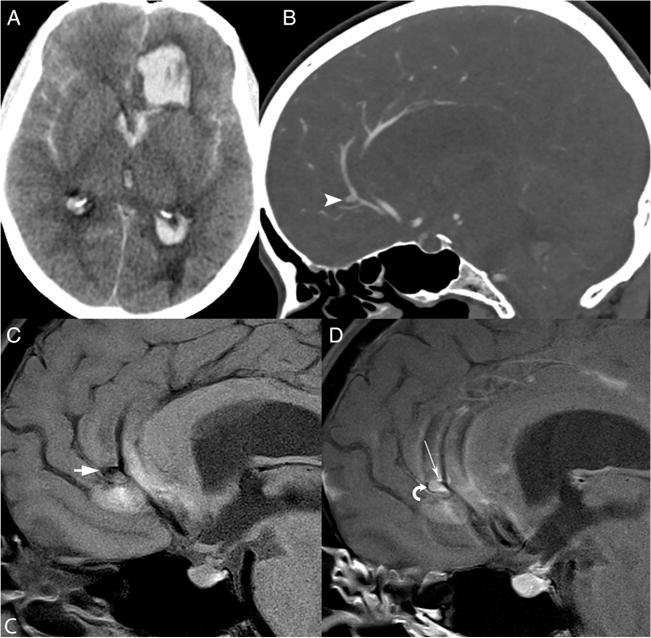
Ruptured intracranial aneurysm. A middle-aged patient presented with sudden-onset severe headache. Axial non-contrast CT of the head (A) demonstrates prominent left frontal intraparenchymal hemorrhage, subarachnoid and intraventricular hemorrhage. Sagittal multiplanar reformat of CT angiography (CTA) (B) shows a left A2 anterior cerebral artery (ACA) aneurysm (arrowhead), which was in close proximity to the intraparenchymal hematoma. Intracranial vessel wall imaging was performed 2 days after aneurysm rupture. Sagittal T1 pre-contrast vessel wall sequence (C) shows the left A2 ACA aneurysm (arrowhead) adjacent to the medial aspect of the parenchymal hematoma. A sagittal T1 post-contrast vessel wall image (D) shows both vessel wall (long arrow) and intraluminal (curved arrow) enhancement. Intraluminal enhancement might have been secondary to stagnant or turbulent flow, or thrombus.
SUMMARY
IVWI is an emerging technique that can complement traditional luminal imaging techniques for the evaluation of intracranial vasculopathies. It has the potential for disease differentiation and lesion characterization that may indicate present or future complications and for longitudinal disease evaluation to determine treatment response. Most studies that have been performed to date are cross-sectional. Prospective longitudinal IVWI investigation of individual disease processes would help to better describe imaging findings at different stages of disease and illuminate underlying pathophysiologic processes, enabling improved understanding of vasculopathy evolution and its contribution to patient outcomes.
Acknowledgments
Funding Research support from NIH 1R56NS092207-01 grant.
Footnotes
Contributors
MM-B: wrote, reviewed, supervised, directed and submitted the manuscript. MA: wrote portions of the manuscript and performed critical review. SG: performed critical review, edited and composed the figure of the manuscript. CY, DG: performed critical review, edited and directed portions of the manuscript.
Competing interests None declared.
Ethics approval Institutional review board.
Provenance and peer review Not commissioned; externally peer reviewed.
References
- 1.Swartz RH, Bhuta SS, Farb RI, et al. Intracranial arterial wall imaging using high-resolution 3-Tesla contrast-enhanced MRI. Neurology. 2009;72:627–34. doi: 10.1212/01.wnl.0000342470.69739.b3. [DOI] [PubMed] [Google Scholar]
- 2.Qiao Y, Steinman DA, Qin Q, et al. Intracranial arterial wall imaging using three-dimensional high isotropic resolution black blood MRI at 3.0 Tesla. J Magn Reson Imaging. 2011;34:22–30. doi: 10.1002/jmri.22592. [DOI] [PubMed] [Google Scholar]
- 3.Alhalabi M, Moore PM. Serial angiography in isolated angiitis of the central nervous system. Neurology. 1994;44:1221–6. doi: 10.1212/wnl.44.7.1221. [DOI] [PubMed] [Google Scholar]
- 4.Duna GF, Calabrese LH. Limitations of invasive modalities in the diagnosis of primary angiitis of the central nervous system. J Rheumatol. 1995;22:662–7. [PubMed] [Google Scholar]
- 5.Harris KG, Tran DD, Sickels WJ, et al. Diagnosing intracranial vasculitis: the roles of MR and angiography. AJNR Am J Neuroradiol. 1994;15:317–30. [PMC free article] [PubMed] [Google Scholar]
- 6.Vollmer TL, Guarnaccia J, Harrington W, et al. Idiopathic granulomatous angiitis of the central nervous system. Diagnostic challenges. Arch Neurol. 1993;50:925–30. doi: 10.1001/archneur.1993.00540090032007. [DOI] [PubMed] [Google Scholar]
- 7.Kadkhodayan Y, Alreshaid A, Moran CJ, et al. Primary angiitis of the central nervous system at conventional angiography. Radiology. 2004;233:878–82. doi: 10.1148/radiol.2333031621. [DOI] [PubMed] [Google Scholar]
- 8.de Havenon A, Yuan C, Tirschwell D, et al. Nonstenotic culprit plaque: the utility of high-resolution vessel wall MRI of intracranial vessels after ischemic stroke. Case Rep Radiol. 2015;2015:356582. doi: 10.1155/2015/356582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xu WH, Li ML, Niu JW, et al. Intracranial artery atherosclerosis and lumen dilation in cerebral small-vessel diseases: a high-resolution MRI study. CNS Neurosci Ther. 2014;20:364–7. doi: 10.1111/cns.12224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhou L, Ni J, Xu W, et al. High-resolution MRI findings in patients with capsular warning syndrome. BMC Neurol. 2014;14:16. doi: 10.1186/1471-2377-14-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Campi A, Benndorf G, Filippi M, et al. Primary angiitis of the central nervous system: serial MRI of brain and spinal cord. Neuroradiology. 2001;43:599–607. doi: 10.1007/s002340100561. [DOI] [PubMed] [Google Scholar]
- 12.Jain KK. Some observations on the anatomy of the middle cerebral artery. Can J Surg. 1964;7:134–9. [PubMed] [Google Scholar]
- 13.Mossa-Basha M, Hwang WD, De Havenon A, et al. Multicontrast high-resolution vessel wall MRI and its value in differentiating intracranial vasculopathic processes. Stroke. 2015;46:1567–73. doi: 10.1161/STROKEAHA.115.009037. [DOI] [PubMed] [Google Scholar]
- 14.Xu WH, Li ML, Gao S, et al. Middle cerebral artery intraplaque hemorrhage: prevalence and clinical relevance. Ann Neurol. 2012;71:195–8. doi: 10.1002/ana.22626. [DOI] [PubMed] [Google Scholar]
- 15.Wang J, Helle M, Zhou Z, et al. Joint blood and cerebrospinal fluid suppression for intracranial vessel wall MRI. Magn Reson Med Sci. doi: 10.1002/mrm.25667. Published Online First: 13 Mar 2015. [DOI] [PubMed] [Google Scholar]
- 16.Yarnykh VL, Yuan C. T1-insensitive flow suppression using quadruple inversion-recovery. Magn Reson Med Sci. 2002;48:899–905. doi: 10.1002/mrm.10292. [DOI] [PubMed] [Google Scholar]
- 17.Zhu C, Graves MJ, Yuan J, et al. Optimization of improved motion-sensitized driven-equilibrium (iMSDE) blood suppression for carotid artery wall imaging. Magn Reson Med. 2014;16:61. doi: 10.1186/s12968-014-0061-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Herfkens RJ, Higgins CB, Hricak H, et al. Nuclear magnetic resonance imaging of atherosclerotic disease. Radiology. 1983;148:161–6. doi: 10.1148/radiology.148.1.6856827. [DOI] [PubMed] [Google Scholar]
- 19.Kaufman L, Crooks LE, Sheldon PE, et al. Evaluation of NMR imaging for detection and quantification of obstructions in vessels. Invest Radiol. 1982;17:554–60. doi: 10.1097/00004424-198211000-00006. [DOI] [PubMed] [Google Scholar]
- 20.Glazer HS, Gutierrez FR, Levitt RG, et al. The thoracic aorta studied by MR imaging. Radiology. 1985;157:149–55. doi: 10.1148/radiology.157.1.2863853. [DOI] [PubMed] [Google Scholar]
- 21.Edelman RR, Mattle HP, Wallner B, et al. Extracranial carotid arteries: evaluation with “black blood” MR angiography. Radiology. 1990;177:45–50. doi: 10.1148/radiology.177.1.2399337. [DOI] [PubMed] [Google Scholar]
- 22.Naghavi M, Libby P, Falk E, et al. From vulnerable plaque to vulnerable patient: a call for new definitions and risk assessment strategies: part II. Circulation. 2003;108:1772–8. doi: 10.1161/01.CIR.0000087481.55887.C9. [DOI] [PubMed] [Google Scholar]
- 23.Naghavi M, Libby P, Falk E, et al. From vulnerable plaque to vulnerable patient: a call for new definitions and risk assessment strategies: part I. Circulation. 2003;108:1664–72. doi: 10.1161/01.CIR.0000087480.94275.97. [DOI] [PubMed] [Google Scholar]
- 24.Saam T, Cai J, Ma L, et al. Comparison of symptomatic and asymptomatic atherosclerotic carotid plaque features with in vivo MR imaging. Radiology. 2006;240:464–72. doi: 10.1148/radiol.2402050390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Saba L, Anzidei M, Sanfilippo R, et al. Imaging of the carotid artery. Atherosclerosis. 2012;220:294–309. doi: 10.1016/j.atherosclerosis.2011.08.048. [DOI] [PubMed] [Google Scholar]
- 26.von Ingersleben G, Schmiedl UP, Hatsukami TS, et al. Characterization of atherosclerotic plaques at the carotid bifurcation: correlation of high-resolution MR imaging with histologic analysis—preliminary study. Radiographics. 1997;17:1417–23. doi: 10.1148/radiographics.17.6.9397455. [DOI] [PubMed] [Google Scholar]
- 27.Choe YH, Han BK, Koh EM, et al. Takayasu’s arteritis: assessment of disease activity with contrast-enhanced MR imaging. AJR Am J Roentgenol. 2000;175:505–11. doi: 10.2214/ajr.175.2.1750505. [DOI] [PubMed] [Google Scholar]
- 28.Jiang L, Li D, Yan F, et al. Evaluation of Takayasu arteritis activity by delayed contrast-enhanced magnetic resonance imaging. Int J Cardiol. 2012;155:262–7. doi: 10.1016/j.ijcard.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 29.Aoki S, Shirouzu I, Sasaki Y, et al. Enhancement of the intracranial arterial wall at MR imaging: relationship to cerebral atherosclerosis. Radiology. 1995;194:477–81. doi: 10.1148/radiology.194.2.7824729. [DOI] [PubMed] [Google Scholar]
- 30.Küker W, Gaertner S, Nagele T, et al. Vessel wall contrast enhancement: a diagnostic sign of cerebral vasculitis. Cerebrovasc Dis. 2008;26:23–9. doi: 10.1159/000135649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wong LK. Global burden of intracranial atherosclerosis. Int J Stroke. 2006;1:158–9. doi: 10.1111/j.1747-4949.2006.00045.x. [DOI] [PubMed] [Google Scholar]
- 32.Chung GH, Kwak HS, Hwang SB, et al. High resolution MR imaging in patients with symptomatic middle cerebral artery stenosis. Eur J Radiol. 2012;81:4069–74. doi: 10.1016/j.ejrad.2012.07.001. [DOI] [PubMed] [Google Scholar]
- 33.Li ML, Xu WH, Song L, et al. Atherosclerosis of middle cerebral artery: evaluation with high-resolution MR imaging at 3T. Atherosclerosis. 2009;204:447–52. doi: 10.1016/j.atherosclerosis.2008.10.019. [DOI] [PubMed] [Google Scholar]
- 34.Xu WH, Li ML, Gao S, et al. In vivo high-resolution MR imaging of symptomatic and asymptomatic middle cerebral artery atherosclerotic stenosis. Atherosclerosis. 2010;212:507–11. doi: 10.1016/j.atherosclerosis.2010.06.035. [DOI] [PubMed] [Google Scholar]
- 35.Degnan AJ, Gallagher G, Teng Z, et al. MR angiography and imaging for the evaluation of middle cerebral artery atherosclerotic disease. AJNR Am J Neuroradiol. 2012;33:1427–35. doi: 10.3174/ajnr.A2697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Skarpathiotakis M, Mandell DM, Swartz RH, et al. Intracranial atherosclerotic plaque enhancement in patients with ischemic stroke. AJNR Am J Neuroradiol. 2013;34:299–304. doi: 10.3174/ajnr.A3209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Qiao Y, Zeiler SR, Mirbagheri S, et al. Intracranial plaque enhancement in patients with cerebrovascular events on high-spatial-resolution MR images. Radiology. 2014;271:534–42. doi: 10.1148/radiol.13122812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Xu WH, Li ML, Gao S, et al. Plaque distribution of stenotic middle cerebral artery and its clinical relevance. Stroke. 2011;42:2957–9. doi: 10.1161/STROKEAHA.111.618132. [DOI] [PubMed] [Google Scholar]
- 39.Chimowitz MI, Lynn MJ, Howlett-Smith H, et al. Comparison of warfarin and aspirin for symptomatic intracranial arterial stenosis. N Engl J Med. 2005;352:1305–16. doi: 10.1056/NEJMoa043033. [DOI] [PubMed] [Google Scholar]
- 40.Shi MC, Wang SC, Zhou HW, et al. Compensatory remodeling in symptomatic middle cerebral artery atherosclerotic stenosis: a high-resolution MRI and microemboli monitoring study. Neurol Res. 2012;34:153–8. doi: 10.1179/1743132811Y.0000000065. [DOI] [PubMed] [Google Scholar]
- 41.Varnava AM, Mills PG, Davies MJ. Relationship between coronary artery remodeling and plaque vulnerability. Circulation. 2002;105:939–43. doi: 10.1161/hc0802.104327. [DOI] [PubMed] [Google Scholar]
- 42.Alexander MD, Meyers PM, English JD, et al. Symptom differences and pretreatment asymptomatic interval affect outcomes of stenting for intracranial atherosclerotic disease. AJNR Am J Neuroradiol. 2014;35:1157–62. doi: 10.3174/ajnr.A3836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Scott RM, Smith ER. Moyamoya disease and moyamoya syndrome. N Engl J Med. 2009;360:1226–37. doi: 10.1056/NEJMra0804622. [DOI] [PubMed] [Google Scholar]
- 44.Kim YJ, Lee DH, Kwon JY, et al. High resolution MRI difference between moyamoya disease and intracranial atherosclerosis. Eur J Neurol. 2013;20:1311–8. doi: 10.1111/ene.12202. [DOI] [PubMed] [Google Scholar]
- 45.Ryoo S, Cha J, Kim SJ, et al. High-resolution magnetic resonance wall imaging findings of Moyamoya disease. Stroke. 2014;45:2457–60. doi: 10.1161/STROKEAHA.114.004761. [DOI] [PubMed] [Google Scholar]
- 46.Milewicz DM, Kwartler CS, Papke CL, et al. Genetic variants promoting smooth muscle cell proliferation can result in diffuse and diverse vascular diseases: evidence for a hyperplastic vasculomyopathy. Genet Med. 2010;12:196–203. doi: 10.1097/GIM.0b013e3181cdd687. [DOI] [PubMed] [Google Scholar]
- 47.Wu Z, Jiang H, Zhang L, et al. Molecular analysis of RNF213 gene for moyamoya disease in the Chinese Han population. PLoS ONE. 2012;7:e48179. doi: 10.1371/journal.pone.0048179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Masuda J, Ogata J, Yutani C. Smooth muscle cell proliferation and localization of macrophages and T cells in the occlusive intracranial major arteries in moyamoya disease. Stroke. 1993;24:1960–7. doi: 10.1161/01.str.24.12.1960. [DOI] [PubMed] [Google Scholar]
- 49.Birnbaum J, Hellmann DB. Primary angiitis of the central nervous system. Arch Neurol. 2009;66:704–9. doi: 10.1001/archneurol.2009.76. [DOI] [PubMed] [Google Scholar]
- 50.Mandell DM, Matouk CC, Farb RI, et al. Vessel wall MRI to differentiate between reversible cerebral vasoconstriction syndrome and central nervous system vasculitis: preliminary results. Stroke. 2012;43:860–2. doi: 10.1161/STROKEAHA.111.626184. [DOI] [PubMed] [Google Scholar]
- 51.Obusez EC, Hui F, Hajj-Ali RA, et al. High-resolution MRI vessel wall imaging: spatial and temporal patterns of reversible cerebral vasoconstriction syndrome and central nervous system vasculitis. AJNR Am J Neuroradiol. 2014;35:1527–32. doi: 10.3174/ajnr.A3909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pfefferkorn T, Linn J, Habs M, et al. Black blood MRI in suspected large artery primary angiitis of the central nervous system. J Neuroimaging. 2013;23:379–83. doi: 10.1111/j.1552-6569.2012.00743.x. [DOI] [PubMed] [Google Scholar]
- 53.Marder CP, Donohue MM, Weinstein JR, et al. Multimodal imaging of reversible cerebral vasoconstriction syndrome: a series of 6 cases. AJNR Am J Neuroradiol. 2012;33:1403–10. doi: 10.3174/ajnr.A2964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sikkema T, Uyttenboogaart M, Eshghi O, et al. Intracranial artery dissection. Eur J Neurol. 2014;21:820–6. doi: 10.1111/ene.12384. [DOI] [PubMed] [Google Scholar]
- 55.Caplan LR. Dissections of brain-supplying arteries. Nat Clin Pract Neurol. 2008;4:34–42. doi: 10.1038/ncpneuro0683. [DOI] [PubMed] [Google Scholar]
- 56.Naggara O, Touzé E, Marsico R, et al. High-resolution MR imaging of periarterial edema associated with biological inflammation in spontaneous carotid dissection. Eur Radiol. 2009;19:2255–60. doi: 10.1007/s00330-009-1415-5. [DOI] [PubMed] [Google Scholar]
- 57.Takano K, Yamashita S, Takemoto K, et al. MRI of intracranial vertebral artery dissection: evaluation of intramural haematoma using a black blood, variable-flip-angle 3D turbo spin-echo sequence. Neuroradiology. 2013;55:845–51. doi: 10.1007/s00234-013-1183-4. [DOI] [PubMed] [Google Scholar]
- 58.Portanova A, Hakakian N, Mikulis DJ, et al. Intracranial vasa vasorum: insights and implications for imaging. Radiology. 2013;267:667–79. doi: 10.1148/radiol.13112310. [DOI] [PubMed] [Google Scholar]
- 59.Park JK, Lee CS, Sim KB, et al. Imaging of the walls of saccular cerebral aneurysms with double inversion recovery black-blood sequence. J Magn Reson Imaging. 2009;30:1179–83. doi: 10.1002/jmri.21942. [DOI] [PubMed] [Google Scholar]
- 60.Tenjin H, Tanigawa S, Takadou M, et al. Relationship between preoperative magnetic resonance imaging and surgical findings: aneurysm wall thickness on high-resolution T1-weighted imaging and contact with surrounding tissue on steady-state free precession imaging. Neurol Med Chir (Tokyo) 2013;53:336–42. doi: 10.2176/nmc.53.336. [DOI] [PubMed] [Google Scholar]
- 61.Matouk CC, Mandell DM, Günel M, et al. Vessel wall magnetic resonance imaging identifies the site of rupture in patients with multiple intracranial aneurysms: proof of principle. Neurosurgery. 2013;72:492–6. doi: 10.1227/NEU.0b013e31827d1012. discussion 96. [DOI] [PubMed] [Google Scholar]
- 62.Horie N, Morikawa M, Fukuda S, et al. Detection of blood blister-like aneurysm and intramural hematoma with high-resolution magnetic resonance imaging. J Neurosurg. 2011;115:1206–9. doi: 10.3171/2011.8.JNS11909. [DOI] [PubMed] [Google Scholar]


