Abstract
Background:
Open reduction and internal fixation (ORIF) of the clavicle is a common procedure that has been shown to have improved outcomes over nonoperative treatment. Several incisions can be used to approach clavicle fractures, the decision of which is variable among surgeons.
Purpose:
To compare patient satisfaction and subjective outcomes between patients with a longitudinal incision versus those with a necklace incision for the treatment of diaphyseal clavicle fractures.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
Thirty-six patients with a diaphyseal clavicle fracture (Orthopaedic Trauma Association type 15-B) were treated by 1 of 7 orthopaedic surgeons. The intervention was ORIF with anatomic contoured plates. Patients were divided into a necklace incision group and a longitudinal incision group depending on the surgical approach used. Medical records were reviewed, and participants completed an online survey with questions related to pain, numbness, scar appearance, and satisfaction. Function was assessed using the American Shoulder and Elbow Surgeons score. Statistical significance was determined with P < .05.
Results:
There were 16 patients in the necklace incision group and 20 in the longitudinal incision group. Patients in the necklace incision group were significantly more satisfied with the appearance of their scars (P = .01), which correlated with overall satisfaction (P = .05). There were no differences in overall satisfaction, pain, numbness, or reoperation rates for hardware removal between the necklace (6%) and longitudinal groups (15%).
Conclusion:
Patients undergoing clavicle ORIF with a necklace incision are more satisfied with their scar appearance than those with a longitudinal incision. The overall satisfaction, rate of numbness, and plate removal were similar in both groups.
Keywords: open reduction internal fixation of clavicle fractures, clavicle fracture outcomes, patient satisfaction, clavicle surgical incision type, shoulder trauma
Open reduction and internal fixation (ORIF) of diaphyseal clavicle fractures (Orthopaedic Trauma Association [OTA] type 15-B)13 is an increasingly common procedure that has been shown to provide lower rates of nonunion and earlier functional return as compared with nonoperative treatment for certain fracture patterns.1,14,16 Several incisions can be used to approach clavicle fractures, the decision of which is variable among surgeons. The incision can be made longitudinally along the subcutaneous border of the clavicle, or as a necklace incision along the Langer lines, which is relatively more vertical and perpendicular to the clavicle (Figure 1).
Figure 1.
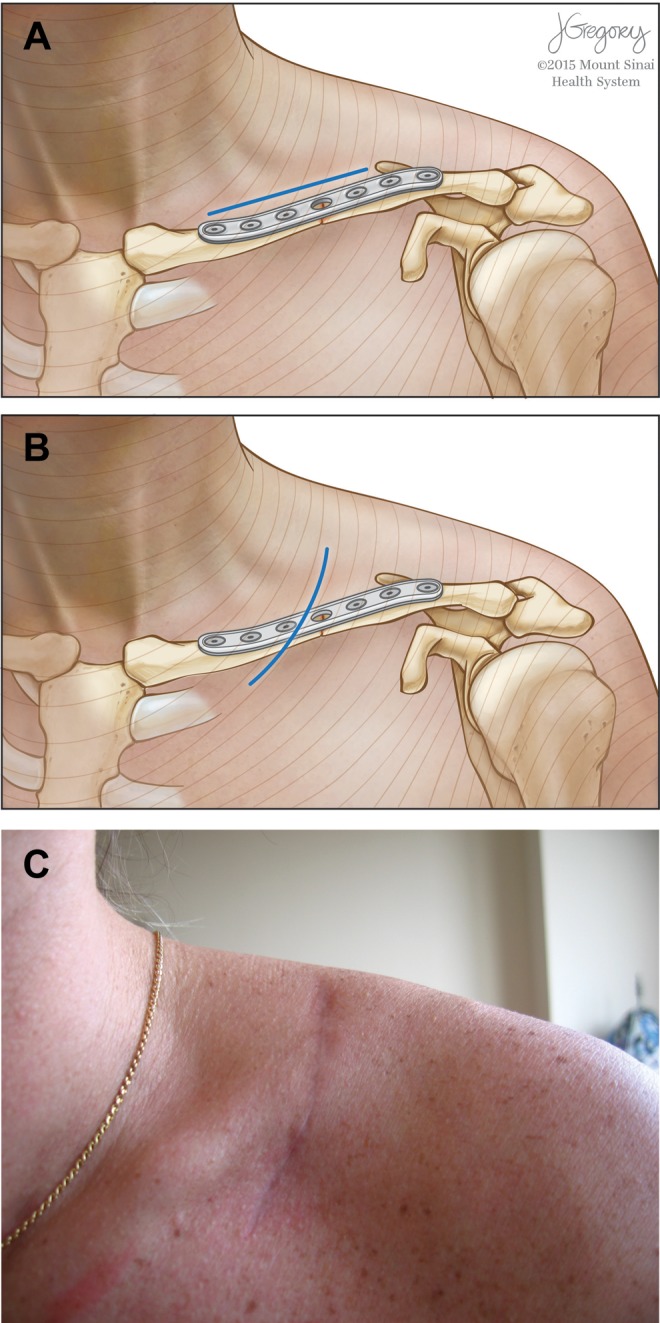
(A) The longitudinal incision for open reduction and internal fixation of the clavicle crosses the Langer lines in a more perpendicular manner versus the (B) necklace-type incision, which is oriented more parallel to the Langer lines. (C) Clinical photo of a healed necklace incision.
While a longitudinal incision affords extensive visualization and exposure of the clavicle, there are reasons to believe that a vertical incision may offer some advantages. One concern after ORIF of the clavicle is persistent numbness over the clavicle, shoulder, and chest4,21 secondary to supraclavicular nerve injury. The nerve branches perpendicularly over the clavicle in a variable manner. Although care is taken to avoid inadvertent injury during ORIF, the varied anatomic positioning of these nerve branches along the midshaft of the clavicle makes them quite susceptible to damage from a longitudinal incision (Figure 2), but they can potentially be better preserved with a necklace-type incision. In addition, a necklace-type incision more closely follows the orientation of the Langer lines of the skin, which may lead to an improved cosmetic result with a smaller scar.15 Incisions following the Langer lines continue to be explored as an important consideration in orthopaedic surgery.5,19
Figure 2.

The supraclavicular nerves have a variable course and lie superficial to the clavicle, and they are at risk of injury during open reduction and internal fixation of the clavicle.
Another complication of ORIF of the clavicle is plate removal22 due to irritating, painful hardware. One recent study found that 86% of a cohort’s reoperations were due to discomfort or pain associated with the plate.6 This may be due to the fact that a scar overlies the plate. A necklace-type incision crosses the plate in a perpendicular manner such that only a minor portion of the plate is covered by scar, which may lower the incidence of symptomatic hardware.
One prior study compared the necklace incision with the longitudinal incision and found an increased incidence of numbness in the longitudinal incision group.20 We hypothesized that patients who had undergone ORIF of OTA type 15-B clavicle fractures with a longitudinal incision may experience increased numbness and painful hardware irritation, leading to an increased incidence of plate removal, compared with those who had the necklace-type incision. We also hypothesized that patients’ satisfaction with their scar cosmesis would affect overall patient satisfaction. To our knowledge, the functional and pain-related impact of the different incision types has not been directly compared.
Methods
The records of 7 orthopaedic surgeons from a single institution were queried for patients who underwent ORIF of OTA type 15-B (diaphyseal) clavicle fractures between 2006 and 2013 using the Current Procedural Terminology (CPT) code 23515 (open treatment of clavicular fracture, includes internal fixation, when performed). All identified patients were contacted and asked to consent by telephone. The study and consent process was approved by the Icahn School of Medicine at Mount Sinai Institutional Review Board.
An online questionnaire was created using the Research Electronic Data Capture (REDcap) system, a secure web application designed to build and manage online surveys specifically for research studies. The survey utilized a design similar to that in a prior study comparing ORIF of clavicle incision types,20 although it included additional questions that we hypothesized would provide further insight, including pain and numbness, American Shoulder and Elbow Surgeons (ASES) scores, scar length, and plate removal incidence. All authors reviewed the survey prior to its being finalized to ensure clarity of language and ease of use in the online format. The survey included questions focused on patient numbness and pain; responses were based on a 5-point scale, with 5 being most severe or extreme. The participants were asked about pain and numbness during the first month after surgery, as well as at the time the survey was completed in order to identify potential differences between shorter and longer term follow-up intervals. Additional sections included scar assessment to measure differences in patient satisfaction with scar appearance and scar length, ASES activities of daily living questionnaire to identify any functional differences between the 2 surgical approaches, and 1 high-level question asking about overall patient satisfaction. Patients were also asked about their dominant arm as well as whether they required any follow-up surgeries after their initial ORIF, specifically for the purpose of symptomatic hardware removal because of pain (ie, not for hardware failure or infection). Additional parameters included age, body mass index (BMI), surgery date, side, mechanism, fracture description, reoperations, incision type, plate size, and screws used.
Inclusion criteria were age older than 18 years, postoperative follow-up of longer than 9 months, closed injuries, and clavicle fractures involving the middle or lateral third, but still diaphyseal. Both simple and comminuted fracture patterns were included in our analysis. Revision ORIFs were excluded. We identified 77 patients who underwent ORIF of the clavicle. Thirty-two of these patients either could not be contacted or declined to participate.
A total of 45 patients consented to the study and completed the online survey. Nine patients did not meet the inclusion criteria, leaving 36 participants included in the final analysis. These 36 patients were divided into 2 groups based on incision type: necklace versus longitudinal. A longitudinal incision was defined as one that was made along the length of the subcutaneous border (long axis) of the clavicle (Figure 1A), while the necklace-type incision was defined as one that was performed along the Langer lines, more perpendicular to the clavicle (Figure 1B). The operating surgeon’s preference for surgical approach as corroborated in the operative note determined the assignment of patients into a specific group.
Continuous variables were analyzed using independent t tests and categorical variables using Pearson chi-square tests. Pearson correlations established associations between specific questions for the cohort as a whole. A P value ≤.05 was considered significant. We used SPSS Statistics (IBM SPSS Statistics for Windows, Version 20.0, IBM Corp) for all statistical analyses.
Results
There were 16 patients in the necklace incision group and 20 in the longitudinal incision group, with a mean follow-up time of 3.2 ± 1.9 years and 3.1 ± 2.4 years, respectively (P = .85). The data from the necklace incision group were derived from 1 surgeon, and data from the longitudinal group were derived from 5 surgeons. All fractures had healed at the time of final follow-up. There were no significant differences found in age, BMI, sex, fracture location, plate size, or number of screws. The necklace incision group had a significantly higher proportion of patients who underwent surgery on their dominant extremity (P = .02). A summary of additional patient characteristics is outlined in Table 1.
TABLE 1.
Patient Characteristicsa
| Necklace Incision (n = 16) | Longitudinal Incision (n = 20) | P | |
|---|---|---|---|
| Age, y | 37.6 ± 10.7 | 44.6 ± 17.5 | .17 |
| Body mass index, kg/m2 | 27.0 ± 13.4 | 25.7 ± 5.3 | .70 |
| Follow-up time, y | 3.2 ± 1.9 | 3.1 ± 2.4 | .85 |
| Dominant side operation | 9 (56) | 4 (20) | .02 |
| Male sex | 13 (81) | 15 (75) | .65 |
| Plate removal | 1 (6) | 4 (20) | .24 |
| Plate size (holes) | 7.9 (1.2) | 8.4 (1.5) | .32 |
| Screws | 7.4 (1.3) | 6.6 (1.3) | .11 |
| Fracture location | |||
| Midshaft | 13 (81) | 15 (75) | |
| Lateral | 2 (13) | 4 (20) | |
| Mechanism | |||
| Bike | 3 (19) | 8 (40) | |
| Motor vehicle | 3 (19) | 4 (20) | |
| Ski/snow | 6 (38) | 1 (5) | |
| Other | 4 (25) | 7 (35) |
aData are expressed either as mean ± SD or n (%). The boldfaced P value denotes a statistically significant value (P ≤ .05).
The necklace incision group was significantly more satisfied with the appearance of their scars (4.3 ± 0.9) versus those who had the longitudinal incision (3.3 ± 1.3) (P = .01). Additionally, while the difference did not reach statistical significance, there was a trend toward a higher overall satisfaction in the necklace incision group, with both groups rating their experience as greater than 4 on the 5-point scale (4.6 ± 0.8 in the necklace group vs 4.1 ± 0.8 in the longitudinal incision group, P = .09). Although the mean scar length was 2.2 cm shorter in the necklace incision group, this difference did not reach significance (P = .12). There were no differences between the 2 groups in the proportion of patients who experienced numbness after surgery (14/16 [87%] vs 18/20 [90%], P = .90) or in the extent that patients were bothered by numbness during the first month (2.3 ± 1.4 vs 2.8 ± 0.9, P = .27) or at latest follow-up (1.8 ± 1.3 vs 1.7 ± 0.8, P = .89). Similarly, no differences were found between the 2 groups with regard to pain, including the amount of pain in the first month (P = .95) and at latest follow-up (P = .57). The survey questions, results, and outcomes of statistical comparisons are outlined in Table 2.
TABLE 2.
Survey Questions and Resultsa
| Question | Scale | Necklace Incision (n = 16) | Longitudinal Incision (n = 20) | P |
|---|---|---|---|---|
| Did you ever experience any numbness in your shoulder, upper chest area, or breast after your clavicle surgery? | Yes/no | 14 (87) | 18 (90) | .81 |
| In your first month after clavicle surgery, to what extent were you bothered by numbness in your shoulder, upper chest area, or breast? | 1-5, 5 being severely | 2.3 ± 1.4 | 2.8 ± 0.9 | .27 |
| In your first month after clavicle surgery, did you notice being more aware of your numbness when wearing shoulder straps (eg, from a bag or clothing)? | 1-5, 5 being extremely | 2.0 ± 1.5 | 2.3 ± 1.4 | .62 |
| How much numbness do you currently have in your shoulder, upper chest area, or breast? | 1-5, 5 being severe | 1.9 ± 1.1 | 1.9 ± 0.7 | .94 |
| To what extent are you currently bothered by numbness in your shoulder, upper chest area, or breast? | 1-5, 5 being severely | 1.8 ± 1.3 | 1.7 ± 0.8 | .89 |
| Do you currently notice being more aware of your numbness when wearing shoulder straps (eg, from a bag or clothing)? | 1-5, 5 being extremely | 1.7 ± 1.4 | 1.6 ± 0.9 | .72 |
| In your first month after clavicle surgery did you have any pain in your shoulder, upper chest area, or breast when wearing shoulder straps (eg, from a bag or clothing)? | 1-5, 5 being extreme pain | 2.9 ± 1.4 | 3.2 ± 1.2 | .44 |
| In your first month after clavicle surgery did you have any pain in your shoulder, upper chest area, or breast when performing an activity requiring you to reach overhead? | 1-5, 5 being extreme pain | 3.5 ± 1.4 | 3.4 ± 1.1 | .72 |
| Do you currently have any pain in your shoulder, upper chest area, or breast when wearing shoulder straps (eg, from a bag or clothing)? | 1-5, 5 being extreme pain | 1.5 ± 1.0 | 1.9 ± 1.0 | .32 |
| Do you currently have any pain in your shoulder, upper chest area, or breast when performing an activity requiring you to reach overhead? | 1-5, 5 being extreme pain | 1.4 ± 0.8 | 1.8 ± 0.9 | .15 |
| Do you currently have any pain in your shoulder, upper chest area, or breast? | 1-5, 5 being extreme pain | 1.3 ± 1.0 | 1.5 ± 0.5 | .60 |
| Overall, how satisfied are you with your clavicle surgery? | 1-5, 5 being extremely | 4.6 ± 0.8 | 4.1 ± 0.8 | .09 |
| How satisfied are you with the appearance of your scar? | 1-5, 5 being extremely | 4.3 ± 0.9 | 3.3 ± 1.3 | .01 |
| What is the length of your scar (in cm)? | Length (cm) | 8.9 ± 2.5 | 11.1 ± 4.5 | .12 |
aData are expressed either as mean ± SD or n (%). The boldfaced P value denotes a statistically significant value (P ≤ .05).
No significant differences in function were found across the 10 ASES questions, and the mean ASES scores were similar (37.0 ± 5.8 vs 36.7 ± 4.1, P = .86) (Table 3). The proportion of patients requiring a secondary surgery for removal of the plate was also similar between groups (1/16 [6%] vs 3/20 [15%], P = .25).
TABLE 3.
ASES Activities of Daily Living Scorea
| Question | Scale | Necklace Incision (n = 16) | Longitudinal Incision (n = 20) | P |
|---|---|---|---|---|
| Put on a coat | 1 = Unable to do 4 = Not difficult | 3.9 ± 0.3 | 3.9 ± 0.4 | .42 |
| Sleep on painful/effected side | 1 = Unable to do 4 = Not difficult | 3.6 ± 0.9 | 3.3 ± 0.8 | .36 |
| Wash back/do up bra in back | 1 = Unable to do 4 = Not difficult | 3.8 ± 0.5 | 3.6 ± 0.5 | .23 |
| Manage toileting | 1 = Unable to do 4 = Not difficult | 3.9 ± 0.3 | 4.0 ± 0.0 | .27 |
| Comb hair | 1 = Unable to do 4 = Not difficult | 3.9 ± 0.3 | 4.0 ± 0.0 | .27 |
| Reach on a high shelf | 1 = Unable to do 4 = Not difficult | 3.7 ± 0.6 | 3.6 ± 0.7 | .53 |
| Lift 10 Ibs over shoulder | 1 = Unable to do 4 = Not difficult | 3.5 ± 1.1 | 3.4 ± 1.0 | .78 |
| Throw a ball overhand | 1 = Unable to do 4 = Not difficult | 3.5 ± 0.9 | 3.6 ± 0.8 | .86 |
| Do usual work | 1 = Unable to do 4 = Not difficult | 3.6 ± 1.0 | 3.7 ± 0.7 | .64 |
| Do usual sport | 1 = Unable to do 4 = Not difficult | 3.6 ± 1.0 | 3.8 ± 0.4 | .47 |
| Combined score | Maximum = 40 | 37.0 ± 5.8 | 36.7 ± 4.1 | .86 |
aData are expressed as mean ± SD. ASES, American Shoulder and Elbow Surgeons.
Pearson correlation analysis demonstrated that satisfaction with the appearance of one’s scar was significantly correlated with overall satisfaction (P = .05) (Table 4). Additionally, significant correlations were observed between the ability to lift 10 lbs (4.5 kg) over one’s shoulder and the ability to throw a ball overhand (Table 4). No correlation was found between the presence of numbness, either early or at latest follow-up, with overall satisfaction.
TABLE 4.
Pearson Correlations With Overall Satisfactiona
| Question | Pearson r | P |
|---|---|---|
| In your first month after clavicle surgery to what extent were you bothered by numbness in your shoulder, upper chest area, or breast? | −0.06 | .71 |
| In your first month after clavicle surgery, did you notice being more aware of your numbness when wearing shoulder straps (eg, from a bag or clothing)? | −0.22 | .19 |
| How much numbness do you currently have in your shoulder, upper chest area, or breast? | −0.10 | .58 |
| To what extent are you currently bothered by numbness in your shoulder, upper chest area, or breast? | −0.20 | .24 |
| Do you currently notice being more aware of your numbness when wearing shoulder straps (eg, from a bag or clothing)? | −0.13 | .45 |
| In your first month after clavicle surgery did you have any pain in your shoulder, upper chest area, or breast when wearing shoulder straps (eg, from a bag or clothing)? | −0.10 | .55 |
| In your first month after clavicle surgery did you have any pain in your shoulder, upper chest area, or breast when performing an activity requiring you to reach overhead? | 0.13 | .47 |
| Do you currently have any pain in your shoulder, upper chest area, or breast when wearing shoulder straps (eg, from a bag or clothing)? | −0.12 | .48 |
| Do you currently have any pain in your shoulder, upper chest area, or breast when performing an activity requiring you to reach overhead? | −0.27 | .11 |
| Do you currently have any pain in your shoulder, upper chest area, or breast? | 0.03 | .85 |
| How satisfied are you with the appearance of your scar? | 0.33 | .05 |
| What is the length of your scar (in cm)? | 0.22 | .22 |
| ASES | ||
| Put on a coat | 0.02 | .89 |
| Sleep on painful/effected side | 0.10 | .56 |
| Wash back/do up bra in back | 0.09 | .60 |
| Manage toileting | −0.14 | .40 |
| Comb hair | −0.14 | .40 |
| Reach on a high shelf | 0.28 | .09 |
| Lift 10 lbs (4.5 kg) over shoulder | 0.41 | .01 |
| Throw a ball overhand | 0.38 | .02 |
| Do usual work | 0.08 | .63 |
| Do usual sport | 0.08 | .66 |
| Total ASES score | 0.24 | .17 |
aThe boldfaced P values denote a statistically significant value (P ≤ .05). ASES, American Shoulder and Elbow Surgeons.
Discussion
We found that after plate fixation of a diaphyseal clavicle fracture, patients who were treated using a necklace-type incision were significantly more satisfied with the appearance of their scar. While the mean length of the necklace incision was 2.2 cm shorter than the mean length of the longitudinal incision, this difference was not statistically significant. Contrary to our initial hypothesis, the necklace incision did not result in a lower incidence of numbness or persistent pain, or a lower rate of revision surgery due to painful hardware. Furthermore, the degree of overall satisfaction did not differ significantly between the 2 groups.
We also found that one of the influential components of overall satisfaction after ORIF of the clavicle may be scar appearance. This was supported by the finding that scar satisfaction across the whole cohort was significantly associated with overall satisfaction.
In some patients, irritative or symptomatic hardware can lead to a second surgery for plate removal.21 Although some of the risk factors that might result in an additional surgery for hardware removal have been explored,2,11 a correlation of the need for plate removal by incision type has not been investigated. We did not find that the incision type influenced the need for hardware removal. However, given the small number of patients who required plate removals within our study (1 and 3 in the necklace and longitudinal groups, respectively), a larger sample size would be needed to determine if incision type affects plate removal incidence.
Our initial hypothesis was that patients would have increased overall satisfaction with a necklace-type incision. This was based in part on the belief that we would observe differences in numbness between the 2 groups that would affect overall satisfaction. Literature related to total knee arthroplasty has shown that numbness after surgery can affect lifestyle and create patient concerns related to the perceived success of the surgery.3,9 The supraclavicular nerve is at risk during ORIF of the clavicle, and damage to the nerve can result in loss of sensation to the clavicle, anteromedial shoulder, and/or proximal chest/breast.8 Rates of numbness after clavicle surgery have been reported to range from 10% to 50%,1,4,17,18,20 and anatomic studies have shown that there is little predictability in the branching of the nerve in the midshaft of the clavicle, where between 69% and 82% of the fractures occur.11,15
Current literature supports the idea that scar appearance can be associated with patient satisfaction. Golkar et al7 studied patients undergoing laparoendoscopic single-site surgery and found that satisfaction was significantly related to scar cosmesis. While preoperative patient concerns were related to safety, postoperative concerns shifted to cosmetic outcomes. Younger patients may tend to value cosmesis after surgery more highly,12 an important fact to consider given the younger average age of patients who undergo ORIF of the clavicle.10 Our study findings support these observations and suggest that a necklace incision may result in a more visually appealing scar. This was confirmed by the positive correlation noted between the patients’ satisfaction with the appearance of the scar and their overall satisfaction.
The effect of incision type on numbness secondary to injury to the supraclavicular cutaneous nerves has been reported. Wang et al20 compared postoperative numbness after plate fixation between patients who received a necklace incision versus patients who received a longitudinal incision, and they noted a reduced incidence and severity of numbness in patients who received a necklace incision. Contrary to our findings, the authors noted that only 3 out of 14 patients who received necklace incisions experienced numbness versus 13 of the 21 patients in the longitudinal incision group. They did not find any significant difference in overall satisfaction.
In concordance with our results, other authors have found no correlation between patient-reported numbness and overall satisfaction.4 This implies that numbness after ORIF of the clavicle is likely not a major factor in overall patient satisfaction. Our data showed that although a large percentage of patients experience some degree of numbness, few are greatly bothered or have their function affected in any significant manner.
We did not find any significant differences in functional outcomes between the 2 groups. Overall outcomes were favorable in both groups, with only the ability to throw a ball overhand (3.5) and ability to lift 10 lbs overhead (3.5) falling at 3.5 or less out of 4 in the combined cohort. These positive functional outcomes are not surprising given the favorable results of ORIF of the clavicle1,14,16 reported in the literature, and they serve to validate the accuracy of the collected data.
This study has several limitations in addition to those inherent to a small retrospective study. First, the follow-up time was not standardized across the different patients. Despite this, the average follow-up interval between the 2 groups was very similar, providing a valid comparison. Furthermore, the data reported for all patients were a minimum of 9 months postsurgery, with the literature showing that changes in numbness tend to occur during the first 6 months after surgery before stabilizing.4 The fact that all data were self-reported by patients rather than collected clinically may be considered an additional limitation. However, subjective criteria such as numbness, pain, and satisfaction are likely most accurate as self-reported scores. Many of our results are consistent with prior studies, and we believe that this is a valid collection method.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: J.N.G. receives honoraria from Mitek. J.M.K. receives honoraria from MicroAire. B.O.P. receives honoraria from Arthrex and Zimmer.
Ethical approval for this study was obtained from Icahn School of Medicine at Mount Sinai Institutional Review Board (HS# 14-01112).
References
- 1. Altamimi SA, McKee MD; and Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. Surgical technique. J Bone Joint Surg Am. 2008;90(suppl 2 pt 1):1–8. [DOI] [PubMed] [Google Scholar]
- 2. Ashman BD, Slobogean GP, Stone TB, et al. Reoperation following open reduction and plate fixation of displaced mid-shaft clavicle fractures. Injury. 2014;45:1549–1553. [DOI] [PubMed] [Google Scholar]
- 3. Borley NR, Edwards D, Villar RN. Lateral skin flap numbness after total knee arthroplasty. J Arthroplasty. 1995;10:13–14. [DOI] [PubMed] [Google Scholar]
- 4. Christensen TJ, Horwitz DS, Kubiak EN. Natural history of anterior chest wall numbness after plating of clavicle fractures: educating patients. J Orthop Trauma. 2014;28:642–647. [DOI] [PubMed] [Google Scholar]
- 5. Ciais G, Waitzenegger T, Parot C, Leclercq C. Universal dorsal approach of the wrist. Tech Hand Up Extrem Surg. 2015;19:124–128. [DOI] [PubMed] [Google Scholar]
- 6. Fridberg M, Ban I, Issa Z, Krasheninnikoff M, Troelsen A. Locking plate osteosynthesis of clavicle fractures: complication and reoperation rates in one hundred and five consecutive cases. Int Orthop. 2013;37:689–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Golkar FC, Ross SB, Sperry S, et al. Patients’ perceptions of laparoendoscopic single-site surgery: the cosmetic effect. Am J Surg. 2012;204:751–761. [DOI] [PubMed] [Google Scholar]
- 8. Havet E, Duparc F, Tobenas-Dujardin AC, Muller JM, Freger P. Morphometric study of the shoulder and subclavicular innervation by the intermediate and lateral branches of supraclavicular nerves. Surg Radiol Anat. 2007;29:605–610. [DOI] [PubMed] [Google Scholar]
- 9. Hopton BP, Tommichan MC, Howell FR. Reducing lateral skin flap numbness after total knee arthroplasty. Knee. 2004;11:289–291. [DOI] [PubMed] [Google Scholar]
- 10. Khan LA, Bradnock TJ, Scott C, Robinson CM. Fractures of the clavicle. J Bone Joint Surg Am. 2009;91:447–460. [DOI] [PubMed] [Google Scholar]
- 11. Leroux T, Wasserstein D, Henry P, et al. Rate of and risk factors for reoperations after open reduction and internal fixation of midshaft clavicle fractures: a population-based study in Ontario, Canada. J Bone Joint Surg Am. 2014;96:1119–1125. [DOI] [PubMed] [Google Scholar]
- 12. Lucas SM, Baber J, Sundaram CP. Determination of patient concerns in choosing surgery and preference for laparoendoscopic single-site surgery and assessment of satisfaction with postoperative cosmesis. J Endourol. 2012;26:585–591. [DOI] [PubMed] [Google Scholar]
- 13. Marsh JL, Slongo TF, Agel J, et al. Fracture and dislocation classification compendium—2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007;21(suppl 20):S1–S133. [DOI] [PubMed] [Google Scholar]
- 14. McKee RC, Whelan DB, Schemitsch EH, McKee MD. Operative versus nonoperative care of displaced midshaft clavicular fractures: a meta-analysis of randomized clinical trials. J Bone Joint Surg Am. 2012;94:675–684. [DOI] [PubMed] [Google Scholar]
- 15. Redfern TR, Owen R. The transverse posterior approach to the neck. J Bone Joint Surg Br. 1985;67:616–617. [DOI] [PubMed] [Google Scholar]
- 16. Robinson CM, Goudie EB, Murray IR, et al. Open reduction and plate fixation versus nonoperative treatment for displaced midshaft clavicular fractures: a multicenter, randomized, controlled trial. J Bone Joint Surg Am. 2013;95:1576–1584. [DOI] [PubMed] [Google Scholar]
- 17. Shen WJ, Liu TJ, Shen YS. Plate fixation of fresh displaced midshaft clavicle fractures. Injury. 1999;30:497–500. [DOI] [PubMed] [Google Scholar]
- 18. Strauss EJ, Egol KA, France MA, Koval KJ, Zuckerman JD. Complications of intramedullary Hagie pin fixation for acute midshaft clavicle fractures. J Shoulder Elbow Surg. 2007;16:280–284. [DOI] [PubMed] [Google Scholar]
- 19. Sundaram RO, Ramakrishnan M, Harvey RA, Parkinson RW. Comparison of scars and resulting hypoaesthesia between the medial parapatellar and midline skin incisions in total knee arthroplasty. Knee. 2007;14:375–378. [DOI] [PubMed] [Google Scholar]
- 20. Wang K, Dowrick A, Choi J, Rahim R, Edwards E. Post-operative numbness and patient satisfaction following plate fixation of clavicular fractures. Injury. 2010;41:1002–1005. [DOI] [PubMed] [Google Scholar]
- 21. Wang L, Ang M, Lee KT, Naidu G, Kwek E. Cutaneous hypoesthesia following plate fixation in clavicle fractures. Indian J Orthop. 2014;48:10–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wijdicks FJ, Van der Meijden OA, Millett PJ, Verleisdonk EJ, Houwert RM. Systematic review of the complications of plate fixation of clavicle fractures. Arch Orthop Trauma Surg. 2012;132:617–625. [DOI] [PMC free article] [PubMed] [Google Scholar]


