Abstract
Background:
Although numerous studies have assessed arthroscopic medial meniscal repairs, few studies have focused on factors affecting outcomes of vertical longitudinal and bucket-handle repairs.
Purpose:
To evaluate the factors affecting clinical outcomes of arthroscopically repaired traumatic vertical longitudinal and bucket-handle medial meniscal tears.
Study Design:
Case series; Level of evidence, 4.
Methods:
A total of 223 patients underwent arthroscopic repair for medial meniscal tears between 2007 and 2012; 140 patients had isolated tears or concurrent anterior cruciate ligament (ACL) reconstruction, and 80 patients (76 men, 4 women; mean age, 29.1 years; range, 18-49 years) had vertical longitudinal tears and were included in the study. Pre- and postoperative functional status was assessed using physical examinations with Lysholm and International Knee Documentation Committee (IKDC) scores. Barrett criteria were used for clinical assessment of meniscal healing, and magnetic resonance imaging (MRI) was used as the radiologic assessment method. The effects of tear location, length, chronicity, and type; suturing technique; concurrent ACL reconstruction; and patient age, sex, and smoking habits were also investigated.
Results:
The mean follow-up period was 51.2 ± 9.4 months (range, 34-85 months). The mean Lysholm and IKDC scores improved at final follow-up (both Ps <.001). According to clinical scores, Barrett criteria, and MRI, failure was noted in 12 patients (15%). There were no significant differences in age, tear length, tear type, concurrent ACL rupture, suturing technique, or location of the meniscal repair between the success and failure groups. Failure rates were higher for red-white zone tears than for red-red zone tears (10/30, 33.3% vs 2/50, 4%; P = .004). Tear chronicity significantly affected failure rates. Early repairs had higher healing rates than late repairs (100% vs 73.4%; P = .008). Failure rates were higher for smokers than for nonsmokers (9/24, 37.5% vs 3/56, 5.3%; P = .008).
Conclusion:
Peripheral tears and early repairs have better outcomes and patient satisfaction. Smoking adversely affects meniscal healing.
Keywords: medial meniscus, vertical longitudinal, meniscal repair, arthroscopy
The menisci in the knees resist different forces, such as tension, compression, and shear stress. They play a crucial role in force distribution, shock absorption, articular cartilage protection, proprioception, joint stabilization, and joint lubrication.28 Thus, there is an increased awareness of the importance of meniscal preservation. Long-term studies have shown that, after meniscectomy, there is an increased incidence of radiological signs of arthritis.6,32 Arthroscopic repair of torn menisci has therefore become the mainstay treatment method if repair is possible.41 Inside-out,8,18 outside-in,43 and all-inside repair37—currently widely used—are the accepted arthroscopic repair techniques.15 Surgeons must consider many factors that may affect the results of meniscal repairs, including tear location, chronicity, size, and extent; repair technique; patient age and habits; and the presence of associated injuries. Most successful results have been reported after treatment of longitudinal acute tears in the peripheral vascular zone of the meniscus and in young individuals with stable knees.17,36 Additionally, medial meniscal repairs are less likely to heal than are lateral meniscal repairs.4,7,13 Previous studies have shown failure rates of up to 40% for medial meniscal repairs.20,29,35
While there are many studies related to meniscal repair in the literature, there are few related to the results of medial meniscal repair,1,11 and those showing results of longitudinal medial meniscal tears are rare.2,16 We hypothesized that specific factors may enhance the success of vertical longitudinal and bucket-handle medial meniscal repair and that superior clinical results could be obtained. Thus, the purpose of this study was to evaluate the clinical outcomes of vertical longitudinal and bucket-handle medial meniscal repairs and investigate the factors affecting the outcomes.
Methods
Patients
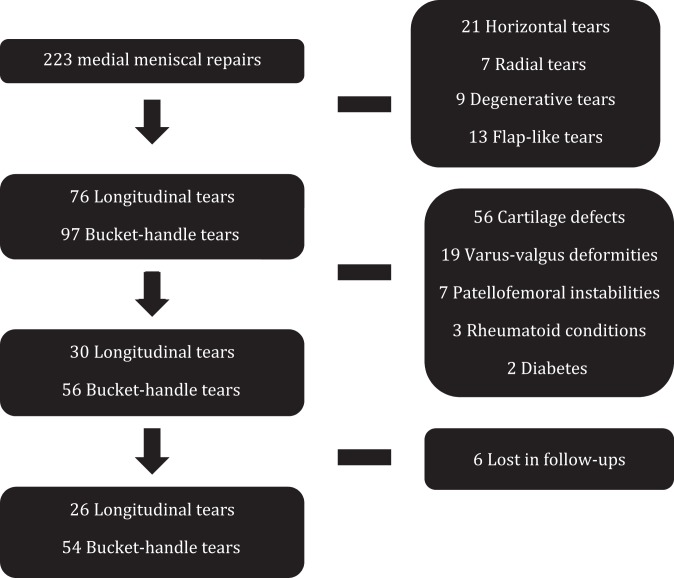
Included in this retrospective study were 233 patients with a medial meniscal tear who underwent arthroscopic medial meniscal repair with or without anterior cruciate ligament (ACL) reconstruction or cartilage procedure between September 2007 and October 2012 and who attended 1-, 6-, 12-, 24-, 48-, and 60-month follow-up visits. The inclusion criteria were as follows: an arthroscopic medial meniscal repair with or without an ACL rupture, a meniscal tear due to trauma or sports injury, a repair involving a displaced (bucket-handle) or nondisplaced vertical longitudinal tear that was 15 to 35 mm in length, and a rupture involving the red-red (RR; within 3 mm of the meniscocapsular junction) or red-white (RW; 3-5 mm from the meniscocapsular junction) zones. Patients were excluded if they had a previous history of knee surgery, a follow-up duration of less than 24 months, degenerative knee osteoarthritis, pathologic conditions in addition to meniscal and/or ACL rupture (eg, cartilage defect), a meniscal tear greater than 35 mm in size, degenerative horizontal or flap-like tears, more than 5° of knee valgus or varus deformity, clinical patellofemoral joint instability, rheumatoid conditions, or diabetes. Patients who did not attend regular follow-up visits were also excluded (Figure 1). After exclusions, 80 patients were included for the study. Of these, 76 patients were men and 4 were women. The study was approved by our hospital research ethics committee.
Figure 1.
Study flowchart and patient exclusion details.
Surgical Method
All patients underwent surgery by the same surgeon. After completion of diagnostic arthroscopy, attention was turned to the medial meniscus. After the meniscal disorder was defined, both edges of the tear were refreshed and a repair was performed using an all-inside (especially for involvement of the posterior two-thirds of the meniscus) or hybrid (especially for involvement of the anterior one-third of the meniscus) suture method with a vertical oblique mattress configuration. For the all-inside repair technique, Fast-Fix anchors (Fast-Fix 360, Smith & Nephew) were used. Depending on the length and stability of the tear, 1 to 5 implants were used. For hybrid repair, Fast-Fix sutures were placed posteriorly and additional outside-in sutures were used for the anterior horn. The outside-in repair technique was performed with absorbable No. 0 polydioxanone II sutures (PDS, Ethicon). All patients with ACL tears underwent a single-bundle reconstruction using autogenous hamstring tendons.
Postoperative Rehabilitation
Patients were mobilized with an angle adjustable brace in order to protect repaired menisci and were allowed only partial weightbearing for the first 6 weeks. Patients with repairs of bucket-handle tears were immobilized in full extension for 2 weeks. Isometric quadriceps and hamstring exercises commenced on postoperative day 1, as did knee movements using a continuous passive motion device. Patients were discharged when they could perform a straight-leg raise and flex the knee to 90°. After 3 weeks, quadriceps muscle exercises with weights were initiated. Six weeks after the surgery, full range of motion and unlimited weightbearing were allowed. Running, squatting, and pivoting were allowed 3, 5, and 6 months after surgery, respectively. Re-initiation of sports activities was allowed at the end of the sixth month.
Other Factors
During the operation, we recorded the meniscal tear patterns, the total number of stitches (all-inside and outside-in), and the location of the tear (anterior, middle, or posterior horn). Based on tear patterns, meniscal tears were categorized into 2 types: nondisplaced vertical longitudinal or displaced vertical longitudinal (bucket-handle) tears. For tear size, because the actual size was difficult to measure, we used an intraoperative scale. We recorded meniscocapsular junction tears and tears within the peripheral RR zone extending to 3 mm of the meniscal peripheral rim as RR, and those from 3 to 5 mm as RW.9
Assessments
At follow-up, all patients were examined clinically and radiologically by an independent examiner. Patient-reported outcomes were assessed preoperatively with the International Knee Documentation Committee (IKDC) rating18 and Lysholm score.39 A 1.5-T magnetic resonance imaging (MRI) scanner (Intera, Philips Electronics NV) was used preoperatively and postoperatively at the last follow-up. Coronal, sagittal, and axial sections with both T1- and T2-weighted sequences were examined. For postoperative follow-up assessments, patient improvement and satisfaction were measured by clinical scores. Functional IKDC status was graded as A (normal), B (nearly normal), C (abnormal), or D (severely abnormal). In addition, Barrett criteria were used for clinical assessment of the healing status of the repaired meniscus,3 in which the absence of joint tenderness, effusion, and the presence of a negative McMurray test indicated a healed meniscus. A negative outcome (defined as having at least 1 positive Barrett criterion) or the need for revision surgery indicated clinical failure. Also, grade 3 signals on postoperative T2-weighted MRI sequences were considered an unhealed meniscus. Fluid within the repair site was considered a failure.15 The effect of concurrent ACL reconstruction, tear location (anterior, middle, and posterior horn of the meniscus), tear zone (RR or RW region), tear length (≥25 vs <25 mm), tear chronicity (≥8 vs <8 wk), tear type (longitudinal, bucket-handle), suture technique (all-inside vs hybrid), patient age (≥30 vs <30 years), and smoking habits were also investigated with regard to clinical improvement results.
Statistical Analysis
Data were analyzed with SPSS version 15 for Windows (IBM Corp). As measures of central location and spread of data, means and standard deviations or medians and ranges were calculated. Nonparametric tests were used because the data were not normally distributed. The Mann-Whitney U test or Kruskal-Wallis test was used for intergroup comparisons of continuous variables, depending on the number of groups compared, and the Wilcoxon test was used for intragroup comparisons (last follow-up vs baseline). The chi-square test was used to compare the incidence of failure in subgroups of patients with different characteristics. A P value <.05 indicated statistical significance.
Results
Of the 80 study patients, 24 underwent medial meniscal repair only, and 56 underwent concurrent ACL reconstruction. The mean patient age was 29.1 ± 7.3 years (range, 18-49 years). All tears were located medially. Distribution of age, time of repair, ACL reconstruction, zone of tears, length of tears, tear shape, affected knee side, repair technique, tear region, and smoking habits in successful and failed repairs are shown in Table 1. Partial meniscectomy was performed for 5 mixed tears. The mean number of suture devices used was 2.3 (range, 1-5), and the mean number of PDS sutures used for outside-in repair was 2.2 (range, 1-4). The mean follow-up period was 51.2 ± 9.4 months (range, 34-85 months). The mean time between trauma and surgery was 5.6 weeks (range, 1-36 weeks).
TABLE 1.
Summary of Factors Affecting the Outcomes for Patients Who Underwent Meniscal Repaira
| Meniscal Repairs, n (%) | Successful Repairs, n (%) | Failed Repairs, n (%) | P Valueb | |
|---|---|---|---|---|
| Age, y | .76 | |||
| <30 | 48 (60) | 40 (83.4) | 8 (16.6) | |
| ≥30 | 32 (40) | 28 (87.5) | 4 (12.5) | |
| Time of repair, wk | .008 | |||
| <8 | 35 (43.8) | 35 (100) | 0 (0) | |
| ≥8 | 45 (56.3) | 33 (73.4) | 12 (26.6) | |
| ACL reconstruction | .62 | |||
| With | 56 (70) | 48 (85.8) | 8 (14.2) | |
| Without | 24 (30) | 20 (83.4) | 4 (16.6) | |
| Zone of tears | .004 | |||
| RR | 50 (62.5) | 48 (96) | 2 (4) | |
| RW | 30 (37.5) | 20 (66.7) | 10 (33.3) | |
| Length of tears, mm | .93 | |||
| <25 | 51 (63.8) | 44 (86.3) | 7 (13.7) | |
| ≥25 | 29 (36.3) | 24 (82.8) | 5 (17.2) | |
| Shape of tears | .63 | |||
| Longitudinal | 26 (32.5) | 22 (84.7) | 4 (15.3) | |
| Bucket-handle | 54 (67.5) | 46 (85.2) | 8 (14.8) | |
| Affected side | .27 | |||
| Right | 46 (57.5) | 41 (89.2) | 5 (10.8) | |
| Left | 34 (42.5) | 27 (79.5) | 7 (20.5) | |
| Repair technique | .76 | |||
| All-inside | 46 (57.5) | 38 (82.7) | 8 (17.3) | |
| Hybrid | 34 (42.5) | 30 (88.3) | 4 (11.7) | |
| Tear region | .95 | |||
| Anterior 2/3 | 15 (18.8) | 12 (80) | 3 (20) | |
| Posterior 2/3 | 24 (30) | 21 (87.5) | 3 (12.5) | |
| Posterior 1/3 | 33 (41.3) | 29 (87.9) | 4 (12.1) | |
| Total failure | 8 (100) | 6 (75) | 2 (25) | |
| Smoking habit | .008 | |||
| Smokers | 24 (30) | 15 (62.5) | 9 (37.5) | |
| Nonsmokers | 56 (70) | 53 (94.7) | 3 (5.3) |
aP values in boldface indicate statistical significance. ACL, anterior cruciate ligament; RR, red-red (within 3 mm of the meniscocapsular junction); RW, red-white (3-5 mm from the meniscocapsular junction).
bChi-square test.
Clinical Assessment
Preoperatively, the mean Lysholm score was 48 (range, 32-76), which improved to 91.8 (range, 44-100) (P < .001) at the last follow-up. IKDC scores also improved significantly (P < .001) (Table 2). Preoperative and postoperative IKDC scores of patients are shown in Table 3. Of the 80 patients (76 men and 4 women) included in this study, 72 (90%) had no complaints at the last follow-up, which indicated clinical success with no or minimal limitations in daily life. According to clinical examination and Barrett criteria, the clinical failure rate was 10% (8 patients) at the last follow-up. MRI showed failure of healing in all of the clinical failures. Additionally, asymptomatic unhealed tears were observed in 4 patients. Patients who achieved clinical success at the last follow-up returned to their preoperative activity levels within 4 to 6 months after surgery. Two patients treated with the outside-in technique had superficial infection around the suture material on the capsule. They were treated with soft tissue debridement and parenteral antibiotics.
TABLE 2.
Functional Resultsa
| Evaluation Method | Preoperative Score | Postoperative Score | P Value |
|---|---|---|---|
| Lysholm (mean ± SD) | 48 ± 10.1 | 91.8 ± 13.7 | <.001b |
| IKDC, median (range) | 4 (2-4) | 1 (1-4) | <.001c |
aIKDC, International Knee Documentation Committee.
bPaired-samples t test.
cWilcoxon signed-rank test.
TABLE 3.
Pre- and Postoperative IKDC Scores of Patientsa
| IKDC Score | Preoperative, n (%) | Postoperative, n (%) |
|---|---|---|
| A | 0 (0) | 50 (62.5) |
| B | 9 (11.3) | 13 (16.3) |
| C | 19 (23.7) | 9 (11.3) |
| D | 52 (65) | 8 (10) |
aIKDC, International Knee Documentation Committee.
Factors Affecting Clinical Outcomes
With regard to the failure rates as a midterm clinical result of medial meniscal vertical longitudinal tear repair, there were no significant differences between age groups (<30 vs ≥30 years), affected knee side, tear length (<25 vs ≥25 mm), tear type (longitudinal vs bucket-handle), presence of additional pathology (meniscal repair only vs concurrent ACL reconstruction), suturing technique (all-inside vs hybrid repair), or location of repair (anterior, middle, or posterior horn) of the meniscus (P > .05). However, higher failure rates were detected in RW zone repairs compared with RR zone repairs (10 of 30, 33.3% vs 2 of 50, 4%) (P = .004), repairs performed ≥8 weeks after injury (12 of 45, 26.6% vs 0 of 35, 0%) (P = .008) and in smokers (9 of 24, 37.5% vs 3 of 56, 5.3%) (P = .008) (Table 1).
Discussion
This study suggests that all-inside and hybrid repair for traumatic vertical longitudinal and bucket-handle meniscal tears are effective repair methods with low clinical failure rates. We used only vertically oriented sutures, which have the strongest pullout strength.14,38 Other repair techniques may have different results.
The tear location, suture type, and tear type do not affect clinical results. Meniscal repair in conjunction with ACL reconstruction does not result in clinical superiority over meniscal repair alone. However, because of their richer vascularity, peripheral tears and early repairs have better outcomes, and smoking adversely affects meniscal healing.
Different methods of assessing meniscal healing have been reported, including physical examination, second-look arthroscopy, and MRI.32,33 Miao et al32 compared these techniques and found that strict clinical evaluation underestimates the healing rate compared with that determined by MRI or second-look arthroscopy. However, physical examination is still an accepted assessment tool because routine second-look arthroscopy or MRI investigation of every patient to assess meniscal healing is not feasible in routine clinical practice. The definition of healing and failure in the present study included clear evidence of clinical failure and MRI investigation.
Most studies involve a postoperative follow-up duration of up to 2 years. According to Lee and Diduch,27 30% of all failures occur after an average follow-up of 2 years. These authors found increased failure rates in the longer term. Furthermore, as noted in a recent review by Nepple et al,34 it has been found that meniscal repair may fail after several years and that a conventional 2-year follow-up evaluation might underestimate the total failure rate. In the current study, the average follow-up was 51.2 months, which may be considered adequate for the assessment of meniscal healing.
Previous studies have shown failure rates of up to 40% for medial meniscal repairs.27 The posterior horn of the medial meniscus is especially subject to anterior-posterior shear force,42 which may be the possible cause of medial meniscal repair failure, especially in ACL-deficient knees.
Stability of the knee is of primary significance in patients undergoing meniscal repair, and ACL reconstruction should be performed in patients with coexistent ACL injury. Since ACL surgery is associated with considerable intra-articular trauma, excessive bleeding and fibrin clots within the joint space are thought to have a benefit on the healing process.44 Accordingly, some studies have demonstrated that concomitant ACL reconstruction during meniscal repair improves the outcomes of the repair.2,15,23,30,31 An association with higher success rates for concurrent ACL reconstruction and medial meniscal repair is generally shown in short-term comparisons.21,44 In contrast, in a meta-analysis by Nepple et al,34 in which long-term results of meniscal repair were evaluated, no differences were found in success rates with regard to the presence of ACL rupture. In our study, concurrent ACL reconstruction and meniscal repair was found to have a similar failure rate as isolated meniscal repair (14.2% vs 16.6%)
Numerous studies have reported results of meniscal repair. A meta-analysis noted that most authors reported Lysholm scores of 90 or greater and IKDC ratings of normal or nearly normal.34 Our results were consistent with those results, with a mean postoperative Lysholm score of 91.8 and 79% of the IKDC scores of A or B. In the literature, different healing rates have been reported for arthroscopic medial meniscal repairs with different suture techniques.9 Haklar et al15 reported an overall healing rate of 88.4%, which increased to 91% with concomitant ACL reconstruction. Similarly, Ahn et al1 reported a 96.4% clinical success rate with concomitant ACL reconstruction. Among 39 patients, Ahn et al2 reported only 1 failure (2.6%) with the all-inside suture technique for medial meniscal lesions in ACL-deficient knees. In contrast, Koukoulias et al24 reported a 27.3% clinical failure rate in their study of medial meniscal repairs with the all-inside method in ACL-deficient knees. For chronic bucket-handle tears of the medial meniscus, Noyes et al36 reported a 17% failure rate with the inside-out and outside-in methods. In a comparison of the all-inside and inside-out suture repair techniques for medial meniscal repair, Choi et al9 found no difference between the 2 techniques. In the current study, we showed a failure rate of 15%, comparable to those reported in the literature. The addition of the outside-in method to the all-inside approach did not result in a difference in clinical outcomes, similar to what Kalliakmanis et al21 reported previously. Thus, previous studies demonstrated that a vertical suture pattern has the highest pull-out strength and superior load-to-failure strength.37,45 We used a vertical or oblique suture pattern for all tears. Some patients who were treated with the outside-in technique had short-term complications, suggesting that the use of the all-inside method may be an effective strategy for reducing the short-term complication rate.
In our study, we found that tear length did not significantly affect the outcome, similar to a study by Kotsovolos et al.23 In contrast, Haklar et al15 reported that if the tear length was >2 cm, it significantly affected meniscal healing negatively.
The zone of the tear with regard to the blood supply is a major factor affecting the results of meniscal repair. RR zone tears are expected to heal more readily than those in the RW zone. Our study had similar findings to Krych et al26 and Ahn et al.1 Outcomes for repairs involving the RR zone were significantly better than those for repairs involving the RW zone. However, many investigators have shown no difference in healing between RR and RW zone tears.12,22,24,30,34
In our study, patient age did not significantly affect outcomes. In agreement with our results, many authors also found no significant differences between younger and older age groups with regard to meniscal healing.1,16,22,29,30 In contrast, Tengrootenhuysen et al40 reported higher failure rates in older patients.
The effect on outcomes of the time from injury to repair for meniscal tears is controversial. Although most authors reported no effect of time from injury to repair for meniscal tear healing,16,19,22,24,30,36 some did report an effect of tear chronicity.4,11,40 Our results agree with the latter. In all failed cases, meniscal repair was performed after 8 weeks from the injury.
There are few studies comparing the clinical success rates of meniscal repairs performed in different anatomic meniscal regions. Cipolla et al10 reported that the anterior and posterior horns of the menisci are better vascularized than the middle horn. It is thought that tears in middle horn have poorer outcomes than do tears in the anterior and posterior horns. Kraus et al25 reported that all recurrent tears were located in the middle horn, and they concluded that the quality of healing in this zone might be inferior. In contrast with these studies, we found that the failure rates were similar and there was no significant difference between the repairs of different anatomic regions of the menisci.
Haklar et al15 reported that smoking negatively influenced medial meniscal healing. Blackwell et al5 also found a higher risk of early meniscal repair failure in smokers. In concordance with the literature, we found that smoking had a negative effect on meniscal healing.
This study has some limitations. First, it was a retrospective study. However, to avoid bias, all data were collected prospectively. Second, to assess the success rate, clinical examination and MRI were used as outcome measures to analyze the results, not the more objective second-look arthroscopy. Thus, it was difficult to address definitive meniscal healing accurately. Third, we examined a large number of parameters in a relatively small number of participants. Also, our results are only valid for peripheral longitudinal, traumatic tears. Results will likely be worse with other tear patterns. We did not investigate outside-in techniques or other all-inside devices. Results may be different for these. A large number of patients underwent concomitant ACL reconstruction, which likely had a greater effect on the improvement in Lysholm and IKDC scores than the meniscal repair did. Future studies with more participants and more homogenous populations are needed to determine the factors that may affect the healing rate of repaired medial menisci.
Conclusion
The midterm results of medial meniscal repair in this study suggest that all-inside and hybrid repair with Fast-Fix suture anchors for traumatic vertical longitudinal meniscal tears are effective repair methods with low failure rates. The tear location, suture type, and tear type did not affect clinical results. Meniscal repair in conjunction with ACL reconstruction did not result in clinical superiority over meniscal repair alone. However, due to their richer vascularity, peripheral tears and early repairs had better outcomes with higher satisfaction rates, and smoking adversely affected meniscal healing.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
Ethical approval for this study was obtained from the Erciyes Unversity Clinical Investigations Ethics Committee.
References
- 1. Ahn JH, Lee YS, Yoo JC, Chang MJ, Koh KH, Kim MH. Clinical and second-look arthroscopic evaluation of repaired medial meniscus in anterior cruciate ligament–reconstructed knees. Am J Sports Med.2010;38:472–477. [DOI] [PubMed] [Google Scholar]
- 2. Ahn JH, Wang JH, Yoo JC. Arthroscopic all-inside suture repair of medial meniscus lesion in anterior cruciate ligament–deficient knees: results of second-look arthroscopies in 39 cases. Arthroscopy. 2004;20:936–945. [DOI] [PubMed] [Google Scholar]
- 3. Barrett GR, Field MH, Treacy SH, Ruff CG. Clinical results of meniscus repair in patients 40 years and older. Arthroscopy. 1998;14:824–829. [DOI] [PubMed] [Google Scholar]
- 4. Bellabarba C, Bush-Joseph CA, Bach BR., Jr Patterns of meniscal injury in the anterior cruciate–deficient knee: a review of the literature. Am J Orthop (Belle Mead NJ). 1997;26:18–23. [PubMed] [Google Scholar]
- 5. Blackwell R, Schmitt L, Flanigan DC, Magnussen RA. Smoking increases the risk of early meniscus repair failure. Knee Surg Sports Traumatol Arthrosc. 2016;24:1540–1543. [DOI] [PubMed] [Google Scholar]
- 6. Bonneux I, Vandekerckhove B. Arthroscopic partial lateral meniscectomy long-term results in athletes. Acta Orthop Belg. 2002;68:356–361. [PubMed] [Google Scholar]
- 7. Buckland MD, Sadoghi P, Wimmer MD, et al. Meta-analysis on biomechanical properties of meniscus repairs: are devices better than sutures? Knee Surg Sports Traumatol Arthrosc. 2015;23:83–89. [DOI] [PubMed] [Google Scholar]
- 8. Cannon WD., Jr Arthroscopic meniscal repair. Inside-out technique and results. Am J Knee Surg. 1996;9:137–143. [PubMed] [Google Scholar]
- 9. Choi NH, Kim TH, Victoroff BN. Comparison of arthroscopic medial meniscal suture repair techniques: inside-out versus all-inside repair. Am J Sports Med. 2009;37:2144–2150. [DOI] [PubMed] [Google Scholar]
- 10. Cipolla M, Cerullo G, Puddu G. Microvasculature of the human medial meniscus: operative findings. Arthroscopy. 1992;8:522–525. [DOI] [PubMed] [Google Scholar]
- 11. Cooper DE, Arnoczky SP, Warren RF. Meniscal repair. Clin Sports Med. 1991;10:529–548. [PubMed] [Google Scholar]
- 12. Ellermann A, Siebold R, Buelow JU, Sobau C. Clinical evaluation of meniscus repair with a bioabsorbable arrow: a 2- to 3-year follow-up study. Knee Surg Sports Traumatol Arthrosc. 2002;10:289–293. [DOI] [PubMed] [Google Scholar]
- 13. Farng E, Sherman O. Meniscal repair devices: a clinical and biomechanical literature review. Arthroscopy. 2004;20:273–286. [DOI] [PubMed] [Google Scholar]
- 14. Haas AL, Schepsis AA, Hornstein J, Edgar CM. Meniscal repair using the FasT-Fix all-inside meniscal repair device. Arthroscopy. 2005;21:167–175. [DOI] [PubMed] [Google Scholar]
- 15. Haklar U, Donmez F, Basaran SH, Canbora MK. Results of arthroscopic repair of partial-or full-thickness longitudinal medial meniscal tears by single or double vertical sutures using the inside-out technique Am J Sports Med. 2013;41:596–602. [DOI] [PubMed] [Google Scholar]
- 16. Heckmann TP, Barber-Westin SD, Noyes FR. Meniscal repair and transplantation: indications, techniques, rehabilitation, and clinical outcome. J Orthop Sports Phys Ther. 2006;36:795–814. [DOI] [PubMed] [Google Scholar]
- 17. Henning CE. Arthroscopic repair of meniscal tears. Orthopaedics. 1983;6:1130–1132. [DOI] [PubMed] [Google Scholar]
- 18. Hurel C, Mertens F, Verdonk R. Biofix resorbable meniscus arrow for meniscal ruptures: results of a 1-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2000;8:46–52. [DOI] [PubMed] [Google Scholar]
- 19. Irrgang JJ, Ho H, Harner CD, Fu FH. Use of the International Knee Documentation Committee guidelines to assess outcome following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 1998;6:107–114. [DOI] [PubMed] [Google Scholar]
- 20. Jones HP, Lemos MJ, Wilk RM, Smiley PM, Gutierrez R, Schepsis AA. Two-year follow-up of meniscal repair using a bioabsorbable arrow. Arthroscopy. 2002;18:64–69. [DOI] [PubMed] [Google Scholar]
- 21. Kalliakmanis A, Zourntos S, Bousgas D, Nikolaou P. Comparison of arthroscopic meniscal repair results using 3 different meniscal repair devices in anterior cruciate ligament reconstruction patients. Arthroscopy. 2008;24:810–816. [DOI] [PubMed] [Google Scholar]
- 22. Konan S, Haddad FS. Outcomes of meniscal preservation using all-inside meniscus repair devices. Clin Orthop Relat Res. 2010;468:1209–1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kotsovolos ES, Hantes ME, Mastrokalos DS, Lorbach O, Paessler HH. Results of all-inside meniscal repair with the FasT-Fix meniscal repair system. Arthroscopy. 2006;22:3–9. [DOI] [PubMed] [Google Scholar]
- 24. Koukoulias N, Papastergiou S, Kazakos K, Poulios G, Parisis K. Mid-term clinical results of medial meniscus repair with the meniscus arrow in the unstable knee. Knee Surg Sports Traumatol Arthrosc. 2007;15:138–143. [DOI] [PubMed] [Google Scholar]
- 25. Kraus T, Heidari N, Švehlík M, Schneider F, Sperl M, Linhart W. Outcome of repaired unstable meniscal tears in children and adolescents. Acta Orthop. 2012;83:261–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Krych AJ, McIntoch AL, Voll AE, Stuart MJ, Dahm DL. Arthroscopic repair of isolated meniscal tears in patients 18 years and younger. Am J Sports Med. 2008;36:1283–1289. [DOI] [PubMed] [Google Scholar]
- 27. Lee GP, Diduch DR. Deteriorating outcomes after meniscal repair using the meniscus arrow in knees undergoing concurrent anterior cruciate ligament reconstruction: increased failure rate with long-term follow-up. Am J Sports Med. 2005;33:1138–1141. [DOI] [PubMed] [Google Scholar]
- 28. Logan M, Watts M, Owen J, Myers P. Meniscal repair in the elite athlete: results of 45 repairs with a minimum 5-year follow-up. Am J Sports Med. 2009;37:1131–1134. [DOI] [PubMed] [Google Scholar]
- 29. Majeed H, Karuppiah S, Sigamoney KV, Geutjens G, Straw RG. All-inside meniscal repair surgery: factors affecting the outcome. J Orthop Traumatol. 2015;16:245–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. McCarthy EC, Marx RG, DeHaven KE. Meniscus repair: considerations in treatment and update of clinical results. Clin Orthop Relat Res. 2002;402:122–134. [PubMed] [Google Scholar]
- 31. McDermott ID, Amis AA. The consequences of meniscectomy. J Bone Joint Surg Br. 2006;88:1549–1556. [DOI] [PubMed] [Google Scholar]
- 32. Miao Y, Yu JK, Ao YF, Zheng ZZ, Gong X, Leung KK. Diagnostic values of 3 methods for evaluating meniscal healing status after meniscal repair: comparison among second-look arthroscopy, clinical assessment, and magnetic resonance imaging. Am J Sports Med. 2011;39:735–742. [DOI] [PubMed] [Google Scholar]
- 33. Morgan CD, Wojtys EM, Casscells CD, Casscells SW. Arthroscopic meniscal repair evaluated by second-look arthroscopy. Am J Sports Med. 1991;19:632–638. [DOI] [PubMed] [Google Scholar]
- 34. Nepple JJ, Dunn WR, Wright RW. Meniscal repair outcomes at greater than five years: a systematic literature review and meta-analysis. J Bone Joint Surg Am. 2012;94:2222–2227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Noyes FR, Barber-Westin SD. Repair of complex and avascular meniscal tears and meniscal transplantation. J Bone Joint Surg Am. 2010;92:1012–1029. [PubMed] [Google Scholar]
- 36. Noyes FR, Heckmann TP, Barber-Westin SD. Meniscus repair and transplantation: a comprehensive update. J Orthop Sports Phys Ther. 2012;42:274–290. [DOI] [PubMed] [Google Scholar]
- 37. Reish MW, Kurzweil PR. FasT-Fix meniscus repair. Tech Knee Surg. 2007;6:161–167. [Google Scholar]
- 38. Rimmer MG, Nawana NS, Keene GC, Pearcy MJ. Failure strengths of different meniscal suturing techniques. Arthroscopy. 1995;11:146–150. [DOI] [PubMed] [Google Scholar]
- 39. Tegner Y, Lysholm J, Lysholm M, Gillquist J. A performance test to monitor rehabilitation and evaluate anterior cruciate ligament injuries. Am J Sports Med. 1986;14:156–159. [DOI] [PubMed] [Google Scholar]
- 40. Tengrootenhuysen M, Meermans G, Pittoors K, Riet RV, Victor J. Long-term outcome after meniscal repair. Knee Surg Sports Traumatol Arthrosc. 2011;19:236–241. [DOI] [PubMed] [Google Scholar]
- 41. Tuckman DV, Bravman JT, Lee SS, Rosen JE, Sherman OH. Outcomes of meniscal repair: minimum of 2-year follow-up. Bull Hosp Jt Dis. 2006;63:100–104. [PubMed] [Google Scholar]
- 42. Von Eisenhart-Rothe R, Bringmann C, Siebert M, et al. Femoro-tibial and menisco-tibial translation patterns in patients with unilateral anterior cruciate ligament deficiency—a potential cause of secondary meniscal tears. J Orthop Res. 2004;22:275–282. [DOI] [PubMed] [Google Scholar]
- 43. Warren RF. Arthroscopic meniscus repair. Arthroscopy. 1985;1:170–172. [DOI] [PubMed] [Google Scholar]
- 44. Wasserstein D, Dwyer T, Gandhi R, Austin PC, Mahomed N, Ogilvie-Harris D. A matched-cohort population study of reoperation after meniscal repair with and without concomitant anterior cruciate ligament reconstruction. Am J Sports Med. 2013;41:349–355. [DOI] [PubMed] [Google Scholar]
- 45. Wolf BR, Rodeo SA. Arthroscopic meniscus repair with suture: inside-out with fibrin clot. Sports Med Arthrosc Rev. 2004;12:15–24. [Google Scholar]