Abstract
Background:
Over the past decade, there has been a resurgence of interest in anterior cruciate ligament (ACL) preservation. Proximal and distal avulsion tears have been treated with arthroscopic primary repair, while augmented repair, remnant tensioning, primary repair with biological scaffold, and remnant preservation have been proposed for different types of midsubstance tears. Currently, the incidence of these different tear types is unknown.
Purpose:
To propose a magnetic resonance imaging (MRI) classification system for different tear types based on clinical relevance and to assess the distribution of these different ACL tear types.
Study Design:
Case series; Level of evidence, 4.
Methods:
A retrospective search in an institutional radiographic database was performed for patients who underwent knee MRI at our institution between June 2014 and June 2016. Patients younger than 18 years and those with reports of chronic tears, partial tears, multiligamentous injuries, were excluded. Tear types were graded as proximal avulsion (distal remnant length >90% of total ligament length, type I), proximal (75%-90%, type II), midsubstance (25%-75%, type III), distal (10%-25%, type IV), and distal avulsion (<10%, type V). An orthopaedic surgeon, a radiologist, and a research fellow graded the tear type on 30 MRIs to determine reliability, and the research fellow graded all MRIs. Inter- and intraobserver reliability were measured using kappa statistics.
Results:
A total of 353 patients (57% male; mean age, 37.1 years; range, 18.1-81.2 years) were included. Interobserver reliability was 0.670 (95% confidence interval, 0.505-0.836), and intraobserver reliability ranged from 0.741 to 0.934. Incidence of type I tears was 16%, type II tears 27%, type III tears 52%, type IV tears 1%, and type V tears 3% (2.5% with bony avulsion). Type I tears were more common in patients older than 35 years compared with those younger than 35 years (23% vs 8%; P < .001).
Conclusion:
This classification system was reliable in assessing tear location in acute ACL injuries. Type I tears were seen in 16%, type II in 27%, and type III in 52% of patients in our cohort. These data suggest that there may be greater potential application for ACL preservation techniques.
Keywords: anterior cruciate ligament, proximal tears, tear types, primary repair, remnant preservation
In the 1970s and 1980s, treatment of anterior cruciate ligament (ACL) injuries consisted of open primary repair, and the short-term outcomes were excellent.8,23 Several authors, however, noted that results deteriorated at longer term follow-up.9,17,30 Sherman et al30 were the first to use multivariate analysis to find an explanation for the deterioration of their results of open primary ACL repair at midterm follow-up. They categorized ACL tears into 4 tear types and found that patients with type I (proximal avulsion) tears were associated with better outcomes when compared with type III or IV (midsubstance) tears. Over the ensuing years, several studies indeed showed excellent results of open primary repair when performed on patients with only proximal (type I) tears.3,12 Despite these findings, open primary repair was abandoned in the 1990s.13,38
More recently, there has been a resurgence of interest in ACL preservation, with its associated advantages of maintaining proprioception, preserving the biology, minimizing surgical morbidity,2,7,24 and allowing for faster recovery,39 as well as experimental findings of restoring native kinematics10 and preventing osteoarthritis.25 Learning from the findings of Sherman et al30 and benefiting from modern advances such as arthroscopy and early range of motion, DiFelice et al7 were the first to report excellent outcomes after arthroscopic primary repair of proximal (type I) ACL tears. More recently, others have confirmed these findings.1,32 Similarly, other surgeons have proposed preservation techniques for different tear types—techniques such as augmented repair, repair with biological scaffold, remnant tensioning, remnant preservation, and distal repair.14,16,19,21,26
With this resurgence of interest in arthroscopic primary repair and other ACL preservation techniques, it is important to know the incidence of the different tear types, but this is currently not known due to ligament debriding in all cases with the current gold standard of ACL reconstruction. Therefore, we aimed to (1) propose a grading system for different tear types based on clinical relevance and feasibility and (2) assess the distribution of different tear types in patients with acute ACL tears. We hypothesized that midsubstance tears are the most common tear type, and that type I tears occur in 10% to 20% of adult patients with acute ACL injuries.
Methods
Patient Selection
After institutional review board approval from our institution, a search was performed in the electronic radiology patient archiving and communication system (PACS) (Sectra Workstation IDS7, version 16.1, Sectra AB) for patients who underwent knee magnetic resonance imaging (MRI) at our institution for ACL injuries between June 3, 2014, and June 2, 2016. The reports by radiologists were screened for the diagnosis of an ACL tear. A total of 710 MRIs with ACL tears were identified. Patients were then excluded if they had partial tears (n = 67); had nonacute tears, defined as >1-month delay between injury and MRI (n = 207); were pediatric patients, defined as younger than 18.0 years (n = 76); or had multiligamentous knee injuries (n = 7). After applying these exclusion criteria, we identified 353 adult patients with an acute isolated complete ACL tear who underwent MRI at our institution.
MRI Measurements
MRI was performed with a 1.5-T or 3.0-T superconducting magnet (GE Medical Systems) using a standardized institutional protocol. ACL tear locations were assessed from 2-dimensional fast-spin echo images acquired along 3 anatomic planes (sagittal, coronal, axial) (repetition time [TR], 4000-6000 ms; echo time [TE], 25-30 ms; echo train length [ETL], 8-16; bandwidth, 32-62.5 kHz over entire frequency range; acquisition matrix, 512 × 256-416; number of excitations [NEX], 1-2; field of view [FOV], 15-16 cm; slice thickness, 3.5 mm with no gap). An additional sagittal inversion recovery sequence was obtained (TR, 5000-8000 ms; TE, 18 ms; ETL, 8-16; inversion time [TI], 150-180 ms; bandwidth, 32-62.5 kHz; acquisition matrix, 256 × 192; NEX, 1-2; FOV, 16-18 cm; slice thickness, 3.5-4.0 cm). Examinations were performed in the supine position with a pillow under the knee supporting it in extension and slight external rotation. The quadriceps was relaxed, and no anesthesia was used in any patient. The extremity was secured in a commercial extremity coil (8-channel knee coil, MedRad) to ensure a consistent extremity position for all patients.
The sagittal, coronal, and axial planes were viewed in order to assess the ACL tear location. The ligament was first viewed on the sagittal plane and was followed from distal to proximal to assess the tear location. The coronal and sagittal planes were then critically reviewed to confirm the tear location. If a spiral tear pattern was noted, the middle of the spiral part was defined as the tear location. If the distal remnant was sagging, indicating that the ligament is wavy because it is not tensioned toward the femur and therefore does not reach the proximal remnant, an assessment was made for the original distal and proximal remnant lengths, and thus the original tear location (some sagging of the ligament is seen in Figure 8). If needed, a digital ruler was used to assess the exact tear location.
Figure 8.
This case is an example of a tear around the proximal–mid third junction, which had a decreased interobserver reliability. After measuring the length of both remnants, this tear was graded as a type III tear. Some slight “sagging” of the ligament can be seen at the distal insertion, which creates a small gap between the proximal and distal remnant.
Classification System
All tears were classified as one of following: type I tear (proximal avulsion tear, located at >90% of distal-proximal length) (Figure 1), type II tear (proximal tear, located at 75%-90% of distal-proximal length) (Figure 2), type III tear (midsubstance tear, located at 25%-75% of distal-proximal length) (Figure 3), type IV tear (distal tear, located at 10%-25% of distal-proximal length) (Figure 4), or type V tear (distal avulsion tear, located at <10% of distal-proximal length). Type I and type V tears were further classified as soft tissue avulsion tears (Figure 5) or bony avulsion tears (Figure 6). If it was seen that the anteromedial and posterolateral bundles were torn at different levels, the tear locations of both separate bundles were noted. This classification was partially based on the tear locations as classified by Sherman et al,30 and partially on a recently published ACL preservation treatment algorithm36,37 in which type I tears were treated with arthroscopic primary repair,1,7 type II tears with augmented repair,16,21,36 type III and type IV tears with ACL reconstruction with remnant tensioning and preservation, respectively,14,16 and type V tears with primary repair or a variety of fixation options for soft tissue avulsion or bony avulsion types, respectively.19,31
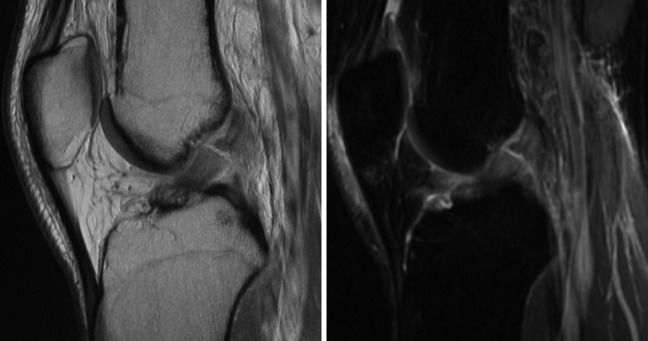
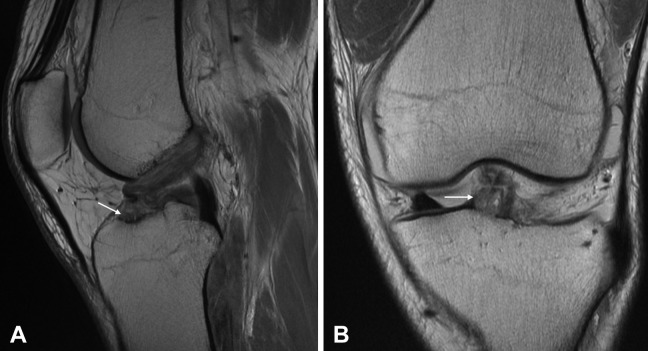
Figure 1.
A type I tear (arrow) is shown on the (A) sagittal T1-weighted view and (B) axial T1-weighted view. It can be noted that the ligament is avulsed with only a few fibers remaining on the femoral wall (asterisk).
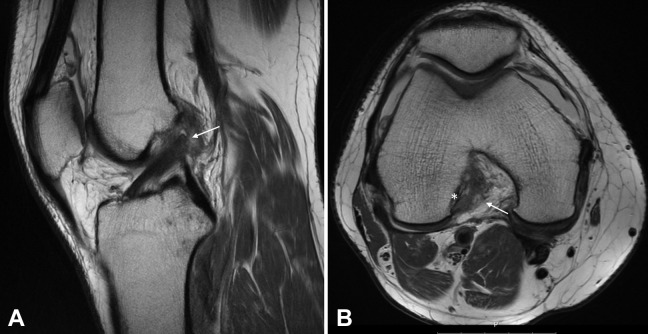
Figure 2.
A type II tear (arrow) is shown on the (A) sagittal T1-weighted view and (B) axial T1-weighted view.
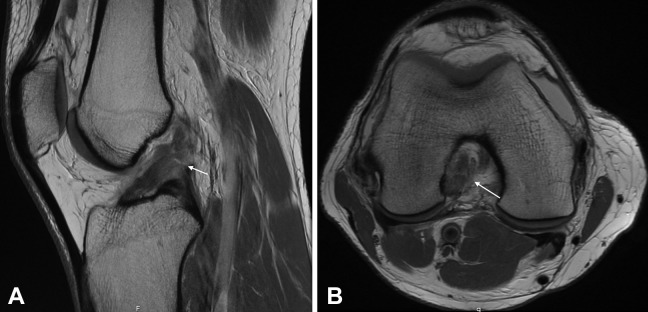
Figure 3.
(A) A type III tear (arrow) is shown on the sagittal T1-weighted view and (B) another more complex type III tear (arrow) is shown on the sagittal T1-weighted view.
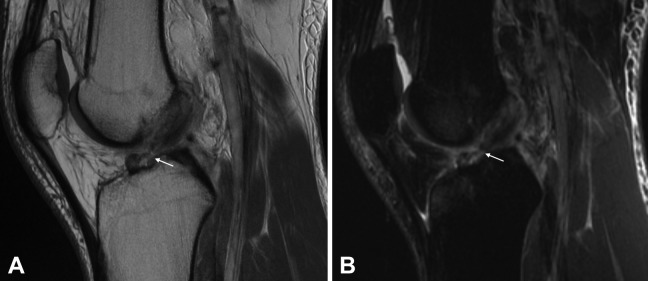
Figure 4.
A type IV tear (arrow) is shown on the (A) sagittal T1-weighted view and (B) sagittal T2-weighted view.
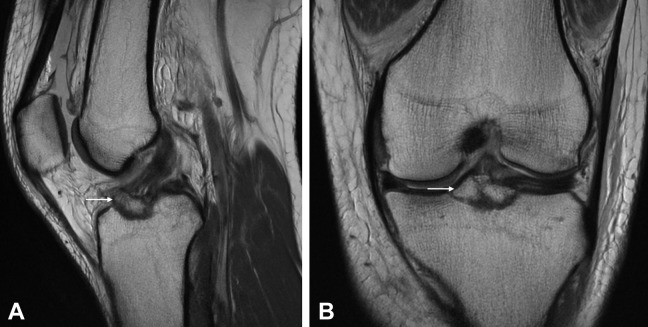
Figure 5.
A type V soft tissue avulsion tear (arrow) is seen on the (A) sagittal T1-weighted view and (B) coronal T1-weighted view.
Figure 6.
A type V bony avulsion (arrow) is seen on the (A) sagittal T1-weighted view and (B) coronal T1-weighted view.
Measurement Protocol
First, 30 patients were randomly selected for the assessment of inter- and intraobserver reliability of this classification method. An orthopaedic surgeon experienced in ligament preservation (G.S.D.), a musculoskeletal radiologist with >15 years of experience (D.N.M), and a research fellow (J.P.L.) graded the tear location in these 30 patients. The orthopaedic surgeon and research fellow had been using the tear type classification for 6 months prior to the start of this study, while the radiologist had not worked with this specific classification prior to this study. Three weeks after initial assessment, the 3 observers repeated the measurements to assess the intraobserver reliability. Finally, the research fellow graded all 353 patients to assess the incidence of the tear types.
Data Collection
Additional collected data from the MRI intake information included patient sex, side of injury, injury mechanism, and date of birth, date of injury, and date of MRI in order to calculate age and delay from injury to MRI. Subgroups were <35 and >35 years of age (mean age was 37 years), male and female patients, and all injury mechanism groups with >30 patients.
Statistical Analysis
Statistical analysis was performed using SPSS version 21.0 (IBM Corp). Interobserver reliability of the 3 observers was calculated using the Fleiss kappa, and intraobserver reliability was calculated using the Cohen kappa. Kappa was reported with 95% confidence intervals (CIs). Interpretation of kappa values was based on guidelines outlined by Landis and Koch,18 representing poor (<0.00), slight (0.00-0.20), fair (0.21-0.40), moderate (0.41-0.60), substantial (0.61-0.80), or almost perfect (0.81-1.00) agreement. Incidence of the different tear types was displayed in percentages for the total group and the different subgroups. Chi-square tests were used to compare the incidence of tear types in the different subgroups. A P value <.05 was considered statistically significant.
Results
Study Cohort
In the study cohort of 353 patients, the mean (±SD) was 37.1 ± 12.9 years (range, 18.1-81.2 years), 57% were male, and 51% had an ACL tear in their right knee. The mean time from injury to MRI was 8 ± 7 days (range, 0-31 days). Most common injury mechanisms were skiing (39%), soccer 13%), and basketball (11%) in this cohort.
Inter- and Intraobserver Reliability
Interobserver reliability for the classification system between the 3 observers was substantial, with a kappa value of 0.670 (95% CI, 0.505-0.836). Intraobserver reliability for the orthopaedic surgeon was 0.934 (95% CI, 0.807-1.000), for the radiologist 0.741 (95% CI, 0.463-1.000), and for the research fellow 0.875 (95% CI, 0.710-1.000).
Incidence of Different Tear Types
Type I tears were seen in 16% of patients, type II tears in 27%, type III tears in 52%, type IV tears in 1%, and type V tears in 3% of patients (Table 1). In 1% of the tears, the tear locations of both bundles differed. All type I tears in this cohort were soft tissue avulsion tears. Type V tears were more commonly bony avulsion (2.5%) than soft tissue avulsion tears (0.6%).
TABLE 1.
Incidence of Tear Type Based on Magnetic Resonance Imaging
| Tear Type | Location,a % | Incidence, % |
|---|---|---|
| Type I | >90 | 16 |
| Type II | 75-90 | 27 |
| Type III | 25-75 | 52 |
| Type IV | 10-25 | 1 |
| Type V | <10 | 3 |
| Bundles differedb | — | 1 |
| Total | — | 100 |
aTear location indicates the length of distal remnant as percentage of ligament length.
bIn these tear types, the anteromedial and posterolateral bundle were torn at different locations.
Subgroup Analyses
In patients older than 35 years, type I tears were significantly more frequently seen when compared with younger patients (23% vs 8%, P < .001). Type III tears (60% vs 45%, P = .006) and type V tears (6% vs 1%, P = .007) were more frequently seen in younger patients. Incidence of tear type by age group is shown in Figure 7.
Figure 7.
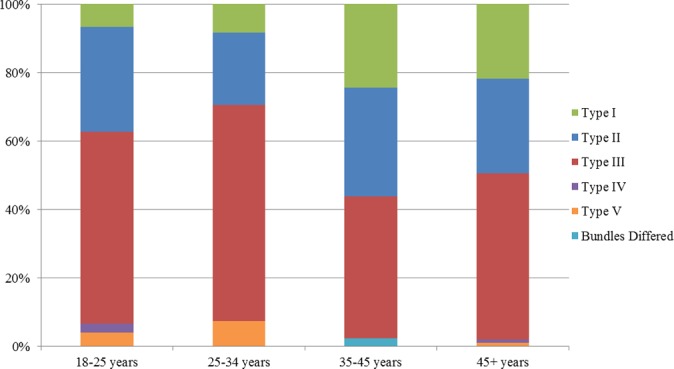
The incidence of the different tear types according to the different age groups. Type I tears were more commonly seen in patients older than 35 years when compared with patients younger than 35 years (P < .001), while type III and type V tears were more commonly seen in patients younger than 35 years (P = .006 and .007, respectively).
With regard to patient sex, a trend toward a higher incidence of type I tears was noted in females (19%) when compared with males (13%, P = .115). No differences between males and females regarding the other tear types were seen.
Skiing, basketball, and soccer were injury mechanisms with >30 patients involved, and these were further analyzed. Although a trend of higher incidence of type I tears was noted with skiing (17%) and soccer (18%) injuries when compared with basketball injuries (12%), no significant differences between the groups were noted for any tear types (Table 2).
TABLE 2.
Incidence of Tear Type Based on Magnetic Resonance Imaging and Stratified by Injury Mechanisma
| Tear Type | Location,b % | Skiing (n = 139), % | Soccer (n = 44), % | Basketball (n = 43), % |
|---|---|---|---|---|
| Type I | >90 | 17 | 18 | 12 |
| Type II | 75-90 | 27 | 23 | 30 |
| Type III | 25-75 | 50 | 59 | 56 |
| Type IV | 10-25 | 1 | 0 | 0% |
| Type V | <10 | 4 | 0 | 2 |
| Bundles differedc | — | 1 | 0 | 0 |
| Total | — | 100 | 100 | 100 |
aNo significant differences were noted between each of the groups (P > .05).
bTear location indicates the length of distal remnant as percentage of ligament length.
cIn these tear types, the anteromedial and posterolateral bundle were torn at different locations.
Discussion
In this study, we proposed a tear type classification using MRI, and we assessed the incidence of the different tear types in adult patients using this classification. Substantial interobserver and substantial to nearly perfect intraobserver reliability was found with this measurement method. It was noted that 16% of tears were type I tears and that these were more commonly seen in patients older than 35 years. Type II tears occurred in 27%, whereas type III tears were most commonly seen (52%). Type IV (1%) and type V tears (3%) were not frequently seen in this cohort. This study is the first to assess ACL tear type incidence using MRI, and these findings may help the orthopaedic surgeon in making a preoperative assessment of which ACL preservation technique might be possible.
In this study, we have validated a classification system with 5 tear locations, which was based on both feasibility (of measurement) and clinical relevance. In the initial tear type classification of Sherman et al,30 4 different tear types were described for the upper (proximal) half of the ligament. This would result in 7 tear types if these types were mirrored to the lower (distal) half of the ligament (tears at the 50% location result in only 1 type when mirrored). Although this classification is very specific, the multiple options lead to disagreement between the observers in our previous experience, while there is no additive value for clinical practice; there are no different ACL preservation treatments between proximal–mid third junction tears, middle third tears, and mid-distal junction tears.36,37 Therefore, the Sherman classification was modified, and these 3 tear types were considered midsubstance tears. This improved the clinical application of the classification system, while increasing agreement between observers. Another frequently used method to describe the tear location is to describe the location as the proximal, middle, or distal third. This classification is not specific enough however, as there is no differentiation between type I and type II tears. Furthermore, many tears occur around the junction of the proximal and middle third (22% in the study of Sherman et al30), which can lead to disagreement between observers, as these tears need to be categorized as either one or the other.
With this in mind, we decided to use the classification system as was earlier proposed: There is no confusion about tears at the junction of the proximal and middle third (these are considered midsubstance tears), and the tear types can be correlated with ACL preservation techniques.36,37 Although the intraobserver reliability was good in this study (substantial to almost perfect), the interobserver reliability was substantial. Disagreement between observers mainly occurred with the type II–type III tears (Figure 8).
Difficulty was seen with the assessment of the original tear location when the ligament was sagging or when the tear had a spiral pattern. This can explain the substantial interobserver reliability. Ultimately, arthroscopy is needed to assess the possibility of using ACL preservation techniques with these tear types, as tissue quality is a critical determinant.
The main findings of this study were that 43% of the ACL tears were located in the proximal quarter, of which 16% were type I tears and 27% were type II tears, whereas the majority (52%) of the tears were located in the midsubstance of the ligament. Since the current gold standard of reconstruction resects the entirety of the torn ligament, there really has been little interest in this topic, and we could identify no studies reporting the incidence of different tear types using MRI. Therefore, we feel it is of additional value to compare our findings with studies in the historical literature that assessed the tear location intraoperatively. Sherman et al30 in their study noted that 13 out of 50 patients (26%) had type I tears, 15 out of 50 (30%) had type II tears, while 22 out of 50 (44%) had type III or IV tears. The incidence of type I and type II tears was slightly higher when compared to this current study, which might be explained by a combination of factors, such as the small number of patients in their cohort (N = 50), the treatment bias in their study (they assessed the tear location only in operated patients), or the regional selection bias in our study. The incidence of type III and IV tears in the study by Sherman et al30 (44%) was quite similar to the incidence of midsubstance tears (type III) tears in this study (52%).
Other historical studies have reported the incidence of tear locations in the proximal, middle, and distal thirds during surgery. Grontvedt et al13 performed a randomized clinical trial between 1986 and 1988 in which patients were treated with primary repair or augmented repair; they reported that in the total study, 104 out of 147 patients (71%) had proximal third tears. This is significantly higher than the findings in our study (incidence of type I and II tears: 43%). This may, however, be explained by the fact that many patients have a tear at the junction of the proximal third and middle third (22% according to the study of Sherman et al30). These patients may have been classified as having a proximal third tear in their study, whereas they are considered middle-third tears in our study. Several other historical clinical studies, similar to our study, reported that most tears were midsubstance tears.5,20,23,29,34
Our study results showed that the incidence of type I tears was significantly higher in patients older than 35 years, while there was a trend of more type I tears in females. We can only speculate on the reasons for these findings. A possible explanation is that the tear location depends on the severity of the injury. It is possible that with low-energy injuries the ligament tends to avulse off the wall, while with high-impact injuries, the ligament is more commonly disrupted in the midsubstance. Another possible explanation may be that the mechanism of injury is associated with different tear types; for example, a hyperextension injury could theoretically be more commonly associated with proximal tears than valgus mechanisms. In our study, no correlation between tear location and sport played during injury was found. However, the exact injury mechanism (eg, valgus, hypertension, etc) was not retrieved. Although many studies have found correlations between valgus or internal rotation movement and ACL tears and have speculated on correlations between injury mechanism and ACL injuries,15,28,33 no other studies in the literature could be identified that suggested a correlation between injury mechanism and different tear types. Future biomechanical or retrospective studies could shed more light on the correlation of injury mechanism and tear type.
Several limitations exist in this study. First of all, the location of ACL tears was assessed on MRI, and these results cannot be extrapolated as the percentage of patients that are eligible for primary repair or other preservation techniques. Tissue quality is an important factor for preservation techniques, and this was not assessed in this study. Furthermore, the correlation between tear type on MRI and arthroscopy is not known, and further studies are therefore needed to assess this. Despite this limitation, outcomes in this study are valuable and may help the orthopaedic surgeon in making a preoperative assessment of whether a patient might be eligible for primary repair or other preservation techniques. Second, it is currently unknown if patients with different tear types have a different sense of instability, and thus perhaps a different length of time from injury to MRI. It is possible that patients with proximal tears have a delayed presentation, since the remnant can reattach to the femoral notch or posterior cruciate ligament with these tear types, providing some form of stability.4,11,35,40 This can lead to less urgency to seek medical care, which contains a potential selection bias. It was only possible to include acute tears because that remnant tissue may retract or reabsorb in the nonacute setting and is therefore less visible on MRI.22,27 We believe that only assessing acute tears is appropriate, however, especially since preservation techniques are generally performed in the acute setting.1,6 Finally, another selection bias cannot be excluded in this study. A relatively high number of patients had skiing injuries, which could have influenced the distribution of tear types. Studies in other geographic regions, with a different mix of sporting activities, are necessary to confirm our tear type distribution.
Conclusion
In this study, a tear type classification was proposed for acute complete ACL injuries using MRI. It was noted that 43% of the tears were in the proximal quarter, of which 16% were type I tears and 27% were type II tears, while type III tears were most common in our cohort (52%). Type I tears were more commonly seen in older patients, while type III and V tears were more frequently seen in those younger than 35 years. Future studies are necessary to correlate these MRI findings to arthroscopic findings to identify the percentage of patients who are eligible for ACL preservation surgery and primary ACL repair surgery.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: G.S.D. is a paid consultant for and receives research funding from Arthrex.
Ethical approval for this study was obtained from the Hospital for Special Surgery (IRB #16009).
References
- 1. Achtnich A, Herbst E, Forkel P, et al. Acute proximal anterior cruciate ligament tears: outcomes after arthroscopic suture anchor repair versus anatomic single-bundle reconstruction. Arthroscopy. 2016;32:2562–2569. [DOI] [PubMed] [Google Scholar]
- 2. Adachi N, Ochi M, Uchio Y, Iwasa J, Ryoke K, Kuriwaka M. Mechanoreceptors in the anterior cruciate ligament contribute to the joint position sense. Acta Orthop Scand. 2002;73:330–334. [DOI] [PubMed] [Google Scholar]
- 3. Bram J, Plaschy S, Lutolf M, Leutenegger A. The primary cruciate ligament suture—is the method outdated? Results in follow-up of 58 patients [in German]. Z Unfallchir Versicherungsmed. 1994;87:91–109. [PubMed] [Google Scholar]
- 4. Crain EH, Fithian DC, Paxton EW, Luetzow WF. Variation in anterior cruciate ligament scar pattern: does the scar pattern affect anterior laxity in anterior cruciate ligament-deficient knees? Arthroscopy. 2005;21:19–24. [DOI] [PubMed] [Google Scholar]
- 5. Cross MJ, Wootton JR, Bokor DJ, Sorrenti SJ. Acute repair of injury to the anterior cruciate ligament. A long-term followup. Am J Sports Med. 1993;21:128–131. [DOI] [PubMed] [Google Scholar]
- 6. DiFelice GS, van der List JP. Arthroscopic primary repair of proximal anterior cruciate ligament tears. Arthrosc Tech. 2016;5:e1057–e1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. DiFelice GS, Villegas C, Taylor SA. Anterior cruciate ligament preservation: early results of a novel arthroscopic technique for suture anchor primary anterior cruciate ligament repair. Arthroscopy. 2015;31:2162–2171. [DOI] [PubMed] [Google Scholar]
- 8. Feagin JA, Abbott HG, Rokous JR. The isolated tear of the anterior cruciate ligament. J Bone Joint Surg Am. 1972;54:1340–1341. [Google Scholar]
- 9. Feagin JA, Jr, Curl WW. Isolated tear of the anterior cruciate ligament: 5-year follow-up study. Am J Sports Med. 1976;4:95–100. [DOI] [PubMed] [Google Scholar]
- 10. Fleming BC, Carey JL, Spindler KP, Murray MM. Can suture repair of ACL transection restore normal anteroposterior laxity of the knee? An ex vivo study. J Orthop Res. 2008;26:1500–1505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fowler PJ, Regan WD. The patient with symptomatic chronic anterior cruciate ligament insufficiency. Results of minimal arthroscopic surgery and rehabilitation. Am J Sports Med. 1987;15:321–325. [DOI] [PubMed] [Google Scholar]
- 12. Genelin F, Trost A, Primavesi C, Knoll P. Late results following proximal reinsertion of isolated ruptured ACL ligaments. Knee Surg Sports Traumatol Arthrosc. 1993;1:17–19. [DOI] [PubMed] [Google Scholar]
- 13. Grontvedt T, Engebretsen L, Benum P, Fasting O, Molster A, Strand T. A prospective, randomized study of three operations for acute rupture of the anterior cruciate ligament. Five-year follow-up of one hundred and thirty-one patients. J Bone Joint Surg Am. 1996;78:159–168. [DOI] [PubMed] [Google Scholar]
- 14. Hong L, Li X, Zhang H, et al. Anterior cruciate ligament reconstruction with remnant preservation: a prospective, randomized controlled study. Am J Sports Med. 2012;40:2747–2755. [DOI] [PubMed] [Google Scholar]
- 15. Johnson SC. Anterior cruciate ligament injury in elite Alpine competitors. Med Sci Sports Exerc. 1995;27:323–327. [PubMed] [Google Scholar]
- 16. Jung YB, Jung HJ, Siti HT, et al. Comparison of anterior cruciate ligament reconstruction with preservation only versus remnant tensioning technique. Arthroscopy. 2011;27:1252–1258. [DOI] [PubMed] [Google Scholar]
- 17. Kaplan N, Wickiewicz TL, Warren RF. Primary surgical treatment of anterior cruciate ligament ruptures. A long-term follow-up study. Am J Sports Med. 1990;18:354–358. [DOI] [PubMed] [Google Scholar]
- 18. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- 19. Leeberg V, Lekdorf J, Wong C, Sonne-Holm S. Tibial eminentia avulsion fracture in children—a systematic review of the current literature. Dan Med J. 2014;61:A4792. [PubMed] [Google Scholar]
- 20. Liljedahl SO, Lindvall N, Wetterfors J. Early diagnosis and treatment of acute ruptures of the anterior cruciate ligament; a clinical and arthrographic study of forty-eight cases. J Bone Joint Surg Am. 1965;47:1503–1513. [PubMed] [Google Scholar]
- 21. Mackay GM, Blyth MJ, Anthony I, Hopper GP, Ribbans WJ. A review of ligament augmentation with the InternalBrace: the surgical principle is described for the lateral ankle ligament and ACL repair in particular, and a comprehensive review of other surgical applications and techniques is presented. Surg Technol Int. 2015;26:239–255. [PubMed] [Google Scholar]
- 22. Magarian EM, Fleming BC, Harrison SL, Mastrangelo AN, Badger GJ, Murray MM. Delay of 2 or 6 weeks adversely affects the functional outcome of augmented primary repair of the porcine anterior cruciate ligament. Am J Sports Med. 2010;38:2528–2534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Marshall JL, Warren RF, Wickiewicz TL. Primary surgical treatment of anterior cruciate ligament lesions. Am J Sports Med. 1982;10:103–107. [DOI] [PubMed] [Google Scholar]
- 24. Murray MM. Current status and potential of primary ACL repair. Clin Sports Med. 2009;28:51–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Murray MM, Fleming BC. Use of a bioactive scaffold to stimulate anterior cruciate ligament healing also minimizes posttraumatic osteoarthritis after surgery. Am J Sports Med. 2013;41:1762–1770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Murray MM, Flutie BM, Kalish LA, et al. The bridge-enhanced anterior cruciate ligament repair (BEAR) procedure: an early feasibility cohort study. Orthop J Sports Med. 2016;4:2325967116672176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. O’Donoghue DH, Rockwood CA, Jr, Frank GR, Jack SC, Kenyon R. Repair of the anterior cruciate ligament in dogs. J Bone Joint Surg Am. 1966;48:503–519. [PubMed] [Google Scholar]
- 28. Pappas E, Zampeli F, Xergia SA, Georgoulis AD. Lessons learned from the last 20 years of ACL-related in vivo-biomechanics research of the knee joint. Knee Surg Sports Traumatol Arthrosc. 2013;21:755–766. [DOI] [PubMed] [Google Scholar]
- 29. Sgaglione NA, Warren RF, Wickiewicz TL, Gold DA, Panariello RA. Primary repair with semitendinosus tendon augmentation of acute anterior cruciate ligament injuries. Am J Sports Med. 1990;18:64–73. [DOI] [PubMed] [Google Scholar]
- 30. Sherman MF, Lieber L, Bonamo JR, Podesta L, Reiter I. The long-term followup of primary anterior cruciate ligament repair. Defining a rationale for augmentation. Am J Sports Med. 1991;19:243–255. [DOI] [PubMed] [Google Scholar]
- 31. Sheth MR, Tapasvi SR, Patil SS. Primary repair of tibial-sided avulsion of the anterior cruciate ligament. Arthrosc Tech. 2016;5:E901–E906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Smith JO, Yasen SK, Palmer HC, Lord BR, Britton EM, Wilson AJ. Paediatric ACL repair reinforced with temporary internal bracing. Knee Surg Sports Traumatol Arthrosc. 2016;24:1845–1851. [DOI] [PubMed] [Google Scholar]
- 33. Speer KP, Warren RF, Wickiewicz TL, Horowitz L, Henderson L. Observations on the injury mechanism of anterior cruciate ligament tears in skiers. Am J Sports Med. 1995;23:77–81. [DOI] [PubMed] [Google Scholar]
- 34. Straub T, Hunter RE. Acute anterior cruciate ligament repair. Clin Orthop Relat Res. 1988;227:238–250. [PubMed] [Google Scholar]
- 35. Vahey TN, Broome DR, Kayes KJ, Shelbourne KD. Acute and chronic tears of the anterior cruciate ligament: differential features at MR imaging. Radiology. 1991;181:251–253. [DOI] [PubMed] [Google Scholar]
- 36. van der List JP, DiFelice GS. Preservation of the anterior cruciate ligament: a treatment algorithm based on tear location and tissue quality. Am J Orthop (Belle Mead NJ). 2016;45:e393–e405. [PubMed] [Google Scholar]
- 37. van der List JP, DiFelice GS. Preservation of the anterior cruciate ligament: surgical techniques. Am J Orthop (Belle Mead NJ). 2016;45:E406–E414. [PubMed] [Google Scholar]
- 38. van der List JP, DiFelice GS. Primary repair of the anterior cruciate ligament: a paradigm shift [published online October 6, 2016]. Surgeon. doi:10.1016/j.surge.2016.09.006. [DOI] [PubMed] [Google Scholar]
- 39. van der List JP, DiFelice GS. Range of motion and complications following primary repair versus reconstruction of the anterior cruciate ligament [published online May 24, 2017]. Knee. doi:10.1016/j.knee.2017.04.007. [DOI] [PubMed] [Google Scholar]
- 40. van der List JP, DiFelice GS. Successful arthroscopic primary repair of a chronic anterior cruciate ligament tear 11 years following injury. HSS J. 2017;13:90–95. [DOI] [PMC free article] [PubMed] [Google Scholar]