Abstract
Background: Although fingertip injuries are common, there is limited literature on the epidemiology and hospital charges for fingertip injuries in children. This descriptive study reports the clinical features of and hospital charges for fingertip injuries in a large pediatric population treated at a tertiary medical center. Methods: Our hospital database was queried using International Classification of Diseases, Revision 9 (ICD-9) codes, and medical records were reviewed. Frequency statistics were generated for 1807 patients with fingertip injuries who presented to the emergency department (ED) at Boston Children’s Hospital (BCH) between 2005 and 2011. Billing records were analyzed for financial data. Results: A total of 1807 patients were identified for this study; 59% were male, and the mean age at time of injury was 8 years. Most commonly, injuries occurred when a finger was crushed (n = 831, 46%) in a door or window. Average length of stay in the ED was 3 hours 45 minutes, 25% of cases needed surgery, and, on average, patients had more than 1 follow-up appointment. About one-third of patients were referred from outside institutions. The average ED charge for fingertip injuries was $1195 in 2014, which would amount to about $320 430 each year (in 2014 dollars) for fingertip injuries presenting to BCH. Conclusion: Fingertip injuries in children are common and result in significant burden, yet are mostly preventable. Most injuries occur at home in a door or window. Although these patients generally heal well, fingertip injuries pose a health, time, and financial burden. Increased awareness and education may help to avoid these injuries.
Keywords: fingertip injuries, hand injuries, pediatric fingertip injuries, pediatric hand surgery, charges for fingertip injuries
Background
Fingertip injuries are among the most common pediatric hand problems treated in emergency departments (EDs) annually.14 While large-scale epidemiological studies are lacking, the few studies that have been conducted show that most fingertip injuries occur at home, or near home, including in the backyard.1,2,5,8,9,14,17 Most children who present with fingertip trauma have experienced a crush injury,10,11 usually from the hinge side of a door,1,2,7,12,14 and often in the living room.8 The fingertip is most often affected because it is the most distal part of the hand.10 After the home, most fingertip injuries happen at school.2,5,9
Fingertip injuries are serious and stressful for families, and may require surgery. Possible short-term complications from fingertip injuries include infection (soft tissue loss), fracture nonunion, and amputation.2,5,9,14 Long-term complications include fingertip deformity, nail dystrophy, and pain.
There is limited evidence-based literature to inform how to prevent these injuries;16 this descriptive study was conducted to learn more about the epidemiology of a large pediatric fingertip injury population in order to meet that need.
Materials and Methods
Following approval from the Institutional Review Board at Boston Children’s Hospital (BCH), patients’ medical records were queried and retrospectively reviewed. The following International Classification of Diseases, Revision 9 (ICD-9) codes were used to identify potential subjects: 816, 816.02, 816.10, 816.12, 883, 883.1, 886, and 886.1. The fingertip was defined as the tissue distal to the midpoint of the distal phalanx. Patients were included if they presented to the BCH ED between 2005 and 2011, and were diagnosed and treated for a fracture of the distal phalanx tip, open finger wounds, or complete or partial distal digit amputation. Data of interest included type and mechanism of injury, injured finger, time spent in the ED, and treatment. Frequency statistics were generated using Microsoft Excel 2010. Hospital billing records were queried to retrieve financial data (charges submitted by the hospital only) associated with these injuries.
Results
Demographics
A total of 1807 patients presenting with fingertip injuries were identified for this study. The mean age at the time of injury was 8 years (SD = 6 years, range = 0-18 years), and 59% of patients were male. Injuries were most common in the middle finger (Figure 1), and more patients presented with an injury to their right hand (n = 939, 52%) than to their left hand (n = 847, 47%). Only 6 patients presented with injuries to both hands, and there were missing data for the affected hand for 15 patients.
Figure 1.
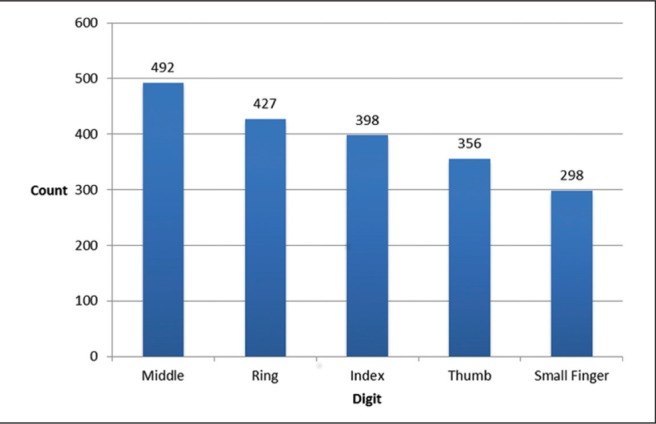
Injury frequency by digit.
Note. Some patients had more than 1 digit affected.
Mechanism of Injury
Patients reported how they were injured, and these causes were classified as a crush, laceration, sports injury, mechanical device, fall, or other (ie, bite, strangulation, burn, fight) (Figure 2). The most common mechanism (n = 831, 46%) was a crush injury, usually in a door or window (data missing for 3 patients). These injuries most often resulted in fractures (n = 615, 43%), but also included nail bed injuries (n = 485, 34%) and amputations (n = 334, 23%) (Figure 3). When stratified by age group, preschool children (ages 0 to 6) were most commonly injured by a crush (n = 551, 61%) or laceration (n = 218, 24%), while school-age children (ages 7 to 12) had higher frequencies of sports injuries (n = 70, 15%) after crush (n = 190, 42%) and laceration (n = 129, 28%) injuries. Adolescents (ages 13 to 18 in our study) had lower frequencies of crush injuries (n = 90, 20%) and were more frequently injured by lacerations (n = 151, 34%), sports (n = 119, 27%), and finally machines (n = 32, 7%) (Figure 4).
Figure 2.
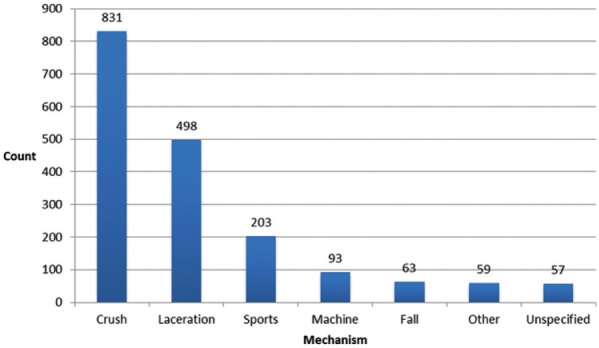
Mechanism of injury (n = 1804).
Note. “Other” includes injuries from a bite, burn, strangulation, or fight.
Figure 3.
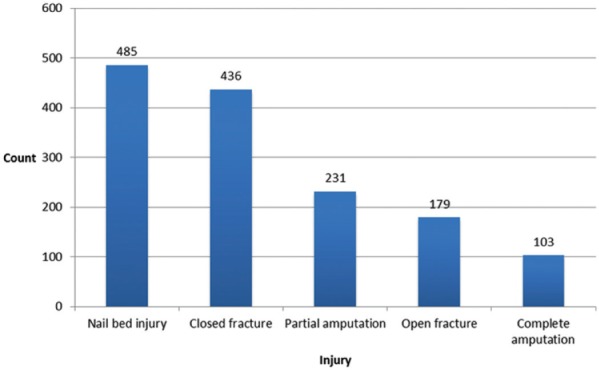
Injury type (n = 1434).
Figure 4.
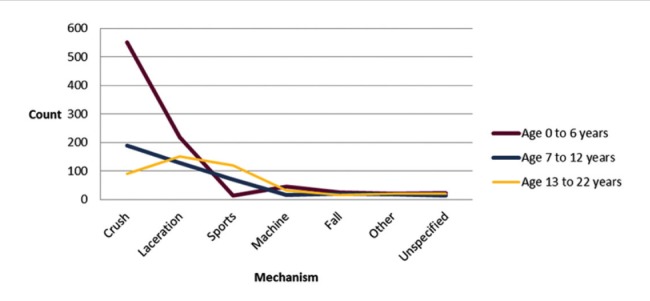
Mechanism of injury, stratified by age group (n = 1804).
Note. “Other” includes injuries caused by a burn, bite, strangulation, or fight. “Unspecified” indicates that it is not clear in the medical record.
Treatment
Roughly one-third of patients (n = 535, 31%) in this study were referred from an outside institution (data missing for 68 patients). At BCH, over half of the patients (n = 1007 patients, 56%) were evaluated and treated by the ED staff without a formal hand surgery consultation (data missing for 2 patients). On average, patients required more than 1 follow-up appointment, and the average length of stay in the ED was 3 hours 45 minutes (data available for 999 patients).
Twenty-five percent (n = 458) of all patients required surgical intervention. Ten percent (n = 190) underwent immediate surgery, which was defined as within 24 hours of presenting to our institution; the remaining 15% (n = 268) had delayed surgery. Thirty-three percent (n = 62) of immediate surgeries were for patients who presented with an amputation; 44% (n = 27) of those cases were complete amputations.
Patients who were referred from an outside institution were 2.31 times as likely to need surgery as those who first presented to our institution (95% confidence interval [CI]: 1.98-2.69). Forty-three percent (n = 232) of patients who were referred from an outside institution required surgery (17% had surgery within 24 hours), while only 19% (n = 226) of patients who first presented to our institution required surgery (8% had surgery within 24 hours) (Figures 5a & 5b).
Figure 5.
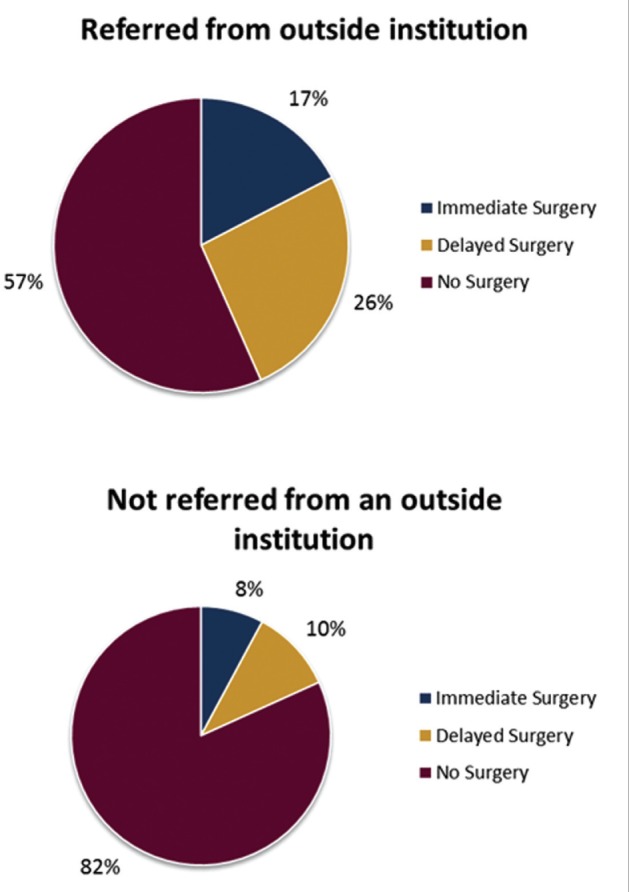
Surgical intervention for patients (n = 1739), stratified by whether they were referred from an outside institution (n = 535) or not (n = 1204).
Note. Immediate surgery is defined as surgery performed within 24 hours of presenting to the ED; delayed surgery is after 24 hours.
Charges
Fingertip injury cases that presented to the ED resulted in averages charges of $1195 per patient during the 2014 calendar year (Figure 6). This includes patients who were diagnosed with an amputation, complicated (ICD-9 code 886.1); open fracture, unspecified (816.10); open fracture, distal (816.12); open wound, complicated (883.1); or closed fracture, distal (816.02). The highest average charge ($2045) was for patients who had a complicated amputation (886.1), while the lowest average charge ($852) was for patients who had a closed fracture of the distal phalanx (816.02).
Figure 6.
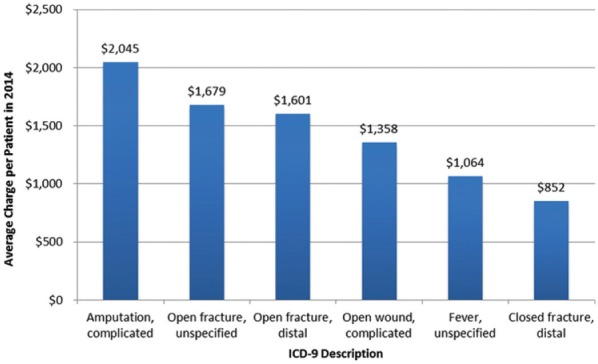
Average charge by ICD-9 code in calendar year 2014.
Note. ICD-9 = International Classification of Diseases, Revision 9.
Discussion
Although fingertip injuries are common in children, there are only a few large series that have examined the demographics, treatment, and charges associated with this problem. To the best of our knowledge, this retrospective study of 1807 fingertip injury patients is one of the largest to date.
Demographics
More injuries (50%) occurred in the preschool age group (0-6 years) than in the older age groups (25% in ages 7 to 12 years, and 25% in ages 13 to 18 years), and this is consistent with what another retrospective study has found.1 Younger children are curious and more apt to explore their environment using their hands without realizing the dangers involved. Our findings also support the outcomes of several other studies where the average pediatric fingertip injury patient is 5 years of age2,5,8,9,12; our study had a higher average, 8 years, possibly because of our larger sample size. Fingertip injuries occur relatively equally among males and females, although our results support previous studies that show these injuries to be more prevalent among males.1,2,5,9
Like numerous other studies,2,5,8,9,12 we found that more fingertip injuries occurred in the right hand (n = 939, 52%), than the left hand (n = 847, 47%). Our findings support the results of other studies that show the middle finger to be the most commonly injured digit.2,5,8
Mechanism of Injury
Most commonly, these injuries were caused when the child caught his or her finger in a door or window. This finding supports multiple studies that describe the most common mechanism of injury to be crushing, usually by a door.2,9 In addition, our findings showed that most crush injuries (66%) occurred in preschool children and that preschool children were more prone to crush injuries; existing smaller studies also noticed this trend.1,17 Specifically, the hinge side of the door is particularly dangerous and was identified as the cause of 57% of injuries in a study by Claudet et al, and 49% of injuries in a study by Doraiswamy.4,8 Because these injuries are mostly preventable, knowing the age group and mechanism to target allows for the creation of more focused prevention strategies (see section on Prevention).
We found that sports injuries were most common among the 13- to 18-year-old age group. Vadivelu et al also found that older children were more prone to sports injuries.17 Fetter-Zarzeka et al described finding the following less common causes: blades and cans (23.5% of injuries), blunt trauma (5%), and sports (4%).9 Less common causes that were found in our study include bites (2%), physical fighting (1.1%), strangulation (0.2%), and burns (0.1%) (Figure 4).
One opportunity for further study is the risk factors associated with these injuries, including the presence of preventive measures (inside and outside the home), the role of other family members in the injury, and special circumstances. Claudet et al found that, within their study population, 94% of patient families did not have any specific preventive measures in place in their home.5 They observed that 75% of patients had an adult present during the accident, and in 25% of the cases, the adult caused the accident;5 Benson et al also found that, in the context of stationary exercise bicycles, adult supervision was not predictive of preventing hand injury.3 Claudet et al reported that, in 44% of cases, another child caused the injury, and more than half (58%) of fingertip injuries happened to a child who had at least 3 siblings, suggesting that children from large families may have a higher risk of experiencing a fingertip injury.5 Last, fingertip injuries have been found to be more likely to occur during the holidays or while on vacation.1
Treatment
Pediatric fingertip injuries are commonly treated in the ED, where they are often treated conservatively.12 Some studies show concern that these injuries are often underestimated2 or undertreated11 by ED physicians. If fingertip injuries are not treated adequately, the patient can experience long-term tenderness, pain, stiffness, sensory problems, deformity in the nail, soft tissue irregularities, and decreased grip strength.6 It has been well documented that optimal outcomes depend on high-quality care from ED physicians who are well trained in diagnosing and managing fingertip injuries,4,14,15,18 and who are prepared to refer complicated cases to a pediatric hand surgeon.6,14
Outcomes depend in part on quality surgical care, and it is estimated that about 10% of all pediatric fingertip injury patients require surgery with general anesthesia.13 In our study, patients most commonly presented with a fracture, and 25% of all patients required surgical intervention; 10% received immediate surgery. Need for immediate versus delayed surgery may be affected by the time between when the patient was injured and when they presented to the ED. Our retrospective data do not provide this time frame, but other studies have found that most patients present within 25 or 4 hours,9 indicating that families perceive that these injuries require urgent care.5,9
Patients who were referred from an outside institution were 2.31 times as likely to need surgery (95% CI: 1.98-2.69). This finding can be construed in 2 ways. One interpretation is that the referrals were appropriate, in that more patients who were referred from an outside institution actually needed an intervention. However, considering the actual frequencies, the alternative interpretation is that only 43% of those referred from an outside institution required surgery and that this percentage should be higher. In other words, 57% of those who were referred from an outside institution did not need acute intervention and could have been treated without emergency referral, thus saving costs and family burden.
Charges
With an average length of stay of 3 hours 45 minutes, and more than 1 follow-up visit on average, these injuries are expensive to facilities, patients, and families. In the calendar year 2014, the average charge to patients who presented to the BCH ED with a fingertip injury was $1195. This amount is higher than the average charge of $1064 for patients who presented with a fever—the most common condition seen in the ED (Figure 4). If the average charge in 2014 of $1195 was applied to each of the patients included in this study, this would amount to about $320 430 each year for fingertip injuries in our institution. These preventable injuries place an additional financial burden on the health care system, and an undue burden on emergency services. There are also additional indirect costs associated with these cases, including cost of transportation (especially if referred from another facility), and time lost from work and school for emergency visits, procedures, and follow-up appointments.
Prevention
Fingertip injuries are expensive and stressful for patient families13 and often result in pain,1,6 difficulty performing daily tasks,1 and time lost at work or school.6 In some cases, fingertip injuries impact the patient’s body image,6 and patients and their families also experience anxiety or psychological trauma.1 In an era of focus on preventative care and conserving health care resources, we should consider increasing education and awareness.11 There is a strong need for prevention strategies around the most common fingertip injuries—crushed fingers among preschool children. In the absence of regulations for door safety measures, we can draw from examples used to keep doors from closing (eg, a stopper in the door hinge or at the bottom of the door; a plastic guard to cover the exposed hinge) or to limit the impact of a door closing on fingers (eg, a piece of rubber fitted over the hinge to make it “pinch-free”).7 Some of these strategies are already at work and have changed the pattern of injuries that are seen in the hand clinics. For example, some car doors have been changed to be lighter with electronic tracking rather than just a hinge, with slowing at closure and mechanical stops. Over time and as technologies advance, these types of innovations will hopefully decrease pediatric fingertip injuries. Last, parents need to be made aware of the causes of fingertip injuries at different ages, and educated on how to prevent them.7
Limitations
There are multiple limitations of this study, some of which have been outlined in the discussion already. Retrospective data are not as clean, and a prospective analysis of a large group of patients is likely to uncover many other nuances that cannot be construed from this study. There were incomplete data on some patients as noted in the results, and this may skew the results. In addition, financial data on charges that were submitted by the hospital are an underestimate of the charges incurred by these patients, as charges for consultations in the ED by specialists (ie, plastic or orthopedic surgeons) are not captured.
Conclusions
A large series of fingertip injuries in children is presented herein. The demographics and epidemiological data reflect and support previous, smaller studies. The distribution of injuries stratified by age group suggests that the most common preventable injuries are crush injuries in preschool children. Given the significant cost and health burden of these injuries, it is worthwhile to consider prevention strategies and educational measures to prevent them from occurring.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: This article does not contain any studies with human or animal subjects.
Statement of Informed Consent: Data were reported in aggregate only, and this study was limited to the review of health information on patients, and was granted expedited review by the Institutional Review Board at Boston Children’s Hospital in Boston, Massachusetts, U.S.A. (IRB-P00000386).
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Al-Anazi AF. Fingertip injuries in paediatric patients—experiences at an emergency centre in Saudi Arabia. J Pak Med Assoc. 2013;63(6):675-679. [PubMed] [Google Scholar]
- 2. Al-Qadhi S, Chan KJ, Fong G, Al-Shanteer S, Ratnapalan S. Management of uncomplicated nail bed lacerations presenting to a children’s emergency department. Pediatr Emerg Care. 2011;27:379-383. [DOI] [PubMed] [Google Scholar]
- 3. Benson LS, Waters PM, Meier SW, Visotsky JL, Williams CS. Pediatric hand injuries due to home exercycles. J Pediatr Orthop. 2000;20(1):34-39. [PubMed] [Google Scholar]
- 4. Bhende MS, Dandrea LA, Davis HW. Hand injuries in children presenting to a pediatric emergency department. Ann Emerg Med. 1993;22:1519-1523. [DOI] [PubMed] [Google Scholar]
- 5. Claudet I, Toubal K, Carnet C, et al. When doors slam, fingers jam! [abstract only]. Arch Pediatr. 2007;14(8):958-963. (In French). [DOI] [PubMed] [Google Scholar]
- 6. de Alwis W. Fingertip injuries. Emerg Med Australas. 2006;18(3):229-237. [DOI] [PubMed] [Google Scholar]
- 7. Doraiswamy NV. Childhood finger injuries and safeguards. Inj Prev. 1999;5:298-300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Doraiswamy NV, Baig H. Isolated finger injuries in children—incidence and aetiology. Injury. 2000;31(8):571-573. [DOI] [PubMed] [Google Scholar]
- 9. Fetter-Zarzeka A, Joseph MM. Hand and fingertip injuries in children. Pediatr Emerg Care. 2002;18(5):341-345. [DOI] [PubMed] [Google Scholar]
- 10. Gellman H. Fingertip-nail bed injuries in children: current concepts and controversies of treatment. J Craniofac Surg. 2009;20:1033-1035. [DOI] [PubMed] [Google Scholar]
- 11. Innis PC. Office evaluation and treatment of finger and hand injuries in children. Curr Opin Pediatr. 1995;7(1):83-87. [DOI] [PubMed] [Google Scholar]
- 12. Kubus M, Andrzejewska E, Kuzanski W. Fingertip injuries in children treated in Department of Pediatric Surgery and Oncology in the years 2008-2010 [abstract only]. Ortop Traumatol Rehabil. 2011;13(6):547-554. [DOI] [PubMed] [Google Scholar]
- 13. Macgregor DM, Hiscrox JA. Fingertip trauma in children from doors. Scot Med J. 1999;44(4):114-115. [DOI] [PubMed] [Google Scholar]
- 14. Patel L. Management of simple nail bed lacerations and subungual hematomas in the emergency department. Pediatr Emerg Care. 2014;30(10):742-745. [DOI] [PubMed] [Google Scholar]
- 15. Russell RC, Casas LA. Management of fingertip injuries [abstract only]. Clin Plast Surg. 1989;16(3):405-425. [PubMed] [Google Scholar]
- 16. Shah SS, Rochette LM, Smith GA. Epidemiology of pediatric hand injuries presenting to United States emergency departments, 1990 to 2009. J Trauma Acute Care Surg. 2002;72: 1688-1694. [DOI] [PubMed] [Google Scholar]
- 17. Vadivelu R, Dias JJ, Burke FD, Stanton J. Hand injuries in children: a prospective study. J Pediatr Orthop. 2006;26(1):29-35. [DOI] [PubMed] [Google Scholar]
- 18. Wang QC, Johnson BA. Fingertip injuries. Am Fam Physician. 2001;63(10):1961-1966. [PubMed] [Google Scholar]


