Abstract
Patient: Male, 60
Final Diagnosis: Hepatocellular carcinoma
Symptoms: None
Medication: —
Clinical Procedure: Hepatectomy
Specialty: Surgery
Objective:
Unusual clinical course
Background:
Carbon dioxide (CO2) is believed to be the safest gas for laparoscopic surgery, which is a standard procedure. We experienced severe cerebral infarction caused by paradoxical CO2 embolism during laparoscopic liver resection with injury of the hepatic vessels despite the absence of a right-to-left systemic shunt.
Case Report:
A 60-year-old man was diagnosed with hepatocellular carcinoma in the right hepatic lobe secondary to alcoholic liver disease. We planned the laparoscopy-assisted liver resection. During the surgery, the root of the right hepatic vein was injured. A 1.5-cm hole was accidentally made in the right hepatic vein, while mobilizing the right hepatic lobe laparoscopically. End-tidal CO2 dropped from 39 to 15.5 mmHg, and systemic blood pressure dropped from 121 to 45 mmHg, returning to normal with the administration of inotropes. The transesophageal echocardiography revealed numerous bubbles in the left atrium and ventricle. The Bispectral Index monitoring system showed low brain activity, suggesting cerebral infarction due to paradoxical gas embolism. The hepatectomy was completed by conversion to open laparotomy. The patient went into a coma and suffered quadriplegia after surgery, despite the cooling of his head and the administration of Thiamylal. Brain MRI revealed cerebral infarction in the broad area of the cerebral cortex right side predominantly, with poor blood flow confirmed by the brain perfusion single-photon emission CT. Rehabilitation was gradually achieved with Botox injections.
Conclusions:
Cerebral infarction by paradoxical gas embolism is a rare complication in laparoscopic surgery, but it is important to be aware of the risk and to be prepared to treat it.
MeSH Key Words: Cerebral Infarction; Embolism, Paradoxical; Hepatectomy; Laparoscopy
Background
Laparoscopic surgery is a common procedure with many advantages, such as a short hospital stay, little blood loss, and reduced post-operative pain. In laparoscopic surgery, positive-pressure insufflation of the peritoneal cavity with carbon dioxide (CO2) is critical to allow for visualization. The biggest advantage of CO2 for laparoscopic surgery is its high solubility in plasma, resulting in rapid absorption of CO2 and its elimination through the lungs. This can decrease the risk of CO2 embolization during laparoscopic surgery. Venous CO2 embolism can occur if a large amount of CO2 enters the vascular systems [1], but it rarely happens in humans: the incidence rate is approximately 0.15% for all types of laparoscopic surgery, 0.06% for laparoscopic cholecystectomy, and 0.2–1.5% for laparoscopic major hepatectomy [2].
Paradoxical gas embolism describes the entry of gas from the venous circulation into the systemic arterial circulation through a right-to-left systemic shunt, such as an atrial septal defect (ASD), ventricular septal defect (VSD), or patent foramen ovale (PFO) [1]. Paradoxical gas embolism can cause cerebral gas embolism, which is also very rare, but it is fatal when it occurs. According to published reports, most patients who developed cerebral gas embolism showed delayed recovery from general anesthesia, a transitional stage of impaired consciousness, or transient hemiparesis [3], but there are no reports of severe cerebral infarction due to cerebral CO2 embolism in laparoscopic liver resection.
Here, we present a case of severe cerebral infarction caused by CO2 embolism during laparoscopic liver resection with injury of the hepatic vessels, despite the absence of a right-to-left systemic shunt.
Case Report
The patient, a 60-year-old man, was diagnosed with hepatocellular carcinoma (HCC) secondary to alcoholic liver disease, and was admitted to hospital for surgery. He was slightly obese, 168 cm in height, and 91 kg in body weight, resulting in a body mass index of 32 kg/m2. His past medical history showed hypertension and post-laparoscopic cholecystectomy. His liver function was preserved, with total serum bilirubin of 0.7 mg/dL, prothrombin time-international normalized ratio (PT-INR) of 1.0, serum albumin of 2.8 g/dL, and AST of 32.6 U/L, demonstrating Class A with Child-Pugh score. The tumor located in the superior and posterior portion of the liver (segment 7) was 1.6 cm, and it was close to the right hepatic vein (Figure 1).
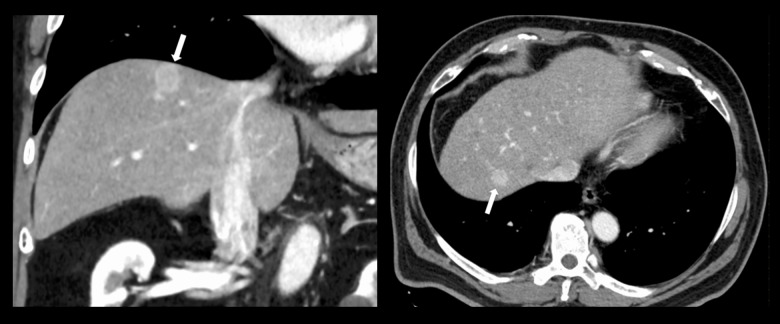
Figure 1.
Dynamic computed tomography (CT). Coronal and axial CT with contrast revealed early enhanced hepatocellular carcinoma (HCC) in segment 7 with 1.6 cm in diameter located just below the diaphragm (white arrow).
We planned the laparoscopy-assisted liver resection, which entails open liver parenchymal resection following laparoscopic mobilization of the right lobe of the liver. This procedure allowed us to perform the hepatectomy with only an upper midline incision, without needing the right subcostal incision, giving us the advantage of less post-operative pain as well as an anticipated early recovery. After the central line was inserted from the right internal jugular vein, the operation started with the patient’s head up and his body in a left lateral position. Intra-abdominal pressure was maintained at 10 mmHg using CO2 and central venous pressure was around 10 mmHg during the laparoscopic procedure. When mobilization of the right hepatic lobe was almost complete, the root of the right hepatic vein was injured by the energy device. We found a 1.5-cm hole at the root of the right hepatic vein (Figure 2). The hole was immediately covered by the instrument for organ traction during the conversion to laparotomy to prevent bleeding and to prevent more gas from entering the hepatic vein after stopping insufflation of CO2. The patient’s position was changed from left semi-lateral to supine position for the laparotomy. End-tidal (ET) CO2 dropped from 39 to 17.2 mmHg, and the anesthesiologist introduced the transesophageal echocardiogram (TEE), which showed many bubbles in the left atrium and ventricle (Video 1). Systemic blood pressure was maintained above 100 mmHg with inotropes support and 100% oxygen was given, although systemic blood pressure dropped from 121 to 45 mmHg for several minutes. As soon as the bubbles were observed in the left atrium and ventricle, the Bispectral Index™ (BIS™) (Covidien, Dublin, Ireland) monitoring system, which links to the electroencephalogram (EEG), was introduced to evaluate brain activity. The BIS monitoring system revealed low activity in the brain, suggesting cerebral infarction due to paradoxical gas embolism. As soon as the abdomen was opened, the hole on the right hepatic vein was closed using 5-0 Prolene. Partial liver resection was completed with a right hemi-hepatic inflow occlusion to avoid small intestinal congestion. Cooling of the head and administration of thiamylal were performed to protect the brain during the open hepatectomy. The patient was transferred to the ICU for further observation and his body temperature was kept low using the Arctic Sun 5000 device (Medivance, Louisville, CO) to minimize brain damage. Fentanyl and Thiamylal were discontinued immediately in the ICU, and glycerol was given daily for 1 week after surgery.
Figure 2.
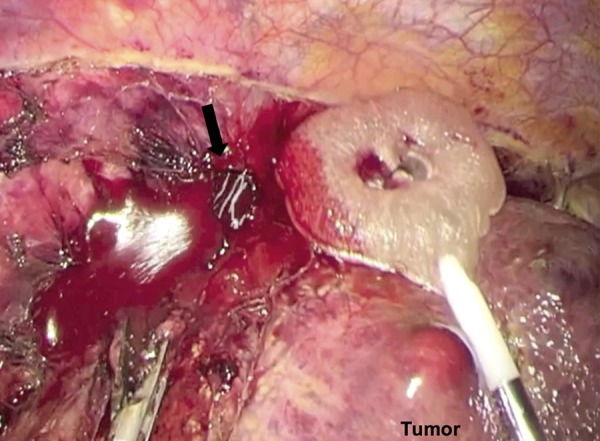
Bleeding from the hole in the right hepatic vein. The hole (black arrow) was covered by the instrument to avoid further bleeding and further infiltration of CO2 into the vein until conversion to laparotomy.
Video 1.
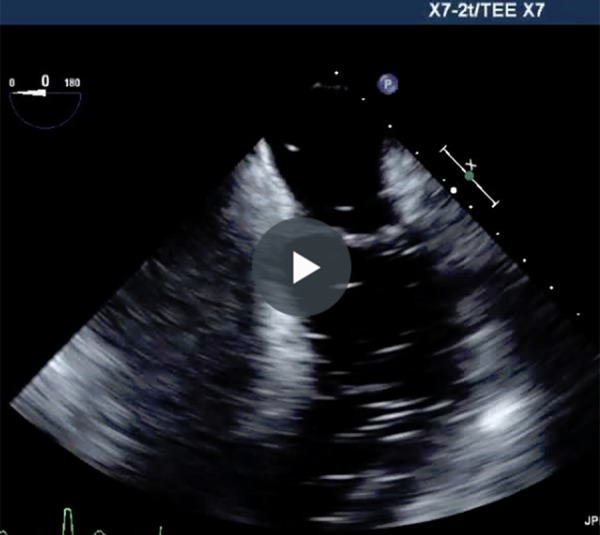
Transesophageal echocardiogram (TEE) after right hepatic vein injury. TEE showed many bubbles in the left atrium and ventricle.
Despite these intensive treatments, he went into a coma and suffered quadriplegia after surgery. Brain MRI revealed multiple cerebral infarction, predominantly in the right side of the cerebral cortex (Figure 3). He showed decorticate rigidity with 3 points by the Glasgow Coma Scale score. Edaravone (3-methyl-1-phenyl-2-pyrazolin-5-one: free radical scavenger) was given for 2 weeks after surgery to prevent brain damage. He presented left-sided hemispatial neglect, was on a feeding tube, and required a low level of oxygen. Liver function improved and became normal 2 weeks after surgery, but poor blood flow was observed in the same area where MRI showed an infarction, confirmed by the brain 123 I-IMP single-photon emission (SPECT) on day 41 after the operation (Figure 4). To determine if the patient had right-to-left systemic shunt in the lung or heart, he received cardiac echo and 99mTc-macroaggregated albumin (MAA) lung perfusion scintigraphy. Cardiac echo revealed no thrombus, ASD, VSD, or PFO. There was no atrial fibrillation on the electrocardiogram monitoring. 99mTc- MAA lung perfusion scintigraphy revealed no right-to-left shunt in the lung, with shunt ratio of 7.9% (normal <15%). Five months after the operation, no HCC recurrence was seen. His neurological status improved slowly with intensive rehabilitation. Six months after the operation, he was able to obey commands to close his eyes, stick out his tongue, and turn his head. The patient still suffers from quadriplegia, but he is able to eat. He recognizes family members. The spasticity in both his arms has lessened through botulinum toxin A (Botox) administration and daily rehabilitation. The pathology report showed moderately differentiated hepatocellular carcinoma with severe liver fibrosis.
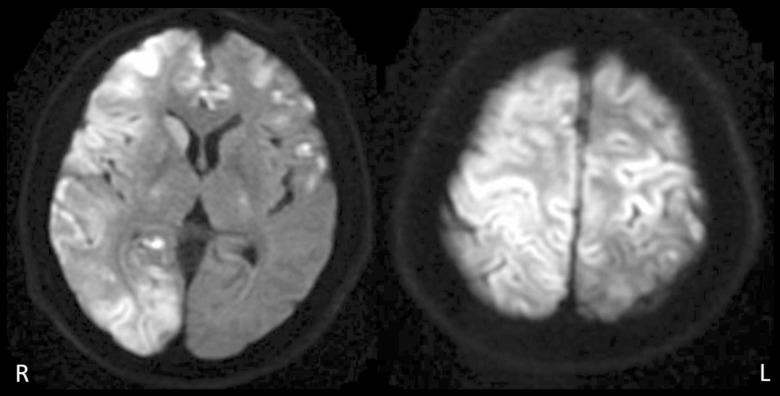
Figure 3.
Magnetic resonance imaging (MRI) of brain after paradoxical CO2 embolism. Diffusion-weighted image showed broad cerebral infarction in the right side of the cerebral hemisphere, predominantly on day 3 after the operation.
Figure 4.
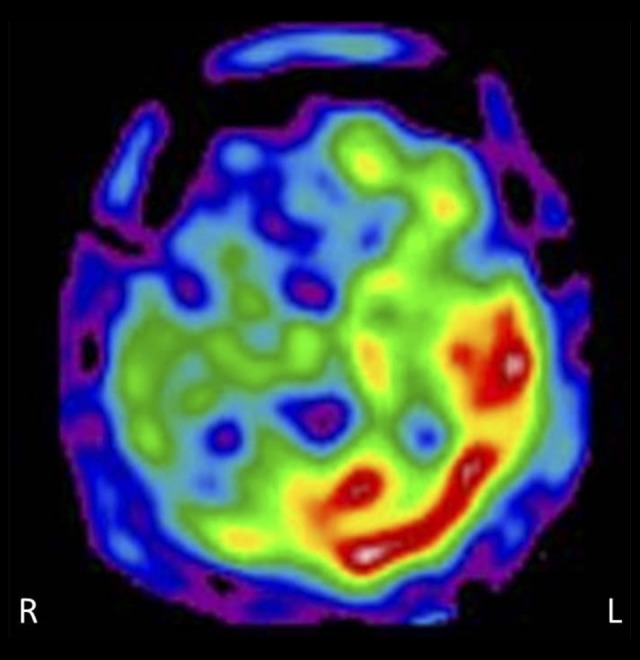
Brain single-photon emission computed tomography (SPECT) after paradoxical CO2 embolism. Brain 123 I-IMP SPECT showed poor cerebral blood flow in the same area where MRI suggested cerebral infarction on day 41 after the operation.
Discussion
CO2 embolism is a dangerous complication of laparoscopic surgery, and associated with a high mortality rate of 28% [4]. If the CO2 enters the portal venous system, the CO2 may be trapped by the liver. CO2, which passes through the liver, may be trapped by the lung. From this point of view, liver surgery appears to carry a higher chance of CO2 embolism because hepatic veins drain directly into the inferior vena cava (IVC). Some cases of paradoxical air embolism during open hepatectomy were reported due to a middle hepatic vein injury or pulmonary shunt secondary to liver cirrhosis, but the patients were discharged with no neurological deficits [5,6]. These reports indicate that there is a high risk of air/gas embolism in either open or laparoscopic hepatectomy, because air/gas passing through the injured hepatic vein goes to the heart or lung without a filter system, which is also true for pulmonary shunt secondary to liver cirrhosis. Laparoscopic liver surgery, in particular, requires positive intra-abdominal pressure using CO2, as well as a head-up position, to obtain a good surgical view. Therefore, CO2 often enters the lung through IVC and the heart. Animal studies demonstrate that CO2 embolism was found in 19 of the 26 cases of laparoscopic liver resection by TEE, but 18 of the 19 animals did not show significant hemodynamic changes, indicating that CO2 embolism during laparoscopic hepatectomy occurs frequently and this finding appears to be nominal [7].
According to a literature review that included 10 papers, 3 cases (0.2%) of gas embolism were reported among 1262 patients who underwent laparoscopic major hepatectomy [2]. First symptoms of CO2 embolism were reported as hypotension, bradycardia, arrhythmia, cardiovascular collapse, or asystole [8]. ET-CO2 monitoring has been suggested as a sensitive and non-invasive tool to monitor CO2 embolism, and most reports showed that a significant decrease in ET-CO2 suggested CO2 embolism, as we experienced in this case [8]. Since CO2 embolism was suspected, we next introduced the TEE, which is the most sensitive for detecting gas embolism, observed myocardial wall motion, and intracardiac bubbles [9].
It surprised us to find paradoxical gas embolism during surgery by TEE. Paradoxical gas embolism is caused by gas going from venous circulation to arterial circulation, and it is a rare complication of laparoscopic surgery.
There are some reports of cerebral gas embolism in laparoscopic surgery. Previously, a young live donor, who underwent laparoscopic right nephrectomy, died of cerebral gas embolism shortly after the operation due to an injured right phrenic vein [10]. There are also reports of patients who developed transient hemiparesis after gynecologic laparoscopy [11] or laparoscopic cholecystectomy [3], and patients who fell into an unexpected coma due to cerebral ischemia confirmed by MRI after laparoscopic partial hepatectomy [12]. Their symptoms were resolved within 5 days after the operation and they were discharged without any complications or sequelae.
In our case, it is not exactly clear why paradoxical gas embolism occurred with the entry of CO2 through the injured right hepatic vein despite no evidence of the right-to-left shunt in both heart and lung. There are 3 possible explanations: (1) elevated right atrium pressure transported the gas bubbles into the arterial circulation through transiently opened PFO, which can be detected in about 30% of the general population, although patent PFO was not clearly observed by TEE in this case during the operation; (2) paradoxical gas embolism occurred through intrapulmonary shunt caused by pulmonary vascular dilatation and arteriovenous communication secondary to liver cirrhosis, which is seen at 15–45% of patients with liver cirrhosis [13]; and (3) spilling over of venous gas bubbles into the arterial circulation through the lung [1]. It was difficult to rule out the possibility of transiently opened PFO caused by increased pressure on the right side of the heart, but the patient was not conscious enough to perform a Valsalva maneuver after the operation in order to increase right atrial pressure provoking the opening of a PFO, but opened PFO was not observed by TEE with manual positive-pressure ventilation during surgery. The results from the cardiac echo and the 99mTc-MAA lung perfusion scintigraphy suggest that the spilling over of venous CO2 bubbles is the most likely explanation for the paradoxical CO2 embolism. There is a report of a paradoxical air embolism during an extended right hepatectomy [5], or right hepatectomy confirmed by TEE with no evidence of ASD, PFO, and VSD [6], but those patients did not show any clinical evidence of neurological sequelae.
To avoid cerebral infarction by gas embolism during laparoscopic hepatectomy, both cautious dissection of the liver and cautious liver parenchymal dissection without major vessel injury are, of course, necessary. Several ways to address the hepatic vein injury during laparoscopic liver resection have been reported. Conversion to laparotomy, like we did, might be the standard procedure, although some reports show primary closure of injured hepatic vein by a laparoscopic stitching technique [14]. It is important that the patient’s position be changed from head up to Trendelenburg position (head down) to avoid gas entering the lung and the heart after stopping insufflation of CO2. Despite all the procedures we completed, cerebral infarction by gas embolism still occurred in this case.
To the best of our knowledge, this is the first report of cerebral paradoxical gas embolism in laparoscopic liver surgery, with severe neurological dysfunctions.
Conclusions
Paradoxical gas embolization may occur without evidence of an apparent right-to-left shunt during laparoscopic surgery. It is a rare but serious complication, which could cause cerebral infarction with severe neurological deficits. Surgeons, anasthesiologists and OR staffs should be aware of this potentially devastaing complication, share the risk information, and prepare for early diagnosis and treatment. Patient also should be informed of possible injury of the hepatic vessels during laparoscopic hepatectomy and potential risk of this complication.
Footnotes
Conflict of interest
The authors declare no conflict of interest associated with this manuscript.
References:
- 1.Muth C, Shank E. Gas embolism. N Engl J Med. 2000;342:476–82. doi: 10.1056/NEJM200002173420706. [DOI] [PubMed] [Google Scholar]
- 2.Otsuka Y, Katagiri T, Ishii J, et al. Gas embolism in laparoscopic hepatectomy: what is the optimal pneumoperitoneal pressure for laparoscopic major hepatectomy? J Hepatobiliary Pancreat Sci. 2013;20:137–40. doi: 10.1007/s00534-012-0556-0. [DOI] [PubMed] [Google Scholar]
- 3.Hye Young S, Dong Wook K, Ju Deok K, et al. Paradoxical carbon dioxide embolism during laparoscopic cholecystectomy as a cause of cardiac arrest and neurologic sequelae. Korean J Anesthesiol. 2014;67:425–28. doi: 10.4097/kjae.2014.67.6.425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gutta CN, Oniub T, Mehrabia A, et al. Circulatory and respiratory complications of carbon dioxide insufflation. Dig Surg. 2004;21:95–105. doi: 10.1159/000077038. [DOI] [PubMed] [Google Scholar]
- 5.Foo E, Williams D, Singh H, et al. Successful management of a large air embolus during an extended right hepatectomy with an emergency cardiopulmonary bypass. HPB (Oxford) 2012;14:871–73. doi: 10.1111/j.1477-2574.2012.00550.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee SY, Choi BIW, Kim JS, Park KS. Paradoxical air embolism during hepatic resection. Br J Anaesth. 2002;88:136–38. doi: 10.1093/bja/88.1.136. [DOI] [PubMed] [Google Scholar]
- 7.Jayaraman S, Khakhar A, Yang H, et al. The association between central venous pressure, pneumoperitoneum, and venous carbon dioxide embolism in laparoscopic hepatectomy. Surg Endosc. 2009;23:1206–9. doi: 10.1007/s00464-009-0359-9. [DOI] [PubMed] [Google Scholar]
- 8.Cottin V, Delafosse B, Viale J. Gas embolism during laparoscopy: A report of seven cases in patients with previous abdominal surgical history. Surg Endosc. 1996;10:166–69. doi: 10.1007/s004649910038. [DOI] [PubMed] [Google Scholar]
- 9.Schmandra T, Mierdl S, Bauer H, et al. Transoesophageal echocardiography shows high risk of gas embolism during laparoscopic hepatic resection under carbon dioxide pneumoperitoneum. Br J Surg. 2002;89:870–76. doi: 10.1046/j.1365-2168.2002.02123.x. [DOI] [PubMed] [Google Scholar]
- 10.Boghossian T, Henri M, Dubé S, et al. Laparoscopic nephrectomy donor death due to cerebral gas embolism in a specialized transplant center: Risk zero does not exist. Transplantation. 2005;79:258–59. doi: 10.1097/01.tp.0000141757.64379.8f. [DOI] [PubMed] [Google Scholar]
- 11.Hieber C, Ihra G, Nachbar S, et al. Near-fatal paradoxical gas embolism during gynecological laparoscopy. Acta Obstet Gynecol Scand. 2000;79:898–99. [PubMed] [Google Scholar]
- 12.Van Gorp V, Diltoer M, Delvaux G, Verborgh C. Delayed recovery following laparoscopic partial hepatectomy. Eur J Anaesthesiol. 2012;29:105–7. doi: 10.1097/EJA.0b013e32834c149f. [DOI] [PubMed] [Google Scholar]
- 13.Hopkins W, Waggoner A, Barzilai B. Frequency and significance of intrapulmonary right to left shunting in end-stage hepatic disease. Am J Cardiol. 1992;70:516–19. doi: 10.1016/0002-9149(92)91200-n. [DOI] [PubMed] [Google Scholar]
- 14.Li H, Wei Y. Hepatic vein injuries during laparoscopic hepatectomy. Surg Laparosc Endosc Percutan Tech. 2016;26:e29–31. doi: 10.1097/SLE.0000000000000244. [DOI] [PubMed] [Google Scholar]