Abstract
Murine gammaherpesvirus 68 (γHV68), like Epstein-Barr virus (EBV), establishes a chronic infection in its host by gaining access to the memory B-cell reservoir, where it persists undetected by the host's immune system. EBV encodes a membrane protein, LMP1, that appears to function as a constitutively active CD40 receptor, and is hypothesized to play a central role in EBV-driven differentiation of infected naive B cells to a memory B-cell phenotype. However, it has recently been shown that there is a critical role for CD40-CD40L interaction in B-cell immortalization by EBV (K.-I. Imadome, M. Shirakata, N. Shimizu, S. Nonoyama, and Y. Yamanashi, Proc. Natl. Acad. Sci. USA 100:7836-7840, 2003), indicating that LMP1 does not adequately recapitulate all of the necessary functions of CD40. The role of CD40 receptor expression on B cells for the establishment and maintenance of γHV68 latency is unclear. Data previously obtained with a competition model, demonstrated that in the face of CD40-sufficient B cells, γHV68 latency in CD40-deficient B cells waned over time in chimeric mice (I.-J. Kim, E. Flano, D. L. Woodland, F. E. Lund, T. D. Randall, and M. A. Blackman, J. Immunol. 171:886-892, 2003). To further investigate the role of CD40 in γHV68 latency in vivo, we have characterized the infection of CD40 knockout (CD40−/−) mice. Here we report that, consistent with previous observations, γHV68 efficiently established a latent infection in B cells of CD40−/− mice. Notably, unlike the infection of normal C57BL/6 mice, significant ex vivo reactivation from splenocytes harvested from infected CD40−/− mice 42 days postinfection was observed. In addition, in contrast to γHV68 infection of C57BL/6 mice, the frequency of infected naive B cells remained fairly stable over a 3-month period postinfection. Furthermore, a slightly higher frequency of γHV68 infection was observed in immunoglobulin D (IgD)-negative B cells, which was stably maintained over a period of 3 months postinfection. The presence of virus in IgD-negative B cells indicates that γHV68 may either directly infect memory B cells present in CD40−/− mice or be capable of driving differentiation of naive CD40−/− B cells. A possible explanation for the apparent discrepancy between the failure of γHV68 latency to be maintained in CD40-deficient B cells in the presence of CD40-sufficient B cells and the stable maintenance of γHV68 B-cell latency in CD40−/− mice came from examining virus replication in the lungs of infected CD40−/− mice, where we observed significantly higher levels of virus replication at late times postinfection compared to those in infected C57BL/6 mice. Taken together, these findings are consistent with a model in which chronic virus infection of CD40−/− mice is maintained through virus reactivation in the lungs and reseeding of latency reservoirs.
Gammaherpesviruses establish a lifelong latent infection within lymphocytes of their respective hosts. Significantly, there is a close association between gammaherpesvirus infection and the development of a diverse set of lymphomas and other tumors. The human gammaherpesviruses Epstein-Barr virus (EBV) and Kaposi's sarcoma-associated herpesvirus (KSHV; also called human herpesvirus 8) have been implicated in the development of a wide range of cancers. EBV is often associated with the development of Burkitt's lymphoma, Hodgkin's disease, gastric carcinoma, and nasopharyngeal carcinoma (for reviews, see references 31, 33, 48, 51, and 64), and there are close associations of KSHV with Kaposi's sarcoma, primary effusion lymphomas, and a variant of multicentric Castleman's disease (11-13, 21, 42).
For both EBV and KSHV, B lymphocytes represent the major reservoir of latent virus; however, KSHV is also known to establish latency in macrophages and dendritic cells (3, 15, 16, 38, 49, 50). Although little is known about KSHV latency in vivo, EBV latency has been relatively well characterized. In sites of active viral replication, such as the tonsils, EBV is found in a variety of B-cell subsets; however, long-term EBV latency in the periphery resides almost exclusively in resting memory B cells (2, 3, 24, 28, 34). Recent data support a model by which EBV gains access to this subset of long-lived B cells by appropriating control of normal B-cell differentiation (reviewed in references 39, 49, and 51). This model suggests that EBV is able to drive B-cell activation through the expression of nine viral gene products (six nuclear antigens [EBNAs] and three membrane proteins [LMPs]) in what is referred to as the “growth program” or latency III program of viral gene expression (4, 27). Some of these EBV growth-transformed lymphoblasts are hypothesized to form germinal centers, with a concomitant downregulation of viral gene expression with expression of EBNA1, LMP1, and LMP2a (4, 5, 9). LMP1 and LMP2A are able to provide surrogate CD40 and BCR engagement signals, respectively, which play important roles in B-cell differentiation and survival during the germinal center reaction and thus facilitating differentiation into memory B cells.
Because of the restricted host ranges of EBV and KSHV and the lack of suitable nonhuman primate models, it is difficult to directly address questions pertaining to the mechanisms involved in the establishment of long-term latency in vivo. Murine gammaherpesvirus 68 (γHV68; also known as MHV-68) infection of mice provides a tractable small-animal model in which central questions pertaining to gammaherpesvirus biology, pathogenesis, and lymphomagenesis can be addressed in the context of a natural host. γHV68 was originally isolated from bank voles in Slovakia (7) and was recently shown to be endemic in European wood mice (6). On the basis of the genomic sequence of γHV68, the virus is closely related to both EBV and KSHV (57). Infection of mice with γHV68 results in an acute, productive infection within the lungs, followed by rapid clearance (46). Concomitant with this process, the virus establishes latency in a variety of tissues, including the spleen, lymph nodes, and bone marrow. B lymphocytes, macrophages, dendritic cells, and possibly lung epithelial cells are all known latency reservoirs (19, 44, 47, 60). As observed with EBV infection, long-term γHV68 latency is narrowly confined to cells expressing a memory B-cell phenotype (20, 62).
It is unclear if γHV68 gains access to the memory B-cell compartment in a manner similar to that proposed for EBV. In a recent report analyzing γHV68 latency in CD40+/CD40− mixed bone marrow chimera mice, the authors demonstrated that viral latency was progressively lost in cells lacking CD40 (30). Furthermore, as expected, they only detected CD40+ B cells in the germinal centers of these infected chimeric mice. These results suggest that access of γHV68 to the memory B-cell compartment may be more reliant upon conventional B-cell activation and differentiation pathways than is the case for EBV. However, these authors did not assess whether γHV68, at least transiently, accesses the memory B-cell reservoir in CD40− B cells and thus they could not rule out the possibility that there is a role for CD40 in the maintenance of γHV68 latency in memory B cells rather than an essential role for CD40 in accessing the memory B-cell reservoir.
The studies described here were aimed at addressing the requirement for CD40 in γHV68 gaining access to memory B cells, as well as to evaluate the ability of γHV68 to establish and maintain long-term latency in mice lacking CD40. CD40 is a surface glycoprotein belonging to the tumor necrosis factor receptor family (43, 53) and is expressed on a wide variety of cell types such as B lymphocytes and specialized antigen-presenting cells, including macrophages and dendritic cells (56). CD40 interactions with its cognate ligand (CD40L [CD154/gp39]) on T cells underpin many of the significant T-cell-dependent B-cell differentiation, survival, and antibody production pathways. As a consequence, CD40-deficient mice are unable to form germinal centers, have impaired memory B-cell formation, and do not generate isotype-switched antibodies in a T-cell-dependent manner (29). We have examined γHV68 latency and reactivation from latency in bulk splenocytes and various sorted splenocyte populations in CD40-deficient mice.
MATERIALS AND METHODS
Virus and tissue culture.
γHV68 clone WUMS (ATCC VR1465) was passaged in and its titers were determined on NIH 3T12 cells as described previously (14). NIH 3T12 and mouse embryonic fibroblast (MEF) cells were maintained in Dulbecco's modified Eagle's medium supplemented with 10% fetal calf serum, 100 U of penicillin per ml, 100 mg of streptomycin per ml, and 2 mM l-glutamine (cMEM). MEF cells were obtained as described previously (36), by homogenizing C57BL/6J day 12 embryos, plating the resulting homogenate in tissue culture flasks for 7 to 14 days, and harvesting adherent cells by trypsinization.
Mice, infections, and organ harvests.
CD40−/− (29) and wild-type C57BL/6J mice (catalog no. 002928/000664; The Jackson Laboratory, Bar Harbor, Maine) were housed and bred at the Yerkes Vivarium in accordance with all federal, university, and facility regulations. Mice were anesthetized with isoflurane and inoculated intranasally with 1,000 PFU of γHV68 in 20 μl of cMEM. Mice were anesthetized prior to sacrifice by cervical dislocation, and spleens and lungs were harvested and treated as described below. Sentinel mice were assayed every 3 months and were negative for adventitious mouse pathogens by parasitology and serology.
Plaque assays.
Plaque assays were performed as described previously, with modifications (55). Briefly, six-well plates were seeded with 2 × 105 NIH 3T12 cells 1 day prior to infection. Lung samples were thawed and mechanically disrupted in 1 ml of medium containing 100 μl of 1.0-mm-diameter zirconia-silica beads (Biospec Products, Inc., Bartlesville, Okla.) with a Mini-Beadbeater-8 (Biospec Products, Inc.) for four 1-min pulses. Serial 10-fold dilutions of lung homogenates were plated onto NIH 3T12 monolayers in a 200-μl volume and allowed to adsorb for 1 h at 37°C with periodic rocking. Samples were overlaid with 5 ml of medium containing 2% methylcellulose and maintained at 37°C. Plaques were scored microscopically 5 to 7 days postplating. All titers were determined in parallel with a laboratory standard with a known titer. The limit of detection of this assay is 50 PFU per organ.
Cell preparation and flow cytometry cell purification.
Single-cell suspensions were generated by disrupting spleens with a TenBroek homogenizer and filtering the homogenate through a 100-um-pore-size nylon cell strainer (Becton Dickinson, Franklin Lakes, N.J.). Following red blood cell lysis, cells were collected by centrifugation, washed, refiltered, enumerated, and assayed for viability with trypan blue (Sigma, St. Louis, Mo.). Rat anti-mouse CD16/CD32 (Fc Block) was used to block Fc receptors prior to staining. Cells were stained for fluorescence-activated cell sorter (FACS) analysis with a phycoerythrin-conjugated antibody directed against CD19 and a fluorescein isothiocyanate-conjugated antibody to immunoglobulin D (IgD; BD Pharmingen). Stained cell populations were sorted expeditiously with a FACSVantage SE (Becton Dickinson, Mountain View, Calif.) or MoFlo (Cytomation, Fort Collins, Colo.) flow cytometer. Data were analyzed with FloJo software (TreeStar, Inc., San Carlos, Calif.). The resultant purified cell populations were resuspended in cMEM supplemented with 10% dimethyl sulfoxide and stored at −80°C for limiting-dilution PCR assays or at 4°C in cMEM for limited-dilution ex vivo reactivation assays as described below. Pooled splenocytes from 5 to 15 mice were used in all experiments.
Frequency of reactivation of virus from latency in cells upon explant culture.
The frequency of reactivation of virus from latency in cells was determined by a limiting-dilution ex vivo reactivation assay (58, 60). Briefly, unsorted splenocytes or purified cell populations were obtained from mice at 16, 42, and 84 days postinfection (dpi). Cells were resuspended in cMEM and plated in serial twofold dilutions (starting with 105 cells) onto MEF monolayers in 96-well plates. Twenty-four replicate wells were plated per dilution, and 12 dilutions were plated per sample. The appearance of a cytopathic effect (CPE) was monitored microscopically at days 14 and 21 postplating. The contribution to reactivation from preformed infectious virus was determined by parallel plating of mechanically disrupted cells (latent virus cannot reactivate from killed cells). This procedure kills >99% of the cells but has only negligible effects on virus titers (58-60).
Frequency of γHV68 viral genome-positive cells.
The frequency of cells harboring the γHV68 genome was determined by a single-copy sensitivity nested PCR assay directed against the γHV68 ORF50 gene sequence as described previously (59, 60). Briefly, the bulk of FACS-sorted splenocytes generated at 16, 42, and 84 dpi were thawed, counted, and resuspended in isotonic buffer. A series of six threefold serial dilutions, starting with 104 cells per well, were plated in a background of 104 uninfected NIH 3T12 cells in 96-well PCR plates. Cells were lysed prior to nested PCR by overnight treatment at 65°C in the presence of detergent and proteinase K. Each experimental plate included both negative and positive control wells to ensure optimal assay sensitivity. All cell lysis and PCR protocols were performed as described previously (59, 60) on a PrimusHT thermal cycler (MWG Biotech). All of the assays reported herein demonstrated near-single-copy sensitivity in the absence of any false-positive PCRs. Twelve replicate PCRs were performed for each cell dilution per sample per experiment.
Measurement of chronic viral persistence in the lungs.
Persistent viral replication in the lungs was measured by a modified form of the limiting-dilution ex vivo reactivation assay described above. Briefly, the lower left lobe of the lung from each animal was pooled into 500 μl of cMEM and mechanically disrupted as described previously (55). The homogenate was brought up to 5 ml with cMEM and plated in twofold serial dilutions onto MEFs in 96-well tissue culture plates. Six dilutions of 24 replicate wells were plated. The appearance of a CPE was monitored microscopically and read 10 to 12 days postplating. Pooled lung lobes from five mice were used in all experiments.
Statistical analysis.
GraphPad Prism software (GraphPad Software, San Diego, Calif.) was used for all data analysis. Frequencies of viral genome-positive cells or reactivation from latency were calculated on the basis of a Poisson statistical distribution in which the intersect of 63.2% represents a single-cell event. Nonlinear regression analysis with a best-fit sigmoidal dose-response algorithm was applied to the experimental data to obtain single-cell frequencies.
RESULTS
Acute γHV68 replication in the lungs is unaffected by the absence of CD40 following intranasal inoculation.
To assess the potential effects of CD40 on acute viral replication, we infected CD40−/− and wild-type C57BL/6J mice intranasally with 1,000 PFU of wild-type γHV68. Lungs were harvested from these mice at both 4 and 9 dpi, and viral titers were determined by plaque assay on murine NIH 3T12 fibroblast monolayers as described in Materials and Methods. Figure 1 demonstrates that at early times postinfection, virus replication in the lungs of CD40−/− mice was indistinguishable from that observed in C57BL/6J mice (ca. 447 versus 385 PFU/ml at 4 dpi and 13,680 versus 11,803 PFU/ml at 9 dpi, respectively). These findings indicate that acute viral replication in the lungs is unaffected by the absence of CD40.
FIG. 1.
Acute-phase γHV68 titers are unaffected by the host mouse strain. C57BL/6J and CD40−/− mice were inoculated with 1,000 PFU of wild-type γHV68, and their lungs were harvested at 4 and 9 dpi. The data shown were compiled from single experiments with 9 or 10 individual mice. Virus titers from lung homogenates were determined by plaque assay on NIH 3T12 monolayers as described in Materials and Methods. Each point represents the virus titer from an individual mouse. The solid line represents the mean virus titer for each group of mice, and the dashed line represents the limit of detection of this assay (50 PFU).
Reactivation from latency in γHV68-infected CD40−/− mice.
Spleens were harvested from γHV68-infected CD40−/− mice at various time points, and single-cell suspensions of splenocytes were generated as described in Materials and Methods. The frequency of reactivation of virus from latency in cells was determined by a limiting-dilution ex vivo reactivation assay (58, 59). For this analysis, splenocytes were enumerated and assessed for viability by trypan blue exclusion and live spleen cells were plated in serial twofold dilutions onto permissive indicator monolayers of MEFs. Spontaneous virus reactivation resulted in a pronounced CPE, which was scored microscopically. To evaluate the contribution to reactivation from preformed infectious virus in the samples, a parallel series of cells were plated following mechanical disruption to kill cells but leave preformed virus intact, as previously described (58, 59).
Examination of infected splenocytes at 16 dpi demonstrated readily detectable levels of reactivation (ca. 1 in 39,000) (Fig. 2 and Table 1). This level of reactivation is approximately 5- to 20-fold lower than we have routinely observed in γHV68-infected C57BL/6J mice at 16 dpi (23, 35, 52, 62). It is possible that this decrease in the reactivation frequency can be attributed to an inherent reactivation defect in latently infected CD40−/− cells, a defect in the ability of γHV68 to establish latency, or both. However, on the basis of the acute virus replication data (Fig. 1), it is unlikely that this defect reflects altered seeding of latency reservoirs.
FIG. 2.
γHV68 reactivation from latency in CD40−/− mice. Unsorted splenocytes or purified splenic cell populations were obtained from γHV68-infected CD40−/− mice at the times indicated and subjected to analysis for reactivation upon explant culture. Serial dilutions of intact (live) cells were plated onto MEF indicator monolayers in parallel with samples that had been mechanically disrupted. The level of reactivation that could be attributed to preformed infectious virus was either undetectable or very low (data not shown). Best-fit curves were derived from nonlinear regression analysis, and each symbol represents the mean percentage of wells positive for a virus-induced CPE ± the standard error of the mean. The dashed line represents 63.2%, from which the frequency of genome-positive cells or the frequency of cell reactivation of virus was calculated with a Poisson distribution. The data shown represent at least two independent experiments with pooled cells from 10 to 15 mice per experimental group.
TABLE 1.
Frequency of cells reactivating γHV68 in explant cultures of unsorted splenocytes
| Day postinfection | Frequency of splenocytes reactivating virus
|
||
|---|---|---|---|
| Frequencya | Total no. of cellsb | Total no. of cells reactivatingc | |
| 16 | 1/39,000 | 9.0 × 107 | 2,310 |
| 42 | 1/80,000 | 5.4 × 107 | 675 |
| 84 | NDd | 5.2 × 107 | N/Ae |
Frequency of cells reactivating represents the mean of at least two independent experiments with splenocytes pooled from 10 to 15 mice per experimental group.
Cell numbers were derived from total numbers of live cells per spleen at 16, 42, and 84 dpi.
The total number of reactivating cells was determined by using the experimental frequency data and the estimated total numbers of cell per subset.
ND, not determined as values were below the limit of detection of the assay and were deemed statistically invalid.
N/A, not applicable as calculations could not be done because of a lack of determined frequencies.
Although the frequency of splenocyte reactivation of virus at 16 dpi in latently infected CD40−/− mice was decreased compared to that in wild-type C57BL/6 mice, virus reactivation from CD40−/− mouse splenocytes was readily detectable (ca. 1 in 80,000) at 42 dpi (Fig. 2 and Table 1). This is in contrast to numerous reports indicating an inability to detect reactivation of wild-type γHV68 from latently infected splenocytes at later time points (e.g., 42 dpi) (26, 58, 59, 62). Furthermore, low levels of reactivation were also seen as late as 84 dpi from infected CD40−/− mice (Fig. 2 and Table 1). In all of our assays, the levels of preformed infectious virus in the splenocyte samples were either undetectable or too low to quantitate (data not shown). The latter is consistent with the reported efficient clearance of acutely replicating virus from the spleen by 12 to 14 dpi (46). Thus, the observed virus growth in ex vivo limiting-dilution analyses could be exclusively attributed to reactivation from latency.
γHV68 infection of the spleen is efficiently maintained over a 3-month period in CD40−/− mice.
Although reactivation frequencies in CD40−/− mice at 16 dpi were slightly lower than those seen for infection of wild-type mice (62), it was unclear if this was a consequence of a defect in the ability of γHV68 to establish latency in this particular knockout strain. To assess this, we determined the frequency of splenocytes harboring the viral genome with a limiting-dilution PCR assay, as described in Materials and Methods. Spleens from infected mice were harvested at 16, 42, and 84 dpi. Bulk splenocytes were serially diluted and proteinase K treated, and the resulting lysate was subjected to a nested PCR assay to detect the viral genome. By calculating the percentage of replicate wells scoring positive for a PCR product at each dilution and applying a Poisson distribution, we were able to determine the frequency of cells harboring the viral genome at various time points postinfection. The results of this analysis indicated the presence of latent virus at all of the time points tested. The frequency of viral genome-positive cells at 16 dpi was approximately 1 in 3,750 splenocytes (Fig. 3 and Table 2), and this frequency remained relatively constant over the time course of the study. Frequencies of viral genome-positive cells at 42 and 84 dpi were determined to be approximately 1 in 2,450 and 1 in 5,400, respectively (Fig. 3 and Table 2).
FIG. 3.
γHV68 splenic latency in CD40−/− mice. Unsorted and FACS-sorted splenocytes were obtained from CD40−/− mice at 16, 42, and 84 dpi. The frequency of viral genome-positive cells within these cell populations was determined by a limiting-dilution PCR assay as described in Materials and Methods. The data shown represent at least two independent experiments with pooled cells from 10 to 15 mice per experimental group. Curve fit lines were derived from nonlinear regression analysis, and symbols represent mean percentages of wells positive for viral DNA. The error bars represent the standard error of the mean. The dotted line represents 63.2%, from which the frequency of viral genome-positive cells was calculated with a Poisson distribution.
TABLE 2.
Analysis of frequency of cells harboring γHV68 in splenocyte populations
| Cell fraction | Time (dpia) | Frequency of viral genome-positive splenocytes
|
||
|---|---|---|---|---|
| Frequencyb | Total no. of cellsc | No. of latently infected cellsd | ||
| Unsorted | 16 | 1/3,750 | 9.0 × 107 | 24,000 |
| 42 | 1/2,450 | 5.4 × 107 | 22,040 | |
| 84 | 1/5,400 | 5.2 × 107 | 9,700 | |
| CD19+ | 16 | 1/2,500 | 4.8 × 107 | 19,225 |
| 42 | 1/2,200 | 4.1 × 107 | 18,800 | |
| 84 | 1/2,500 | 2.8 × 107 | 11,110 | |
| CD19− | 16 | NDe | 4.2 × 107 | N/Af |
| 42 | ND | 1.3 × 107 | N/A | |
| 84 | ND | 2.4 × 107 | N/A | |
| CD19+ IgD+ | 16 | 1/18,900 | 4.4 × 107 | 2,340 |
| 42 | 1/7,500 | 3.9 × 107 | 5,190 | |
| 84 | 1/9,000 | 2.6 × 107 | 2,840 | |
| CD19+ IgD− | 16 | 1/600 | 3.8 × 106 | 6,300 |
| 42 | 1/560 | 1.7 × 106 | 3,035 | |
| 84 | 1/515 | 2.2 × 106 | 4,270 | |
dpi, days postinfection.
Frequency of viral genome-positive cells represents the mean of at least two independent experiments with splenocytes pooled from 10 to 15 mice per experimental group.
Cell numbers were derived from the total number of cells per spleen at 16, 42, and 84 dpi (9.0 × 107, 5.4 × 107, and 5.2 × 107, respectively) and the percentage of total spleen cells that each subset represents as calculated from FACS gating at days 16 and 84 (CD19+, 53.4%; CD19−, 46.6%; CD19+ IgD+, 49.2%; CD19+ IgD−, 4.2.%) and at day 42 (CD19+, 76.6%; CD19−, 24.9%; CD19+ IgD+, 72.0%; CD19+ IgD−, 3.1%).
The total number of latently infected cells or reactivating cells was determined by using the experimentally determined frequency of genome-positive cells and the estimated total number of cells per subset.
ND, not determined as values were either very low or below the limit of detection of the assay and were deemed statistically invalid.
N/A, not applicable as calculations could not be done because of a lack of determined frequencies.
By combining results obtained from the reactivation assay with data obtained from this limiting-dilution PCR assay, we could calculate the efficiency of reactivation at each time point. The calculated efficiency of reactivation at 16 dpi was 9.6% of latently infected cells that underwent spontaneous reactivation upon explant culture. This number decreased to 3.1% by 42 dpi. The ability of γHV68 to reactivate from latency in CD40−/− mice is not markedly different from that of 10.8% reported for wild-type mice at 16 dpi (62). Thus, the decreased reactivation frequency observed in CD40−/− mice compared to historical data on C57BL/6J mice at 16 dpi can be largely accounted for by a decrease in the frequency of cells harboring virus at 16 dpi in CD40−/− mice. However, by 42 dpi the observed frequency of latently infected splenocytes in CD40−/− mice was very similar to that historically observed in C57BL/6J mice (1 in 2,450 versus 1 in ca. 3,000, respectively).
B cells are the predominant splenic latency reservoir in CD40−/− mice.
From the analysis presented above, γHV68 is able to establish and maintain long-term latency in the spleen. Although γHV68 can establish latency in a variety of cell types and maintain long-term splenic latency in memory B cells in wild-type mice, it was unclear what subset(s) of splenocytes harbored latent γHV68 in CD40−/− mice. Initially we purified B-cell and non-B-cell populations by FACS, following the staining of bulk splenocytes with an antibody directed against the pan-B-cell marker CD19 (data not shown). CD19+ (B) and CD19− (non-B) cells were purified to mean purities of 97.4 and 99.4%, respectively, and subjected to limiting-dilution PCR analyses to determine the frequency of cells harboring the viral genome in each population (Fig. 3). This analysis revealed a marked propensity for γHV68 to establish latency within the B-cell population. Notably, B cells harbored high levels of latent virus at early times postinfection, and this frequency of viral genome-positive cells remained constant over the time course of the study (ca. 1 in 2,200 to 2,500) (Fig. 3 and Table 2). In contrast, the frequency of latent virus in the non-B-cell subset was either very low or undetectable, which precluded any valid frequency analysis (Fig. 3 and Table 2). On the basis of calculations of the total numbers of latently infected B cells compared to the total number of latently infected cells within bulk unsorted splenocytes, the virus present within B cells accounts for most of the virus present in bulk splenocytes (Table 2).
Having established that B cells represent the predominant splenic reservoir of γHV68 latency in CD40−/− mice, we extended the above analysis to assess virus infection of specific B-cell subsets. In wild-type mice, both germinal-center and memory B cells harbor very high frequencies of latent virus at early times postinfection, and memory B cells are known to be a critical reservoir for long-term latency (20, 62). However, because CD40−/− mice exhibit a profound defect in the development of memory B cells, it was unclear if γHV68 would preferentially partition into any specific B-cell subset in CD40−/− mice. Thus, B cells were sorted on the basis of cell surface expression of IgD (Fig. 4). Mature, naive B cells express high levels of IgD on their surface, and this expression is down-regulated during B-cell differentiation within the germinal center. Spleen cells were isolated at various times postinfection and stained with antibodies directed against CD19 and IgD and sorted into naive (CD19+ IgD+) and CD19+ IgD− B cells (Fig. 4). Notably, CD40−/− mice have a significant population of surface IgD− B cells (ca. 5%), which is only slightly reduced compared to that of C57BL/6 mice. Analysis of virus infection in these B-cell populations revealed that both naive and IgD− B cells harbor high levels of latent γHV68 (Fig. 3). Interestingly, IgD− B cells harbored a ca. 15- to 30-fold higher frequency of latent virus than that in naive B cells (Fig. 3 and Table 2). Importantly, the purity of the CD19+ IgD− B-cell population was 95% and CD19− non-B cells, which harbor a very low frequency of latent virus, were the major contaminating population (Fig. 4). Thus, latency observed in the IgD− B-cell population could not be accounted for by contaminating naive B cells. Furthermore, the frequency of viral genome-positive cells within each cell population did not deviate significantly over a 3-month time course (Fig. 3; Table 2), in contrast to infection of normal C57BL/6J mice, in which naive B-cell infection rapidly declines by 3 months (20, 23) and is not detectable by 6 months postinfection (62). The total number of latently infected cells observed within the sorted IgD− and IgD+ B-cell populations did not completely account for that observed in the bulk B-cell fraction; however, this is most likely due to the loss of virus-infected cells because conservative FACS gates were set.
FIG. 4.
FACS analysis of splenocyte populations in CD40−/− mice. Splenocytes collected from CD40−/− mice were isolated and prepared as described in Materials and Methods. Purification of B-cell and non-B-cell fractions was based on surface expression of the pan-B-cell marker CD19 (data not shown). Purified B cells (CD19+) were further fractionated into naive (IgD+) and IgD− B cells with a fluorescein isothiocyanate-conjugated antibody to IgD. Representative FACS plots from one replicate experiment are shown. (A) Presorting analysis of total splenocytes stained with antibodies directed against CD19 and IgD. (B) Postsorting FACS analysis indicating the purity of sorted lymphocyte subsets. Mean postsorting purities were as follows: CD19+, 97.4% ± 2.0%; CD19−, 99.4% ± 0.9%; CD19+ IgD+, 95.0% ± 5.2%; CD19+ IgD−, 94.8% ± 0.6.%. The contaminating fractions for B-cell and non-B-cell fractions were 2.5 and 0.6%, respectively. Contamination within the naive B-cell fraction was 0.45% IgD− B cells, and contamination within the IgD− B-cell population with naive B cells was 2.5%.
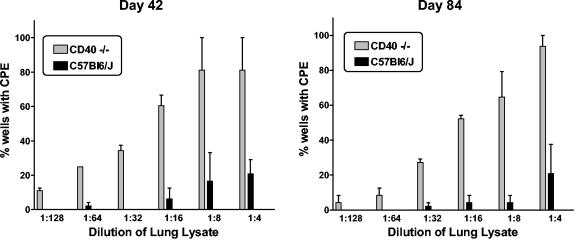
CD40 knockout mice are unable to clear persistent γHV68 replication from the lungs.
As noted above, one intriguing observation was that latent virus was maintained in all B-cell populations at significant levels and did not appear to decrease markedly over the duration of the study. It is noteworthy that γHV68 was able to maintain moderate levels of latent virus in the naive B-cell population to at least 3 months postinfection. This is in sharp contrast to γHV68 infection of wild-type mice, in which latent γHV68 infection of naive B cells decreases rapidly from 16 to 42 dpi and is undetectable by 6 months postinfection (62). Although γHV68 infection in wild-type mice is usually cleared from the lungs by 10 to 12 dpi, CD40−/− mice have impaired T-cell-dependent antibody responses and clearance of virus from sites of acute replication may be compromised in these animals. An inability to clear lytic virus from the lungs could provide a source of virus, which then serves to seed sites of latency, such as the spleen, and thus maintain latency reservoirs that have a relatively short half-life (e.g., naive B cells).
To examine ongoing virus replication in the lungs of infected mice, we harvested infected lung tissue from both CD40−/− and wild-type C57BL/6J control mice, prepared lysates as described in Materials and Methods, and limiting dilution plated these lysates onto MEFs. This analysis revealed that, as previously shown (55), by 42 dpi C57BL/6J mice have very low levels of replicating virus in the lungs (Fig. 5). However, significantly more virus was detected in the lungs of CD40−/− mice at both 42 and 84 dpi (Fig. 5).
FIG. 5.
Persistent γHV68 viral replication in the lungs of CD40−/− mice. Lung homogenates from γHV68-infected CD40−/− and C57BL/6J mice were generated at 42 and 84 dpi as described in Materials and Methods. Serial dilutions of lung homogenates were plated onto MEF indicator monolayers and scored microscopically for the presence of a CPE 10 to 12 days postplating. Twenty-four replicates were plated per dilution. The data represent two replicate experiments with pooled lungs from five mice per experiment.
DISCUSSION
The prototypic gammaherpesvirus EBV establishes and maintains life-long latency within memory B lymphocytes in its human host. It is widely accepted that EBV gains access to this cell type via manipulation of normal B-cell differentiation pathways. Activation of B cells in response to antigen relies upon specific interactions with T-helper cells, costimulation, and the appropriate cytokine milieu. Activated B lymphocytes traffic to primary lymphoid follicles at anatomic locations such as the spleen or lymph nodes and initiate rapid rounds of proliferation, resulting in the de novo generation of a germinal center. It is within this germinal center that isotype switching, affinity maturation, commitment to plasma cell lineage, and generation of B-cell memory take place. The ability of EBV to manipulate this process relies in part upon two virus-encoded gene products, LMP1 and LMP2a. Together, these gene products are able to provide requisite signals for B-cell activation, differentiation, and survival during this highly selective process.
γHV68 infection of mice, which is gaining popularity as a small-animal model for human gammaherpesvirus infections, exhibits some striking similarities to EBV latency. Acute infection of mice with γHV68 manifests itself as a mononucleosis-like syndrome, followed by the establishment of life-long latency (46). The development of lymphomas has also been reported in mice infected with γHV68 (45). Importantly, like that of EBV, long-term latency of γHV68 is narrowly restricted to memory B cells (20, 62), which suggests that gammaherpesviruses may have evolved common mechanisms for gaining access to this particular cell type. Memory B cells are known to be long-lived, can traffic throughout the host via the peripheral blood, and are able to take up residence in numerous anatomic locations, including the spleen, bone marrow, and thymus. However, in contrast to EBV, γHV68 does not appear to encode homologues of LMP1 and LMP2a (57) and it is unclear whether γHV68 actively promotes B-cell activation and differentiation to gain access to the memory B-cell reservoir. Recent experiments monitoring γHV68 infection and latency within CD40 mixed bone marrow chimeric mice demonstrated a role for CD40 in the persistence of virus infection (30). These results suggest that γHV68 may rely to a greater extent upon non-virus-encoded B-cell differentiation pathways to gain access to and/or persist within memory B cells. It is also possible that γHV68 gains access to this compartment via direct infection of memory B cells. However, it is important to note with respect to the role of CD40 in gammaherpesvirus infection of B cells that it has recently been shown that CD40 plays an important role in EBV infection even though EBV LMP1 mimics many aspects of CD40 signaling (25). The latter studies showed that EBV infection of naive B cells results in upregulation of CD40L expression on EBV B lymphoblasts, which appears to play a critical role by engaging CD40 on the surface of infected B lymphoblasts. Thus, the requirement of CD40 to persist within the infected host may reflect a role for CD40 in maintaining latency within memory B cells.
The experiments described here were aimed at further defining the requirement for CD40 in γHV68 infection of murine B cells in vivo. Although we observed at early times postinfection a decreased frequency of latently infected B cells in CD40−/− mice than has been routinely observed in normal C57BL/6J mice, γHV68 was able to establish a stable chronic infection in these mice. This decreased frequency of latently infected cells observed at early times postinfection was not due to an inherent replication or packaging defect in CD40−/− mice, as γHV68 replicated to comparable titers in the lungs of CD40−/− and CD57Bl/6 mice during the acute phase of infection. Notably, infection of both naive IgD+ B cells and more mature IgD− B cells was observed and, as has been previously reported for infection of immunocompetent mice, infection was biased toward the IgD− population of B cells (62). Thus, in the absence of competition from CD40-sufficient B cells, γHV68 can persist in CD40−/− B cells. However, it also seems likely that chronic infection of B cells in CD40−/− mice is driven by persistent virus replication in the lungs and reseeding of B-cell latency.
The data presented here are in good agreement with a recent report by Kim et al. (30) demonstrating efficient establishment of latency in cells lacking CD40 and suggest that involvement of CD40 is not required at least for the early stages of latency. In contrast to a prior report (32), we did not observe any deaths in CD40−/− mice as a result of infection with γHV68 within the first 6 months postinfection. This discrepancy most likely represents the difference between the inoculating doses used, with our studies using 10-fold less virus. Importantly, we have observed a 50% mortality rate from 8 to 10 months postinfection, while no deaths were observed in control infected C57BL/6 mice (data not shown).
In contrast to γHV68 infection of wild-type mice, we could readily detect virus reactivation at 42 dpi, and low levels of reactivating virus could be seen as late as 3 months postinfection. The ability to detect viral reactivation at later times postinfection likely stems from the inability of these mice to effectively clear lytic virus from the lungs. In wild-type mice, acutely replicating virus is efficiently cleared from the lungs by 10 to 12 dpi (46). The clearance is largely effected by an efficient antiviral antibody response and CD8 T-cell response (17). Although Usherwood et al. (54) reported that antiviral antibodies are not required for resolution of acute infection in the lungs, these studies were conducted with mice that lacked B cells, the very cell type within which γHV68 preferentially establishes latency. It is difficult to directly address the role of antiviral antibodies in B-cell knockout mice. We have shown previously that adoptive transfer of immune serum from γHV68-infected C57BL/6J mice can efficiently control lytic-virus titers in mice that lack B cells (μMT) and thus cannot generate appropriate antiviral antibodies (22). We confirmed that CD40−/− mice have only very limited antibody production compared to wild-type C57BL/6J mice by analyzing total antibody levels by enzyme-linked immunosorbent assay in both mock- and γHV68-infected CD40−/− and control wild-type mice (data not shown). It is also formally possible that the inability to control lytic virus in the lungs over the duration of this study may be due in part to a less-than-optimal CD4 T-cell response. Stimulation via CD40 is an important component of this T-cell response, and this may also contribute to failure to control chronic virus replication in the lungs. Finally, engagement of CD40 has been shown for γHV68, as well as EBV and KSHV, to suppress virus reactivation from B cells (1, 41). Thus, the observed chronic virus production in the lungs of CD40−/− may, at least in part, be due to the absence of appropriate suppression of virus reactivation mediated through CD40. Furthermore, the latter could also explain the attrition of latently infected CD40−/− B cells in the experiments performed with mixed bone marrow chimeric mice (30).
It is notable that both surface IgD+ naive B cells and surface IgD− B cells are reservoirs of latent virus and that the surface IgD− subset harbors approximately 15- to 30-fold higher frequencies of latent virus than naive B cells at all of the time points examined. Surface IgD is a faithful marker for naive B cells, which is downregulated during the germinal-center response in wild-type mice. However, mice lacking CD40 are largely unable to generate germinal centers, and in this case the specific identity of these B cells is difficult to ascertain. It is possible that these IgD− B cells may represent marginal-zone B cells or B1 cells (reviewed in reference 40), both of which can exhibit low levels of surface IgD. Moreover, it is formally possible that isotype-switched B cells could be generated in the absence of CD40-CD40L signaling. Indeed, with a cocktail of antibodies directed at identifying isotype-switched IgD−/IgM− B cells we were able to detect a small percentage of bona fide memory B cells (data not shown). This phenomenon has been reported previously in both CD40- and CD40L-deficient mice, which have been shown to generate IgA and IgG isotypes in response to T-cell-independent antigens (10, 29, 37, 63). Furthermore, isotype-switched antibodies are also generated in mice lacking CD40-CD40L signaling in response to various pathogens, including vaccinia virus, lymphocytic choriomeningitis virus, and Borrelia burgdorferi (8, 18, 61). It is formally possible that γHV68 infection of CD40−/− mice results in the generation of isotype-switched antibodies in a T-cell-independent manner, perhaps through reprogramming of B-cell differentiation. However, the small percentage of these cells within the spleen precluded examination of the frequency of viral genome-positive cells in this population.
It remains to be determined whether γHV68 is able to drive differentiation of latently infected naive CD40−/− B cells. Further analysis of γHV68 infection of CD40−/− mice, coupled with an effective approach to stem the contribution to long-term latency from acute lytic virus in the lungs, may offer a more definitive picture of the requirement for memory B cells in the maintenance of long-term latency. Experiments are under way to generate replication-defective viruses to address this issue.
Acknowledgments
S. H. Speck was supported by NIH grants CA43143, CA52004, CA58524, and CA87650. David O. Willer is a Research Fellow of the National Cancer Institute of Canada supported by funds provided by the Terry Fox Run.
We thank Robert E. Karaffa II and Mike Hulsey for cell sorting and analysis and members of the Speck laboratory for helpful comments and discussions.
REFERENCES
- 1.Adler, B., E. Schaadt, B. Kempkes, U. Zimber-Strobl, B. Baier, and G. W. Bornkamm. 2002. Control of Epstein-Barr virus reactivation by activated CD40 and viral latent membrane protein 1. Proc. Natl. Acad. Sci. USA 99:437-442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Babcock, G. J., L. L. Decker, R. B. Freeman, and D. A. Thorley-Lawson. 1999. Epstein-Barr virus-infected resting memory B cells, not proliferating lymphoblasts, accumulate in the peripheral blood of immunosuppressed patients. J. Exp. Med. 190:567-576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Babcock, G. J., L. L. Decker, M. Volk, and D. A. Thorley-Lawson. 1998. EBV persistence in memory B cells in vivo. Immunity 9:395-404. [DOI] [PubMed] [Google Scholar]
- 4.Babcock, G. J., D. Hochberg, and A. D. Thorley-Lawson. 2000. The expression pattern of Epstein-Barr virus latent genes in vivo is dependent upon the differentiation stage of the infected B cell. Immunity 13:497-506. [DOI] [PubMed] [Google Scholar]
- 5.Babcock, G. J., and D. A. Thorley-Lawson. 2000. Tonsillar memory B cells, latently infected with Epstein-Barr virus, express the restricted pattern of latent genes previously found only in Epstein-Barr virus-associated tumors. Proc. Natl. Acad. Sci. USA 97:12250-12255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Blasdell, K., C. McCracken, A. Morris, A. A. Nash, M. Begon, M. Bennett, and J. P. Stewart. 2003. The wood mouse is a natural host for Murid herpesvirus 4. J. Gen. Virol. 84:111-113. [DOI] [PubMed] [Google Scholar]
- 7.Blaskovic, D., M. Stancekova, J. Svobodova, and J. Mistrikova. 1980. Isolation of five strains of herpesviruses from two species of free living small rodents. Acta Virol. 24:468. [PubMed] [Google Scholar]
- 8.Borrow, P., A. Tishon, S. Lee, J. Xu, I. Grewal, M. Oldstone, and R. Flavell. 1996. CD40L-deficient mice show deficits in antiviral immunity and have an impaired memory CD8+ CTL response. J. Exp. Med. 183:2129-2142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brooks, L., D. Hochberg, and D. A. Thorley-Lawson. 2000. The expression pattern of Epstein-Barr virus latent gene transcription in nasopharyngeal carcinoma cells: coexpression of EBNA1, LMP1, and LMP2 transcripts. J. Virol. 66:2689-2697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Castigli, E., F. Alt, L. Davidson, A. Bottaro, E. Mizoguchi, A. Bhan, and R. Geha. 1994. CD40-deficient mice generated by recombination-activating gene-2-deficient blastocyst complementation. Proc. Natl. Acad. Sci. USA 91:12135-12139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cesarman, E., Y. Chang, P. S. Moore, J. W. Said, and D. M. Knowles. 1995. Kaposi's sarcoma-associated herpesvirus-like DNA sequences in AIDS-related body-cavity-based lymphomas. N. Engl. J. Med. 332:1186-1191. [DOI] [PubMed] [Google Scholar]
- 12.Cesarman, E., R. G. Nador, K. Aozasa, G. Delsol, J. W. Said, and D. M. Knowles. 1996. Kaposi's sarcoma-associated herpesvirus in non-AIDS-related lymphomas occurring in body cavities. Am. J. Pathol. 149:53-57. [PMC free article] [PubMed] [Google Scholar]
- 13.Chang, Y., E. Cesarman, M. S. Pessin, F. Lee, J. Culpepper, D. M. Knowles, and P. S. Moore. 1994. Identification of herpesvirus-like DNA sequences in AIDS-associated Kaposi's sarcoma. Science 266:1865-1869. [DOI] [PubMed] [Google Scholar]
- 14.Clambey, E. T., H. W. Virgin IV, and S. H. Speck. 2000. Disruption of the murine gammaherpesvirus 68 M1 open reading frame leads to enhanced reactivation from latency. J. Virol. 74:1973-1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Du, M.-Q., H. Liu, T. C. Diss, H. Ye, R. A. Hamoudi, N. Dupin, V. Meignin, E. Oksenhendler, C. Boshoff, and P. G. Isaacson. 2001. Kaposi sarcoma-associated herpesvirus infects monotypic (IgMλ) but polyclonal naive B cells in Castleman disease and associated lymphoproliferative disorders. Blood 97:2130-2136. [DOI] [PubMed] [Google Scholar]
- 16.Dupin, N., T. L. Diss, P. Kellam, M. Tulliez, M.-Q. Du, D. Sicard, R. A. Weiss, P. G. Isaacson, and C. Boshoff. 2000. HHV-8 is associated with a plasmablastic variant of Castleman disease that is linked to HHV-8-positive plasmablastic lymphoma. Blood 95:1406-1412. [PubMed] [Google Scholar]
- 17.Ehtisham, S., N. P. Sunil-Chandra, and A. A. Nash. 1993. Pathogenesis of murine gammaherpesvirus infection in mice deficient in CD4 and CD8 T cells. J. Virol. 67:5247-5252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fikrig, E., S. Barthold, M. Chen, I. Grewal, J. Craft, and R. Flavell. 1996. Protective antibodies to murine Lyme disease arise independently of CD40 ligand. J. Immunol. 157:1-3. [PubMed] [Google Scholar]
- 19.Flano, E., S. M. Husain, J. T. Sample, D. L. Woodland, and M. A. Blackman. 2000. Latent murine gamma-herpesvirus infection is established in activated B cells, dendritic cells, and macrophages. J. Immunol. 165:1074-1081. [DOI] [PubMed] [Google Scholar]
- 20.Flano, E., I.-J. Kim, D. L. Woodland, and M. A. Blackman. 2002. γ-Herpesvirus latency is preferentially maintained in splenic germinal center and memory B cells. J. Exp. Med. 196:1363-1372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ganem, D. 1997. KSHV and Kaposi's sarcoma: the end of the beginning? Cell 91:157-160. [DOI] [PubMed] [Google Scholar]
- 22.Gangappa, S., S. B. Kapadia, S. H. Speck, and H. W. Virgin IV. 2002. Antibody to a lytic cycle viral protein decreases gammaherpesvirus latency in B-cell-deficient mice. J. Virol. 76:11460-11468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Herskowitz, J., M. Jacoby, and S. H. Speck. 2005. The murine gammaherpesvirus 68 M2 gene is required for efficient reactivation from latently infected B cells. J. Virol. 79:2261-2273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hochberg, D., T. Souza, M. Catalina, J. L. Sullivan, K. Luzuriaga, and D. A. Thorley-Lawson. 2004. Acute infection with Epstein-Barr virus targets and overwhelms the peripheral memory B-cell compartment with resting, latently infected cells. J. Virol. 78:5194-5204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Imadome, K.-I., M. Shirakata, N. Shimizu, S. Nonoyama, and Y. Yamanashi. 2003. CD40 ligand is a critical effector of Epstein-Barr virus in host cell survival and transformation. Proc. Natl. Acad. Sci. USA 100:7836-7840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jacoby, M. A., H. W. Virgin IV, and S. H. Speck. 2002. Disruption of the M2 gene of murine gammaherpesvirus 68 alters splenic latency following intranasal, but not intraperitoneal, inoculation. J. Virol. 76:1790-1801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Joseph, A. M., G. J. Babcock, and D. A. Thorley-Lawson. 2000. Cells expressing the Epstein-Barr virus growth program are present in and restricted to the naive B-cell subset of healthy tonsils. J. Virol. 74:9964-9971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Joseph, A. M., G. J. Babcock, and D. A. Thorley-Lawson. 2000. EBV persistence involves strict selection of latently infected B cells. J. Immunol. 165:2975-2981. [DOI] [PubMed] [Google Scholar]
- 29.Kawabe, T., T. Naka, K. Yoshida, T. Tanaka, H. Fujiwara, S. Suematsu, N. Yoshida, T. Kishimoto, and H. Kikutani. 1994. The immune responses in CD40-deficient mice: impaired immunoglobulin class switching and germinal center formation. Immunity 1:167-178. [DOI] [PubMed] [Google Scholar]
- 30.Kim, I.-J., E. Flano, D. L. Woodland, F. E. Lund, T. D. Randall, and M. A. Blackman. 2003. Maintenance of long term γ-herpesvirus B cell latency is dependent on CD40-mediated development of memory B cells. J. Immunol. 171:886-892. [DOI] [PubMed] [Google Scholar]
- 31.Kuppers, R. 2003. B cells under influence: transformation of B cells by Epstein-Barr virus. Nat. Rev. Immunol. 3:801-812. [DOI] [PubMed] [Google Scholar]
- 32.Lee, B. J., S. K. Reiter, M. Anderson, and S. R. Sarawar. 2002. CD28−/− mice show defects in cellular and humoral immunity but are able to control infection with murine gammaherpesvirus 68. J. Virol. 76:3049-3053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Macsween, K. F., and D. H. Crawford. 2003. Epstein-Barr virus—recent advances. Lancet Infect. Dis. 3:131-140. [DOI] [PubMed] [Google Scholar]
- 34.Miyashita, E. M., B. Yang, G. J. Babcock, and D. A. Thorley-Lawson. 1997. Identification of the site of Epstein-Barr virus persistence in vivo as a resting B cell. J. Virol. 71:4882-4891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Moorman, N. J., D. O. Willer, and S. H. Speck. 2003. The gammaherpesvirus 68 latency-associated nuclear antigen homolog is critical for the establishment of splenic latency. J. Virol. 77:10295-10303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pollock, J. L., and H. W. Virgin IV. 1995. Latency, without persistence, of murine cytomegalovirus in the spleen and kidney. J. Virol. 69:1762-1768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Renshaw, B., W. Fanslow III, R. Armitage, K. Campbell, D. Liggitt, B. Wright, B. Davison, and C. Maliszewski. 1994. Humoral immune response in CD40 ligand-deficient mice. J. Exp. Med. 180:1889-1900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rettig, M. B., H. J. Ma, R. A. Vescio, M. Pold, G. Schiller, D. Belson, A. Savage, C. Nishikubo, C. Wu, J. Fraser, J. W. Said, and J. R. Berenson. 1997. Kaposi's sarcoma-associated herpesvirus infection of bone marrow dendritic cells from multiple myeloma patients. Science 276:1851-1854. [DOI] [PubMed] [Google Scholar]
- 39.Rickenson, A. B., and P. J. Lane. 2000. Epstein-Barr virus: co-opting B-cell memory and migration. Curr. Biol. 10:R120-R123. [DOI] [PubMed] [Google Scholar]
- 40.Sagaert, X., and C. De Wolf-Peeters. 2003. Classification of B-cells according to their differentiation status, their micro-anatomical localisation and their developmental lineage. Immunol. Lett. 90:179-186. [DOI] [PubMed] [Google Scholar]
- 41.Sarawar, S. R., B. J. Lee, S. K. Reiter, and S. P. Schoenberger. 2001. Stimulation via CD40 can substitute for CD4 T cell function in preventing reactivation of a latent herpesvirus. Proc. Natl. Acad. Sci. USA 98:6325-6329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Soulier, J., L. Grollet, E. Oksenhendler, P. Cacoub, D. Cazals-Hatem, P. Babinet, M. F. d'Agay, J. P. Clauvel, M. Raphael, and L. Degos. 1995. Kaposi's sarcoma-associated herpesvirus-like DNA sequences in multicentric Castleman's disease. Blood 86:1276-1280. [PubMed] [Google Scholar]
- 43.Stamenkovic, I., E. A. Clark, and B. Seed. 1989. A B-lymphocyte activation molecule related to the nerve growth factor receptor and induced by cytokines in carcinomas. EMBO J. 8:1403-1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stewart, J. P., E. J. Usherwood, A. Ross, H. Dyson, and T. Nash. 1998. Lung epithelial cells are a major site of murine gammaherpesvirus persistence. J. Exp. Med. 187:1941-1951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sunil-Chandra, N. P., J. Arno, J. Fazakerley, and A. A. Nash. 1994. Lymphoproliferative disease in mice infected with murine gammaherpesvirus 68. Am. J. Pathol. 145:818-826. [PMC free article] [PubMed] [Google Scholar]
- 46.Sunil-Chandra, N. P., S. Efstathiou, J. Arno, and A. A. Nash. 1992. Virological and pathological features of mice infected with murine gamma-herpesvirus 68. J. Gen. Virol. 73:2347-2356. [DOI] [PubMed] [Google Scholar]
- 47.Sunil-Chandra, N. P., S. Efstathiou, and A. A. Nash. 1992. Murine gammaherpesvirus 68 establishes a latent infection in mouse B lymphocytes in vivo. J. Gen. Virol. 73:3275-3279. [DOI] [PubMed] [Google Scholar]
- 48.Thompson, M. P., and R. Kurzrock. 2004. Epstein-Barr virus and cancer. Clin. Cancer Res. 10:803-821. [DOI] [PubMed] [Google Scholar]
- 49.Thorley-Lawson, D. A. 2001. Epstein-Barr virus: exploiting the immune system. Nat. Rev. Immunol. 1:75-82. [DOI] [PubMed] [Google Scholar]
- 50.Thorley-Lawson, D. A., and G. J. Babcock. 1999. A model for persistent infection with Epstein-Barr virus: the stealth virus of human B cells. Life Sci. 65:1433-1453. [DOI] [PubMed] [Google Scholar]
- 51.Thorley-Lawson, D. A., and A. Gross. 2004. Persistence of the Epstein-Barr virus and the origins of associated lymphomas. N. Engl. J. Med. 350:1328-1337. [DOI] [PubMed] [Google Scholar]
- 52.Tibbetts, S. A., J. Loh, V. van Berkel, J. S. McClellan, M. A. Jacoby, S. B. Kapadia, S. H. Speck, and H. W. Virgin IV. 2003. Establishment and maintenance of gammaherpesvirus latency are independent of infective dose and route of infection. J. Virol. 77:7696-7701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Torres, R. M., and E. A. Clark. 1992. Differential increases of an alternatively polyadenylated mRNA species of murine CD40 upon B lymphocyte activation. J. Immunol. 148:620-626. [PubMed] [Google Scholar]
- 54.Usherwood, E. J., J. P. Stewart, K. Robertson, D. J. Allen, and A. A. Nash. 1996. Absence of splenic latency in murine gammaherpesvirus 68-infected B cell-deficient mice. J. Gen. Virol. 77:2819-2825. [DOI] [PubMed] [Google Scholar]
- 55.van Dyk, L. F., H. W. Virgin IV, and S. H. Speck. 2003. Maintenance of gammaherpesvirus latency requires viral cyclin in the absence of B lymphocytes. J. Virol. 77:5118-5126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Van Kooten, C., and J. Banchereau. 1997. Functions of CD40 on B cells, dendritic cells and other cells. Curr. Opin. Immunol. 9:330-337. [DOI] [PubMed] [Google Scholar]
- 57.Virgin, H. W., IV, P. Latreille, P. Wamsley, K. Hallsworth, K. E. Weck, A. J. Dal Canto, and S. H. Speck. 1997. Complete sequence and genomic analysis of murine gammaherpesvirus 68. J. Virol. 71:5894-5904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Weck, K. E., M. L. Barkon, L. I. Yoo, S. H. Speck, and H. W. Virgin IV. 1996. Mature B cells are required for acute splenic infection, but not for establishment of latency, by murine gammaherpesvirus 68. J. Virol. 70:6775-6780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Weck, K. E., S. S. Kim, H. W. Virgin IV, and S. H. Speck. 1999. B cells regulate murine gammaherpesvirus 68 latency. J. Virol. 73:4651-4661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Weck, K. E., S. S. Kim, H. W. Virgin IV, and S. H. Speck. 1999. Macrophages are the major reservoir of latent murine gammaherpesvirus 68 in peritoneal cells. J. Virol. 73:3273-3283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Whitmire, J., M. Slifka, I. Grewal, R. Flavell, and R. Ahmed. 1996. CD40 ligand-deficient mice generate a normal primary cytotoxic T-lymphocyte response but a defective humoral response to a viral infection. J. Virol. 70:8375-8381. Erratum, 71:1736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Willer, D. O., and S. H. Speck. 2003. Long-term latent murine gammaherpesvirus 68 infection is preferentially found within the surface immunoglobulin D-negative subset of splenic B cells in vivo. J. Virol. 77:8310-8321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Xu, J., T. Foy, J. Laman, E. Elliot, J. Dunn, T. Waldschmidt, J. Elsemore, R. Noelle, and R. Flavell. 1994. Mice deficient for the CD40 ligand. Immunity 1:423-431. [DOI] [PubMed] [Google Scholar]
- 64.Young, L. S., and P. G. Murray. 2003. Epstein-Barr virus and oncogenesis: from latent genes to tumours. Oncogene 22:5108-5121. [DOI] [PubMed] [Google Scholar]