Abstract
Ventricular safety pacing (VSP) is used to avoid cross talk by delivering ventricular stimulus shortly after an atrial-paced event if ventricular-sensed event occurs. Although VSP is a protective feature that exists for decades in different pacing devices, there are some reports of unfavorable outcomes of this algorithm. More so, health care providers sometimes face difficulties in interpreting and dealing with VSP strips. This case report discusses an important pacemaker algorithm and encourages further attention to possible pitfalls and hence avoids unnecessary interventions.
Keywords: Pacemakers, ventricular safety pacing
Case Presentation
We present a case of 57-year-old man with dual-chamber permanent pacemakers (PPM) implanted initially for sinus node dysfunction who had “pacing spikes all over” on telemetry 1 day after mitral valve repair and coronary artery bypass grafting. On device interrogation, we noted normally functioning dual-chamber pacemaker (50/130 bpm). Atrial and ventricular lead impedance, sensing, and pacing testing were within normal range.
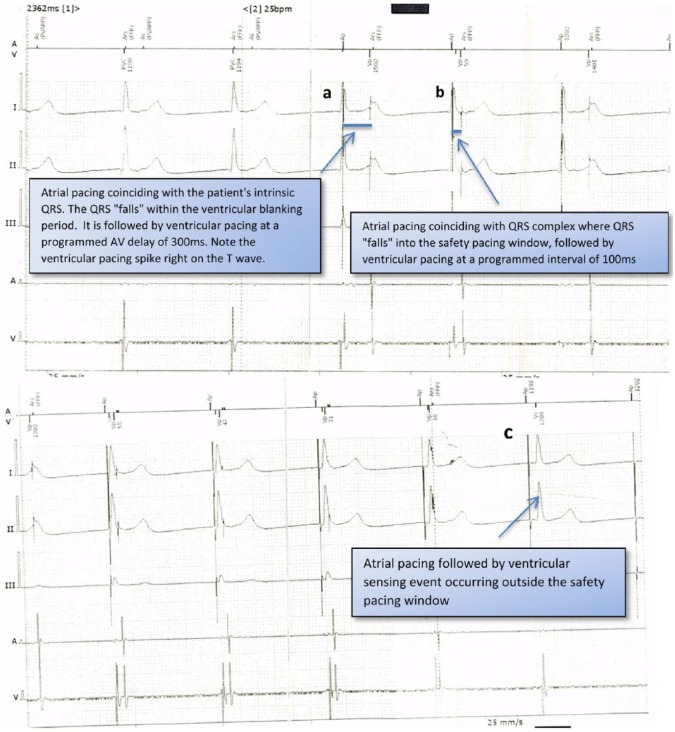
Underlying rhythm was junctional rhythm at 50 bpm. Electrograms (EGMs) showed the following (Figure 1): (a) atrial pacing on R wave followed by ventricular pacing on T wave at programmed atrioventricular delay 300 ms, (b) atrial pacing at the beginning of QRS complex followed by ventricular pacing on R wave at short intervals of 100 ms, and (c) atrial pacing followed by ventricular sensing event at the interval >100 ms. These pacing behaviors were puzzling. In particular, it was unclear why the atrial pacing was introduced on QRS complex, and in other occasions, atrial pacing preceded the QRS and was followed by ventricular pacing 100 ms later. Differential diagnosis at that point was as follows: leads dislodgement after cardiac surgery (as suggested by the manufacturer), atrial lead pacing ventricle, ventricular undersensing, and ventricular loss of capture. Chest x-rays were done prior and post-cardiac surgery and confirmed leads integrity. After reviewing EGMs, we believe that these episodes represent ventricular safety pacing (VSP), which is nonprogrammable feature in all Biotronik devices.
Figure 1.
Ventricular safety pacing due to the patient junctional rhythm coinciding with the programmed device lower rate. Ventricular blanking after atrial pacing = 30 ms and safety pacing window = 100 ms including ventricular blanking.
In this particular case, VSP was not triggered by ventricular oversensing but by underlying junctional rhythm coincidently going at the same rate (50 bpm) as atrial pacing and the QRS complexes are falling into at Safety Pacing Window (100 ms). The initial 30 ms of Safety Window is blanked which explains pacing on T wave. In final programming we increased lower pacemaker rate to 60 bpm to override junctional rhythm, which solved the issue.
Discussion
Several Algorithms have been introduced over the years to enhance PPM and implantable cardioverter defibrillator (ICD) function.1,2 Cross talk is a serious complication that might occur in dual-chamber PPMs and ICDs.3 Ventricular safety pacing is a vital pacemaker function that prevents inhibition of ventricular pacing due to oversensing of an atrial pacing impulse on the ventricular channel, yet VSP algorithm is not entirely without pitfalls.4–6
We present a unique case where a simple algorithm, such as VSP, gets confused by the patient’s underlying rhythm. In rare cases, ventricular sensing immediately after atrial pacing can be due to coinciding junctional rhythm. In our case scenario, atrial pacing was on or immediately before the QRS, and the following junctional beat activated the VSP algorithm. A simple intervention such as increasing lower pacemaker rate has solved the issue. This has avoided further untimely ventricular pacing, and hence, the device continued to function normally. Increasing lower rate not only solved the issue but also eliminated the junctional rhythm and thus confirmed the diagnosis.
Physicians and nurses involved in the care of patients with devices should be familiar with such algorithms’ pitfalls and hence avoid unnecessary interventions.
Footnotes
PEER REVIEW: Four peer reviewers contributed to the peer review report. Reviewers’ reports totaled 353 words, excluding any confidential comments to the academic editor.
FUNDING: The author(s) received no financial support for the research, authorship, and/or publication of this article.
DECLARATION OF CONFLICTING INTERESTS: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions
MS: data collection and writing the manuscript. TP and AS: data collection and contributed to the writing of the manuscript. DN and IL: critical revisions and drafts approval. EC: critical revisions and approved the final draft.
REFERENCES
- 1.Shurrab M, Healey JS, Haj-Yahia S, et al. Reduction in unnecessary ventricular pacing fails to affect hard clinical outcomes in patients with preserved left ventricular function: a meta-analysis [published online ahead of print October 26, 2016] Europace. doi: 10.1093/europace/euw221. [DOI] [PubMed] [Google Scholar]
- 2.Shurrab M, Elitzur Y, Healey JS, et al. VDD vs DDD pacemakers: a meta-analysis. Can J Cardiol. 2014;30:1385–1391. doi: 10.1016/j.cjca.2014.04.035. [DOI] [PubMed] [Google Scholar]
- 3.Helguera ME, Pinski SL. Cross-talk inhibition and asystole resulting from post-shock high-output pacing: a new form of implantable cardioverter-defibrillator proarrhythmia. Heart Rhythm. 2005;2:310–312. doi: 10.1016/j.hrthm.2004.11.020. [DOI] [PubMed] [Google Scholar]
- 4.Hayashi M, Takatsuki S, Messali A, et al. Short-long-short sequence caused by ventricular safety pacing inducing ventricular tachycardia in a patient with a dual-chamber implantable cardioverter defibrillator. Europace. 2008;10:1238–1242. doi: 10.1093/europace/eun176. [DOI] [PubMed] [Google Scholar]
- 5.Debie L, Broers B, van Opstal J, van Gelder BM. Atrioventricular cross-talk leading to ventricular pacing inhibition in a dual-chamber ICD. Case Rep Cardiol. 2011;2011:624508. doi: 10.1155/2011/624508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lim S. Ventricular safety pacing, ventricular sense response, and ventricular tachycardia. Heart Rhythm. 2010;7:567–569. doi: 10.1016/j.hrthm.2009.11.008. [DOI] [PubMed] [Google Scholar]