Abstract
Purpose
In contrast to other US racial/ethnic groups, Asian Americans (AA) have experienced steadily increasing breast cancer rates in recent decades. To better understand potential contributors to this increase, we examined incidence trends by age and stage among women from seven AA ethnic groups in California from 1988 through 2013, and incidence patterns by subtype and age at diagnosis for the years 2009 through 2013.
Methods
Joinpoint regression was applied to California Cancer Registry data to calculate annual percentage change (APC) for incidence trends. Incidence rate ratios were used to compare rates for AA ethnic groups relative to non-Hispanic whites (NHW).
Results
All AA groups except Japanese experienced incidence increases, with the largest among Koreans in 1988–2006 (APC: 4.7, 95% CI: 3.8, 5.7) and Southeast Asians in 1988–2013 (APC: 2.5, 95% CI: 0.8, 4.2). Among women younger than age 50, large increases occurred for Vietnamese and other Southeast Asians; among women over age 50, increasing trends occurred in all AA ethnic groups. Rates increased for distant stage disease among Filipinas (2.2% per year, 95% CI: 0.4, 3.9). Compared to NHW, Filipinas and older Vietnamese had higher incidence rates of some HER2+ subtypes.
Conclusions
Breast cancer incidence rates have risen rapidly among California AA, with the greatest increases in Koreans and Southeast Asians. Culturally-tailored efforts to increase awareness of and attention to breast cancer risk factors are needed. Given the relatively higher rates of HER2-overexpressing subtypes in some AA ethnicities, research including these groups and their potentially unique exposures may help elucidate disease etiology.
Keywords: Asian, Asian American, breast cancer, subtype, trend, HER2Neu
INTRODUCTION
Over the last 15 years, breast cancer incidence has remained stable or declined in most US populations defined by race/ethnicity (1). However, among Asian Americans (AA), incidence has been increasing steadily, at 1.1% from 2003–2012 (1, 2). The AA category is heterogeneous, comprising populations from nearly 30 countries, and differing widely in migration patterns, socioeconomic status, health behaviors, and culture (3–5), all of which contribute to differences in disease incidence (6). Indeed, for breast cancer incidence, research including eight AA populations showed inter-ethnic variation in rate trends over the period 1990–2008, with annual increases ranging from 1.2% among Chinese and Vietnamese to 4.7% among Koreans, but stable rates for Japanese (7). Moreover, several studies have shown that rates in AA women differ by age and nativity, with higher rates among young US-born AA women (8–10). Rapidly increasing incidence rates also have been noted in Asian countries, and international data suggest that among more recent generations, rates in Asian countries may be surpassing rates in the US, particularly those for white women (11).
Breast cancer incidence also varies by disease subtype defined by tumor expression of hormone receptors (HR) and human epidermal growth factor receptor 2 (HER2), and knowledge is growing about the differential impact of risk factors on the incidence of these subtypes (12). Within California, proportionally more breast cancers expressed HER2 relative to HR+/HER2- in Korean, Filipino, Vietnamese, and Chinese women than in non-Hispanic White (NHW) women (13). However, whether subtype-specific incidence rates differ across AA ethnicities is unknown.
Documenting breast cancer incidence trends among distinct AA populations has the potential to help us understand the observed overall increases, to better target prevention and screening efforts, and to guide further research into subtype-specific risk factors. Therefore, utilizing data from the population-based California Cancer Registry (CCR), in a state that is both the largest in US and has the most substantial population of Asian Americans (14), we examined breast cancer incidence patterns from 1988–2013 by detailed AA ethnic groups, age, and stage. For the most recent years of data from 2009–2013, we were also able to explore differences by age and subtype.
METHODS
Study data
Female invasive breast cancer incidence data (ICD-O-3 C50.0–50.9) were obtained from the CCR (comprising four National Cancer Institute Surveillance, Epidemiology and End Results (SEER) program registries) to analyze trends from 1988 through 2013. To examine the incidence patterns by both age and breast cancer subtypes, we focused on the most recent 5-year data (2009 through 2013). We excluded 670 breast sarcomas (histology codes 8800–8801, 8805, 8815, 8830, 8850, 8858, 8890, 8935, 8980, 8982–8983, 9120, 9180–9181, and 9260 (15)). Patient information included race/ethnicity, stage, and age at diagnosis, routinely reported to the registry. We examined AA as a single group and then by seven major AA ethnicities: Chinese, Japanese, Korean, Filipino, Vietnamese, South Asians (Asian Indians and Pakistanis), and Southeast Asians (Cambodians, Laotians, Hmong, Thai). Comparison data were drawn for non-Hispanic whites (NHW).
For each breast cancer, we obtained data on subtype classified based on pathology report review regarding expression of estrogen receptor (ER) and/or progesterone receptor (PR), which are commonly combined for defining HR status, and HER2. HR positivity is based on positive status for ER and/or PR. HER2 has been reported to the CCR since approximately 2000, although data are more complete and clinically relevant (given availability of targeted treatment) in recent years. Subtype analyses focused on the period 2009–2013 and excluded the 11% of breast cancers with unknown ER, PR, and/or HER2 status; the percentages of tumors missing subtype information were similar for AA and NHW. Annual population counts by race/ethnicity were estimated using linear interpolation and extrapolation of 1990, 2000, and 2010 Census counts.
Statistical analysis
We calculated annual cancer incidence rates as cases per 100,000 persons, age-adjusted to the 2000 US standard population, using SEER*Stat software (16). Joinpoint regression models were used to calculate annual percent change (APC) for each AA ethnicity and NHW, for all ages combined and by age group (younger than age 50 (“younger”), ages 50 and over (“older”)). To accommodate the smaller annual case counts in analysis of data by disease stage, we used three-year cumulative rates for determining stage-specific APCs for each AA ethnicity and for NHW (17, 18).
Incidence rate ratios (IRRs) and 95% confidence intervals (CI) were computed relative to NHW for 1988–2013 overall and for 2009–2013 by breast cancer subtype (HR+/HER2−, HR+/HER2+, HR−/HER2+, triple-negative (HR-/HER2-, “TNBC”)). A maximum of five joinpoints was allowed based on single-year data. APCs were considered statistically significant if the associated 95% CI excluded zero.
RESULTS
Incidence trends 1988–2013
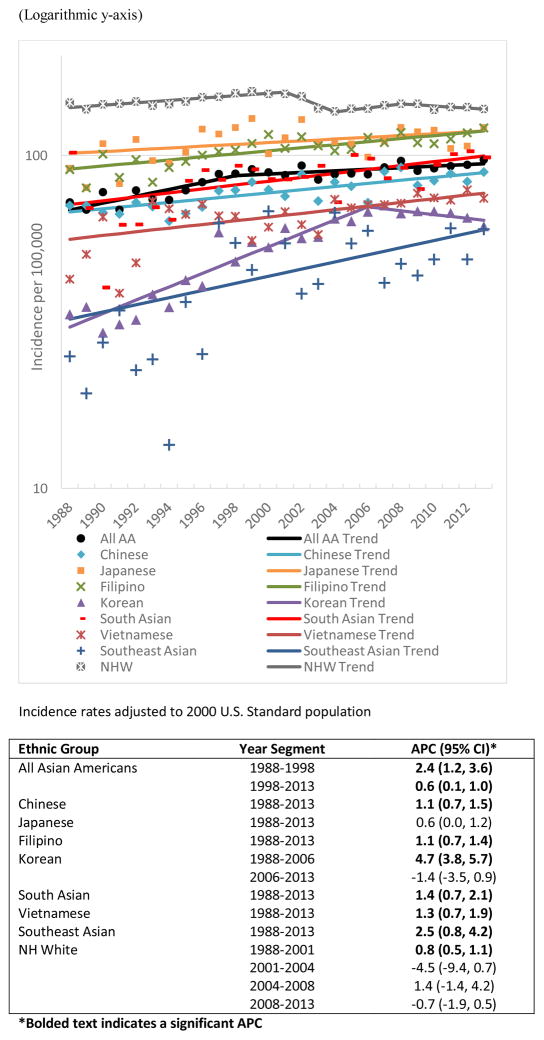
From 1988 through 2013, 548,259 new invasive breast cancer cases were diagnosed in California women, including 383,478 in NHW and 45,721 in AA. Compared to NHW women, AA women as a group experienced a larger incidence rate increase in breast cancer (APC: 2.4, 95% CI: 1.2, 3.6 from 1988–1998, compared to 0.8 (0.5–1.1) from 1988–2001 among NHW) (Figure 1). Whereas rates for NHW women fluctuated between 1998 and 2013, rates for AA women increased modestly (APC: 0.6, 95% CI: 0.1, 1.0). Breast cancer incidence increased significantly in all AA ethnicities except Japanese over the 26-year period. The largest increases occurred among Koreans from 1988 through 2006 (APC: 4.7, 95% CI: 3.8, 5.7) and Southeast Asians from 1988 through 2013 (APC: 2.5, 95% CI: 0.8, 4.2). From 1988 through 2013, small incidence increases were noted for Chinese (APC: 1.1, 95% CI: 0.7, 1.5), Filipinas (APC: 1.1, 95% CI: 0.7, 1.4), South Asians (APC: 1.4, 95% CI: 0.7, 2.1), and Vietnamese (APC: 1.3, 95% CI: 0.7, 1.9).
Figure 1.
Incidence rates over time of invasive breast cancer among Asian American ethnic groups and non-Hispanic Whites, 1988–2013, California.
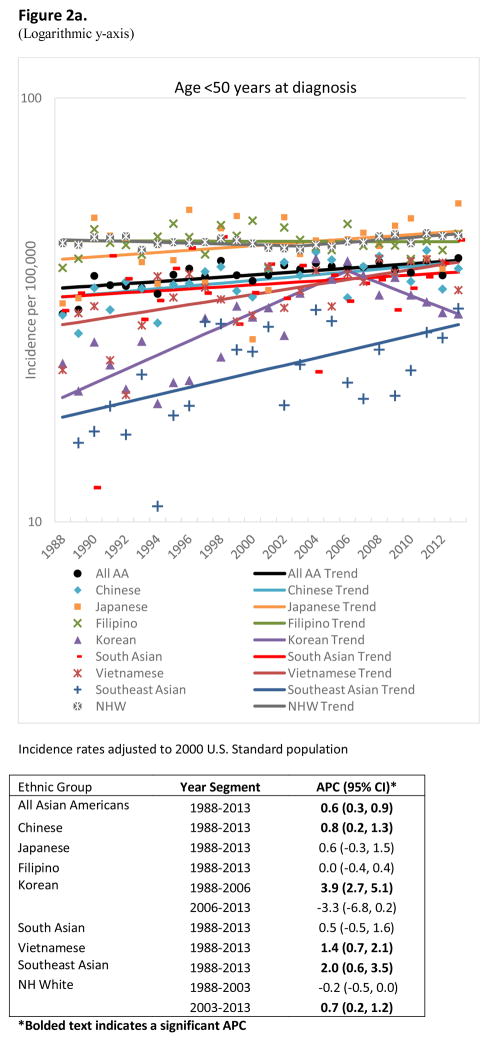
Among younger (<50 years) AA women (Figure 2a), incidence increases occurred over time for all groups except Japanese, Filipinas, and South Asians. For younger women, increases in incidence were observed among Koreans from 1988 through 2006 (APC: 3.9, 95% CI: 2.7, 5.1), Vietnamese from 1988 through 2013 (APC: 1.4, 95% CI: 0.7, 2.1), and Southeast Asians from 1988 through 2013 (APC: 2.0, 95% CI: 0.6, 3.5).
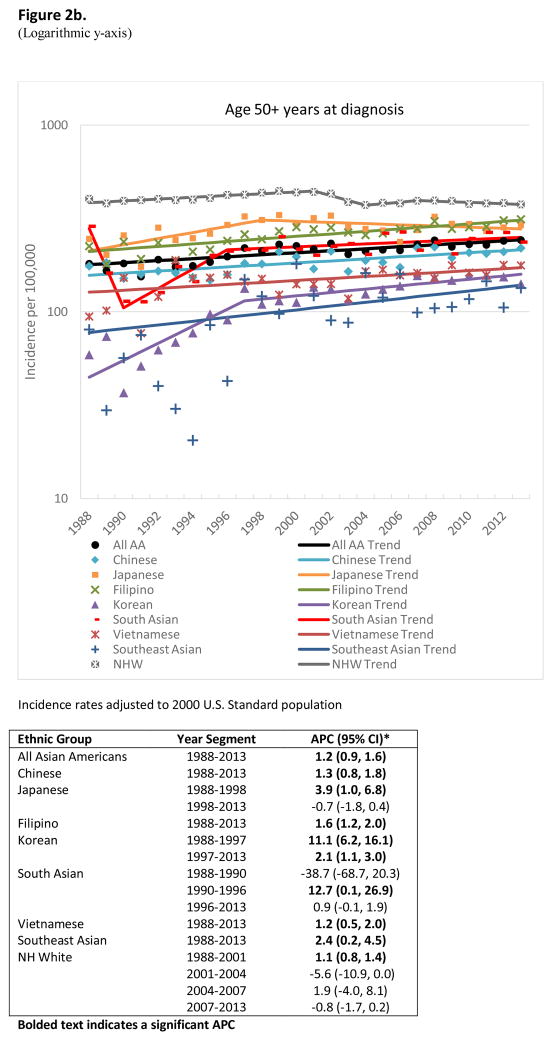
Figure 2.
Incidence rates over time of invasive breast cancer among Asian American ethnic groups and non-Hispanic Whites, 1988–2013, California
a. ages <50 years
b. ages 50+ years
Among older women (Figure 2b), rates increased across all AA ethnic groups, notably among Japanese in 1988 through 1998 (APC: 3.9, 95% CI: 1.0, 6.8), Koreans in 1988 through 1997 (APC: 11.1, 95% CI: 6.2, 16.1) and South Asians in 1990 through 1996 (APC: 12.7, 95% CI: 0.1, 26.9). Incidence rates among older Japanese and NHW women were generally stable in more recent years.
Considering stage at diagnosis, incidence increases occurred among AA combined primarily for localized (APC: 1.4, 95% CI: 0.8, 1.9) and distant stage (APC: 1.4, 95% CI: 0.1, 2.8) disease; rates were stable for regional stage, and decreased for unstaged tumors (APC: −4.7, 95% CI: −6.4, −2.9) (Table 1). Localized stage increases from 1988–1990 through 2012–2013 occurred annually (APC) among Chinese (1.6%), Japanese (3.2% for 1998–1990 through 1997–1999), Filipinas (1.4%), South Asians (1.9%), Vietnamese (2.1%), and Southeast Asians (3.1%). For regional stage disease, annual increases occurred among Koreans (5.8% for 1988–1990 to 2003–2005) and South Asians (0.6%). Distant stage increases were significant among Filipinas (2.2%) and non-significant for Koreans and South Asians (4.1% and 2.6%, respectively).
Table 1.
Invasive breast cancer incidence rates and annual percent change (APC) by stage for Non-Hispanic Whites (NHW) and Asian American (AA) ethnic group, 1988–2013, California
| Stage | Ethnic Group | Years* | APC (95% CI) | 2009–2013 Incidence Rate (per 100,000) |
|---|---|---|---|---|
| Localized | Non-Hispanic White | 1988–1990 to 2012–2013 | 0.1 (−0.5, 0.6) | 91.4 (90.6, 92.2) |
| All Asian Americans | 1988–1990 to 2012–2013 | 1.4 (0.8, 1.9) | 60.6 (59.4, 61.9) | |
| Chinese | 1988–1990 to 2012–2013 | 1.6 (1.0, 2.2) | 57.3 (55.1, 59.7) | |
| Japanese | 1988–1990 to 1997–1999 | 3.2 (0.3, 6.3) | 78.7 (73.9, 83.9) | |
| 1997–1999 to 2012–2013 | −0.1 (−1.2, 1) | |||
| Filipino | 1988–1990 to 2012–2013 | 1.4 (0.9, 1.9) | 72.1 (69.5, 74.7) | |
| Korean | 1988–1990 to 2006–2008 | 4.9 (2.5, 7.3) | 41 (37.8, 44.5) | |
| 2006–2008 to 2012–2013 | −2.1 (−13.7, 11.1) | |||
| South Asian | 1988–1990 to 2012–2013 | 1.9 (0.7, 3.2) | 57.4 (53, 62) | |
| Vietnamese | 1988–1990 to 2012–2013 | 2.1 (1.4, 2.9) | 50.2 (46.8, 53.8) | |
| Southeast Asian | 1988–1990 to 2012–2013 | 3.1 (0.3, 5.9) | 32.5 (28.1, 37.3) | |
| Regional | Non-Hispanic White | 1988–1990 to 2012–2013 | −0.3 (−1, 0.3) | 39.4 (38.8, 40) |
| All Asian Americans | 1988–1990 to 2000–2002 | 2.3 (0, 4.7) | 27.4 (26.5, 28.2) | |
| 2000–2002 to 2012–2013 | −0.5 (−2.2, 1.4) | |||
| Chinese | 1988–1990 to 2012–2013 | 0.6 (−0.4, 1.5) | 24 (22.6, 25.6) | |
| Japanese | 1988–1990 to 2012–2013 | 0.3 (−0.8, 1.4) | 30.1 (27, 33.4) | |
| Filipino | 1988–1990 to 2012–2013 | 0.8 (−0.1, 1.8) | 34.7 (32.9, 36.5) | |
| Korean | 1988–1990 to 2003–2005 | 5.8 (2.4, 9.3) | 19.8 (17.6, 22.3) | |
| 2003–2005 to 2012–2013 | −1.4 (−6.7, 4.2) | |||
| South Asian | 1988–1990 to 2012–2013 | 0.6 (0.1, 1.1) | 32 (28.8, 35.4) | |
| Vietnamese | 1988–1990 to 2012–2013 | 0.4 (−1, 1.8) | 21.4 (19.3, 23.8) | |
| Southeast Asian | 1988–1990 to 2012–2013 | 2.4 (−0.1, 4.9) | 16.5 (13.3, 20.2) | |
| Distant | Non-Hispanic White | 1988–1990 to 2000–2002 | −1.3 (−2.3, −0.4) | 6.9 (6.7, 7.2) |
| 2000–2002 to 2012–2013 | 2.4 (1.3, 3.6) | |||
| All Asian Americans | 1988–1990 to 2012–2013 | 1.4 (0.1, 2.8) | 4.1 (3.8, 4.4) | |
| Chinese | 1988–1990 to 2012–2013 | −0.1 (−2, 1.9) | 3 (2.5, 3.6) | |
| Japanese | 1988–1990 to 2012–2013 | 1.3 (−1.4, 4.1) | 4.1 (3, 5.4) | |
| Filipino | 1988–1990 to 2012–2013 | 2.2 (0.4, 3.9) | 5.7 (5, 6.4) | |
| Korean | 1988–1990 to 2012–2013 | 4.1 (−1.3, 9.9) | 3.3 (2.5, 4.4) | |
| South Asian | 1988–1990 to 2012–2013 | 2.6 (−0.8, 6.1) | 5.2 (4, 6.8) | |
| Vietnamese | 1988–1990 to 2012–2013 | 0.1 (−1.6, 1.9) | 3.2 (2.4, 4.2) | |
| Southeast Asian | 1988–1990 to 2012–2013 | 1.9 (−4.4, 8.6) | 2.8 (1.6, 4.5) | |
| Unstaged | Non-Hispanic White | 1988–1990 to 2012–2013 | −4.9 (−6.0, −3.9) | 2.0 (1.9, 2.1) |
| All Asian Americans | 1988–1990 to 2012–2013 | −4.7 (−6.4, −2.9) | 1.2 (1.1, 1.4) | |
| Chinese | 1988–1990 to 2012–2013 | −5.1 (−7.4, −2.7) | 1.1 (0.8, 1.5) | |
| Japanese | 1988–1990 to 2012–2013 | −4.2 (−7.0, −1.4) | 1.3 (0.7, 2.1) | |
| Filipino | 1988–1990 to 2012–2013 | −5.5 (−8.8, −2.2) | 1.5 (1.2, 1.9) | |
| Korean | 1988–1990 to 2012–2013 | −2.3 (−6.3, 1.8) | 1.7 (1.1, 2.5) | |
| South Asian | 1988–1990 to 2012–2013 | −3.3 (−7.6, 1.3) | 1.1 (0.6, 1.8) | |
| Vietnamese | 1988–1990 to 2012–2013 | −3.2 (−8.3, 2.2) | 0.9 (0.5, 1.6) | |
| Southeast Asian | 1988–1990 to 2012–2013 | −0.8 (−8.3, 7.3) | 0.8 (0.3, 1.9) |
Bolded text indicates a significant APC.
Three-year cumulative incidence rates were used to calculate APC, except for 2012–2013.
Incidence rate ratios (relative to NHW) by age and subtype, 2009 through 2013
During the time period 2009–2013, overall incidence rates were statistically significantly lower among AA women than NHW women. The only exception was observed among younger Japanese and Filipino women, who had rates very similar to those of similarly aged NHW (Japanese IRR: 1.02, 95% CI: 0.91, 1.14; Filipino IRR: 0.95, 95% CI: 0.90, 1.01) (Table 2).
Table 2.
Incidence rates and incidence rate ratios (IRR) of invasive breast cancer for Asian American ethnic groups compared to non-Hispanic Whites, by age and subtype, 2009–2013, California
| All Ages | Age <50 years | Age 50+ years | |||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| N cases | Rate (95% CI) | IRR (95% CI) | Rate (95% CI) | IRR (95% CI) | Rate (95% CI) | IRR (95% CI) | |
| All | |||||||
|
| |||||||
| NH White | 75,670 | 139.76 (138.72,140.80) | ref | 47.15 (46.29,48.02) | ref | 382.25 (379.24,385.27) | ref |
| Chinese | 3,716 | 85.46 (82.69, 88.28) | 0.61 (0.59, 0.63) | 38.75 (36.48, 41.14) | 0.82 (0.77, 0.87) | 207.75 (199.76, 215.98) | 0.54 (0.52, 0.57) |
| Japanese | 1,525 | 114.12 (108.20, 120.31) | 0.82 (0.78, 0.86) | 48.01 (42.95, 53.54) | 1.02 (0.91, 1.14) | 287.26 (270.58, 304.67) | 0.75 (0.71, 0.80) |
| Filipino | 4,905 | 113.92 (110.70, 117.22) | 0.82 (0.79, 0.84) | 44.87 (42.34,47.52) | 0.95 (0.90,1.01) | 294.74 (285.18,304.55) | 0.77 (0.75, 0.80) |
| Korean | 975 | 65.90 (61.80, 70.22) | 0.47 (0.44, 0.50) | 33.37 (29.90, 37.15) | 0.71 (0.64, 0.79) | 151.10 (139.47, 163.48) | 0.4 (0.37, 0.43) |
| South Asian | 1,201 | 95.71 (90.09, 101.58) | 0.68 (0.65, 0.72) | 38.73 (35.11, 42.61) | 0.82 (0.75, 0.90) | 244.91 (227.04, 263.88) | 0.64 (0.60, 0.69) |
| Vietnamese | 1,295 | 75.76 (71.60, 80.10) | 0.54 (0.51, 0.57) | 39.48 (36.03, 43.18) | 0.84 (0.76, 0.92) | 170.74 (158.83, 183.36) | 0.45 (0.42, 0.48) |
| Southeast Asian | 345 | 52.59 (46.91,58.76) | 0.38 (0.34,0.42) | 26.04 (21.62,31.05) | 0.55 (0.46,0.66) | 122.11 (105.40,140.88) | 0.32 (0.28, 0.36) |
| All Asian Americans | 13,962 | 93.29 (91.73, 94.87) | 0.67 (0.66, 0.68) | 39.94 (38.70, 41.20) | 0.85 (0.82, 0.88) | 233.01 (228.40, 237.69) | 0.61 (0.60, 0.62) |
|
| |||||||
| HR+/HER2− | |||||||
|
| |||||||
| NH White | 52,012 | 95.09 (94.25, 95.95) | ref | 28.88 (28.21, 29.56) | ref | 268.49 (265.97, 271.02) | ref |
| Chinese | 2,379 | 55.07 (52.84, 57.36) | 0.58 (0.56, 0.60) | 24.48 (22.68, 26.39) | 0.85 (0.78, 0.92) | 135.17 (128.7, 141.88) | 0.50 (0.48, 0.53) |
| Japanese | 1,066 | 80.20 (75.24, 85.42) | 0.84 (0.79, 0.90) | 34.19 (29.96, 38.90) | 1.18 (1.04, 1.35) | 200.69 (186.75, 215.37) | 0.75 (0.70, 0.80) |
| Filipino | 3,052 | 70.80 (68.27, 73.42) | 0.74 (0.72, 0.77) | 25.88 (23.97, 27.91) | 0.90 (0.83, 0.97) | 188.44 (180.79, 196.34) | 0.70 (0.67, 0.73) |
| Korean | 570 | 38.56 (35.44, 41.91) | 0.41 (0.37, 0.44) | 19.73 (17.08, 22.7) | 0.68 (0.59, 0.79) | 87.89 (79.07, 97.43) | 0.33 (0.30, 0.36) |
| South Asian | 758 | 62.35 (57.76, 67.2) | 0.66 (0.61, 0.70) | 23.22 (20.41, 26.29) | 0.80 (0.71, 0.91) | 164.81 (150.03, 180.7) | 0.61 (0.56, 0.67) |
| Vietnamese | 741 | 43.54 (40.4, 46.88) | 0.46 (0.43, 0.49) | 21.39 (18.87, 24.16) | 0.74 (0.65, 0.84) | 101.55 (92.37, 111.44) | 0.38 (0.35, 0.41) |
| Southeast Asian | 183 | 29.34 (25.00, 34.19) | 0.31 (0.27, 0.36) | 13.41 (10.3, 17.11) | 0.46 (0.36, 0.59) | 71.03 (57.88, 86.37) | 0.26 (0.22, 0.32) |
| All Asian Americans | 8,749 | 58.71 (57.47, 59.96) | 0.62 (0.6, 0.63) | 23.97 (23.02, 24.96) | 0.83 (0.79, 0.87) | 149.66 (145.96, 153.44) | 0.56 (0.54, 0.57) |
|
| |||||||
| HR-/HER2+ | |||||||
|
| |||||||
| NH White | 2,563 | 4.94 (4.74, 5.14) | ref | 2.1 (1.92, 2.29) | ref | 12.37 (11.83, 12.92) | ref |
| Chinese | 245 | 5.46 (4.79, 6.21) | 1.11 (0.97, 1.26) | 2.45 (1.90, 3.12) | 1.17 (0.91, 1.5) | 13.35 (11.42, 15.51) | 1.08 (0.93, 1.26) |
| Japanese | 57 | 3.95 (2.94, 5.24) | 0.8 (0.62, 1.04) | 1.07 (0.43, 2.27) | 0.51 (0.24, 1.07) | 11.51 (8.43, 15.33) | 0.93 (0.70, 1.23) |
| Filipino | 343 | 7.76 (6.95, 8.65) | 1.57 (1.40, 1.76) | 3.75 (3.04, 4.57) | 1.79 (1.44, 2.22) | 18.28 (16.03, 20.76) | 1.48 (1.29, 1.69) |
| Korean | 61 | 4.08 (3.11, 5.27) | 0.83 (0.64, 1.06) | 1.79 (1.06, 2.86) | 0.85 (0.53, 1.36) | 10.08 (7.26, 13.65) | 0.81 (0.60, 1.10) |
| South Asian | 59 | 4.40 (3.31, 5.74) | 0.89 (0.69, 1.15) | 1.87 (1.16, 2.85) | 0.89 (0.58, 1.36) | 11.03 (7.65, 15.51) | 0.89 (0.64, 1.23) |
| Vietnamese | 122 | 6.82 (5.65, 8.18) | 1.38 (1.15, 1.66) | 2.85 (1.98, 3.98) | 1.36 (0.96, 1.91) | 17.22 (13.72, 21.41) | 1.39 (1.12, 1.73) |
| Southeast Asian | 33 | 4.55 (3.11, 6.46) | 0.92 (0.65, 1.30) | 1.93 (0.88, 3.59) | 0.92 (0.48, 1.78) | 11.40 (7.22, 17.58) | 0.92 (0.62, 1.38) |
| All Asian Americans | 920 | 5.97 (5.58, 6.37) | 1.21 (1.12, 1.30) | 2.59 (2.29, 2.93) | 1.23 (1.06, 1.43) | 14.79 (13.68, 15.98) | 1.20 (1.10, 1.31) |
|
| |||||||
| HR+/HER2+ | |||||||
|
| |||||||
| NH White | 6,279 | 12.37 (12.05, 12.69) | ref | 6.14 (5.83, 6.46) | ref | 28.66 (27.84, 29.50) | ref |
| Chinese | 369 | 8.41 (7.56, 9.33) | 0.68 (0.61, 0.76) | 4.59 (3.83, 5.48) | 0.75 (0.62, 0.90) | 18.4 (16.12, 20.92) | 0.64 (0.56, 0.73) |
| Japanese | 114 | 9.26 (7.57, 11.23) | 0.75 (0.62, 0.9) | 5.81 (4.14, 7.99) | 0.95 (0.69, 1.30) | 18.27 (14.22, 23.08) | 0.64 (0.51, 0.80) |
| Filipino | 610 | 14.18 (13.06, 15.38) | 1.15 (1.05, 1.25) | 7.36 (6.36, 8.49) | 1.20 (1.03, 1.39) | 32.03 (28.99, 35.31) | 1.12 (1.01, 1.24) |
| Korean | 110 | 7.36 (6.04, 8.89) | 0.59 (0.49, 0.72) | 3.74 (2.64, 5.16) | 0.61 (0.44, 0.84) | 16.83 (13.13, 21.28) | 0.59 (0.47, 0.74) |
| South Asian | 141 | 10.80 (9.01, 12.84) | 0.87 (0.74, 1.03) | 5.38 (4.09, 6.93) | 0.88 (0.68, 1.13) | 25.01 (19.6, 31.53) | 0.87 (0.70, 1.09) |
| Vietnamese | 139 | 7.79 (6.54, 9.23) | 0.63 (0.53, 0.75) | 5.46 (4.23, 6.95) | 0.89 (0.70, 1.14) | 13.9 (10.83, 17.65) | 0.48 (0.38, 0.61) |
| Southeast Asian | 54 | 7.86 (5.84, 10.38) | 0.64 (0.49, 0.83) | 4.22 (2.57, 6.47) | 0.69 (0.44, 1.07) | 17.41 (11.77, 25.12) | 0.61 (0.43, 0.85) |
| All Asian Americans | 1,537 | 10.14 (9.63, 10.67) | 0.82 (0.78, 0.87) | 5.47 (5.02, 5.95) | 0.89 (0.81, 0.98) | 22.36 (20.97, 23.82) | 0.78 (0.73, 0.84) |
|
| |||||||
| Triple negative breast cancer | |||||||
|
| |||||||
| NH White | 6,789 | 13.17 (12.84, 13.51) | ref | 6.02 (5.71, 6.34) | ref | 31.89 (31.03, 32.77) | Ref |
| Chinese | 317 | 7.33 (6.53, 8.20) | 0.56 (0.50, 0.62) | 3.27 (2.63, 4.03) | 0.54 (0.44, 0.67) | 17.95 (15.66, 20.49) | 0.56 (0.49, 0.64) |
| Japanese | 143 | 10.32 (8.61, 12.30) | 0.78 (0.66, 0.92) | 3.60 (2.30, 5.41) | 0.60 (0.40, 0.90) | 27.95 (22.95, 33.68) | 0.88 (0.73, 1.05) |
| Filipino | 354 | 8.46 (7.58, 9.40) | 0.64 (0.58, 0.71) | 3.69 (2.99, 4.51) | 0.61 (0.50, 0.75) | 20.93 (18.41, 23.71) | 0.66 (0.58, 0.74) |
| Korean | 106 | 7.21 (5.89, 8.75) | 0.55 (0.45, 0.66) | 4.04 (2.89, 5.51) | 0.67 (0.49, 0.92) | 15.53 (11.94, 19.88) | 0.49 (0.38, 0.62) |
| South Asian | 133 | 9.20 (7.64, 10.99) | 0.70 (0.59, 0.83) | 5.40 (4.15, 6.90) | 0.90 (0.70, 1.14) | 19.13 (14.67, 24.67) | 0.60 (0.47, 0.77) |
| Vietnamese | 110 | 6.45 (5.27, 7.81) | 0.49 (0.41, 0.59) | 3.16 (2.25, 4.33) | 0.52 (0.38, 0.72) | 15.05 (11.65, 19.17) | 0.47 (0.37, 0.60) |
| Southeast Asian | 37 | 5.17 (3.59, 7.23) | 0.39 (0.28, 0.54) | 2.98 (1.62, 4.93) | 0.50 (0.29,0.84) | 10.93 (6.74, 17.15) | 0.34 (0.23, 0.52) |
| All Asian Americans | 1,200 | 8.06 (7.61, 8.54) | 0.61 (0.58, 0.65) | 3.73 (3.36, 4.13) | 0.62 (0.55, 0.69) | 19.41 (18.09, 20.80) | 0.61 (0.57, 0.65) |
Incidence rates age adjusted to the 2000 U.S. Standard
Among all women, the most common breast cancer subtype was HR+/HER2− (Table 2). Incidence rates of HR+/HER2− were significantly lower for all AA groups than for NHW women; the exception was for young Japanese women (IRR: 1.18, 95% CI: 1.04, 1.35). For all racial/ethnic groups, the lowest rates occurred for the HR−/HER2+ subtype; nevertheless, rates were 20% higher in AA than NHW women (IRR for all ages: 1.21, 95% CI: 1.12, 1.30). Among younger women, Filipinas had the highest incidence of HR−/HER2+, with rates significantly higher than NHW women (IRR: 1.79, 95% CI: 1.44, 2.22). Among older women, HR−/HER2+ rates were significantly higher among Filipinas (IRR: 1.48, 95% CI: 1.29, 1.69) and Vietnamese (IRR: 1.39, 95% CI: 1.12, 1.73) than NHW.
For the HR+/HER2+ subtype, incidence rates were significantly lower in all AA ethnic groups than in NHW women, except for Filipinas, whose rate was significantly higher (IRR: 1.15, 95% CI: 1.05, 1.25).
For TNBC, the rate among AA ethnicities combined was significantly lower than NHW women (IRR: 0.61, 95% CI: 0.58, 0.65). However, young South Asian women and older Japanese women had rates similar to those in NHW women.
DISCUSSION
This report provides new insights into the epidemiology of breast cancer among the most prominent AA ethnic groups in California. Using 26 years of surveillance data, we found that breast cancer incidence has risen rapidly among AA women, in contrast to declines reported in California and nationwide (1) among NHW. Rates increased across all seven AA ethnic subgroups, particularly among Koreans and Southeast Asians, the groups with the lowest absolute rates. Although breast cancer incidence rates in AA women combined were lower than rates for NHW, the rates for Japanese and Filipinas under age 50 were comparable to rates for similarly aged NHW women. We found particularly rapid rate increases among older Koreans and South Asian women during the 1990s, although these increases slowed in more recent years. While increases occurred for localized stage disease, the more substantial rate increases in distant stage, particularly among Filipino, Korean, and South Asian women, were concerning, albeit not statistically significant in the latter two groups.
Using US cancer registry data, DeSantis et al. reported a 1.5% annual increase in breast cancer incidence among Asian/Pacific Islander women as a combined group from 2008 through 2012 (1). This trend contrasts with stable or declining trends among other racial/ethnic groups, but is similar to increasing trends in South Korea, China, Taiwan, Japan, and Hong Kong. In age-period-cohort analyses, Sung et al. (11) and Wang et al. (19) found dramatically increasing trends of breast cancer incidence (11) and mortality (19) in recent cohorts in Asia, with incidence rates through 2009 surpassing those of US NHW women (11). These authors attributed increases to increasing prevalence among Asian women of established reproductive breast cancer risk factors.
Although prior research has examined subtype-specific incidence patterns among Asians/Pacific Islanders as an aggregate group, ours is the first examination of subtype-specific incidence patterns among AA ethnicities, unmasking the heterogeneity among AA ethnic groups. We found that AA women in California generally had lower rates of the HR+/HER2−, HR+/HER2+, and TNBC subtypes relative to NHW women; exceptions were the higher rates of HR+/HER2− cancer among younger Japanese women and of HR+/HER2+ cancers among Filipino women. In addition, Filipino and Vietnamese women had higher rates of HR−/HER2+ breast cancer than NHW women, and Chinese women had rates comparable to those of NHW women. These patterns are consistent with the higher proportional odds of HR−/HER2+ tumors relative to HR+/HER2− tumors among AA than NHW in this population (13, 20). Using SEER data from 2010 forward, Kohler et al. reported lower breast cancer rates in Asian/Pacific Islander women than NHW women, with the exception of higher HR−/HER2+ incidence in Asian/Pacific Islander women (21). Most studies have found that socioeconomic status, body mass index, and reproductive factors are related mainly to the HR+ cancers (12, 22–25), with less evidence of associations with the rarer subtypes, such as HR−/HER2+ cancers (12). However, in a recent examination of subtype differences and several reproductive factors in an ethnically diverse group of women with breast cancer, Chen et al. found that higher parity increased risk for HER2−overexpressing tumors (26).
Although California’s population comprises 32% of all US AA, our results may not be generalizable to AA populations in other geographic areas. Misclassification of ethnicity could bias our findings, although misclassification in AA ethnicity is fairly minimal in cancer registry data (27, 28), and surname- and nativity-based algorithms are routinely applied to classify cases that are “Asian, not otherwise specified” into specific AA ethnic groups. The proportion of cases with unknown subtype was relatively high, primarily due to unknown HER2 status; this could have resulted in under-estimation of subtype-specific rates. In addition, subtype classification based on immunohistochemical assays commonly used in pathology labs may differ from subtypes classified based on gene expression profiling (29, 30).
When breast cancer incidence was examined for women from specific AA ethnicities, several noteworthy patterns emerged. These included continuing increases in rates of breast cancer among women from all seven AA ethnic groups, with the largest increases for South Asians, Vietnamese, and Southeast Asians – the most recently immigrated groups; rates among Japanese and Filipino women under age 50 comparable to those in NHW women; increasing trends over time of distant stage disease, particularly among Filipino, Korean, and South Asian women; and higher rates of some types of HER2−overexpressing tumors among Filipino and Vietnamese women relative to NHW women. These patterns warrant additional attention to public health prioritization of disparities in access to care, as well as further research in identifying relevant breast cancer risk factors. In particular, studies should investigate risk factors, perhaps early-life exposures, underlying the higher rates of breast cancer among young Filipino and Japanese women, with attention to possible genetic susceptibility. Further, increasing trends of late stage disease suggest a need for higher rates of mammography screening in these populations. Mammography utilization rates in California are slightly lower in Asian American women than in NHW, NHBs and Hispanics (31), and among the AA ethnic groups, Korean and South Asian women have the lowest mammography utilization, consistent with their higher rates of distant stage disease (31, 32). The disproportionately high rates of some HER2-overexpressing subtypes also require better understanding, as this subtype tends to grow more quickly, spread more aggressively, and present more often as high-grade disease than the more common HR+/HER2- tumors (12). Further evaluation is needed to assure that these groups are properly treated with targeted trastuzumab treatment. As little is known regarding risk factors for these breast cancer subtypes, studies that include these ethnic groups and their potential unique exposures may provide insights into their etiology. This research highlights the value and insights gained from considering distinct AA ethnicities in breast cancer research. Future research should always aim to disaggregate AAs given their heterogeneous incidence patterns.
Acknowledgments
The collection of cancer incidence data used in this study was supported by the California Department of Public Health as part of the statewide cancer reporting program mandated by California Health and Safety Code Section 103885; the National Cancer Institute’s Surveillance, Epidemiology and End Results Program under contract HHSN261201000140C awarded to the Cancer Prevention Institute of California, contract HHSN261201000035C awarded to the University of Southern California, and contract HHSN261201000034C awarded to the Public Health Institute; and the Centers for Disease Control and Prevention’s National Program of Cancer Registries, under agreement U58DP003862-01 awarded to the California Department of Public Health. The ideas and opinions expressed herein are those of the author(s) and endorsement by the State of California, Department of Public Health the National Cancer Institute, and the Centers for Disease Control and Prevention or their Contractors and Subcontractors is not intended nor should be inferred.
Funding: This work was supported by the Stanford Cancer Institute (SL Gomez, SL Glaser) and the National Cancer Institute’s Surveillance, Epidemiology and End Results Program under contract HHSN261201000140C awarded to the Cancer Prevention Institute of California (PI: SL Glaser).
Abbreviations used
- AA
Asian American
- HR
hormone receptor
- HER2
HER2Neu
- NHW
non-Hispanic white
- NHB
non-Hispanic black
- CCR
California Cancer Registry
- SEER
Surveillance, Epidemiology, End Results
- APC
annual percentage change
- TNBC
triple-negative breast cancer
Footnotes
Conflicts of interest: None.
Author contributions: SL Gomez and SL Glaser conceived and oversaw the study. M McKinley conducted the data analysis. All authors contributed substantially to the analysis and interpretation of data, revisions of the manuscript, and approval of the final version.
References
- 1.DeSantis CE, Fedewa SA, Goding Sauer A, Kramer JL, Smith RA, Jemal A. Breast cancer statistics, 2015: Convergence of incidence rates between black and white women. CA Cancer J Clin. 2016;66(1):31–42. doi: 10.3322/caac.21320. [DOI] [PubMed] [Google Scholar]
- 2.Torre LA, Sauer AM, Chen MS, Jr, Kagawa-Singer M, Jemal A, Siegel RL. Cancer statistics for Asian Americans, Native Hawaiians, and Pacific Islanders, 2016: Converging incidence in males and females. CA Cancer J Clin. 2016;66(3):182–202. doi: 10.3322/caac.21335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tseng W, McDonnell D, Ho W, Lee C, Wong S. Ethnic Health Assessment for Asian Americans, Native Hawaiians and Pacific Islanders in California. 2010 [Google Scholar]
- 4.Asian Pacific American Legal Center of Southern California. The Diverse Face of Asians and Pacific Islanders in California: Asian & Pacific Islander Demographic Profile. 2005 [Google Scholar]
- 5.Frisbie WP, Cho Y, Hummer RA. Immigration and the health of Asian and Pacific Islander adults in the United States. Am J Epidemiol. 2001;153(4):372–80. doi: 10.1093/aje/153.4.372. [DOI] [PubMed] [Google Scholar]
- 6.Bateman WB, Abesamis NF, Ho-Asjoe H. Praeger Handbook of Asian American Health. 2009. [Google Scholar]
- 7.Gomez SL, Noone AM, Lichtensztajn DY, Scoppa S, Gibson JT, Liu L, et al. Cancer incidence trends among Asian American populations in the United States, 1990–2008. J Natl Cancer Inst. 2013;105(15):1096–110. doi: 10.1093/jnci/djt157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reynolds P, Hurley S, Goldberg D, Quach T, Rull R, Von Behren J. An excess of breast cancer among young California-born Asian women. Ethn Dis. 2011;21(2):196–201. [PubMed] [Google Scholar]
- 9.Gomez SL, Quach T, Horn-Ross PL, Pham JT, Cockburn M, Chang ET, et al. Hidden breast cancer disparities in Asian women: disaggregating incidence rates by ethnicity and migrant status. Am J Public Health. 2010;100(Suppl 1):S125–31. doi: 10.2105/AJPH.2009.163931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu L, Zhang J, Wu AH, Pike MC, Deapen D. Invasive breast cancer incidence trends by detailed race/ethnicity and age. Int J Cancer. 2012;130(2):395–404. doi: 10.1002/ijc.26004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sung H, Rosenberg PS, Chen WQ, Hartman M, Lim WY, Chia KS, et al. Female breast cancer incidence among Asian and Western populations: more similar than expected. J Natl Cancer Inst. 2015;107(7) doi: 10.1093/jnci/djv107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Anderson KN, Schwab RB, Martinez ME. Reproductive risk factors and breast cancer subtypes: a review of the literature. Breast Cancer Res Treat. 2014;144(1):1–10. doi: 10.1007/s10549-014-2852-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Telli ML, Chang ET, Kurian AW, Keegan TH, McClure LA, Lichtensztajn D, et al. Asian ethnicity and breast cancer subtypes: a study from the California Cancer Registry. Breast Cancer Res Treat. 2011;127(2):471–8. doi: 10.1007/s10549-010-1173-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hoeffel E, Rastogi S, Kim M, Shahid H. The Asian Population: 2010. 2010 Census Briefs. 2012 [Google Scholar]
- 15.Howlader N, Altekruse SF, Li CI, Chen VW, Clarke CA, Ries LA, et al. US incidence of breast cancer subtypes defined by joint hormone receptor and HER2 status. J Natl Cancer Inst. 2014;106(5) doi: 10.1093/jnci/dju055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Surveillance Research Program: National Cancer Institute. SEER*Stat software. ( seer.cancer.gov/seerstat)
- 17.Joinpoint Regression Program Version 3.5.1. Statistical Research and Applications Branch of the National Cancer Institute; Jul, 2011. [Google Scholar]
- 18.Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19(3):335–51. doi: 10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 19.Wang Z, Bao J, Yu C, Wang J, Li C. Secular Trends of Breast Cancer in China, South Korea, Japan and the United States: Application of the Age-Period-Cohort Analysis. Int J Environ Res Public Health. 2015;12(12):15409–18. doi: 10.3390/ijerph121214993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Parise C, Caggiano V. Disparities in the risk of the ER/PR/HER2 breast cancer subtypes among Asian Americans in California. Cancer Epidemiol. 2014;38(5):556–62. doi: 10.1016/j.canep.2014.08.001. [DOI] [PubMed] [Google Scholar]
- 21.Kohler BA, Sherman RL, Howlader N, Jemal A, Ryerson AB, Henry KA, et al. Annual Report to the Nation on the Status of Cancer, 1975–2011, Featuring Incidence of Breast Cancer Subtypes by Race/Ethnicity, Poverty, and State. J Natl Cancer Inst. 2015;107(6):djv048. doi: 10.1093/jnci/djv048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Althuis MD, Fergenbaum JH, Garcia-Closas M, Brinton LA, Madigan MP, Sherman ME. Etiology of hormone receptor-defined breast cancer: a systematic review of the literature. Cancer Epidemiol Biomarkers Prev. 2004;13(10):1558–68. [PubMed] [Google Scholar]
- 23.Yang XR, Chang-Claude J, Goode EL, Couch FJ, Nevanlinna H, Milne RL, et al. Associations of breast cancer risk factors with tumor subtypes: a pooled analysis from the Breast Cancer Association Consortium studies. J Natl Cancer Inst. 2011;103(3):250–63. doi: 10.1093/jnci/djq526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Akinyemiju TF, Pisu M, Waterbor JW, Altekruse SF. Socioeconomic status and incidence of breast cancer by hormone receptor subtype. Springerplus. 2015;4:508. doi: 10.1186/s40064-015-1282-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sisti JS, Collins LC, Beck AH, Tamimi RM, Rosner BA, Eliassen AH. Reproductive risk factors in relation to molecular subtypes of breast cancer: Results from the nurses' health studies. Int J Cancer. 2016;138(10):2346–56. doi: 10.1002/ijc.29968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen L, Li CI, Tang MT, Porter P, Hill DA, Wiggins CL, et al. Reproductive Factors and Risk of Luminal, HER2-Overexpressing, and Triple-Negative Breast Cancer Among Multiethnic Women. Cancer Epidemiol Biomarkers Prev. 2016;25(9):1297–304. doi: 10.1158/1055-9965.EPI-15-1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gomez SL, Glaser SL. Misclassification of race/ethnicity in a population-based cancer registry (United States) Cancer Causes Control. 2006;17(6):771–81. doi: 10.1007/s10552-006-0013-y. [DOI] [PubMed] [Google Scholar]
- 28.Clegg LX, Reichman ME, Hankey BF, Miller BA, Lin YD, Johnson NJ, et al. Quality of race, Hispanic ethnicity, and immigrant status in population-based cancer registry data: implications for health disparity studies. Cancer Causes Control. 2007;18(2):177–87. doi: 10.1007/s10552-006-0089-4. [DOI] [PubMed] [Google Scholar]
- 29.Cancer Genome Atlas N. Comprehensive molecular portraits of human breast tumours. Nature. 2012;490(7418):61–70. doi: 10.1038/nature11412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Parker JS, Mullins M, Cheang MC, Leung S, Voduc D, Vickery T, et al. Supervised risk predictor of breast cancer based on intrinsic subtypes. J Clin Oncol. 2009;27(8):1160–7. doi: 10.1200/JCO.2008.18.1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.California Health Interview Survey (CHIS) Health Policy Fact Sheet: Asians Below State Average for Timely Mammograms. UCLA Center for Health Policy Research; Apr, 2014. [Google Scholar]
- 32.Chawla N, Breen N, Liu B, Lee R, Kagawa-Singer M. Asian American women in California: a pooled analysis of predictors for breast and cervical cancer screening. Am J Public Health. 2015;105(2):e98–e109. doi: 10.2105/AJPH.2014.302250. [DOI] [PMC free article] [PubMed] [Google Scholar]