Abstract
Background
The 30-day readmission rate is an indicator of the quality of hospital care and transition to the outpatient setting. Recent studies suggest HIV infection might increase the risk of readmission though estimates of 30-day readmission rates are unavailable among HIV infected individuals living in middle/low income settings. Additionally, factors that may increase readmission risk in HIV infected populations are poorly understood.
Methods
30-day readmission rates were estimated for HIV-infected adults from the Instituto Nacional de Infectologia Evandro Chagas/Fiocruz cohort in Rio de Janeiro, Brazil, from January 2007 to December 2013. Cox regression models were used to evaluate factors associated with the risk of 30-day readmission.
Results
Between January 2007 and December 2013, 3991 patients were followed and 1861 hospitalizations were observed. The estimated 30-day readmission rate was 14% (95% confidence interval 12.3%–15.9%). Attending a medical visit within 30 days after discharge (aHR 0.73, p=0.048) and being hospitalized in more recent calendar years (aHR 0.89, p=0.002) reduced the risk of 30-day readmission. In contrast, low CD4 counts (51–200 cells/mm3: aHR 1.70, p=0.024 and ≤ 50 cells/mm3: aHR 2.05, p=0.003), time since HIV infection diagnosis ≥10 years (aHR 1.58, p=0.058) and leaving hospital against medical advice (aHR 2.67, p=0.004) increased the risk of 30-day readmission.
Conclusions
Patients with advanced HIV/AIDS are most at risk of readmission and should be targeted with prevention strategies to reduce this risk. Efforts to reduce discharge against medical advice and to promote early post-discharge medical visit would likely reduce 30-day readmission rates in our population.
Keywords: HIV, hospitalization, readmission, healthcare utilization, length of stay, antiretroviral therapy
Introduction
Hospital readmission within 30 days of discharge, i.e. 30-day readmission, has been increasingly proposed as an indicator of the quality of hospital care and of transition care to the outpatient setting1. In Brazil, since 2015 the National Agency for Supplementary Health also incorporated 30-day readmission as an indicator of health care assistance quality2. Between hospitals comparisons, adjusted for patients’ characteristics and for the community within which a hospital is located3, can help identify institutions with worse performance allowing for adoption/reviewing of clinical protocols to improve hospital care4. Economically, readmissions are expensive and consume a great share of health designated expenditures5. Altogether, studies have suggested that the keeping of 30-day readmission rates within the expected average values can result in a win-win scenario: improvement in hospital quality and efficiency allowing for better allocation of health expenditures.
In the United States, all-cause 30-day readmission rates in the general population is estimated at 14%6. Additionally, of the overall 30-day readmissions, 30% are thought to be potentially preventable events7. Several chronic medical conditions have been associated with high 30-day readmission rates with HIV being recently included among these conditions8–10. A recent study conducted in the United States showed a 1.5-fold increase in the risk of readmission for HIV infected patients compared to their non-HIV infected counterparts10. Moreover, among HIV infected patients, the proportion of potentially preventable readmissions is suggested to be even higher, reaching 53%11.
The study of 30-day readmission rates and its predictors among HIV infected patients can provide relevant information to guide monitoring of hospital quality and transition of care with the goal of reducing morbidity of the HIV infected population. To the best of our knowledge, studies addressing 30-day readmission rates and its determinants in HIV infected populations are restricted to high-income settings10–17 and the findings likely do not reflect low- to middle-income settings due to dissimilarities in infectious diseases burden as well as differences in the provision and structure of health care. In this study, we sought to 1) estimate 30-day readmissions rates among HIV patients living in a middle-income setting and 2) identify patient- and health care-level factors that were associated with higher risk of 30-day readmission among HIV infected patients from a cohort in Rio de Janeiro, Brazil, during the period of 2007–2013.
Methods
Study site and population
Since 1986, Instituto Nacional de Infectologia Evandro Chagas of Fundacao Oswaldo Cruz (INI/FIOCRUZ) has been a national referral center for infectious diseases care, research and training, being one of the largest providers of primary, specialty, and tertiary care for HIV infected individuals in Rio de Janeiro State. INI comprises an Infectious Disease tertiary hospital, Evandro Chagas Hospital, a day clinic (for chemotherapy and other parenteral drugs administration), an outpatient clinic and an emergency department, all funded by the Brazilian national health system (known as Sistema Único de Saúde). All HIV infected patients followed in the INI cohort have free-of-charge access to INI’s facilities as well as to antiretroviral treatment and other medications (such as opportunistic infections prophylaxis, Kaposi sarcoma chemotherapy, and diabetes, hypertension medications, etc.) provided by the Brazilian national health system. A longitudinal, periodically updated, observational clinical database has been maintained on patients receiving HIV care at INI. The database includes socio-demographic, laboratory, clinical, and therapeutic information abstracted from the medical records by trained staff. Additionally, dates of admission and discharge to Evandro Chagas Hospital are also included in the database along with discharge diagnoses and summary. Cohort procedures have been described and results published18–20.
For the present study, the study population included adult (≥18 years of age at cohort enrollment) HIV infected patients, enrolled in the INI cohort between 01 January 1985 and 01 December 2013, who were alive after 01 January 2007 and in active care (at least one medical visit after 01 January 2007) from 1997 to 2013.
Outcome definition
Index hospitalizations were defined as: 1) the first hospitalization in the study period or any hospitalization occurring >30 days after the most recent previous hospitalization, and 2) for which there was a live discharge. Hospitalizations occurring from 01 January 2007 (or from date of cohort enrollment for those enrolled after this date) until 31 December 2013 were considered. Patients were not censored after a hospitalization such that all hospitalization events during the years 2007–2013 were included. The only exceptions were the exclusion of hospitalizations (1) with admission date prior to 01 February 2007 because of the need to observe 30 days before a potential index hospitalization, and (2) with discharge date after 30 November 2013 because of the need to observed 30 days after a discharge for potential 30-day readmissions. Hospital readmissions occurring within 30 days of an index hospitalization discharge were defined as 30-day readmissions. When a “chain” of multiple readmissions with less than 30-day intervals each followed an index hospitalization, all readmissions in the chain were excluded from being an index hospitalization. 30-day readmission rate was calculated by dividing the number of 30-day readmissions by the number of index hospitalizations.
Independent variables
Socio-demographic and clinical variables were evaluated for association with 30-day readmission risk. CD4 count and HIV viral load closest to index hospitalization were selected on a timeframe of 180 days before and 30 days after the hospital admission date. Antiretroviral therapy (ART) use prior to index hospitalization was defined as a dichotomous yes/no variable based on ART initiation any time before index hospitalization admission. Since we do not have information on adherence, after ART first prescription, participants were defined as on ART. Time since HIV infection diagnosis was calculated as the difference between date of index hospitalization admission and date of the first positive HIV test. Type of hospitalization discharge was based on discharge reports and categorized as follows: according to medical advice, against medical advice, transfer to another hospital facility and unknown. Length of stay (LOS) was calculated by subtracting hospital admission date from date of discharge and adding 1. Use of intensive care unit (ICU) (yes/no) was used as a proxy for the severity of the patient’s clinical condition. Early transition from hospital to outpatient care was evaluated through the presence of a medical visit within 30-days of index hospitalization discharge or before readmission for those readmitted within 30-days.
Hospitalization discharge reports were reviewed and all the diagnoses listed in the discharge report were classified using the 10th Edition of the International Classification of Disease (ICD-10), into 24 different categories19. Since some ICD-10 codes could be allocated to several categories, we considered a hierarchical classification scheme with a decreasing order of priority as follows: AIDS-events, non-AIDS malignancies, infections and then systemic events19. Subsequently, to determine the primary cause of a hospitalization, the one or more ICD-10 codes listed in the discharge reports were hierarchically classified as follows: AIDS-defining diseases, non-AIDS malignancies, cardiovascular disease, bacterial infections, fungal infections, viral infections, parasitic infection, digestive diseases, renal diseases, respiratory diseases, neurologic diseases, endocrine diseases, hematological diseases, psychiatric diseases, viral hepatitis, non-viral hepatitis, dermatological diseases, rheumatologic diseases, trauma, gynecologic disease, toxicities, others and sings and symptoms.
Statistical analysis
The evaluation of the factors associated with 30-day readmission risk was performed using Cox extended regression models (accounting for clusters within patients). Patient’s follow-up started on the day of discharge from the index hospitalization and ended at the readmission date, date of death or 30 days after index discharge, whichever occurred first. Variables with p-value below 0.10 in the unadjusted analysis were included in the adjusted model in order to explore their effects after adjusting for all potential confounding. The variable “medical visit within 30-day of discharge” was included in the model as a time-dependent variable such that a patient’s follow up time was split into before and after the medical visit for those who attended a medical visit within 30-days of discharge. Using this approach, we also prevented a potential time-dependent bias, whereas patients who are soon readmitted have a decreased chance of having a medical visit after discharge. Proportional hazards assumption was tested using Schoenfeld residuals. R (version 3.0.3) and library “survival” were used for the analyses.
Ethical considerations
This study was approved by the ethics committee of the INI (CAAE 0032.0.009.000-10) and was conducted according to the principles expressed in the Declaration of Helsinki. All patient records/information were de-identified prior to analysis.
Results
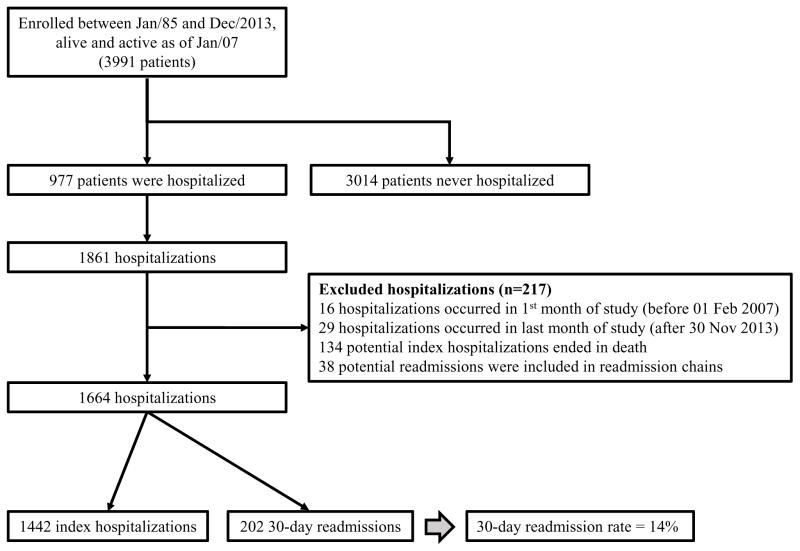
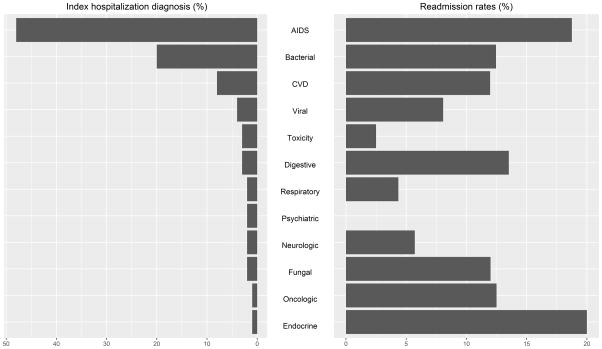
During the study period, from the 3991 included patients, 3014 were never hospitalized while 977 had at least one hospitalization during the study period. In total, 1861 hospitalization events occurred: 1442 were considered index hospitalizations, 202 were 30-day readmissions, and 16 index hospitalizations were followed by death after discharge (without readmission) (Figure 1). Thirty-day readmission rate was estimated as 14.0% (95% confidence interval [CI] 12.3%–15.9%). For those who readmitted, the median time between index discharge and readmission was 14 days (interquartile range [IQR]: 7–21). The three most frequent causes of index hospitalizations were AIDS-defining diseases (688/1442, 47.7%), bacterial infections (289/1442, 20.0%), and cardiovascular diseases (117/1442, 8.1%) (Figure 2). 30-day readmission rate among AIDS-defining diseases index hospitalizations reached 18.8% (95% CI 15.9%–21.9%) which is higher than the overall rate. The highest readmission rate was observed for endocrine diseases (20.0%, 95% CI 3.5%–55.8%) which comprised only 0.7% (n=10) of the index hospitalizations (Figure 2). Among the 202 readmissions, the most frequent cause of hospitalization was AIDS-defining diseases (129/202, 63.9%) and the second most frequent cause was bacterial infections (36/202, 17.8%).
Figure 1. Patients and hospitalizations.
Flowchart showing patient selection, total number of hospitalizations, hospitalization exclusion criteria and 30-day readmission rate.
Figure 2. Index hospitalizations causes and 30-day readmission rates per diagnosis.
Left panel shows proportion of index hospitalizations by cause of hospitalization. Right panel shows readmissions rate by index hospitalization cause. CVD: cardiovascular diseases.
Patients’ characteristics at the moment of the index hospitalization admission (stratified by yes/no 30-day readmission), as well as the unadjusted hazard ratios (cHR) are shown in Table 1. Compared to patients not readmitted, those who were readmitted were more likely to have recent (≤30 days) HIV infection diagnosis (14.9% vs. 8.5% among non-readmitted, Chi-squared p-value=0.019) and lower CD4 counts (median 118 cells/mm3 vs. 191 cells/mm3 among non-readmitted, Wilcoxon Rank-Sum test p-value<0.0001). On the other hand, patients who were readmitted were less likely to have used ART prior to index hospitalization (66.3% vs. 76.3% among non-readmitted, Chi-squared p-value=0.003) and to attend a medical visit within 30 days after index discharge (37.6% vs. 74.7% among non-readmitted, Chi-squared p-value<0.001). Moreover, index hospitalizations that were followed by 30-day readmissions had longer LOS (median 16 days vs. 12 days among non-readmitted, Wilcoxon Rank-Sum test p-value<0.001), had higher frequency of ICU stay (15.3% vs. 9.4% among non-readmitted, Chi-squared p-value=0.015), and more likely ended with a discharge against medical advice (5.4% vs. 2.5% among non-readmitted, Chi-squared p-value=0.029).
Table 1.
Socio-demographic and clinical characteristics and unadjusted hazard ratios (95% confidence interval) for patients who hospitalized stratified by readmission, INI cohort.
| Index hospitalizations | 30-day readmission | Unadjusted models uHR (95% CI) | ||
|---|---|---|---|---|
| Total (N = 1442) | No (N = 1240a) | Yes (N = 202) | ||
| Sex at birth | ||||
| Male | 932 (64.6) | 802 (64.7) | 130 (64.4) | ref |
| Female | 510 (35.4) | 438 (35.3) | 72 (35.6) | 1.02 (0.75, 1.37) |
| Age* (years) median (IQR) | 39.9 (33.2,47.1) | 40 (33.3,47.2) | 38.8 (32.2,46.7) | 0.99 (.098, 1.01) |
| <30 years | 233 (16.2) | 195 (15.7) | 38 (18.8) | ref |
| 30–39 years | 496 (34.4) | 428 (34.5) | 68 (33.7) | 0.85 (0.57, 1.27) |
| 40–49 years | 447 (31) | 388 (31.3) | 59 (29.2) | 0.81 (0.54, 1.22) |
| ≥50 years | 266 (18.4) | 229 (18.5) | 37 (18.3) | 0.87 (0.55, 1.36) |
| Race/ethnicity | ||||
| White | 616 (42.7) | 536 (43.2) | 80 (39.6) | ref |
| Non White | 826 (57.3) | 704 (56.8) | 122 (60.4) | 1.16 (0.87, 1.56) |
| Educational level | ||||
| Up to 9 years | 1026 (71.2) | 878 (70.8) | 148 (73.3) | ref |
| More than 9 years | 416 (28.8) | 362 (29.2) | 54 (26.7) | 0.88 (0.64, 1.22) |
| HIV exposure category | ||||
| Heterosexual | 900 (62.4) | 782 (63.1) | 118 (58.4) | ref |
| MSM | 446 (30.9) | 381 (30.7) | 65 (32.2) | 1.11 (0.82, 1.52) |
| IDU | 46 (3.2) | 36 (2.9) | 10 (5) | 1.76 (0.88, 3.51) |
| Other/unknown | 50 (3.5) | 41 (3.3) | 9 (4.5) | 1.45 (0.71, 2.94) |
| Time since HIV diagnosis (years)* | 5.4 (0.8,11.3) | 5.4 (0.9,11.3) | 4.6 (0.3,11.3) | |
| ≤30 days | 136 (9.4) | 106 (8.5) | 30 (14.9) | 2.16 (1.32, 3.55) |
| 31–365 days | 257 (17.8) | 218 (17.6) | 39 (19.3) | 1.42 (0.88, 2.29) |
| 1–5 years | 305 (21.2) | 272 (21.9) | 33 (16.3) | ref |
| 5–10 years | 294 (20.4) | 260 (21) | 34 (16.8) | 1.07 (0.68, 1.69) |
| >10 years | 450 (31.2) | 384 (31) | 66 (32.7) | 1.38 (0.89, 2.14) |
| CD4* (cells/mm3), median (IQR) | 177 (56,395) | 191 (62,414) | 118 (32,257) | |
| >350 | 360 (25) | 327 (26.4) | 33 (16.3) | ref |
| 201–350 | 222 (15.4) | 198 (16) | 24 (11.9) | 1.18 (0.69, 2.01) |
| 51–200 | 391 (27.1) | 328 (26.5) | 63 (31.2) | 1.87 (1.20, 2.91) |
| ≤50 | 283 (19.6) | 223 (18) | 60 (29.7) | 2.51 (1.61, 3.92) |
| Missing | 186 (12.9) | 164 (13.2) | 22 (10.9) | 1.36 (0.80, 2.31) |
| HIV viral load* (copies/mL) | ||||
| ≤400 | 499 (34.6) | 436 (35.2) | 63 (31.2) | ref |
| >400 | 699 (48.5) | 597 (48.1) | 102 (50.5) | 1.16 (0.85, 1.60) |
| Missing | 244 (16.9) | 207 (16.7) | 37 (18.3) | 1.19 (0.79, 1.79) |
| ART use prior to index hospitalization | ||||
| No | 362 (25.1) | 294 (23.7) | 68 (33.7) | ref |
| Yes | 1080 (74.9) | 946 (76.3) | 134 (66.3) | 0.64 (0.47, 0.87) |
| Time on ART (years), median (IQR)*b | 4.2 (1.1, 9.1) | 4.2 (1.1, 9.1) | 4.2 (0.8, 8.6) | |
| Length of stay, median (IQR)* | 12 (7,22) | 12 (7,22) | 16 (8,28) | |
| ≤7 days | 12 (7,22) | 364 (29.4) | 45 (22.3) | ref |
| 8–14 days | 409 (28.4) | 356 (28.7) | 50 (24.8) | 1.12 (0.75, 1.67) |
| 15–21 days | 406 (28.2) | 198 (16) | 34 (16.8) | 1.35 (0.86, 2.12) |
| >21 days | 232 (16.1) | 322 (26) | 73 (36.1) | 1.74 (1.19, 2.54) |
| Type of discharge* | ||||
| Medical discharge | 1300 (90.2) | 1128 (91) | 172 (85.1) | ref |
| Against medical advice | 42 (2.9) | 31 (2.5) | 11 (5.4) | 2.35 (1.25, 4.42) |
| Transfer | 33 (2.3) | 25 (2) | 8 (4) | 1.87 (0.98, 3.59) |
| Unknown | 67 (4.6) | 56 (4.5) | 11 (5.4) | 1.25 (0.68, 2.30) |
| ICU admission* | 148 (10.3) | 117 (9.4) | 31 (15.3) | 1.68 (1.14, 2.48) |
| Medical visit within 30 days after dischargec | 1002 (69.5) | 926 (74.7) | 76 (37.6) | 0.75 (0.55, 1.03) |
| Year of hospitalization | 0.87 (0.81, 0.94)d | |||
| 2007 | 126 (8.7) | 101 (8.1) | 25 (12.4) | |
| 2008 | 217 (15) | 177 (14.3) | 40 (19.8) | |
| 2009 | 226 (15.7) | 196 (15.8) | 30 (14.9) | |
| 2010 | 211 (14.6) | 170 (13.7) | 41 (20.3) | |
| 2011 | 268 (18.6) | 241 (19.4) | 27 (13.4) | |
| 2012 | 220 (15.3) | 198 (16) | 22 (10.9) | |
| 2013 | 174 (12.1) | 157 (12.7) | 17 (8.4) | |
MSM: Men who have sex with men; IDU: Injectable drug use; ART: combination antiretroviral therapy; ICU: intensive care unit; uHR: unadjusted hazard ratio.
Refers to index hospitalization or index hospitalization admission date.
Includes 16 patients who died within 30 days (without been readmitted)
Length of time of ART use prior to index hospitalization admission.
Defined as a medical visit before end of follow-up or readmission, for those who readmitted.
Year of hospitalization was included in the model as a continuous variable.
In unadjusted models, recent HIV infection diagnosis (≤30 days), CD4 counts bellow 200 cells/mm3, LOS longer than 21 days, ICU stay and discharge against medical advice significantly increased the risk of 30-day readmission. On the other hand, ART use prior to index hospitalization, being hospitalized in most recent calendar years and attending medical visit within 30 days after discharge protected against 30-day readmission (though this last variable had a p-value=0.072) (Table 1).
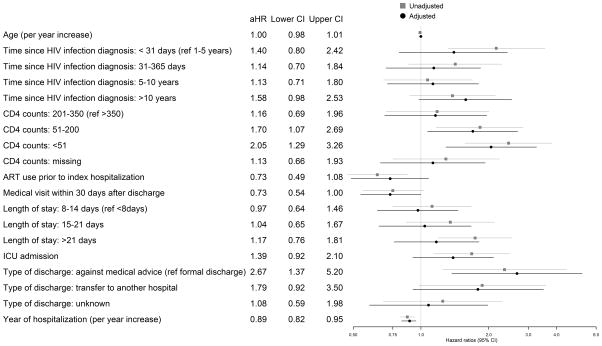
The final adjusted model is shown in Figure 3. Comparing the effects of the independent variables in the unadjusted and adjusted models, we found that after adjusting for covariates, the protective effect of attending a medical visit within 30 days of discharge remained similar but it gained statistical significance (adjusted hazard ratio [aHR] 0.73, p-value=0.048). Being hospitalized in most recent years also remained significant in the adjusted models (aHR 0.89, p-value=0.002). The protective effect of ART use prior to hospitalization observed in the unadjusted model was attenuated but the point estimate remained protective (although not statistically significant) after controlling for covariates (aHR 0.73, p-value = 0.113). On the other hand, CD4 counts ≤ 50 cells/mm3 (aHR 2.05, p-value = 0.003) and between 200-51 cells/mm3 (aHR 1.70, p-value = 0.024) and leaving the hospital against medical advice (aHR 2.67, p-value = 0.004) increased the risk of 30-day readmission. Additionally, after adjusting for covariates, having HIV infection diagnosis for 10 or more years also borderline increased the risk of 30-day readmission (aHR 1.58, p-value= 0.058).
Figure 3. Adjusted extended Cox regression model.
Hazard ratios and 95% confidence intervals for 30-day readmission.
Discussion
In the present study, we have estimated the 30-day readmission rate for an HIV infected cohort followed in Rio de Janeiro, Brazil. Our estimated 14% readmission rate is lower than the rates reported for HIV infected patients in high-income settings. Nijhawan et al. estimated a 25% readmission rate in Dallas, US17, Berry at al. reported 19% readmission rate for the HIV Research Network (HIVRN, which includes 12 sites in the US) 16, and a US national report (using data from Healthcare Cost and Utilization Project) found a readmission rate of 20% for HIV infected patients10. The reasons for the disparate readmission rates likely include patient, hospital and health care system as well as community characteristics3 beyond those that we have been able to address. Nonetheless, patient-level characteristics shown to increase the risk of readmission, such as those indicative of advanced disease, were similar among ours and the previous studies16,17,21, highlighting sub-populations for whom efforts could be targeted. Moreover, our results shed light on the benefits of an early post-discharge medical visit in preventing readmission.
After adjusting for potential confounding variables, having an early post discharge medical visit reduced the risk of readmission by 27% in our study population. This finding is in agreement with a previously described protective effect of careful transitioning to the outpatient setting on reducing the risk of readmission among patients with other chronic conditions22–25. Additionally, it might indicate a better post discharge support system (i.e family and social support) that has also been associated with lower risk of hospital readmission24,26. Interestingly, among HIV-infected patients, only one study reported on this association and found no link between early transition to outpatient care and 30-day readmission16. Thus, although our results are consistent with previous studies that included patients with other chronic diseases, confirmatory studies are needed to provide more reliable information on the effect of attending an outpatient visit on 30-day readmission rates for the HIV infected population.
Our study corroborates results reported by Berry et al, Feller et al and Nijhawan et al16,17,21 by showing that a proxy of advanced HIV/AIDS disease such as low CD4 counts at index hospitalization is associated with an increased risk of readmission. This finding highlights the impact that advanced chronic diseases27,28, in our case, advanced HIV disease, has on 30-day readmission risk. To focus clinical efforts in this severely ill sub-population seems feasible given they represent only a small fraction of patients under follow-up. For the present cohort, this sub-population would amount to approximately 15% of the patients under follow-up as only 588 patients had an AIDS-defining disease or poor immune function at index hospitalization out of 3991 patients under follow-up. Additionally, ART use prior to the index hospitalization may likely reduced the risk of 30-day readmission (though this result was not statistically significant in the present analysis). Importantly, when we stratified ART use into recent start (≤30 days) or not (more than 30 days of use prior to index hospitalization admission) we did not find an increased risk of readmission associated with recent ART start that could be linked to Immune Reconstitution Inflammatory Syndrome and/or acute toxic events (data not shown). Similarly, both Berry et al and Nijhawan et al explored this possible risk association (recent ART and readmission risk) and neither found an association16,17. Taken together, these findings suggest that early ART use for all HIV-infected patients might not only prevent HIV disease progression and HIV transmission but may as well reduce 30-day readmission.
Another interesting finding from our study was the fact that long term HIV infected patients, i.e. those diagnosed for 10 or more years, were at higher risk of 30-day readmissions after controlling for all other covariates (including age). We can speculate on some plausible explanations for this finding. It is possible that some chronically HIV infected patients, likely heavily ART experienced, are presenting with multidrug HIV resistance and/or poor adherence and therefore disease progression, leading to increased risk of readmission. This hypothesis is supported by the fact that although 94.2% of those patients had used ART prior to index hospitalization, less than half (47%) had a viral load < 400 copies/mL (data not shown). Another possible reason would be the fact that HIV chronic infection leads to persistent inflammation and immune activation which is associated with increased risk of cardiovascular disease, cancer and other non-AIDS related events29,30. Corroborating this hypothesis, we found that index hospitalizations among patients with HIV diagnosis for 10 or more years were less likely to be due to an AIDS defining disease (29% vs. 47% among all index hospitalizations), and that the readmission rate for digestive diseases index hospitalizations surpassed the one for AIDS-defining diseases index hospitalizations (23.8% vs. 21.4%) highlighting the importance of non-AIDS events on the risk of readmission for this particular population subset. In summary, a multicausal pathway that encompasses aging, higher prevalence of non-communicable diseases, ART failure seems to be a more plausible explanation for the increased readmission risk observed among HIV long term infected patients.
Additionally, our results show that patients who left the hospital against medical advice had a two-fold higher risk of 30-day readmission. Indeed, discharge against medical advice had already been associated with increased risk of 30-day readmission in the general population31 and among those with HIV13,21,32. Interestingly, compared to HIV-uninfected patients, HIV infected patients were shown to have a higher risk of leaving the hospital against medical advice32. Specifically, among HIV infected patients, leaving hospital against medical advice led to a 5-fold increased odds of 30-day readmission for a related diagnosis and was associated with longer readmission LOS (compared to those who had been formally discharged)13. Altogether, interventions focusing on reducing such discharges are needed to improve patients’ health and reduce unnecessary costs with readmissions.
AIDS-defining diseases were the main cause of index hospitalizations comprising almost half of all admissions, followed by bacterial infections. Endocrine diseases had the highest readmission rate in our study population, a finding that results from the very small number of index hospitalizations (i.e. small denominator) while AIDS-defining diseases led to the second highest readmission rate. These findings are somewhat different from those observed in previous studies. In the HIVRN population, non-AIDS infections were the main cause of index hospitalizations, and the highest 30-day readmission rate was observed for oncologic index hospitalizations, with the second highest 30-day readmission rate for an AIDS-defining disease index hospitalization16. Nijhawan et al also found AIDS-defining diseases as the main cause of index hospitalizations but the oncologic hospitalizations led the 30-day readmission rates and AIDS-related diseases came in fifth 17. Several factors can explain these differences in the rating of the causes of index hospitalizations and readmissions. Foremost, the burden of AIDS diseases in the context of hospitalizations is quite different between our study population and HIVRN population. In our population, the proportion of index hospitalizations due to AIDS-defining diseases was 5-fold higher than that observed for the HIVRN population (47.7% vs. 9.6%) 16 likely driving the ranking for both index hospitalizations and readmissions. Additionally, differences in the burden of cancer among our study population and HIV-infected populations from high-income settings might explain some of these disparities. A recent study compared the incidence of cancer (AIDS and non-AIDS defining) between HIV infected patients from INI cohort and Vanderbilt Comprehensive Care Clinic cohort (Nashville, US) and showed significant differences on the incidence of cancer between these two HIV-infected populations33. They showed that the incidence of AIDS defining cancer was higher in INI than in Vanderbilt, mainly driven by Kaposi sarcoma incidence (almost three times higher in INI). On the other hand, non-AIDS defining cancer incidence was higher in Vanderbilt than in INI, and the most incident cancer types were also different (anal cancer in INI vs. lung cancer in Vanderbilt). It is worthwhile mentioning that although INI provides treatment of Kaposi sarcoma, mostly administrated in a day clinic (including monitoring and management of potential side effects such as leukopenia), all other oncologic and chemotherapy-relate hospitalization are referred to another facility and thus not included in this analysis. As such, the findings regarding oncologic admissions and readmissions should be compared with caution to other published results.
Overall, the median LOS of index hospitalizations (12 days) surpasses the one reported for the HIVRN population (median of 5 days)16 and the one reported by Nijhawan et al (mean 7 days)17 but is closer to a national HIV-infected Portuguese estimate (median 11 days)34. And similarly to Berry et al16, we found that compared with other causes, hospitalizations due to AIDS defining diseases were associated with longer LOS (median of 18 vs. 9 days for AIDS and non-AIDS related hospitalizations, respectively, data not shown). Differences in hospital structure, hospital setting and health system level factors could be the sources of such disparities. For the purpose of comparison with Brazilian data, we searched publicly available databases that provide mean LOS and found that overall the mean LOS estimated for the state of Rio de Janeiro in the period of 2008–2015 was 9 days, while, for the same period, the national mean was 7 days revealing the high heterogeneity that exists when it comes to hospital outcomes even within Brazil35.
There are several limitations that need to be highlighted in the present study, some of which were already addressed throughout this discussion. First, the comparison of readmission rates in our setting with that reported in the United States and other high-income countries must be made cautiously since there are hospital and health systems level factors, in addition to patient level factors, that can influence this outcome. In fact, such factors likely influence two other outcomes related to hospitalizations, LOS and in-hospital mortality, for which published results can be compared. The median index hospitalization LOS observed in our study is >2-fold higher than previously described in a US study (12 days versus 5 days reported by Berry et al16). One explanation for this difference is the primary cause of the hospitalization as AIDS-related hospitalizations are associated with longer LOS than non-AIDS related ones both in high- and middle-income settings36–38. Moreover, in our study, AIDS-related hospitalizations comprised almost half of the hospitalizations while in Berry et al. in represented only 9.6% of the index hospitalizations16. In addition, the pressure to reduce LOS in US hospitals has led to significant reductions in LOS39 while this is much less present in the Brazilian public health system. An examination of in-hospital mortality results also shed light on the discussion. In a previous study from our hospital, we found that in-hospital mortality for HIV-infected patients was 9.2%, which contrasts with the 2.6% mortality rate reported by a tertiary hospital in New York40. Of note, the potential inverse correlation between in-hospital mortality and readmission risk (i.e. the higher the mortality rate the lower the readmission41) may also be playing a role.
Second, our study sample is from a single cohort that has access to an outpatient clinic as well as an infectious diseases hospital located in Rio de Janeiro, hence our results may not reflect those for other HIV populations in Brazil. Third, hospitalizations at Evandro Chagas hospital are restricted to non-surgical and non-obstetrics procedures, and, as mentioned earlier, oncologic hospitalizations (except for Kaposi sarcoma) are mainly referred to an oncological hospital and therefore our rates do not represent the entire sort of events that can happen to an HIV infected patient. Furthermore, we cannot rule out the occurrence of readmissions to other hospitals, implying that our readmission rate may be underestimated. Finally, other factors, not addressed in the present study, were found associated with readmission and merit further investigation including socioeconomic (income, housing stability, social/family support), behavioral (alcohol use) as well as comorbidities (in particular mental illnesses). For instance, Feller et al., while studying readmission in HIV infected patients in New York State, identified that multiple comorbidities, alcohol abuse, diagnosis of depression or psychosis, previous hospitalizations and emergency department visits and unstable housing all increased the risk of 30-day readmission21. Additionally, recent studies have shown that functional status at index hospitalization can also be associated with early readmissions42,43.
In summary, we found that the 30-day readmission rate in our HIV infected cohort of patients was 14%. To our knowledge, ours is the first study to estimate and address 30-day readmission among HIV infected individuals in Brazil and, as such, provides a benchmark until more comprehensive data is available for the country. We also showed that attending an early medical visit after discharge had an important effect on preventing readmissions; this finding could be used to create/modify transition protocols to reduce readmission rates in the future. Finally, we demonstrated that patients with advanced HIV/AIDS (i.e. low CD4 counts) have higher risk of readmission and that ART may reduce this risk, thus indicating early HIV diagnosis and prompt ART start as strategies that could reduce 30-day readmissions.
Acknowledgments
Acknowledgements and funding
PML and BG acknowledge funding from the National Council of Technological and Scientific Development (CNPq) and the Research Funding Agency of the State of Rio de Janeiro (FAPERJ). This work was supported in part by the NIH-funded Caribbean, Central and South America network for HIV epidemiology (CCASAnet), a member cohort of the International Epidemiologic Databases to Evaluate AIDS (leDEA) (U01AI069923).
Footnotes
Authors’ contributions
LEC and PML conceived the study, performed the analyses, and drafted the manuscript. LEC, SRR and PCL reviewed hospitalizations’ discharge summaries and followed the protocol for assigning ICD-10 codes/causes to all hospitalizations. AMJ and RIM were in charge of obtaining and reviewing patient data and were responsible for data harmonization. BG and VGV contributed to the study’s design and were involved in revising the manuscript for important intellectual content. All authors read and approved the final manuscript.
Competing interests
The authors declare no competing interests.
References
- 1.Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011;155(8):520–528. doi: 10.7326/0003-4819-155-8-201110180-00008. [DOI] [PubMed] [Google Scholar]
- 2.Brasil. Agência Nacional de Saúde Suplementar - ANS. Fichas Técnicas e Nota técnica n° 34/DIDES. [Accessed February 2, 2017];Indicadores do Fator de Qualidade. 2015 Dez; http://www.ans.gov.br/images/stories/Plano_de_saude_e_Operadoras/Area_do_prestador/contrato_entre_operadoras_e_prestadores/indicadores-e-nota.pdf.
- 3.Joynt KE, Jha AK. Thirty-day readmissions--truth and consequences. N Engl J Med. 2012;366(15):1366–1369. doi: 10.1056/NEJMp1201598. [DOI] [PubMed] [Google Scholar]
- 4.Dharmarajan K, Hsieh AF, Lin Z, et al. Hospital readmission performance and patterns of readmission: retrospective cohort study of Medicare admissions. BMJ. 2013;347(nov19 23):f6571–f6571. doi: 10.1136/bmj.f6571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 6.Barret ML, Wier LM, Jiang J, Steiner CA. All-Cause Readmissions by Payer and Age, 2009–2013. Agency Healthc Res Qual HCUP Stat Brief. 2015;199 [Google Scholar]
- 7.van Walraven C, Bennett C, Jennings A, Austin PC, Forster AJ. Proportion of hospital readmissions deemed avoidable: a systematic review. CMAJ Can Med Assoc J J Assoc Medicale Can. 2011;183(7) doi: 10.1503/cmaj.101860.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ross JS, Mulvey GK, Stauffer B, et al. Statistical models and patient predictors of readmission for heart failure: a systematic review. Arch Intern Med. 2008;168(13):1371–1386. doi: 10.1001/archinte.168.13.1371. [DOI] [PubMed] [Google Scholar]
- 9.Mannino DM, Thomashow B. Reducing COPD readmissions: great promise but big problems. Chest. 2015;147(5):1199–1201. doi: 10.1378/chest.15-0380. [DOI] [PubMed] [Google Scholar]
- 10.Berry S, Fleishman J, Moore R, Gebo K. Thirty-day hospital readmissions for adults with and without HIV infection: HIV readmissions. HIV Med. 2015 Aug; doi: 10.1111/hiv.12287.. n/a - n/a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nijhawan AE, Kitchell E, Etherton SS, Duarte P, Halm EA, Jain MK. Half of 30-Day Hospital Readmissions Among HIV-Infected Patients Are Potentially Preventable. AIDS Patient Care STDs. 2015;29(9):465–473. doi: 10.1089/apc.2015.0096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barba Martin R, Marco Martinez J, Plaza Canteli S, et al. Retrospective study of early readmissions at an internal medicine service. Rev Clin Esp. 2000;200(5):252–256. doi: 10.1016/s0014-2565(00)70624-2. [DOI] [PubMed] [Google Scholar]
- 13.Anis AH, Sun H, Guh DP, Palepu A, Schechter MT, O’Shaughnessy MV. Leaving hospital against medical advice among HIV-positive patients. Can Med Assoc J. 2002;167(6):633–637. [PMC free article] [PubMed] [Google Scholar]
- 14.Chew KW, Yen IH, Li JZ, Winston LG. Predictors of Pneumonia Severity in HIV-Infected Adults Admitted to an Urban Public Hospital. AIDS Patient Care STDs. 2011;25(5):273–277. doi: 10.1089/apc.2010.0365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hsieh Y-H, Rothman RE, Bartlett JG, Yang S, Kelen GD. HIV seropositivity predicts longer duration of stay and rehospitalization among nonbacteremic febrile injection drug users with skin and soft tissue infections. JAIDS J Acquir Immune Defic Syndr. 2008;49(4):398–405. doi: 10.1097/qai.0b013e318183ac84. [DOI] [PubMed] [Google Scholar]
- 16.Berry SA, Fleishman JA, Yehia BR, et al. Thirty-day hospital readmission rate among adults living with HIV. AIDS. 2013;27(13):2059–2068. doi: 10.1097/QAD.0b013e3283623d5f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nijhawan AE, Clark C, Kaplan R, Moore B, Halm EA, Amarasingham R. An electronic medical record-based model to predict 30-day risk of readmission and death among HIV-infected inpatients. JAIDS J Acquir Immune Defic Syndr. 2012;61(3):349–358. doi: 10.1097/QAI.0b013e31826ebc83. [DOI] [PubMed] [Google Scholar]
- 18.Grinsztejn B, Veloso VG, Friedman RK, et al. Early mortality and cause of deaths in patients using HAART in Brazil and the United States. AIDS. 2009;23(16):2107–2114. doi: 10.1097/QAD.0b013e32832ec494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ribeiro SR, Luz PM, Campos DP, et al. Incidence and determinants of severe morbidity among HIV-infected patients from Rio de Janeiro, Brazil, 2000–2010. Antivir Ther. 2014;19(4):387–397. doi: 10.3851/IMP2716. [DOI] [PubMed] [Google Scholar]
- 20.Grinsztejn B, Luz PM, Pacheco AG, et al. Changing Mortality Profile among HIV-Infected Patients in Rio de Janeiro, Brazil: Shifting from AIDS to Non-AIDS Related Conditions in the HAART Era. In: Yazdanpanah Y, editor. PLoS ONE. 4. Vol. 8. 2013. p. e59768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Feller DJ, Akiyama M, Gordon P, Agins BD. Readmissions in HIV-infected Inpatients: A Large Cohort Analysis. JAIDS J Acquir Immune Defic Syndr. 2015 Oct;:1. doi: 10.1097/QAI.0000000000000876.. [DOI] [PubMed] [Google Scholar]
- 22.Coleman EA, Parry C, Chalmers S, Min S. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006;166(17):1822–1828. doi: 10.1001/archinte.166.17.1822. [DOI] [PubMed] [Google Scholar]
- 23.Peikes D, Chen A, Schore J, Brown R. Effects of care coordination on hospitalization, quality of care, and health care expenditures among Medicare beneficiaries: 15 randomized trials. Jama. 2009;301(6):603–618. doi: 10.1001/jama.2009.126. [DOI] [PubMed] [Google Scholar]
- 24.Sharma G, Kuo Y-F, Freeman JL, Zhang DD, Goodwin JS. Outpatient follow-up visit and 30-day emergency department visit and readmission in patients hospitalized for chronic obstructive pulmonary disease. Arch Intern Med. 2010;170(18):1664–1670. doi: 10.1001/archinternmed.2010.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen H, Tisminetzky M, Lapane KL, et al. Decade-Long Trends in 30-Day Rehospitalization Rates After Acute Myocardial Infarction. J Am Heart Assoc. 2015;4(11):e002291. doi: 10.1161/JAHA.115.002291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Arbaje AI, Wolff JL, Yu Q, Powe NR, Anderson GF, Boult C. Postdischarge environmental and socioeconomic factors and the likelihood of early hospital readmission among community-dwelling Medicare beneficiaries. The Gerontologist. 2008;48(4):495–504. doi: 10.1093/geront/48.4.495. [DOI] [PubMed] [Google Scholar]
- 27.Berry CE, Kalhan R. Chronic Obstructive Pulmonary Disease Rehospitalization. A Big Problem that Now Needs Solutions. Ann Am Thorac Soc. 2015;12(12):1741–1742. doi: 10.1513/AnnalsATS.201510-687ED. [DOI] [PubMed] [Google Scholar]
- 28.Desai AS, Stevenson LW. Rehospitalization for Heart Failure: Predict or Prevent? Circulation. 2012;126(4):501–506. doi: 10.1161/CIRCULATIONAHA.112.125435. [DOI] [PubMed] [Google Scholar]
- 29.Erlandson KM, Campbell TB. Inflammation in Chronic HIV Infection: What Can We Do? J Infect Dis. 2015;212(3):339–342. doi: 10.1093/infdis/jiv007. [DOI] [PubMed] [Google Scholar]
- 30.Deeks SG, Lewin SR, Havlir DV. The end of AIDS: HIV infection as a chronic disease. The Lancet. 2013;382(9903):1525–1533. doi: 10.1016/S0140-6736(13)61809-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Glasgow JM, Vaughn-Sarrazin M, Kaboli PJ. Leaving Against Medical Advice (AMA): Risk of 30-Day Mortality and Hospital Readmission. J Gen Intern Med. 2010;25(9):926–929. doi: 10.1007/s11606-010-1371-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Alfandre D, Yang J, Harwood K, et al. “Against Medical Advice” Discharges Among HIV-Infected Patients: Health and Health Services Outcomes. J Assoc Nurses AIDS Care. 2017;28(1):95–104. doi: 10.1016/j.jana.2016.10.002. [DOI] [PubMed] [Google Scholar]
- 33.Castilho JL, Luz PM, Shepherd BE, et al. HIV and cancer: a comparative retrospective study of Brazilian and U.S. clinical cohorts. Infect Agent Cancer. 2015:10. doi: 10.1186/1750-9378-10-4.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Catumbela E, Freitas A, Lopes F, et al. HIV disease burden, cost, and length of stay in Portuguese hospitals from 2000 to 2010: a cross-sectional study. BMC Health Serv Res. 2015;15(1) doi: 10.1186/s12913-015-0801-8.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ministério da Saúde. Departamento de informática do SUS (DATASUS) Sistema de Informações Hospitalares do SUS (SIH/SUS) Brasil: [Access date: 02/02/2016]. www.datasus.gov.br. [Google Scholar]
- 36.Krentz HB, Dean S, Gill MJ. Longitudinal assessment (1995–2003) of hospitalizations of HIV-infected patients within a geographical population in Canada. HIV Med. 2006;7(7):457–466. doi: 10.1111/j.1468-1293.2006.00408.x. [DOI] [PubMed] [Google Scholar]
- 37.Berry SA, Fleishman JA, Moore RD, Gebo KA. Trends in reasons for hospitalization in a multisite United States cohort of persons living with HIV, 2001–2008. J Acquir Immune Defic Syndr 1999. 2012;59(4):368–375. doi: 10.1097/QAI.0b013e318246b862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Coelho LE, Ribeiro SR, Veloso VG, Grinsztejn B, Luz PM. Hospitalization rates, length of stay and in-hospital mortality in a cohort of HIV infected patients from Rio de Janeiro, Brazil. Braz J Infect Dis. 2016 Dec; doi: 10.1016/j.bjid.2016.10.007.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kaboli PJ, Go JT, Hockenberry J, et al. Associations between reduced hospital length of stay and 30-day readmission rate and mortality: 14-year experience in 129 Veterans Affairs hospitals. Ann Intern Med. 2012;157(12):837–845. doi: 10.7326/0003-4819-157-12-201212180-00003. [DOI] [PubMed] [Google Scholar]
- 40.Kim JH, Psevdos G, Gonzalez E, Singh S, Kilayko MC, Sharp V. All-cause mortality in hospitalized HIV-infected patients at an acute tertiary care hospital with a comprehensive outpatient HIV care program in New York City in the era of highly active antiretroviral therapy (HAART) Infection. 2013;41(2):545–551. doi: 10.1007/s15010-012-0386-7. [DOI] [PubMed] [Google Scholar]
- 41.Gorodeski EZ, Starling RC, Blackstone EH. Are all readmissions bad readmissions? N Engl J Med. 2010;363(3):297–298. doi: 10.1056/NEJMc1001882. [DOI] [PubMed] [Google Scholar]
- 42.Shih SL, Gerrard P, Goldstein R, et al. Functional Status Outperforms Comorbidities in Predicting Acute Care Readmissions in Medically Complex Patients. J Gen Intern Med. 2015;30(11):1688–1695. doi: 10.1007/s11606-015-3350-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Greysen SR, Stijacic Cenzer I, Auerbach AD, Covinsky KE. Functional Impairment and Hospital Readmission in Medicare Seniors. JAMA Intern Med. 2015;175(4):559. doi: 10.1001/jamainternmed.2014.7756. [DOI] [PMC free article] [PubMed] [Google Scholar]