Abstract
Background
Management of adolescent patients with end-stage arthritis is challenging. Nonoperative treatments may be ineffective and total knee arthroplasty (TKA) is rarely performed. Currently, minimal long-term data are available on the outcomes in this patient population. Our goal was to describe TKA for patients with end-stage arthritis who were aged 20 years and younger.
Methods
The Joint Registry at our institution was used to identify 19 patients (29 TKAs) aged 20 years and younger that underwent a primary TKA. The average age was 18 years (range 14-20 years) and follow-up was 14.5 years (range: 2.1-25.5 years).
Results
The preoperative diagnoses were juvenile idiopathic arthritis (n = 19), avascular necrosis (n = 4), sepsis (n = 2), trauma (n = 2), dysplasia (n = 1), and hemophilia (n = 1). There was a decrease in the number of TKAs performed for inflammatory arthritis over the last several decades. Implant survivorship at 5 and 10 years was 96% and 94%, respectively.
Conclusions
We identified a 95% 10-year implant survivorship utilizing standard TKA components in pediatric patients. Performing a TKA in adolescent patients has long-term potential risks including infection and bone loss but may provide pain relief and good long-term results and should be used with caution.
Keywords: Total knee arthroplasty, Adolescent orthopedics, Arthritis
Introduction
Total knee arthroplasty (TKA) in patients less than 20 years old is a very rarely performed procedure. At our institution, this patient population comprises approximately 0.09% of all patients undergoing TKA. However, severe debilitating gonarthrosis has limited treatment options in adolescent patients. Most commonly, nonoperative modalities are recommended initially, which include activity modification, nonsteroidal anti-inflammatory agents, and knee braces. In some patients, nonoperative modalities do not provide enough pain relief and patients may experience an unacceptable decrease in quality of life. Current operative interventions are limited, and long-term outcomes are poorly defined. The goal of this project was to define these outcomes for TKA in this unique patient population.
Surgical indications for adolescent TKA have been inadequately defined, and this operation should likely be reserved for a very specific subset of patients. Common pathologies that lead to severe joint destruction include juvenile rheumatoid arthritis, avascular necrosis (AVN), infection, and trauma.
There has been very limited research on adolescent TKA [1], [2], [3]. Most of the studies include a wide variety of patient populations encompassing both total hip arthroplasty patients and patients over 20 years old. One recent study specifically examined 105 patients 21 years and younger who underwent primary TKA [4]. However, most of this cohort had joint replacement surgery performed secondary to a preoperative diagnosis of tumor.
The aim of our present study was to determine the long-term outcomes in a subset of patients 20 years or younger who underwent TKA for end-stage arthritis. We specifically limited our patient population to patients who underwent TKA with primary knee replacements (excluding distal femoral replacements and hinges) and excluded patients with underlying malignancy or oncology diagnosis. We identified the most common complications and mechanisms of failure in this patient population. Finally, we determined the overall implant survivorship in this cohort.
Material and methods
The Total Joint Registry at our institution was evaluated from 1979 to 2013 to identify all cases of primary TKA performed on patients 20 years or younger. Institutional review board approval was obtained per institutional guidelines, and patients who denied research authorization were excluded. Both demographic and clinical data are routinely updated from inpatient and outpatient electronic medical records to ensure accurate and up-to-date information on patient outcomes in the Joint Registry. Selection criteria for our study included (1) primary TKA, (2) minimum follow-up of 2 years, and (3) age 20 years or less. Patients with an underlying diagnosis of tumor were excluded. Utilizing these criteria, we identified 19 patients (29 knees).
Demographic data were recorded for each patient including age at the time of the index surgery, sex, body mass index, and preoperative diagnosis. Underlying diagnoses were categorized as posttraumatic arthritis, inflammatory arthritis, degenerative arthritis, congenital conditions, and other diagnoses (including osteonecrosis). Standard patient follow-up included a 3-month, 1-year, 2-year, 5-year, and every subsequent 5-year recheck with clinical and radiographic evaluation at each time interval. Complications and reoperations were recorded on a continuous basis throughout the duration of the study. Complications were separated into intraoperative and postoperative as well as type of complication. Due to the complexity of the various complication codes entered into the Joint Registry Database, an all cause complication rate as well as the most common complication diagnoses were recorded.
Results
From 1979 to 2013, approximately 30,000 primary TKAs were performed at our institution. We identified 19 patients with 29 total knee arthroplasties with a minimum of 2-year follow-up (0.09% of all patients undergoing primary TKA). The average follow-up was 14.5 years (range 2-25). There were 24 TKAs (15 patients) with at least 5 years of follow-up and 17 TKAs (12 patients) available for follow-up at 10 years. Most patients were female (n = 15). The age at time of surgery ranged from 14 to 20 years old with an average age of 18 years old. Juvenile idiopathic arthritis was the most common underlying diagnosis for TKA (n = 10). Other underlying diagnoses included: AVN (n = 3), septic arthritis (n = 2), posttraumatic arthritis (n = 2), knee dysplasia (n = 1), and hemophilia (n = 1). Twenty-three of the 29 knees were posterior stabilized knees, 2 were constrained condylar knees, and 4 were unknown custom implants (Table 1).
Table 1.
Patient demographic information.
| TKA | Gender | Side | Diagnosis | Age at surgery | Implant | Follow-up (y) |
|---|---|---|---|---|---|---|
| 1 | Female | Right | AVN: steroid induced | 15 | PSa | 5.90 |
| 2 | Male | Left | AVN: steroid induced | 18 | PS | 2.06 |
| 3 | Female | Right | DJD | 19 | PS | 9.50 |
| 4 | Female | Left | DJD | 19 | PS | 5.76 |
| 5 | Male | Right | Inflammatory arthritis (JIA) | 19 | PS | 2.30 |
| 6 | Female | Left | Post-traumatic DJD | 19 | PS | 5.54 |
| 7 | Female | Right | DJD secondary to septic arthritis | 20 | PS | 2.90 |
| 8 | Male | Right | Blounts | 19 | PSa | 5.51 |
| 9 | Female | Left | Inflammatory arthritis (JIA) | 15 | CCK | 16.19 |
| 10 | Female | Right | Inflammatory arthritis (JIA) | 15 | CCK | 16.19 |
| 11 | Female | Left | Inflammatory arthritis (JIA) | 16 | PS | 20.59 |
| 12 | Female | Right | Inflammatory arthritis (JIA) | 16 | PS | 20.59 |
| 13 | Female | Right | Inflammatory arthritis (JIA) | 19 | PSa | 15.26 |
| 14 | Female | Left | Inflammatory arthritis (JIA) | 20 | PS | 14.07 |
| 15 | Female | Left | Post-traumatic DJD | 19 | PS | 20.40 |
| 16 | Female | Left | Inflammatory arthritis (JIA) | 17 | Custom | 20.02 |
| 17 | Female | Right | Inflammatory arthritis (JIA) | 17 | Custom | 19.86 |
| 18 | Female | Left | Inflammatory arthritis (JIA) | 17 | PS | 19.84 |
| 19 | Female | Right | Inflammatory arthritis (JIA) | 17 | PS | 19.84 |
| 20 | Female | Left | Inflammatory arthritis (JIA) | 19 | Custom | 20.85 |
| 21 | Female | Right | Inflammatory arthritis (JIA) | 19 | Custom | 20.71 |
| 22 | Female | Left | Inflammatory arthritis (JIA) | 19 | PS | 22.57 |
| 23 | Female | Right | Inflammatory arthritis (JIA) | 19 | PS | 22.57 |
| 24 | Female | Left | Inflammatory arthritis (JIA) | 19 | PS | 25.54 |
| 25 | Female | Right | Inflammatory arthritis (JIA) | 19 | PS | 25.54 |
| 26 | Female | Right | Inflammatory arthritis (JIA) | 19 | PS | 6.01 |
| 27 | Female | Left | Inflammatory arthritis (JIA) | 19 | PS | 5.76 |
| 28 | Female | Left | AVN: steroid induced | 14 | PSa | 2.24 |
| 29 | Female | Right | AVN: steroid induced | 14 | PSa | 2.24 |
CCK, constrained condylar knees; DJD, degenerative joint disease; JIA, juvenile idiopathic arthritis; PS, posterior stabilized.
Designates rotating platform design.
Of the 19 knees that had a preoperative diagnosis of juvenile inflammatory arthritis, 8 were performed in the 1980s, 8 in the 1990s, 3 in the 2000s, and 0 in the 2010s (Fig. 1). In this group that underwent TKAs for inflammatory arthritis, no patients were on a biologic agent for inflammatory arthritis at the time of the TKA.
Figure 1.
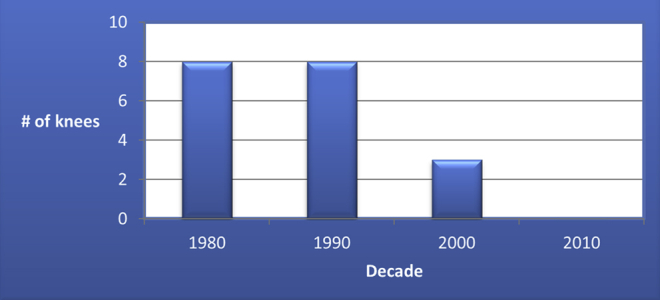
Incidence of inflammatory arthritis.
The overall revision free survival at 5 and 10 years was 96 and 94%, respectively. Twenty-two percent of knees required revision surgery (n = 6) at the time of final follow-up. The most common reasons for revision surgery included: aseptic loosening or polyethylene wear (n = 4) and infection requiring a 2-stage revision 16 years after the index procedure (n = 1) and one patient was revised at an outside facility for an unknown reason (n = 1) (Table 2). One patient had bilateral TKAs and developed significant polyethylene wear at 12 years postoperatively, subsequently undergoing simultaneous bilateral polyethylene exchange. Two patients underwent revision surgery for aseptic loosening at 9 and 11 years post TKA.
Table 2.
Patient revision data.
| Reason for revision | Time from index surgery | Treatment | Outcome |
|---|---|---|---|
| Infection | 16 y | Two stage revision | Knee doing well at follow-up. ROM 0°-105°. |
| Aseptic loosening | 11 y | Revision TKA | 6 y after revision, painless ROM 0°-90° |
| Aseptic loosening | 5 y | Revision TKA | Painless ROM 0°-90° at 15 y from revision |
| Poly wear | 12 y | Poly exchange | At 8 y after poly exchange, mild knee pain with knee ROM 0°-120°. No evidence of osteolysis |
| Poly wear | 12 y | Poly exchange | At 8 years after poly exchange mild knee pain with knee ROM 0°-130°. Mild poly wear lateral compartment, no osteolysis |
Poly, polyethylene; ROM, range of motion.
In our studied patient population, 44% (n = 11) experienced a complication (Table 3). Stiffness was the most common complication with 15% of knees requiring a manipulation under anesthesia (n = 4). One of the knees requiring postoperative manipulation was noted to have had a preoperative diagnosis of arthrofibrosis requiring manipulation before the index TKA procedure. This patient had developed arthrofibrosis following an infection after knee arthroscopy before undergoing a TKA. Another patient had a traumatic injury to the extensor mechanism which required an allograft extensor mechanism reconstruction. Five years postoperatively, this patient had full extension but was limited in flexion to 80°. At final follow-up, the patient was satisfied with her overall function. One other patient had partial wound necrosis which required revision of the surgical wound about 2 weeks postoperatively. This patient did not develop a deep infection or any additional sequelae.
Table 3.
Patient complication data.
| Complication | Time from index surgery | Treatment | Outcome |
|---|---|---|---|
| Stiffness | 7 d | MUA | Pre MUA 20°-110° flexion. Five years after MUA, knee ROM 15°-115° |
| Stiffness | 7 d | MUA | Pre MUA 15°-105° flexion, 5 y after MUA, knee ROM 5°-115° |
| Stiffness in setting of hemophilia | 1 mo | MUA | Pre MUA 30°-60° flexion. Required 3 MUA over 3 mo. Current follow-up at 5 y has ROM 0°-100° |
| Stiffness | 3 mo | MUA | Pre MUA 5°-80°, post MUA ROM 0°-95° flexion at 18 mo s/p MUA |
| Stiffness preoperatively due to gunshot with extensor mechanism disruption | — | Did not require manipulation | Knee ROM 0°-80° flex. Improved from preop 0°-15° |
| Wound necrosis | 2 wk | Wound revision, primary closure | No further wound issues or infection at 2 y follow-up |
MUA, manipulation under anesthesia; preop, preoperative; ROM, range of motion.
A radiographic analysis was performed on 23 of the 29 knees (79%). Two knees (9%) were noted to have significant polyethylene wear throughout the duration of this study. Osteolysis was noted in 3 knees (13%). Of the 5 patients that were noted to have polyethylene wear or osteolysis, 4 were revised. Only one patient was noted to have growth plates present at the time of the TKA. This patient had no evidence of polyethylene wear, osteolysis, or coronal or sagittal malalignment consistent with a growth arrest or angular deformity (Table 4).
Table 4.
Patient radiographic data.
| Most recent radiograph (years from index surgery) | Polywear | Osteolysis | Malalignment (coronal and sagittal) | Comments |
|---|---|---|---|---|
| 2.2 | No | No | No | Growth plates present at time of surgery |
| 2.2 | No | No | No | |
| 4.5 | No | No | No | |
| 5.7 | No | No | No | |
| 2.0 | No | No | No | |
| 5.1 | No | No | No | |
| 2.3 | No | No | No | |
| 5.5 | No | No | No | |
| 1.8 | No | No | No | |
| 5.4 | No | No | No | |
| 16.4 | No | No | No | Reimplanted for infection at 17 y from index surgery |
| 16.4 | No | Yes | No | Lucency around femoral component, revised for osteolysis at 9 y from index surgery |
| 20.3 | No | No | No | |
| 20.3 | Yes | No | No | Wear of the medial compartment, moderate pain |
| 15.5 | No | No | No | |
| 14.3 | No | No | No | |
| 20.3 | No | Yes | No | Osteolysis of femoral component, no pain at last follow-up |
| 19.8 | No | No | No | |
| 19.8 | No | No | No | |
| 22.6 | No | Yes | No | Lucency around the patella, has some grinding sensations, had poly exchange at 12 y from index surgery |
| 22.6 | Yes | No | No | Mild wear lateral compartment, had poly exchange at 12 y from index surgery |
| 5.4 | No | No | No | |
| 5.1 | No | No | No |
Discussion
Adolescent TKA is a rare procedure and comprises only 0.09% of the TKA patient population at our institution. Due to the paucity of cases, published long-term outcome data in this patient population is essentially nonexistent. Our goal was to determine the long-term outcomes in adolescent patients undergoing TKA, review the complication rates, and determine notable trends in this unique patient population.
Inflammatory arthritis has been previously described as one of the most common preoperative diagnoses in adolescent patients undergoing TKA [3], [5], [6]. We also identified inflammatory arthritis as the most common preoperative diagnosis leading to TKA in adolescent patients. Interestingly, we noted that most of our TKAs performed in this patient population were in the 1980s and 1990s, with only 3 in the 2000s and none since. This drastic decrease shares a temporal relationship with the release of the biologic disease modifying antirheumatic drugs, which were introduced in the late 1990s. None of our patients that underwent TKA with a preoperative diagnosis of inflammatory arthritis had been on these medications before surgery. It is likely that the widespread use of these biologic agents has greatly impacted the incidence of patients with inflammatory arthritis requiring a TKA at a young age.
Long-term outcomes were good in this cohort with a 10-year implant survivorship of 94% which is similar to implant survivorships in the adult patient population [7]. One patient had revision of all components at approximately 16 years secondary to an infection. Another patient had both knees revised secondary to aseptic loosening at 5 and 11 years. Another patient died 21 years postoperatively at the age of 41 secondary to unrelated causes. At final follow-up, one patient had radiographic evidence of osteolysis; however 4 knees were revised for aseptic loosening during the study. Therefore, while the overall 10-year implant survival rates were high, several of the failures occurred after 10 years. This is an important point as this patient population is substantially younger than most patients undergoing primary TKA and therefore will require several revisions throughout their lifetimes.
The most common complication was stiffness. Four patients required manipulation secondary to continued postoperative stiffness that had failed physical therapy and a trial of bracing. Stiffness in this patient population is likely multifactorial. The patients who developed stiffness had severe preoperative gonarthrosis and significant preoperative flexion contractures. The decrease in range of motion may have been directly related to the preoperative deformity or could be related to overstuffing of the joint in this adolescent patient population with adult sized implants. In addition, given the young patient age and increased functional demands, decreased range of motion may be poorly tolerated, leading to a lower threshold for intervention.
Only one patient in our series had open physes at the time of surgical intervention. This patient was a 14-year-old female that underwent bilateral TKAs secondary to steroid induced AVN. A discussion was held with the patient with regard to the risk of physeal arrest secondary to use of standard intramedullary femoral guides. The risk was felt to be minimal given the patient's age and size of the intramedullary guide. However, in a younger patient population extramedullary guides would be a consideration to avoid any potential complications associated with disrupting the growth plate. One additional physeal consideration pertains to the anterior phalange of the implant. The anterior phalange crosses the anterior portion of the growth plate and could theoretically act as a tether leading to a recurvatum deformity (Fig. 2).
Figure 2.
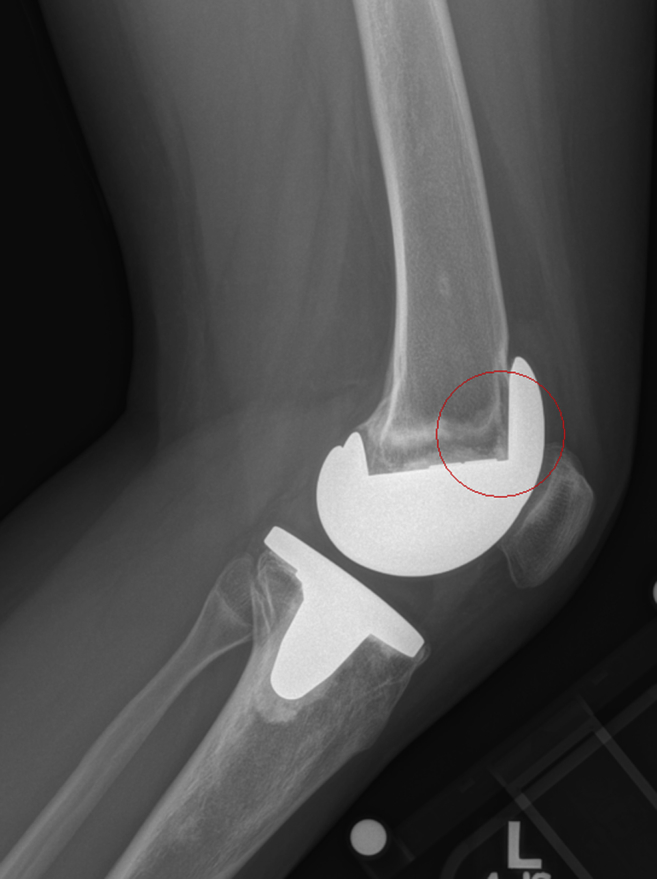
The anterior phalange crosses the anterior portion of the growth plate and could theoretically act as a tether leading to a recurvatum deformity.
There are only a few studies that include patients under the age of 20 that have undergone TKA. One recent study specifically examined patients 21 and younger with both total hip arthroplasty and TKA. The TKA population included a majority (77%) of patients with a preoperative diagnosis of tumor. The authors did not comment on the types of implants present in this patient population. However, it is likely that these patients required a distal femoral replacement and would have been excluded from our study. In addition, they included a 4-year implant revision rate of 4.6%. They did not mention complication rates, radiographic analysis, or patient outcomes in this study. Several other studies have examined limited outcomes in mixed patient populations which include adolescent patients as well [6], [8], [9].
There are several limitations of this study. This was a retrospective case study and, therefore, suffers the inherent limitations of the study design. In addition, this study includes a relatively small patient population with midterm follow-up. However, even with 19 patients, it remains one of the largest published series on the topic. Finally, we had only one patient with growth plates present at the time of surgery. For this reason, we are unable to comment on the impact of joint replacement surgery on growth disturbance or growth arrest.
Conclusions
Adolescent TKA is a rarely performed surgical intervention. Based on our limited data, the midterm outcomes, and perioperative complications appear to be similar to the adult patient population with a 10-year implant survivorship of 95%. Our patient population had excellent pain relief and functional outcomes at midterm follow-up. However, several of the failures occurred after 10 years and it is likely that 20-year implant survivorship will be substantially lower. After exploring all nonoperative treatment modalities, TKA may be a reasonable option in a select subpopulation of well-informed adolescent patients. Finally, we noted a drastic decrease in the number of TKA performed in adolescent patients with inflammatory arthritis which appears to be temporally related to the introduction of biologic rheumatoid medications.
Footnotes
One or more of the authors of this paper have disclosed potential or pertinent conflicts of interest, which may include receipt of payment, either direct or indirect, institutional support, or association with an entity in the biomedical field which may be perceived to have potential conflict of interest with this work. For full disclosure statements refer to http://dx.doi.org/10.1016/j.artd.2016.04.002.
Appendix A. Supplementary data
Conflict of Interest Statement for Martin
References
- 1.Palmer D.H., Mulhall K.J., Thompson C.A., Severson E.P., Santos E.R., Saleh K.J. Total knee arthroplasty in juvenile rheumatoid arthritis. J Bone Joint Surg Am. 2005;87(7):1510. doi: 10.2106/JBJS.D.02200. [DOI] [PubMed] [Google Scholar]
- 2.Parvizi J., Lajam C.M., Trousdale R.T., Shaughnessy W.J., Cabanela M.E. Total knee arthroplasty in young patients with juvenile rheumatoid arthritis. J Bone Joint Surg Am. 2003;85-A(6):1090. doi: 10.2106/00004623-200306000-00017. [DOI] [PubMed] [Google Scholar]
- 3.Cage D.J., Granberry W.M., Tullos H.S. Long-term results of total arthroplasty in adolescents with debilitating polyarthropathy. Clin Orthop Relat Res. 1992;283:156. [PubMed] [Google Scholar]
- 4.Sedrakyan A., Romero L., Graves S. Survivorship of hip and knee implants in pediatric and young adult populations: analysis of registry and published data. J Bone Joint Surg Am. 2014;96(Suppl 1):73. doi: 10.2106/JBJS.N.00541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carmichael E., Chaplin D.M. Total knee arthroplasty in juvenile rheumatoid arthritis. A seven-year follow-up study. Clin Orthop Relat Res. 1986;(210):192. [PubMed] [Google Scholar]
- 6.Boublik M., Tsahakis P.J., Scott R.D. Cementless total knee arthroplasty in juvenile onset rheumatoid arthritis. Clin Orthop Relat Res. 1993;(286):88. [PubMed] [Google Scholar]
- 7.Diduch D.R., Insall J.N., Scott W.N., Scuderi G.R., Font-Rodriguez D. Total knee replacement in young, active patients. Long-term follow-up and functional outcome. J Bone Jt Surg Am. 1997;79(4):575. doi: 10.2106/00004623-199704000-00015. [DOI] [PubMed] [Google Scholar]
- 8.Thomas A., Rojer D., Imrie S., Goodman S.B. Cemented total knee arthroplasty in patients with juvenile rheumatoid arthritis. Clin Orthop Relat Res. 2005;(433):140. doi: 10.1097/01.blo.0000151440.81939.c5. [DOI] [PubMed] [Google Scholar]
- 9.Sarokhan A.J., Scott R.D., Thomas W.H., Sledge C.B., Ewald F.C., Cloos D.W. Total knee arthroplasty in juvenile rheumatoid arthritis. J Bone Joint Surg Am. 1983;65(8):1071. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Conflict of Interest Statement for Martin


