Abstract
Background
Hip and knee arthroplasty aims to restore the joint function and to improve health-related quality of life (HRQoL) in patients with articular damage. It is important to quantify the HRQoL improvement and when this is achieved. The Oxford knee score and the Oxford hip score were developed to evaluate patients after knee and hip arthroplasty. We sought to evaluate HRQoL changes in the short and mid term following either primary or revision hip and knee arthroplasty.
Methods
Prospective cohort study during a 20-month period (August 2013 to March 2015) in a tertiary referral hospital. Primary arthroplasties secondary to osteoarthritis and any-cause revisions were included (328, 160 knees, and 88 hips). They were divided into 4 groups: (1) primary knee replacement, (2) primary hip replacement, (3) revision knee replacement, and (4) revision hip replacement. Oxford knee and hip scores were obtained prior the surgery and compared with the short- and mid-term follow-up scores.
Results
Follow-up in the short term and mid term was: 75.6% and 67.4%, respectively. Improvement was found in both short-term and mid-term follow-up for each group and for the overall group in HRQoL as measured by the Oxford knee and hip scores (P < .001). The greatest improvement was seen in the short term with an increase of 21 points for primary knee arthroplasty; 24 points for primary hip arthroplasty; 22 points for revision knee arthroplasty; and 23 points for revision hip arthroplasty.
Conclusions
Improvement in HRQoL in patients following primary or revision hip or knee arthroplasty is crucial and can be achieved early after the surgery.
Keywords: Hip arthroplasty, Knee arthroplasty, Quality of life
Introduction
Hip and knee osteoarthritis (OA) are frequent chronic degenerative conditions that usually cause pain and physical disability, thus altering health-related quality of life (HRQoL) [1], [2]. Its increasing prevalence and its growing impact on public health may prove critical for health systems in the near future [3]. Arthroplasties are common orthopaedic procedures to treat OA that emerged in the last century as a cost-effective alternative to conservative management [4], [5], [6], [7], [8]. As an elective surgery, it is necessary, however, to assess, with a quantitative instrument, joint functionality restoration and improvement in HRQoL, which are the main patient-related outcomes of interest after an arthroplasty.
Aside from the technical aspects of arthroplasties that have been the focus of outcome assessment for many years in orthopaedics, patient-reported outcome measures (PROMs) now play an increasingly important role in the determinants of clinical success, these providing valuable information regarding HRQoL and patient satisfaction after the intervention. HRQoL is, however, only one part of overall quality of life, which corresponds to the physical, psychological, and social factors that affect the overall health condition of an individual. It is, therefore, important to keep in mind that this component can provide information on only one chapter of a complete quality of life assessment.
Currently, in hip and knee replacement patients, HRQoL is evaluated through different scores and questionnaires, meaning that there is a lack of uniformity, which makes it challenging to understand the diverse literature [9], [10]. Most of these tests have been validated and show proven reproducibility [11], [12], [13]; however, research shows that hip and knee replacement patients prefer pen-and-paper questionnaires to other types of questionnaires [14]. The Oxford knee score (OKS) and Oxford hip score (OHS) are short and practical pen-and-paper tests which were developed to assess patient perspectives of HRQoL outcomes following a hip or knee arthroplasty [15], [16]. The OKS has also been validated in outpatients with knee OA [17]. These scores have shown reliability in different languages [18], [19], [20], [21].
Clinical consensus recommends that the optimal time point to start assessing PROMs is within the first 6 months post surgery [22]; and it is well known that changes in HRQoL could be achieved at this point and, later, after surgery [22], [23], [24], [25]. There is scarce information of PROMs using OKS and OHS before the first 6-month period. We sought, therefore, to evaluate whether significant improvement could be achieved in an earlier follow-up stage for overall hip and knee arthroplasties, in the primary and revision subgroups using OKS and OHS.
Material and methods
A prospective cohort study was performed at a tertiary referral hospital in Cali, Colombia, during a 20-month period between August 2013 and March 2015. Enrolled patients were obtained from the Hip and Knee Arthroplasty Registry prospective cohort at Fundacion Valle del Lili. The hospital ethics committee and its institutional review board approved the study protocol and the Arthroplasty Registry used.
All patients undergoing hip or knee arthroplasty (primary or revision) in the hospital during the study period were included in the registry, and in this study. Prior to their arthroplasty, patients included in the registry were asked to complete the OKS or OHS questionnaire to assess their levels of pain and disability over the previous 4 weeks for the specific symptomatic joint. The OKS and OHS are 12-item multiple-choice questionnaires, giving a score from 0 to 4 for each question, thus giving a range that goes from 0 for the worst joint status to 48 for a normal joint. Only patients with OA were included; other indications of arthroplasty such as musculoskeletal cancer, acute femoral neck fracture, and periprosthetic fractures were excluded. These groups were excluded because in these patients, the HRQoL assessment by the OKS or OHS might be not affected, given their other conditions, leading to an asymptomatic state for their hip or knee prior to the surgery; furthermore, the validation of this score in such groups of patient is unknown.
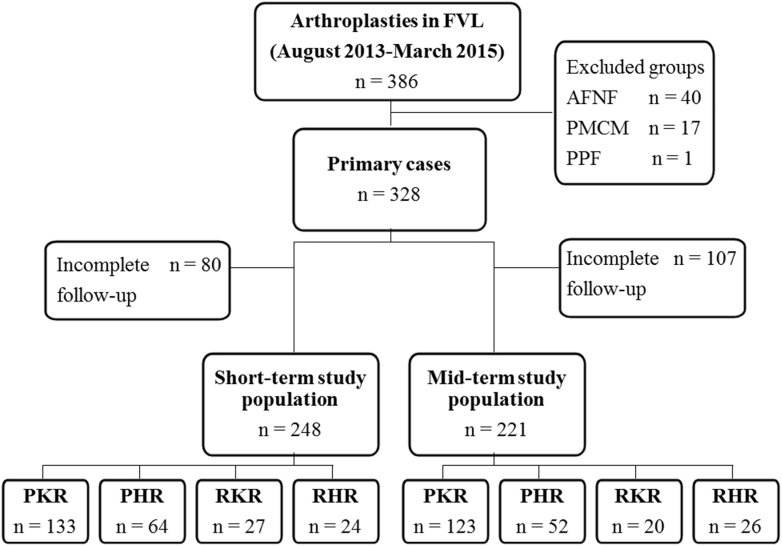
Enrolled patients were divided into 4 groups regarding the type of arthroplasty performed: (1) primary knee replacement (PKR); (2) primary hip replacement (PHR); (3) revision knee replacement (RKR); and (4) revision hip replacement (RHR). Figure 1 shows the study population and its distribution. Patients were assessed in 2 periods: the first was named the short-term follow-up, which was defined as the period between 2 and 6 months after the surgery; and the second was named the mid-term follow-up, which was defined as the period between 10 and 14 months after the surgery.
Figure 1.
Study population. FVL, Fundación Valle del Lili Joint Registry; AFNF, acute femoral neck fracture; PMCM, primary musculoskeletal cancer or metastasis; PPF, periprosthetic fracture; PKR, primary knee replacement; PHR, primary hip replacement; RKR, revision knee replacement; RHR, revision hip replacement.
During the short-term and mid-term follow-up periods, patients were asked to complete the OKS/OHS during each visit at the consulting room. Patients that missed the appointment in this period of time were called on their contact telephone and were assessed by phone. Before including a patient in the lost to follow-up group, at least 5 different attempts of contacting them by telephone were made. Any patient who had undergone an arthroplasty and who then assisted for a limb amputation or revision of their prosthesis, or who died, was excluded from the follow-up assessments and was therefore excluded from the statistical analyses. Furthermore, patients lost to follow-up were also excluded from the analysis. Demographic and additional study variables were obtained from the Arthroplasty Registry. The main study outcome was to compare the initial OKS/OHS with the short- and mid-term follow-up scores for the overall group and for each study group.
Descriptive analysis of the variables was performed. Categorical variables were summarized as absolute frequencies and percentages. Continuous variables were summarized as mean ± standard deviation or median (interquartile range), and they were compared using parametric tests (paired t test) or nonparametric tests (Wilcoxon rank-sum test) according to their distribution. Box plots were used to display patterns of quantitative data. Values of P < .05 were used to indicate statistical significance. All statistical analyses were performed using STATA 13.0 software.
Results
During the 20-month study period, a total of 386 arthroplasties were performed at the institution. Of these, 58 arthroplasties met the exclusion criteria: 40 acute femoral neck fractures, 17 primary musculoskeletal cancer or metastasis, and 1 periprosthetic fracture. A total of 328 arthroplasties were therefore initially included. For the short-term analysis, 80 additional patients were excluded from the analysis because of loss to follow-up (n = 77), prosthesis revision (n = 2), and patient death (n = 1), for the mid-term analysis, 37 more were excluded from analysis, for loss at follow-up (n= 32), prosthesis revision (n = 3), patient death (n = 2), and limb amputation (n= 1). Finally, 248 arthroplasties were included for the short-term analysis and 221 for the mid-term follow-up analysis, giving a 76%/67% response rate for the short-term and mid-term analyses, respectively. Of the included arthroplasties for the short-term follow-up analysis, 197 (79%) were primary arthroplasties (133 [68%] PKR and 64 [32%] PHR) and 51 (21%) were revision arthroplasties (27 [53%] RKR and 24 [47%] RHR). For the mid-term follow-up analysis, 175 (79%) were primary arthroplasties (123 [70%] PKR and 52 [30%] PHR) and 46 (21%) were revision arthroplasties (20 [43%] RKR and 26 (57%) RHR) (Fig. 1).
For all the primary arthroplasties, the only surgical indication was OA. For hip revision arthoplasty, the principal indication was loosening (55.6%), followed by infection (25.9%), instability (14.8%), and arthrofibrosis (3.7%); and for knee revision, the first cause was loosening (50.0%), followed by infection (33.5%), instability (8.3%), osteolysis (4.1%), and polyethylene wear (4.1%). Mean times for OKS/OHS follow-up assessment are detailed in Table 1, for each group and follow-up stage. Table 1 also describes patient characteristics for those patients included in the study for short- and mid-term follow-up.
Table 1.
Patient characteristics.
| Hip and knee arthroplasties with complete short-term follow-up | |||||
|---|---|---|---|---|---|
| Variable | Overall (n = 248) | PKR (n = 133) | PHR (n = 64) | RKR (n = 27) | RHR (n = 24) |
| Age, mean (SD) | 66.6 (12.5) | 70 (9.0) | 63 (14.9) | 62.4 (11.9) | 63.5 (12.2) |
| Female, n (%) | 174 (70%) | 108 (81%) | 35 (55%) | 15 (56%) | 16 (67%) |
| BMI, mean (SD) | 28.2 (4.8) | 29 (4.7) | 26.1 (4.4) | 29.5 (4.6) | 26.4 (4.1) |
| Days to follow-up, mean (SD) |
135 (57.3) |
135 (62.7) |
131.7 (47.3) |
137.5 (54.8) |
146 (54.2) |
| Hip and knee arthroplasties with complete mid-term follow-up | |||||
| Variable |
Overall (n = 221) |
PKR (n = 123) |
PHR (n = 52) |
RKR (n = 20) |
RHR (n = 26) |
| Age, mean (SD) | 66.6 (12.7) | 70.4 (9.0) | 62.5 (15.2) | 62.8 (13.0) | 60 (15.9) |
| Female, n (%) | 159 (72%) | 99 (81%) | 32 (62%) | 12 (60%) | 16 (62%) |
| BMI, mean (SD) | 28 (4.8) | 28.9 (4.7) | 26.1 (4.6) | 29.9 (5.4) | 25.9 (3.8) |
| Days to follow-up, mean (SD) | 408.3 (56.6) | 400.8 (61.4) | 416.2 (47.7) | 418.6 (58.8) | 419.5 (44.6) |
BMI, body mass index; SD, standard deviation; PKR, primary knee replacement; PHR, primary hip replacement; RKR, revision knee replacement; RHR, revision hip replacement.
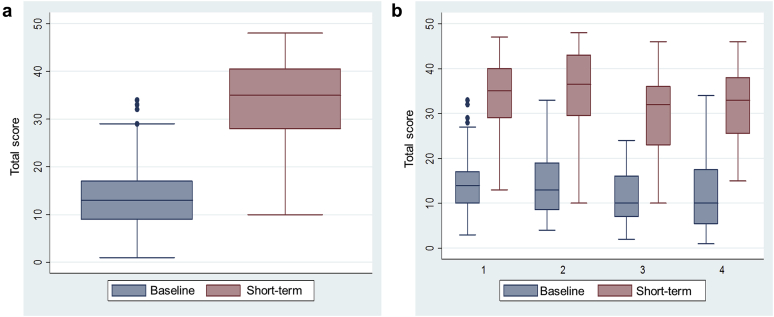
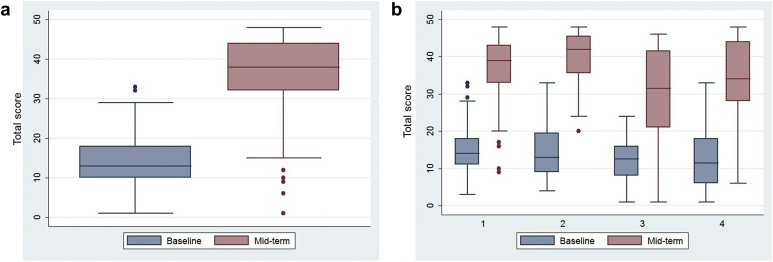
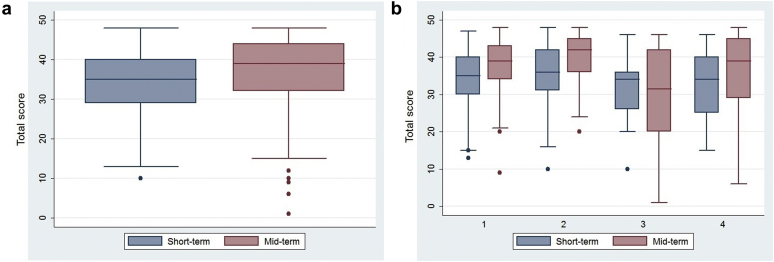
The OKS and OHS mean scores for the overall group and subgroups are shown in Table 2 for the baseline, short-term, and mid-term stages. Comparisons were made between baseline score and short-term score, baseline and mid-term scores, and between short-term and mid-term scores (Figure 2, Figure 3, Figure 4). The OKS and OHS mean scores changed significantly over time. For primary knee arthroplasty, the Oxford median score increased by 21 points at the short-term measurement point and by 25 points at mid term. For primary hip arthroplasty, Oxford median score increased by 24 points at the short-term measurement point and by 29 points at mid term. For revision knee arthroplasty, Oxford median score increased by 22 points at the short-term measurement point and by 19 points at mid term. Finally, for revision hip arthroplasty, Oxford median score increased by 23 points at the short-term measurement point and by 22 points at mid term. Comparisons between baseline short-term and baseline mid-term scores were statistically significant for the overall arthroplasties and for each individual study group (P < .001; Table 2).
Table 2.
Comparisons between presurgery, short-term, and mid-term follow-up in Oxford knee and hip scores (median).
| Group | Presurgery Median (interquartile range) |
Short term Median (interquartile range) |
Mid term Median (interquartile range) |
P valuea |
|---|---|---|---|---|
| Presurgery vs short term | ||||
| Overall (n = 248) | 13 (9-17) | 35 (28-41) | — | <.001 |
| PKR (n = 133) | 14 (10-17) | 35 (29-40) | — | <.001 |
| PHR (n = 64) | 13 (9-19) | 37 (30-43) | — | <.001 |
| RKR (n = 27) | 10 (7-16) | 32 (23-36) | — | <.001 |
| RHR (n = 24) | 10 (6-18) | 33 (26-38) | — | <.001 |
| Presurgery vs mid term | ||||
| Overall (n = 221) | 13 (10-18) | — | 38 (32-44) | <.001 |
| PKR (n = 123) | 14 (11-18) | — | 39 (33-43) | <.001 |
| PHR (n = 52) | 13 (9-20) | — | 42 (36-46) | <.001 |
| RKR (n = 20) | 13 (8-16) | — | 32 (21-42) | <.001 |
| RHR (n = 26) | 12 (6-18) | — | 34 (28-44) | <.001 |
| Short term vs mid term | ||||
| Overall (n = 187) | — | 35 (29-40) | 39 (32-44) | <.001 |
| PKR (n = 105) | — | 35 (30-40) | 39 (34-43) | <.001 |
| PHR (n = 45) | — | 36 (31-42) | 42 (36-45) | <.001 |
| RKR (n = 18) | — | 34 (26-36) | 32 (20-42) | .631 |
| RHR (n = 19) | — | 34 (25-40) | 39 (29-45) | .135 |
PKR, primary knee replacement; PHR, primary hip replacement; RKR, revision knee replacement; RHR, revision hip replacement.
Wilcoxon rank-sum test.
Figure 2.
Box-plot diagram comparing presurgery vs short-term Oxford knee score/Oxford hip score follow-up. Box plots show the interquartile range (box), median values (horizontal line inside the box), 10th/90th percentile values (whiskers), and outlier values (dots). (a) Overall comparison. (b) Subgroup comparisons by type of arthroplasties. Group 1: PKR, primary knee replacement; group 2: PHR, primary hip replacement; group 3: RKR, revision knee replacement; group 4: RHR, revision hip replacement.
Figure 3.
Box-plot diagram comparing presurgery vs mid-term Oxford knee score/Oxford hip score follow-up. (a) Overall comparison. (b) Subgroup comparisons by type of arthroplasties. Group 1: PKR, primary knee replacement; group 2: PHR, primary hip replacement; group 3: RKR, revision knee replacement; group 4: RHR, revision hip replacement.
Figure 4.
Box-plot diagram comparing short-term vs mid-term Oxford knee score/Oxford hip score follow-up. (a) Overall comparison. (b) Subgroup comparisons by type of arthroplasties. Group 1: PKR, primary knee replacement; group 2: PHR, primary hip replacement; group 3: RKR, revision knee replacement; group 4: RHR, revision hip replacement.
These results can be interpreted more easily when they are normalized to a scale from 0 to 100 and when the short-term and mid-term measurement points are expressed in mean time in months. When comparing patients, the baseline results may change between comparisons, according to the participants included in the analysis. The results are as follows:
-
•
Overall group: from baseline (27.1%) to 4.5 months (72.9%) and from baseline (27.1%) to 13.6 months (79.2%).
-
•
PKR: from baseline (29.2%) to 4.5 months (72.9%) and from baseline (29.2%) to 13.4 months (81.2%).
-
•
PHR: from baseline (27.1%) to 4.4 months (77.1%) and from baseline (27.1%) to 13.9 months (87.5%).
-
•
RKR: from baseline (20.8%) to 4.6 months (66.7%) and from baseline (27.1%) to 14.0 months (66.7%).
-
•
RHR: from baseline (20.8%) to 4.9 months (68.8%) and from baseline (25.0%) to 14.0 months (70.8%).
Arthroplasties with complete short- and mid-term follow-up (n = 187) were also analyzed to observe the differences in OKS and OHS between the short- and the mid-term follow-up (Fig. 4). The improvement according to OKS and OHS between the short-term and mid-term scores was statistically significant for primary replacements (P < .001) but not for revision replacements (Table 2). Actually, for RKR, there was a nonsignificant decrease in OKS between short and mid term.
Discussion
Results are consistent with short-term HRQoL improvement after hip and knee arthroplasties. This improvement continues more gradually into the mid term, demonstrating that most important changes are observed during the first few months. Both, primary and revision arthroplasties showed similar scores in the short term, but in the mid term, no additional significant improvements were observed for the revision groups. This can be related to the smaller numbers for the mid-term follow-up for revision replacements. Scores, such as the Oxford knee and hip scores, may have a ceiling effect in the mid and long term, as is probably shown in the scores from the revision arthroplasties [1], [22], [23].
These results confirm that most important changes in HRQoL occur during early stages after the surgery for all arthroplasty groups; moreover we demonstrated that this improvement could be evidenced as early as in the first few months after the surgery. Other studies have shown improvement at 6 months after surgery [26], [27], consistent with our results, but to our knowledge, this is the first study to show improvement before the 6-month period. This new fact helps to understand the natural history of these procedures and what expectations may be offered to the patient in the short term and mid term. The group of patients with the most improvement, for both the short term and mid term, was the PHR group. This is especially important when compared to the PKR group, where improvement is not as good, consistent with previous studies [1].
Patient perceptions and self-reported HRQoL scores are critical in PROMs assessments. It has been demonstrated that higher patient baseline expectations for total joint replacement are related to better HRQoL outcomes. In conjunction with the HRQoL assessment, the clinician could also measure other PROM outcomes with the hope of achieving better results in the short and mid term [28], [29].
The assessment of HRQoL following a hip or knee arthroplasty has further concerns. Interpreting changes in HRQoL remains challenging. The clinician must correctly correlate the patient’s environment and perspective, clinical factors, and social/economic burden with PROMs in order to fully interpret the result in each case [10]. Despite the difficulties, comparing the change in the median for a group of patients gives a general idea of what is happening with patients, which is valuable. In the case of this study, a significant trend toward improvement was found.
As discussed, arthroplasties have good results, in terms of improvements on the HRQoL, in the short and mid term. In the case of this cohort, we still have to wait for longer follow-up results in order to evaluate the long-term results, which we expect may show that the improvement is maintained over time, as has been shown in other studies [30]. Long-term follow-up, in our study, could confirm the duration of the effect of this improvement in HRQoL and would allow an exploration of a possible ceiling effect.
The limitations of this study include the exclusion from the analysis of participants whose prosthesis failed and those patients who required a revision or a limb amputation. These exclusion criteria led to the exclusion of 2 patients for the short-term follow-up and 4 for the mid-term follow-up. Follow-up was above 75% in the short term but it decreased to 67% in the mid term; this could introduce bias in the overall results. Patients could not attend for their follow-up for various reasons: because, for example, they felt well and decided not to come back as they felt they did not need any follow-up or, conversely, perhaps because they felt so bad that they decided to change their doctor. There are, additionally, 2 well-known problems that commonly arise in Colombia that can affect follow-up. The first problem is administrative changes at the patient’s insurance company, which can mean that the patient is later assigned to a different health facility; and the second is that patients frequently change their cell phone numbers. It is very challenging, because of these problems, to improve the follow-up percentages, as discussed in other publications [10]. In the current study, we actually have good follow-up percentages; other studies using PROMs have, for example, presented similar problems with follow-up at 6 months of 59% and at 2 years of 37% [25].
Conclusions
Significant improvement of patients HRQoL is achieved following either a primary or revision hip/knee arthroplasty. Most important HRQoL enhancement is observed during earlier stages (4-5 months) and continues during the mid term (12-14 months). HRQoL can be assessed earlier than 6 months after the surgery demonstrating significant changes. Among studied arthroplasties, PHR has the highest impact in HRQoL.
Acknowledgments
The authors thank Helen Louise Reina for her help in the final edition of the manuscript.
Footnotes
No author associated with this paper has disclosed any potential or pertinent conflicts which may be perceived to have impending conflict with this work. For full disclosure statements refer to http://dx.doi.org/10.1016/j.artd.2016.09.008.
Appendix A. Supplementary data
References
- 1.Ethgen O., Bruyere O., Richy F., Dardennes C., Reginster J.Y. Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg Am. 2004;86-A:963. doi: 10.2106/00004623-200405000-00012. [DOI] [PubMed] [Google Scholar]
- 2.Jones C.A., Beaupre L.A., Johnston D.W., Suarez-Almazor M.E. Total joint arthroplasties: current concepts of patient outcomes after surgery. Rheum Dis Clin North Am. 2007;33(1):71. doi: 10.1016/j.rdc.2006.12.008. [DOI] [PubMed] [Google Scholar]
- 3.Lawrence R.C., Felson D.T., Helmick C.G. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008;58:26. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kurtz S., Ong K., Lau E. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 5.Liang M.H., Cullen K.E., Larson M.G. Cost-effectiveness of total joint arthroplasty in osteoarthritis. Arthritis Rheum. 1986;29(8):937. doi: 10.1002/art.1780290801. [DOI] [PubMed] [Google Scholar]
- 6.Rissanen P., Aro S., Sintonen H. Costs and cost-effectiveness in hip and knee replacements. A prospective study. Int J Technol Assess Health Care. 1997;13:575. doi: 10.1017/s0266462300010059. [DOI] [PubMed] [Google Scholar]
- 7.Losina E., Walensky R.P., Kessler C.L. Cost-effectiveness of total knee arthroplasty in the United States: patient risk and hospital volume. Arch Intern Med. 2009;169:1113. doi: 10.1001/archinternmed.2009.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chang R.W., Pellisier J.M., Hazen G.B. A cost-effectiveness analysis of total hip arthroplasty for osteoarthritis of the hip. JAMA. 1996;275(11):858. [PubMed] [Google Scholar]
- 9.Riddle D.L., Stratford P.W., Bowman D.H. Findings of extensive variation in the types of outcome measures used in hip and knee replacement clinical trials: a systematic review. Arthritis Rheum. 2008;59(6):876. doi: 10.1002/art.23706. [DOI] [PubMed] [Google Scholar]
- 10.Singh J., Sloan J.A., Johanson N.A. Challenges with health-related quality of life assessment in arthroplasty patients: problems and solutions. J Am Acad Orthop Surg. 2010;18(2):72. [PMC free article] [PubMed] [Google Scholar]
- 11.Bellamy N., Buchanan W.W., Goldsmith C.H., Campbell J., Stitt L.W. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J. Rheumatol. 1988;15:1833. [PubMed] [Google Scholar]
- 12.Lequesne M.G., Mery C., Samson M., Gerard P. Indexes of severity for osteoarthritis of the hip and knee. Validation – value in comparison with other assessment tests. Scand J Rheumatol. 1987;65(Suppl):85. doi: 10.3109/03009748709102182. [DOI] [PubMed] [Google Scholar]
- 13.Roos E.M., Roos H.P., Ekdahl C., Lohmander L.S. Knee injury and Osteoarthritis Outcome Score (KOOS) – validation of a Swedish version. Scand J Med Sci Sports. 1988;8:439. doi: 10.1111/j.1600-0838.1998.tb00465.x. [DOI] [PubMed] [Google Scholar]
- 14.Keurentjes J.C., Fiocco M., So-Osman C. Hip and knee replacement patients prefer pen-and-paper questionnaires: Implications for future patient-reported outcome measure studies. Bone Joint Res. 2013;2(11):238. doi: 10.1302/2046-3758.211.2000219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dawson J., Fitzpatrick R., Carr A., Murray D. Questionnaire on the perceptions of patients about total hip replacement. J Bone Joint Surg Br. 1996;78-B:185. [PubMed] [Google Scholar]
- 16.Dawson J., Fitzpatrick R., Murray D., Carr A. Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg Br. 1998;80-B:63. doi: 10.1302/0301-620x.80b1.7859. [DOI] [PubMed] [Google Scholar]
- 17.Xie F., Ye H., Zhang Y. Extension from inpatients to outpatients: validity and reliability of the Oxford Knee Score in measuring health outcomes in patients with knee osteoarthritis. Int J Rheum Dis. 2011;14(2):206. doi: 10.1111/j.1756-185X.2010.01580.x. [DOI] [PubMed] [Google Scholar]
- 18.Jenny J.Y., Diesinger Y. Validation of a French version of the Oxford knee questionnaire. Orthop Traumatol Surg Res. 2011;97(3):267. doi: 10.1016/j.otsr.2010.07.009. [DOI] [PubMed] [Google Scholar]
- 19.Dunbar M.J., Robertsson O., Ryd L., Lidgren L. Translation and validation of the Oxford-12 item knee score for use in Sweden. Acta Orthop Scand. 2000;71:268. doi: 10.1080/000164700317411861. [DOI] [PubMed] [Google Scholar]
- 20.Takeuchi R., Sawaguchi T., Nakamura N. Cross-cultural adaptation and validation of the Oxford 12-item knee score in Japanese. Arch Orthop Trauma Surg. 2011;131(2):247. doi: 10.1007/s00402-010-1185-1. [DOI] [PubMed] [Google Scholar]
- 21.Naal F.D., Impellizzeri F.M., Sieverding M. The 12-item Oxford Knee Score: cross-cultural adaptation into German and assessment of its psychometric properties in patients with osteoarthritis of the knee. Osteoarthr Cartil. 2009;17:49. doi: 10.1016/j.joca.2008.05.017. [DOI] [PubMed] [Google Scholar]
- 22.Browne J.P., Bastaki H., Dawson J. What is the optimal time point to assess patient-reported recovery after hip and knee replacement? A systematic review and analysis of routinely reported outcome data from the English patient-reported outcome measures programme. Health Qual Life Outcomes. 2013;11:128. doi: 10.1186/1477-7525-11-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Marx R.G., Jones E.C., Atwan N.C. Measuring improvement following total hip and knee arthroplasty using patient-based measures of outcome. J Bone Joint Surg Am. 2005;87(9):1999. doi: 10.2106/JBJS.D.02286. [DOI] [PubMed] [Google Scholar]
- 24.Jenny J.Y., Diesinger Y. The Oxford Knee Score: compared performance before and after knee replacement. Orthop Traumatol Surg Res. 2012;98(4):409. doi: 10.1016/j.otsr.2012.03.004. [DOI] [PubMed] [Google Scholar]
- 25.Xie F., Lo N.N., Pullenayegum E.M. Evaluation of health outcomes in osteoarthritis patients after total knee replacement: a two-year follow-up. Health Qual Life Outcomes. 2010;8:87. doi: 10.1186/1477-7525-8-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fortin P.R., Clarke A.E., Joseph L. Outcomes of total hip and knee replacement: preoperative functional status predicts outcomes at six months after surgery. Arthritis Rheum. 1999;42(8):1722. doi: 10.1002/1529-0131(199908)42:8<1722::AID-ANR22>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 27.Johansson H.R., Bergschmidt P., Skripitz R. Impact of preoperative function on early postoperative outcome after total hip arthroplasty. J Orthop Surg (Hong Kong) 2010;18(1):6. doi: 10.1177/230949901001800102. [DOI] [PubMed] [Google Scholar]
- 28.Gonzalez Sáenz de Tejada M., Escobar A., Herrera C. Patient expectations and health-related quality of life outcomes following total joint replacement. Value Health. 2010;13(4):447. doi: 10.1111/j.1524-4733.2009.00685.x. [DOI] [PubMed] [Google Scholar]
- 29.Gonzalez Saenz de Tejada M., Escobar A., Bilbao A. A prospective study of the association of patient expectations with changes in health-related quality of life outcomes, following total joint replacement. BMC Musculoskelet Disord. 2014;15:248. doi: 10.1186/1471-2474-15-248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bruyère O., Ethgen O., Neuprez A. Health-related quality of life after total knee or hip replacement for osteoarthritis: a 7-year prospective study. Arch Orthop Trauma Surg. 2012;132(11):1583. doi: 10.1007/s00402-012-1583-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.