Abstract
Pericardial cysts are rare with an incidence of about 1 in every 100,000 persons and one in 10 pericardial cysts may actually be a pericardial diverticulum. Pericardial cysts and diverticula share similar developmental origin and may appear as an incidental finding in chest roentgenogram in an asymptomatic patient. CT scan is considered as best modality for diagnosis and delineation of the surrounding anatomy. Cardiac MRI is recommended in the evaluation of the compressive effects caused by the pericardial cysts. The authors recommend echocardiography for serial follow up and image guided aspiration of the pericardial cyst in presence of compressive effects leading to cardiovascular and airway symptoms. A systematic approach is desirable for management of pericardial cysts depending on size, shape and compression effects, symptoms and easy access to serial Echocardiographic follow up. However, pericardial diverticulum may not be differentiated from cysts by the above testing, and only identified at surgery.
Keywords: Pericardial cyst, Pericardial diverticulum, Pericardial coelomic cyst, Springwater cyst, Mesothelial cyst, Thin walled cyst, Algorithmic approach, Historical perspective
1. Introduction
Cystic lesions within the pericardial space are a rare entity and comprise 7% of the mediastinal masses and 33% of mediastinal cysts.1, 2 The incidence of a pericardial cyst is 1 in 100,000 populations and most of the pericardial cysts presenting as mediastinal opacity are detected incidentally.3, 4, 5, 6 They are usually found in the third or the fourth decade of the life and male and female are affected equally.5 In 70% of the cases, these cysts are located in right cardiophrenic angle, in 22% cases in the left cardiophrenic angle and in 8% cases are located in the posterior or the anterior-superior part of the mediastinum.7 Most of the cases (50–75%) are asymptomatic and are diagnosed incidentally during radiological investigations ordered as routine investigation for other causes of illness.6, 7, 8, 9, 10, 11 Symptoms may appear due to compression of the nearby structures, such as heart, great vessels, oesophagus and the tracheobronchial tree.11 Pericardial cysts are described in the medical literature under various terminologies like: le kyste pleuropericardique (Jeaubert de Beaujeu et al., 1945; Roche et al., 1954), pleural cyst, pericardial cyst, pericardial coelomic cyst (Lambert et al., 1940), springwater cyst (Greenfield et al., 1943), mesothelial cyst (Churchill and Mallory, 1937), and thin-walled cyst.12
2. History
Preliminary reports of pericardial cysts date back to middle of 19th century when the pathologists encountered the initial cases on post mortem examination.13 Advances in radiographic imaging made antemortem diagnosis possible and Le Roux et al. reported three cases in 300,000 people in a mass chest roentgenography campaign in Edinburgh in 1958.14 Progress in the field of thoracic surgery ushered a new era in management of these lesions and Otto Pickhardt et al. from Lenox Hill Hospital performed the first resection of pericardial cyst in New York in 193115 in a 53 year old woman. The first reported incidence of pericardial diverticulum was presented by T. Hart of the Park Street School of Medicine in Dublin, in 1837.16 Subsequently a new concept of origin of pericardial cysts and diverticula was proposed, according to which pericardial cysts and diverticula represent different stages of a lesion with a common embryonic origin. Greenfield et al. coined the term ‘springwater cysts’ because of the presence of thin, transparent cyst wall and crystal clear fluid content within the pericardial cyst.17 Surgical approach to the pericardial cysts and diverticula has undergone several refinements with the present evidence based medical diagnosis and treatment approach. Currently video assisted thoracoscopic surgery is considered as the most promising technique in the diagnosis and in the management of these lesions. A brief chronology of events in discovery and gradual evolution of different modalities of management is outlined in Table 1.
Table 1.
A brief chronology of events in discovery and gradual evolution of different modalities of management.
| Year | Events |
|---|---|
| 1837 | T. Hart of the Park Street School of Medicine in Dublin described the first case of a pericardial diverticulum on autopsy16 |
| 1903 | Rohn, from the Charles University of Prague first published a case series comprising of four diverticula and one cyst based on autopsy finding of these lesions. The interrelationship between pericardial diverticulum and cyst sharing a common embryonic origin was first recognised in this case series.23 |
| 1931 | Wallace Yater (Georgetown University) detailed the radiological appearance and the differential diagnosis of pericardial cysts25 |
| 1931 | Otto Pickhardt, at Lenox Hill Hospital in New York performed first surgical removal of pericardial cyst15 |
| 1937 | First pneumogram of pericardial cyst was performed by E. H. Cushing26 |
| 1940 | Adrian Lambert first suggested similar embryological origin of pericardial cyst and diverticula from disconnected mesenchymal lacunae, which later unite to form the pericardial coelom27 |
| 1943 | First resection of a pericardial diverticulum by Richard Sweet at Massachusetts General Hospital in Boston29 |
| 1943 | Greenfield et al introduced the term ‘Springwater cyst’17 |
| 1958 | Le Roux reported the incidence of three cases of pericardial cysts in 300,000 people in a mass X-ray campaign in Edinburgh14 |
3. Pericardial cyst and diverticula
Although radiologically a lesion may appear to be a pericardial cyst, in 10% of the time, it is actually a diverticulum.18 Although dissimilar on anatomical basis, both pericardial cyst and diverticula are considered as a sequelae of common embryogenesis going wrong and are usually discussed together by most embryologists.18, 19, 20, 21, 22, 23, 24 Pericardial cysts and diverticula usually arise due to herniation through a structural defect in the pericardium.19, 20 Rohn et al. first described similar origin of both the lesions and concluded that the pericardial cyst probably is a remnant of a diverticulum whose communication to the pericardial cavity has been obliterated.23 To assure that it is truly a “cyst”, it might be necessary to trace the communicating channels during dissection of the pericardial cysts and if found be ligated to prevent a diverticulum from reoccurring.18 Pericardial diverticula may be congenital or acquired. Congenital cases may result from a failure in the fusion of one of the mesenchymal lacunae that normally combine to form the pericardial sac. Acquired pericardial diverticula may be due to sequelae of pericardial diseases and effusion.18, 19, 20, 21, 22
4. Origin
Pericardial cysts are usually congenital in origin but other causes of origin of pericardial cysts have also been described in literature (Table 2). Pericardial cysts usually arise from failure of fusion of one of the mesenchymal lacunae that form the pericardial sac.5 Adrian Lambert suggested that the cyst and diverticulum embryologically originate from the disconnected mesenchymal lacunae which normally unite to form the pericardial coelom.27 Mazer described the fluid shift from pericardial diverticula to pericardial sac and attributed this as the cause of congestive chest symptoms and chest discomfort.28 Lillie et al. expounded the origin of the pericardial cysts by the concept of differential persistence and graded constriction of ventral recess of the pericardial coelom. Persistence of the ventral recess of the pericardial coelom forms the diverticulum, constriction of the proximal part of the persistent recess accounts for either a diverticulum with a narrow neck or results in the origin of a pericardial cyst in communication with the pericardial cavity and complete closure of the proximal recess forms the pericardial cyst.29 Prenatal diagnosis of pericardial cyst is made possible with ultrasound examination beyond 14th week of gestation.30 Cases of spontaneous regression of pericardial cysts have also been described in literature.31 Inflammatory cysts and pseudocysts appear due to loculated pericardial effusion.6 Isolated hydatid cyst of pericardium is extremely rare and they are usually found in association with myocardial cysts or hydatid cysts in the liver and the lungs.32, 33
Table 2.
Etiology of pericardial cyst.6
5. Clinical presentation
Patients with pericardial cysts are mostly asymptomatic (50–75% cases) 5, 6, 7, 8, 9, 10, 11 and the diagnosis is usually an incidental finding in chest X-ray. Symptoms usually appear when the cyst compresses on a nearby structure, or undergoes complications39, 40, 41, 42 (vide Table 5) . Common symptoms include chronic cough, chest pain, dyspnea and a feeling of retrosternal pressure.40, 41 Abdul- Mannan Masood et al. described a case of a large pericardial cyst (11 cm × 11 cm) in a patient presenting with right shoulder discomfort radiating to the left shoulder, with associated heaviness in the substernal area along with shortness of breath.43 Recurrent attacks of palpitation due to cardiac dysrrhythmias and frequent lower respiratory tract infections have been described in literature.5 Unusual presentations of pericardial cysts include recurrent syncope,44 pneumonia,45 congestive heart failure and sudden cardiac death.
Table 5.
| 1. Complication due to compression of surrounding structure | I. Cardiac compression39, 53, 54, 58, 59 |
| a. Compression of right side of heart with deviation of septum | |
| b. Diastolic dysfunction | |
| c. Right ventricular outflow tract obstruction | |
| d. Pulmonary stenosis | |
| e. Mitral valve prolapse | |
| f. Congestive heart failure | |
| II. Compression of lung: Obstruction of the right main stem bronchus, Compression of the adjacent lobes of the lung | |
| 2. Inflammation | Pericarditis60, Infected pericardial cyst61 |
| 3. Cardiac tamponade | May occur due to |
| I. Rupture into the pericardial sac62 | |
| II. Hemorrhage within the pericardial cyst39, 55, 56, 63 | |
| III. Hydatid pericardial cyst rupture64 | |
| 4. Sudden cardiac death65 | |
| 5. Others: | I. Atrial fibrillation66 |
| II. Erosion of the cyst into the superior vena cava and right ventricular wall | |
| III. Recurrent syncope44 | |
| IV. Pneumonia45 |
Patients with pericardial diverticula may have atypical symptoms that cannot be explained. There is typically no evidence of any compression of the adjacent surrounding structures. Symptoms may include intermittent chest discomfort, palpitations, tachycardia, worsening of symptoms at night associated with increased anxiety and restlessness. These symptoms may not correlate with activity. Nocturnal symptoms may be gravity dependent, possibly due to a shift of the fluid from the pericardium back into the pericardial sac, potentially causing a tamponade effect affecting venous return.18 Mazer28 first described this fluid shift in 1946 and Money reported a case with a pericardial diverticulum that had been misdiagnosed for 30 years as a cyst, wherein intermittent nocturnal symptoms resolved after surgical removal.18
Compression of the adjacent surrounding structures near the pericardium due to pericardial diverticula may produce myriad of symptoms including chest congestion and discomfort, palpitation during sleep at night, tachycardia, and restlessness. Such chest discomfort is position and gravity dependent and arising due to gravity dependent fluid shift between the pericardial sac and the cyst cavity. This fluid accumulation in the pericardial sac causes a tamponade like effect thereby obstructing venous return.18 Mazer28 first described this fluid shift in 1946 and Money18 has been attributed in successfully explaining the causes for these gravity dependent drainage of pericardial fluid leading to the positional symptoms in patients with pericardial diverticulum.
6. Diagnosis
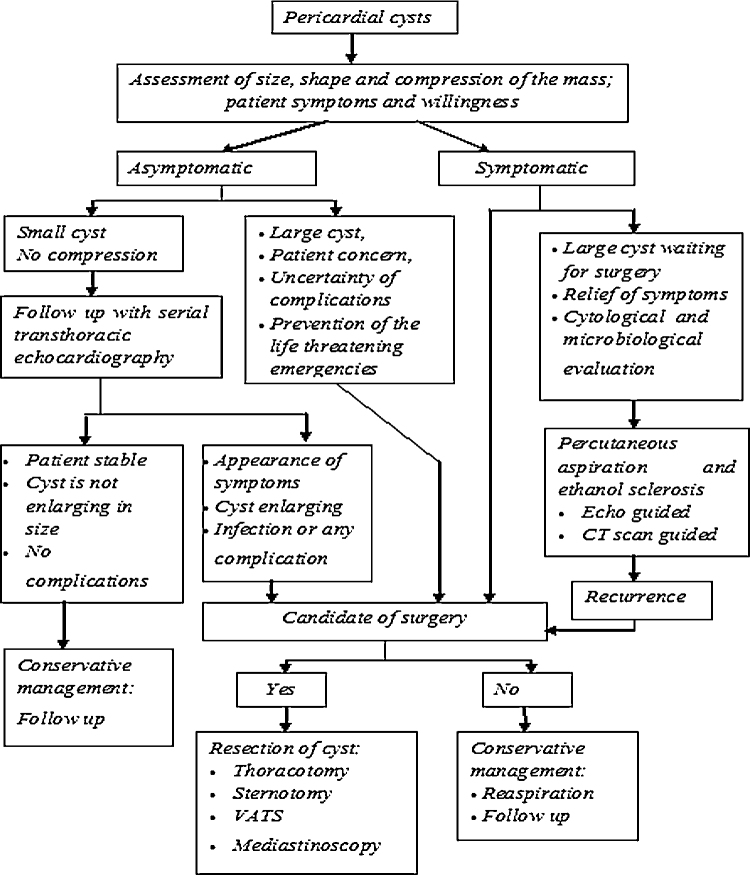
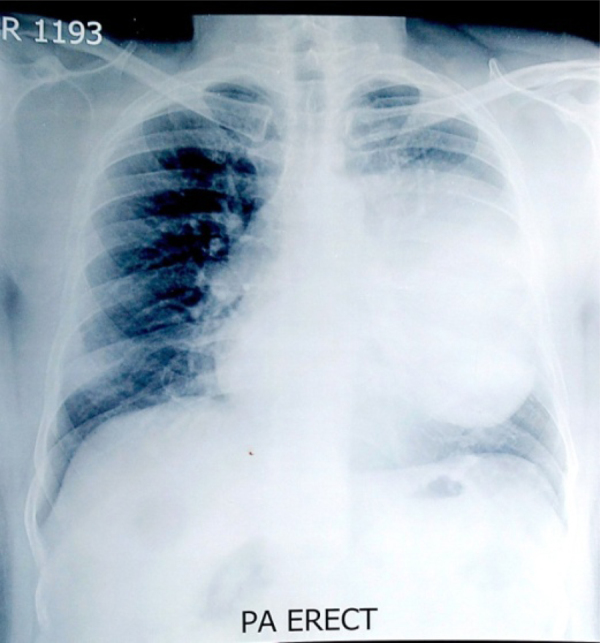
Most of the cases are diagnosed as an incidental finding in chest X-rays, as an isolated cystic shadow adjacent to the heart (Fig. 1). Differentiation of pericardial cysts from diverticula is usually impossible and poses a nightmare for the radiologist as both the lesions have similar radiological appearance. The lone differentiating feature is the presence of communicating tract between pericardium and the cyst cavity which is not usually recognized in any of the imaging modalities including CT scans, MRI, or echocardiography. Radiological appearance of pericardial cysts by different imaging modalities are depicted in Table 3. Computerised tomography scan (CT scan) (Fig. 2A & B) is considered as the best modality for the diagnosis as it provides an excellent delineation of the pericardial anatomy and can aid in the precise localization and characterization of various pericardial lesions, including effusion, pericardial thickening, pericardial masses, and congenital anomalies helping in surgical decision making.4, 46, 47 Inaccuracies in diagnosis arise when the cyst is in an unusual location, or the protein content of the cyst fluid is high.48, 49 Magnetic resonance imaging is a promising imaging modality and the fluid in the pericardial cyst produces a hyperintense signal on T2-weighted MRI images and hypointense signals on T1-weighted images.48 Elevated protein content may also distort MRI image as it decreases T2-weighted MRI signals and increases T1-weighted signals.48 This may make the differentiation of hematomas or neoplasms from pericardial cysts difficult. Diffusion weighted MRI may be helpful in selected cases. Echocardiography is useful for the assessment of functional status of the heart and follow up. Echocardiography is not preferred as primary diagnostic modality because of narrow window of visualization and pericardial cysts at unusual sites might be missed by this modality. Characteristic features of pericardial cyst in different modes of imaging along with their advantages and shortcomings are enumerated in Table 3 and differential diagnosis of pericardial cyst in relation to other lesions with radiological similarity is depicted in Table 4. Differentiating pericardial cysts from pericardial diverticulum is difficult as both the lesions have similar radiological findings. The lone differentiating feature is the presence of communicating tract between pericardium and the cyst cavity which is not usually recognised in any of the imaging modalities.
Fig. 1.
Chest X-ray showing huge pericardial cyst in the left hilum.
Table 3.
Imaging modalities in pericardial cyst.
| CT scan5, 47, 50, 51 |
|
|
|
| Lack of motion artefact- clear and sharp image Short acquisition time |
|
Radiation Lack of functional assessment Hypersensitivity reaction to iodinated contrast Need for breath holding |
|
| Cardiac MRI47, 23 |
|
|
|
|
Disadvantage: Time consuming High cost Altered signalling if cyst protein content is high Calcification less well visualised |
|
| Echocardiography31, 49 |
|
Low cost May be performed on unstable patients Diagnostic modality for follow up and image guided percutaneous aspiration |
|
Technical difficulties in case of obesity, obstructive lung disease or immediately post- cardiothoracic surgery Localisation of cyst at uncommon location difficult Operator dependent |
Fig. 2.
A& 2B. CT scan appearance of pericardial cyst.
Table 4.
Differential diagnosis of isolated cystic shadow adjacent to the heart.
| Lesion | Differentiating feature |
|---|---|
| Bronchial cysts: | Lined with bronchial epithelium46 |
| Localised pericardial effusion: | Fluid between visceral and parietal pericardium |
| Teratoma: | Usually associated with some solid components along with cystic components52 |
| Neuroenteric cyst: | Located in the right posterior chest and associated with vertebral anomalies31 |
| Lymphangioma: | Multilocular or multiple cysts31 |
| Congenital cysts of primitive foregut origin (bronchogenic cyst, gastroenteric cyst, and esophageal duplication cyst): | Usually located in posterior mediastinum and are lined by epithelium |
7. Complications
Pericardial cysts are usually benign but complications may arise eventually in case of compression of the structures adjacent to the heart, inflammation, haemorrhage or rupture of the cyst (Table 5). Compression of the right sided cardiac chambers may result in elevated venous pressures with engorged superficial veins of the upper and lower extremities, ascites, hepatomegally and may result in right sided heart failure.53 Pankaj Kaul et al.54 described a case of massive benign pericardial cyst in a 66 year old woman presenting with congestive chest symptoms and with features of right heart failure. Haemorrhage within the pericardial cyst cavity may occur spontaneously39, 55 or may result from external thoracic trauma.56
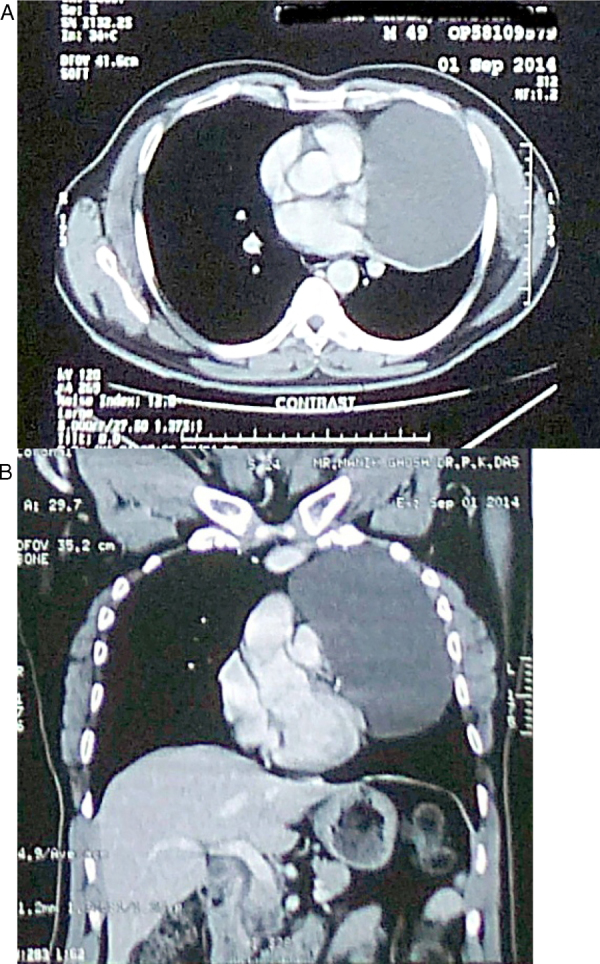
8. Management
Management of pericardial cyst is similar to that of mediastinal mass67 and should follow a systematic approach (Fig. 3). Management options include conservative management with follow up, percutaneous aspiration of the cyst and excision of the cyst. Data regarding safety of conservative management are scarce and frequent follow up with periodic imaging induces anxiety and stress in the mind of the patients and in addition increases treatment cost. Task force on the diagnosis and management of pericardial diseases of the European Society of Cardiology recommended percutaneous aspiration and ethanol sclerosis as initial treatment of congenital and inflammatory cysts.6 Video assisted thoracotomy or surgical resection were recommended as a second line management. Kinoshita et al.68 reported a case of a 41 year old patient treated with ethanol sclerosis and no recurrence was found at 6 months follow up. However data regarding safety, efficacy and long term follow up with this technique is inadequate to support this technique as a first line management option. The authors recommend a systematic approach for management of pericardial cysts, based on the presence or the absence of symptoms, size of the mass, and compression over the blood vessels, heart and airway. Surgery is recommended in symptomatic patients, large cysts, pericardial cysts with radiological features of compression or impending compression to vital structures and potential for malignant transformation.Surgery is also indicated for prevention of life threatening emergencies such as cardiac tamponade, obstruction of right main stem bronchus and sudden cardiac death. Video assisted thoracoscopic surgery (VATS) is associated with less blood loss, minimal incision and better wound healing, leading to early postoperative discharge. The authors prefer echocardiography over CT scan for follow up to minimize cumulative radiation exposure to the patient and recommend CT scan imaging in the postoperative period with suspected complications. Surgery may not be required in asymptomatic patients5, 69 and these patients will be under serial echocardiography follow up to detect any compressive effect of the cyst on vital structures, haemorrhage, infection or cyst rupture as outlined in Fig. 3.
Fig. 3.
Management algorithm of pericardial cyst.
N.B., VATS- Video assisted thoracoscopic surgery.
9. Conclusion
Pericardial cyst and diverticulum share similar developmental origin and may appear as an incidental finding in chest X-ray in an asymptomatic patient. The authors recommend CT scan as the diagnostic modality of choice in the preoperative period in all cases and diffusion weighted cardiac MRI for cases with diagnostic confusion. The authors recommend echocardiography for serial follow up in asymptomatic patient and image guided aspiration of the pericardial cyst in presence of compressive effects on adjacent vital structures leading to cardiovascular and airway symptoms. Management protocol of pericardial cysts is similar to that of a mediastinal mass. A systematic approach should be followed for management depending on size, shape and compressibility of the mass, patient symptoms, easy access to serial echocardiographic follow up and ability to tolerate anaesthesia related cardiovascular and airway perturbations. However, a pericardial diverticulum should be considered if a patient has unexplained recurrent symptoms and offered elective thoracic surgery.
Conflicts of interest
None.
References
- 1.Davis R.D., Jr., Oldham H.N., Jr., Sabiston D.C., Jr. Primary cysts and neoplasms of the mediastinum: recent changes in clinical presentation, methods of diagnosis, management, and results. Ann Thorac Surg. 1987;44(3):229–237. doi: 10.1016/s0003-4975(10)62059-0. [DOI] [PubMed] [Google Scholar]
- 2.Cohen A.J., Thompson L., Edwards F.H., Bellamy R.F. Primary cysts and tumors of the mediastinum. Ann Thorac Surg. 1991;51(March (3)):378–384. doi: 10.1016/0003-4975(91)90848-k. discussion 385-6. [DOI] [PubMed] [Google Scholar]
- 3.Unverferth D.V., Wooley C.F. The differential diagnosis of paracardiac lesions: pericardial cysts. Cathet Cardiovasc Diagn. 1979;5(1):31–40. doi: 10.1002/ccd.1810050105. [DOI] [PubMed] [Google Scholar]
- 4.Patel J., Park C., Michaels J., Rosen S., Kort S. Pericardial cyst: case reports and a literature review. Echocardiography. 2004;21(April (3)):269–272. doi: 10.1111/j.0742-2822.2004.03097.x. [DOI] [PubMed] [Google Scholar]
- 5.Elamin W.F., Hannan K. Pericardial cyst: an unusual cause of pneumonia. Cases J. 2008;1(July (1)):26. doi: 10.1186/1757-1626-1-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maisch B., Seferović P.M., Ristić A.D. Task Force on the diagnosis and management of pericardial diseases of the European Society of Cardiology. Guidelines on the diagnosis and management of pericardial diseases executive summary; the task force on the diagnosis and management of pericardial diseases of the european society of cardiology. Eur Heart J. 2004;25(April (7)):587–610. doi: 10.1016/j.ehj.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 7.Demos T.C., Budorick N.E., Posniak H.V. Benign mediastinal cysts: pointed appearance on CT. J Comput Assist Tomogr. 1989;13(January-February (1)):132–133. doi: 10.1097/00004728-198901000-00030. [DOI] [PubMed] [Google Scholar]
- 8.Patel J., Park C., Michaels J., Rosen S., Kort S. Pericardial cyst: case reports and a literature review. Echocardiography. 2004;21:269–272. doi: 10.1111/j.0742-2822.2004.03097.x. [DOI] [PubMed] [Google Scholar]
- 9.Yared K., Baggish A.L., Picard M.H., Hoffmann U., Hung J. Multimodality imaging of pericardial diseases. JACC Cardiovasc Imaging. 2010;3:650–660. doi: 10.1016/j.jcmg.2010.04.009. [DOI] [PubMed] [Google Scholar]
- 10.Bezgin T., Elveran A., Varol S., Doğan C., Karagöz A., Esen A.M. Pericardial cyst. Herz. 2014;39:1005–1007. doi: 10.1007/s00059-013-3933-9. [DOI] [PubMed] [Google Scholar]
- 11.Saldaña Dueñas C., Hernández Galán A. Posttraumatic pericardial cyst. An Sist Sanit Navar. 2015;38(September-December (3)):475–478. doi: 10.4321/s1137-66272015000300015. [DOI] [PubMed] [Google Scholar]
- 12.De Roover P., Maisin J., Laquet A. Congenital pleuro-pericardial cysts. Thorax. 1963;18(June (2)):146–150. doi: 10.1136/thx.18.2.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schweigert M., Dubecz A., Beron M., Ofner D., Stein H.J. The tale of spring water cysts: a historical outline of surgery for congenital pericardial diverticula and cysts. Tex Heart Inst J. 2012;39(3):330–334. [PMC free article] [PubMed] [Google Scholar]
- 14.Le Roux B.T. Pericardial coelomic cysts. Thorax. 1959;14(1):27–35. doi: 10.1136/thx.14.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pickhardt O.C. Pleuro-diaphragmatic cyst. In: transactions of the new York surgical society-stated meeting held april 12, 1933. Ann Surg. 1934;99(5):814–816. [PMC free article] [PubMed] [Google Scholar]
- 16.Hart T. An account of hernia pericardii. Dublin J Med Sci. 1837;11(3):365–367. [Google Scholar]
- 17.Greenfield L., Steinberg L., Touroff A.S.W. Spring water cyst of the mediastinum. J Thorac Surg. 1943;12:495–502. [Google Scholar]
- 18.Money M.E., Park C. Pericardial diverticula misdiagnosed as pericardial cysts. J Thorac Cardiovasc Surg. 2015;149(June (6)):e103–e107. doi: 10.1016/j.jtcvs.2015.01.032. Epub 2015 Jan 21. [DOI] [PubMed] [Google Scholar]
- 19.Carretta A., Negri G., Pansera M., Melloni G., Zannini P. Thoracoscopic treatment of a pericardial diverticulum. Surg Endosc. 2003;17(January (1)):158. doi: 10.1007/s00464-002-4241-2. Epub 2002 Oct 29. [DOI] [PubMed] [Google Scholar]
- 20.Peebles C.R., Shambrook J.S., Harden S.P. Pericardial disease–anatomy and function. Br J Radiol. 2011;84(December) doi: 10.1259/bjr/16168253. Spec No 3:S324-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maier H.C. Diverticulum of the pericardium with observations on mode of development. Circulation. 1957;16(December (6)):1040–1045. doi: 10.1161/01.cir.16.6.1040. [DOI] [PubMed] [Google Scholar]
- 22.Rajiah P. Cardiac MRI: part 2, pericardial diseases. Am J Roentgenol. 2011;197:W621–W634. doi: 10.2214/AJR.10.7265. [DOI] [PubMed] [Google Scholar]
- 23.Rohn A. Ueber divertikel-und cystenbildung am perikard [in German] Prag Med Wochschr. 1903;28:461–464. [Google Scholar]
- 24.Schweigert M., Dubecz A., Beron M., Ofner D., Stein H.J. The tale of spring water cysts: a historical outline of surgery for congenital pericardial diverticula and cysts. Tex Heart Inst J. 2012;39(3):330–334. [PMC free article] [PubMed] [Google Scholar]
- 25.Yater W.M. Cyst of the pericardium. Am Heart J. 1931;6(5):710–712. [Google Scholar]
- 26.Cushing E.H. Diverticulum of the pericardium. Arch Intern Med. 1937;59(1):56–64. [Google Scholar]
- 27.Lambert A.V.S. Etiology of thin-walled thoracic cysts. J Thorac Surg. 1940;10(1):1–7. [Google Scholar]
- 28.Mazer M.L. True pericardial diverticulum; report of a case, with safe operative removal. Am J Roentgenol Radium Ther. 1946;55:27–29. [PubMed] [Google Scholar]
- 29.Lillie W.I., McDonald J.R., Clagett O.T. Pericardial celomic cysts and pericardial diverticula; a concept of etiology and report of cases. J Thorac Surg. 1950;20(3):494–504. [PubMed] [Google Scholar]
- 30.Lewis K.M., Sherer D.M., Gonçalves L.F., Fromberg R.A., Eglinton G.S. Mid-trimester prenatal sonographic diagnosis of a pericardial cyst. Prenat Diagn. 1996;16:549–553. doi: 10.1002/(SICI)1097-0223(199606)16:6<549::AID-PD879>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 31.Bernasconi A., Yoo S.J., Golding F., Langer J.C., Jaeggi E.T. Etiology and outcome of prenatally detected paracardial cystic lesions: a case series and review of the literature. Ultrasound Obstet Gynecol. 2007;29:388–394. doi: 10.1002/uog.3963. [DOI] [PubMed] [Google Scholar]
- 32.Dasbaksi K., Haldar S., Mukherjee K., Mukherjee P. A rare combination of hepatic and pericardial hydatid cyst and review of literature. Int J Surg Case Rep. 2015;10:52–55. doi: 10.1016/j.ijscr.2015.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kosecik M., Karaoglanoglu M., Yamak B. Pericardial hydatid cyst presenting with cardiac tamponade. The Canadian Journal of Cardiology. 2006;22(2):145–147. doi: 10.1016/s0828-282x(06)70254-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vural M., Sayin B., Pasaoglu L., Koparal S., Elverici E., Dede D. Isolated pericardial hydatid cyst in an asymptomatic patient: a remark on its radiologic diagnosis. Clin Imaging. 2007;31(January-February (1)):37–39. doi: 10.1016/j.clinimag.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 35.Narin N., Meşe T., Unal N., Pinarli S., Cangar S. Pericardial hydatid cyst with a fatal course. Acta Paediatr Jpn. 1996;38(February (1)):61–62. doi: 10.1111/j.1442-200x.1996.tb03437.x. [DOI] [PubMed] [Google Scholar]
- 36.Guven A., Sokmen G., Yuksel M., Kokoglu O.F., Koksal N., Cetinkaya A. A case of asymptomatic cardiopericardial hydatid cyst. Jpn Heart J. 2004;45(May (3)):541–545. doi: 10.1536/jhj.45.541. [DOI] [PubMed] [Google Scholar]
- 37.Patel J., Park C., Michaels J., Rosen S., Kort S. Pericardial cyst: case reports and a literature review. Echocardiography. 2004;21(April (3)):269–272. doi: 10.1111/j.0742-2822.2004.03097.x. [DOI] [PubMed] [Google Scholar]
- 38.Pugliatti P., Donato R., Crea P., Zito C., Patanè S. Image diagnosis: pericardial cyst in a dialysis patient. J Cardiovasc Ultrasound. 2016;24(June (2)):177–178. doi: 10.4250/jcu.2016.24.2.177. Epub 2016 Jun 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Borges A.C., Gellert K., Dietel M., Baumann G., Witt C. Acute right-sided heart failure due to hemorrhage into a pericardial cyst. Ann Thorac Surg. 1997;63(March (3)):845–847. doi: 10.1016/s0003-4975(96)01373-2. [DOI] [PubMed] [Google Scholar]
- 40.Sokouti M., Halimi M., Golzari S.E.J. Pericardial cyst presented as chronic cough: a rare case report. Tanaffos. 2012;11(4):60–62. [PMC free article] [PubMed] [Google Scholar]
- 41.Mejía Lozano P., Pérez Ortiz E., Puchaes Manchón C. Cardiac tamponade due to a pleuropericardial cyst with invasive lung cancer. Arch Bronconeumol. 2010;46(December (12)):658–659. doi: 10.1016/j.arbres.2009.12.003. 10.10.1016/j.arb Ann Thorac Surg. 1996 Jan;61(1):208-10. [DOI] [PubMed] [Google Scholar]
- 42.Satur C.M., Hsin M.K., Dussek J.E. Giant pericardial cysts. Ann Thorac Surg. 1996;61(January (1)):208–210. doi: 10.1016/0003-4975(95)00720-2. [DOI] [PubMed] [Google Scholar]
- 43.Masood A.-M., Ali O.M., Sequeira R. A hiding in the lining: painful pericardial cyst. BMJ Case Reports. 2013;2013 doi: 10.1136/bcr-2013-008618. bcr2013008618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ilhan E., Altin F., Ugur O. An unusual presentation of pericardial cyst: recurrent syncope in a young. Cardiol J. 2012;19(2):188–191. doi: 10.5603/cj.2012.0032. patient. [DOI] [PubMed] [Google Scholar]
- 45.Forouzandeh F., Krim S.R., Bhatt R., Abboud L.N., Ramchandani M., Chang S.M. Giant Pericardial Cyst Presenting as Pneumonia. In: Stainback R.F., editor. Texas Heart Institute Journal; 2012. pp. 296–297. 39 (2) [PMC free article] [PubMed] [Google Scholar]
- 46.Lau C.L., Davis R.D. 17th ed. Vol. 1758. Elsevier; Philadelphia: 2004. Chapter 56: the mediastinum; pp. 1738–1739. (Sabiston’s Textbook of Surgery). [Google Scholar]
- 47.Wang Z.J., Reddy G.P., Gotway M.B., Yeh B.M., Hetts S.W., Higgins C.B. CT and MR imaging of pericardial disease. Radiographics. 2003;23(October):S167–S180. doi: 10.1148/rg.23si035504. Spec No:S167-80. [DOI] [PubMed] [Google Scholar]
- 48.Raja A., Walker J.R., Sud M. Diagnosis of pericardial cysts using diffusion weighted magnetic resonance imaging: a case series. J Med Case Rep. 2011;5:479. doi: 10.1186/1752-1947-5-479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jeung M.Y., Gasser B., Gangi A. Imaging of cystic masses of the mediastinum. Radiographics. 2002;22(October):S79–S93. doi: 10.1148/radiographics.22.suppl_1.g02oc09s79. Spec No:S79-93. [DOI] [PubMed] [Google Scholar]
- 50.Peebles C.R., Shambrook J.S., Harden S.P. Pericardial disease—anatomy and function. The British Journal of Radiology. 2011;84(Spec Iss 3):S324–S337. doi: 10.1259/bjr/16168253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Verhaert D., Gabriel R.S., Johnston D., Lytle B.W., Desai M.Y., Klein A.L. The role of multimodality imaging in the management of pericardial disease. Circ Cardiovasc Imaging. 2010;3(May (3)):333–343. doi: 10.1161/CIRCIMAGING.109.921791. [DOI] [PubMed] [Google Scholar]
- 52.de Bustamante T.D., Azpeitia J., Miralles M., Jiménez M., Santos-Briz A., Rodríguez-Peralto J.L. Prenatal sonographic detection of pericardial teratoma. J Clin Ultrasound. 2000;28(May (4)):194–198. doi: 10.1002/(sici)1097-0096(200005)28:4<194::aid-jcu8>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 53.Mwita J.C., Chipeta P., Mutagaywa R., Rugwizangoga B., Ussiri E. Pericardial cyst with right ventricular compression. Pan Afr Med J. 2012;12:60. [PMC free article] [PubMed] [Google Scholar]
- 54.Kaul P., Javangula K., Farook S.A. Massive benign pericardial cyst presenting with simultaneous superior vena cava and middle lobe syndromes. J Cardiothoracic Surg. 2008;3:32. doi: 10.1186/1749-8090-3-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Marigliano A., Cirio E.M., Versace R. Pericardial cyst with intracystic hemorrhage. A case report and review of the literature. G Ital Cardiol (Rome) 2010;11(June (6)):493–497. [PubMed] [Google Scholar]
- 56.Temizkan V., Onan B., Inan K., Ucak A., Yilmaz A.T. Hemorrhage into a pericardial cyst and associated right ventricular compression after blunt chest trauma. Ann Thorac Surg. 2010;89(April (4)):1292–1295. doi: 10.1016/j.athoracsur.2009.09.018. [DOI] [PubMed] [Google Scholar]
- 57.Najib M.Q., Chaliki H.P., Raizada A., Ganji J.L., Panse P.M., Click R.L. Symptomatic pericardial cyst: a case series. Eur J Echocardiogr. 2011;12(November (11)):E43. doi: 10.1093/ejechocard/jer160. Epub 2011 Sep 6. [DOI] [PubMed] [Google Scholar]
- 58.Martins I.M., Fernandes J.M., Gelape C.L., Braulio R., Silva Vde C., Nunes Mdo C. A large pericardial cyst presenting with compression of the right-side cardiac chambers. Rev Bras Cir Cardiovasc. 2011;26(July-September (3)):504–507. doi: 10.5935/1678-9741.20110032. [DOI] [PubMed] [Google Scholar]
- 59.Lesniak-Sobelga A.M., Olszowska M., Tracz W. Giant pericardial cyst compressing the right ventricle. Ann Thorac Surg. 2008;85(May (5)):1811. doi: 10.1016/j.athoracsur.2007.12.043. [DOI] [PubMed] [Google Scholar]
- 60.McMillan A., Souza C.A., Veinot J.P., Turek M., Hendry P., Alvarez G.G. A large pericardial cyst complicated by a pericarditis in a young man with a mediastinal mass. Ann Thorac Surg. 2009;88(August (2)):e11–e13. doi: 10.1016/j.athoracsur.2009.05.024. [DOI] [PubMed] [Google Scholar]
- 61.Hoque M., Siripurapu S. Methicillin-resistant Staphylococcus aureus-infected pericardial cyst. Mayo Clin Proc. 2005;80(September (9)):1116. doi: 10.4065/80.9.1116. [DOI] [PubMed] [Google Scholar]
- 62.El Hammoumi M.M., Sinaa M., El Oueriachi F., Arsalane A., Kabiri E.H. Pleuropericardial cyst rupturing into the pericardium causing tamponade. Rev Mal Respir. 2014;31(May (5)):442–446. doi: 10.1016/j.rmr.2013.08.004. Epub 2013 Oct 25. [DOI] [PubMed] [Google Scholar]
- 63.Shiraishi I., Yamagishi M., Kawakita A., Yamamoto Y., Hamaoka K. Acute cardiac tamponade caused by massive hemorrhage from pericardial cyst. Circulation. 2000;101(May (19)):E196–7. doi: 10.1161/01.cir.101.19.e196. [DOI] [PubMed] [Google Scholar]
- 64.Kumar Paswan A., Prakash S., Dubey R.K. Cardiac tamponade by hydatid pericardial cyst: a rare case report. Anesth Pain Med. 2013;4(December (1)):e9137. doi: 10.5812/aapm.9137. eCollection 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Fredman C.S., Parsons S.R., Aquino T.I., Hamilton W.P. Sudden death after a stress test in a patient with a large pericardial cyst. Am Heart J. 1994;127(April (4 Pt 1)):946–950. doi: 10.1016/0002-8703(94)90572-x. [DOI] [PubMed] [Google Scholar]
- 66.Generali T., Garatti A., Gagliardotto P., Frigiola A. Right mesothelial pericardial cyst determining intractable atrial arrhythmias. Interact Cardiovasc Thorac Surg. 2011;12(May (5)):837–839. doi: 10.1510/icvts.2010.261594. Epub 2011 Feb 8. [DOI] [PubMed] [Google Scholar]
- 67.Kar S.K., Ganguly T., Dasgupta C.S., Goswami A. Cardiovascular and airway considerations in mediastinal mass during thoracic surgery. J Clin Exp Cardiolog. 2014;5:354. [Google Scholar]
- 68.Kinoshita Y., Shimada T., Murakami Y. Ethanol sclerosis can be a safe and useful treatment for pericardial cyst. Clin Cardiol. 1996;19(October (10)):833–835. doi: 10.1002/clc.4960191015. [DOI] [PubMed] [Google Scholar]
- 69.Khandaker M.H., Espinosa R.E., Nishimura R.A. Pericardial disease: diagnosis and management. Mayo Clin Proc. 2010;85(6):572–593. doi: 10.4065/mcp.2010.0046. [DOI] [PMC free article] [PubMed] [Google Scholar]