Abstract
In clinical practice, dynamic left ventricular outflow tract obstruction (LVOTO) in the setting of tako-tsubo cardiomyopathy (TTC) has been regarded as an early-onset complication typically emerging in accordance with wall motion abnormalities. However, dynamic LVOTO has, very rarely, been reported as a late-onset phenomenon in the setting of TTC as well (arising in the late stage or after recovery). Accordingly, the present paper aims to highlight clinical relevance and potential implications of late-onset LVOTO in the setting of TTC.
Keywords: Tako-tsubo cardiomyopathy, Late-onset left ventricular outflow tract obstruction, Clinical implications
Tako-tsubo cardiomyopathy (TTC) has been considered as a unique form of reversible acute myocardial disease primarily characterized by a variety of spesific complications including dynamic left ventricular outflow tract (LVOT) obstruction.1, 2 In the setting of TTC, LVOT gradient is well known to present as an early-onset phenomenon arising simultaneously with wall motion abnormalities, and generally appears to be associated with significant hemodynamic compromise.2 On the other hand, dynamic LVOT obstruction in the setting of TTC was rarely reported as a late-onset pathology (during the late course or after convalascence) in a couple of previous reports as well.1, 3 However, the authors of these reports 1, 3 did not elaborate on potential pathogenesis or clinical implications of this rare phenomenon.
On the other hand, we and others previously suggested that TTC might have the potential to induce a variety of persistent or permanent alterations in left ventricle (LV) geometry (increased interventricular septal thickness, chamber dilatation etc.) that only appear to be of trivial significance in previously normal hearts.4 However, we also stated previously that these TTC-induced changes might elicit a variety of significant clinical presentations (late-onset LVOT gradient, aggravation of diastolic dysfunction and arrhythmogenesis etc.) in the setting of a pre-existing myocardial pathology including hypertrophic cardiomyopathy (HCM), hypertensive heart disease, etc.4 As expected, a certain period of time is essential for these geometric changes (and; hence for the occurence of these potential presentations) to evolve in the setting of TTC. In particular, TTC-induced late-onset LVOT gradient merits further attention with regard to its pathogenesis and spesific clinical characteristics, etc. More importantly, particular care should be given to differentiate this phenomenon from the early-onset counterpart since it potentially confers diagnostic, prognostic and therapeutic implications in clinical practice:
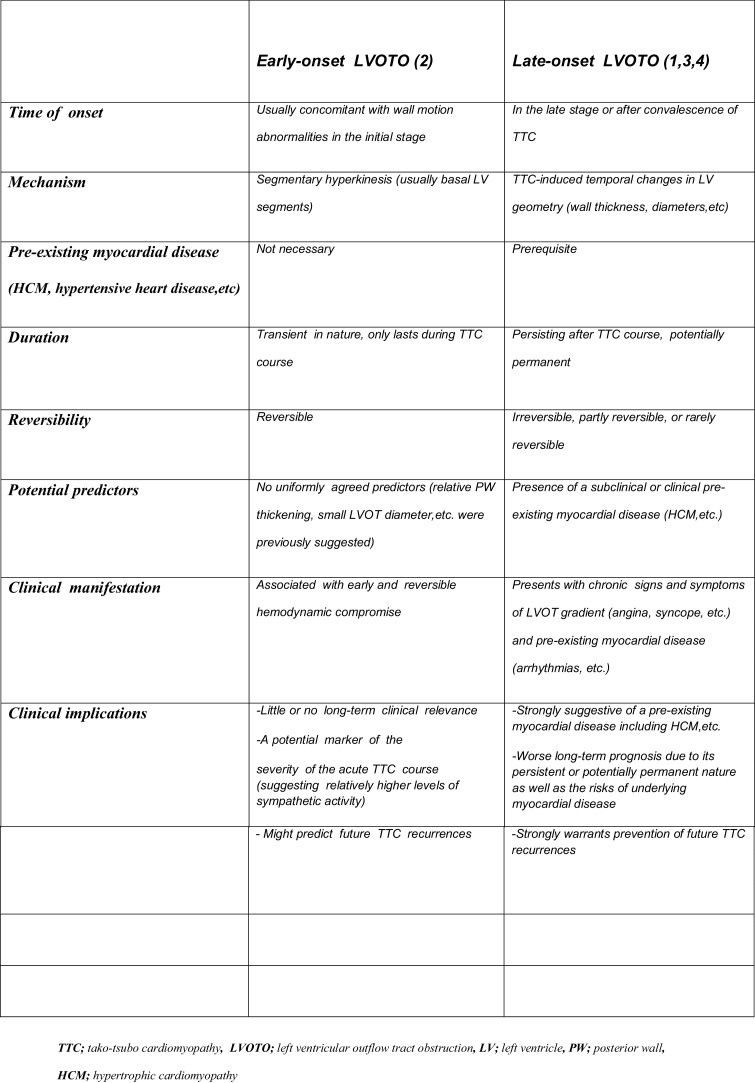
Firstly, potential occurence of this phenomenon in patients with TTC might potentially signify a pre-existing myocardial disease4 (even if echocardiographic findings remain inconclusive). Secondly, in contrast with early-onset LVOT gradient (with a transient nature and a limited prognostic relevance in the long-term2), late-onset LVOT gradient might portend a worse long- term prognosis due to its persistent or potentially permanent nature as well as inherent risks of pre-existing myocardial disease.4 Accordingly, sudden cardiac death (SCD) (due to sudden increases in LVOT gradient or ventricular arrhythmias associated with underlying myocardial disease) might be considered as the major complication among these patients in the long term. Thirdly, since any future TTC recurrences in patients with a late-onset LVOT gradient might have the potential to induce further alterations in LV geometry, and hence to intensify LVOT obstruction as well as arrhythmic risk,4 every effort should be made to prevent TTC recurrences. Within a therapeutic context, stress and anger management, a variety of yoga practices enhancing parasympathetic activity5 and prophylactic use of certain sympatholytic regimens including ganglion blockage, etc. might be of utmost clinical value for the prevention of TTC recurrences in patients with a late-onset LVOT gradient. Furthermore, percutaneous or surgical relief of LVOT gradient may be necessary in a portion of severely symptomatic cases despite avoidence of certain tiggers (hypovolemia, anemia etc.) and optimal medical therapy.3 A comparison of clinical characteristics and potential implications of early and late-onset LVOT obstructions in the setting of TTC is presented in Fig. 1.
Fig. 1.
Early versus late-onset dynamic left ventricular outflow tract gradient in the setting of tako- tsubo cardiomyopathy (TTC). TTC; tako-tsubo cardiomyopathy, LVOTO; left ventricular outflow tract obstruction, LV; left ventricle, PW; posterior wall, HCM; hypertrophic cardiomyopathy.
In conclusion, late-onset LVOT gradient may be considered as an extremely rare and poorly understood entity with different clinical characteristics and implications in comparison to classical early-LVOT obstruction in the setting of TTC. However, further studies are warranted to illuminate the clinical relevance of this interesting phenomenon in patients with TTC.
References
- 1.Fu H., Jiao Z., Chen K., Liu T., Li G. Dynamic left ventricular outflow tract obstruction in recovery process of stress cardiomyopathy. Int J Cardiol. 2016;30(March (214)):202–203. doi: 10.1016/j.ijcard.2016.03.152. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 2.Kawaji T., Shiomi H., Morimoto T. Clinical impact of left ventricular outflow tract obstruction in takotsubo cardiomyopathy. Circ J. 2015;79(4):839–846. doi: 10.1253/circj.CJ-14-1148. [DOI] [PubMed] [Google Scholar]
- 3.Akita K., Maekawa Y., Tsuruta H. Moving left ventricular obstruction due to stress cardiomyopathy in a patient with hypertrophic obstructive cardiomyopathy treated with percutaneous transluminal septal myocardial ablation. Int J Cardiol. 2016;202(January (1)):194–195. doi: 10.1016/j.ijcard.2015.08.145. [DOI] [PubMed] [Google Scholar]
- 4.Yalta K., Yılmaztepe M., Ozkalaycı F., Ucar F. Tako-tsubo cardiomyopathy may lead to permanent changes in left ventricular geometry: potential implications in the setting of pre-existing myocardial disease. Int J Cardiol. 2016;202:889–891. doi: 10.1016/j.ijcard.2015.10.022. [DOI] [PubMed] [Google Scholar]
- 5.Yalta K., Sivri N., Yetkin E. Sahaja yoga: a unique adjunctive approach for the management of cardiac arrhythmias? Int J Cardiol. 2011;152(1):99–100. doi: 10.1016/j.ijcard.2011.07.004. [DOI] [PubMed] [Google Scholar]