Abstract
INTRODUCTION:
This study presents a novel technique to perform cholecystectomy and assess its outcome and feasibility.
PATIENTS AND METHODS:
This study presents the novel Dhillon technique and experience of hybrid natural orifice transluminal endoscopic surgery (NOTES) technique, that is, laparoscopic-assisted transvaginal cholecystectomy. We have evaluated the outcomes in terms of cosmesis, post-operative recovery and analgesic requirement. The study included 257 patients who underwent hybrid NOTES cholecystectomy at single tertiary hospital. The biographical data, surgical time, pain score on day 1 and 2, need of analgesia, intra- and post-operative complication and aesthetic assessment on day 7 were recorded.
RESULTS:
Out of a total of 1100 cases of laparoscopic cholecystectomy 257 had hybrid NOTES cholecystectomy. Only two of these cases were converted to standard laparoscopic cholecystectomy. The mean operative time was 31.5 ± 5.1 (25–40) min. None of the patients had any complication or biliary leakage. The mean pain score on day 1 and 2 was 3.6 ± 0.4 (3–4) and 1.0 ± 0.06 (1–2), respectively. The mean paracetamol (analgesic) dose requirement was 6.1 ± 0.6 (4–6.9) g. The aesthetic score was excellent in all the cases.
CONCLUSIONS:
Using the present technique of hybrid NOTES is beneficial in terms of cosmetic results, lesser need of analgesic and shorter hospital stay.
Keywords: Cholecystectomy, laparoscopy, natural orifice transluminal endoscopic surgery
INTRODUCTION
Kurt Semm first used laparoscopy for removal of an appendix in 1981.[1] However, with the passage of time, the technique has evolved. The advantages of laparoscopy include decreased post-operative pain, increased peri-operative ambulation resulting in reduced hospital stay and faster return to routine activities. The ultimate goal of laparoscopic surgery is to decrease access trauma by minimising the number of abdominal incisions.[2,3]
The technique of entry to peritoneum/retroperitoneum through natural orifices using flexible or rigid instruments and with or without additional transabdominal route is called natural orifice transluminal endoscopic surgery (NOTES).[4,5] Day by day NOTES surgery is getting refined and standardised. The ‘access port’ related technical difficulties have been overcome. The first transvaginal cholecystectomy (TVC) in a human being was carried out in 2003 at the Mount Sinai Hospital by Tsin et al., utilising rigid laparoscopic instruments and minimal abdominal assistance.[6] With NOTES multiple incisions in the abdominal wall for entry into the cavity is minimised/avoided. The greatest advantage with NOTES is ability of retrieval of the specimen, without requiring classical retrieval incision. Bulian et al. evaluated role of NOTES in cholecystectomy and reported decrease in pain scale and post-operative hospital stay compared to classical laparoscopic technique.[7] In the present prospective report, we present our experience of hybrid technique, that is, laparoscopic assisted TVC.
PATIENTS AND METHODS
The study was carried out at the Department of Advanced Laparoscopy and General Surgery, Max Super Speciality Hospital, Mohali, India from January 2012 to September 2015. Patients <65 years of age and body mass index (BMI) <35 underwent cholecystectomy by NOTES technique. Patients with severe acute cholecystitis, vaginitis or active pelvic infection were excluded from the study. The study was approved by the Department Review Committee and was conducted in accordance with Declaration of Helsinki. Written informed consent was obtained from all patients.
The biographical data, surgical time, pain score on day 1 and 2, need of analgesia, intra- and post-operative complication and aesthetic assessment on day 7 were recorded.
Surgical technique
A gynaecologist pre-operatively evaluated all patients scheduled for Hybrid NOTES. In patients with no contraindication for hybrid NOTES, under general anaesthesia subjects were placed in Lithotomy position after emptying the urinary bladder. Umbilicus was inspected and incision of 5 mm was given under upper margin of umbilicus. The first port was made with safety trocar 5 mm inserted through the superior incision by closed method with a safety trocar. After insertion, pneumoperitoneum was induced with CO2. The peritoneal cavity was inspected with 5 mm 30° laparoscope to assess the feasibility of procedure. The pouch of Douglas (POD) inspected to rule out Pelvic adhesions. To proceed with the surgery second 5 mm incision was given under the lower margin of umbilicus. Then, second 5 mm trocar was inserted through the lower incision. Each incision was given at the upper and lower margin in the skin crease along the lines of Langerhans inside the Umbilicus [Figure 1]. A soft bowel grasper is inserted through the second port. Under vision 10 mm long metallic/bariatric trocar cannula is inserted through vagina in the POD. Long bariatric telescope is put through vaginal port under vision and thereafter the camera and light source is shifted to the vaginal telescope [Figure 2]. The Cholecystectomy was performed through two umbilical ports with grasper in the left hand and Maryland connected to unipolar cautery on the right hand. Only two instruments are used to dissect out the gall bladder (GB). The dissection of Calot's triangle and the division and sealing of cystic artery and duct were carried out. The GB was then mobilised from the liver. The specimen was retrieved through vagina under vision. The GB is held at cystic duct end and the thinner end is taken into post, then the GB is pulled along with the port outside. In case of a large calculi, the vaginal access is dilated bluntly with a long artery forceps. Final inspection of the GB fossa and the Pelvis was done byagain inserting a 5 mm telescope from the Umbilical port [Figure 2]. The posterior fornix was sutured with vicryl 2.0. After securing haemostasis camera and instrument were removed. Since the ports size was 5 mm rectus sheath was not sutured. No suture was taken in skin as well. As the incision is in the skin crease the margins of incision get approximated. Plain gauze dressing was done at umbilicus, which was removed on post-operative day 3–5. Skin approximation and umbilical shape was retained as is in pre-operative state [Figure 3]. Patients were allowed full oral nutrition 4 h after extubation, and they were fully mobilised on the same day of surgery in the evening. Patients were discharged either the same day or next day in the morning. Standardised analgesics schedule: 1 g paracetamol, initially (intravenous) and then every 8 hourly until the morning of the 1st post-operative day and afterwards orally as tablets. In case of an NAS ≥5, diclofenac 75 mg was given intravenous in 100 ml normal saline. In case of nausea, 4 mg ondansetron was given intravenously. Patients were followed up in post-operative period on the surgery day, POD 1, 2 and after 1 week for pain scoring and cosmetic outcome.
Figure 1.
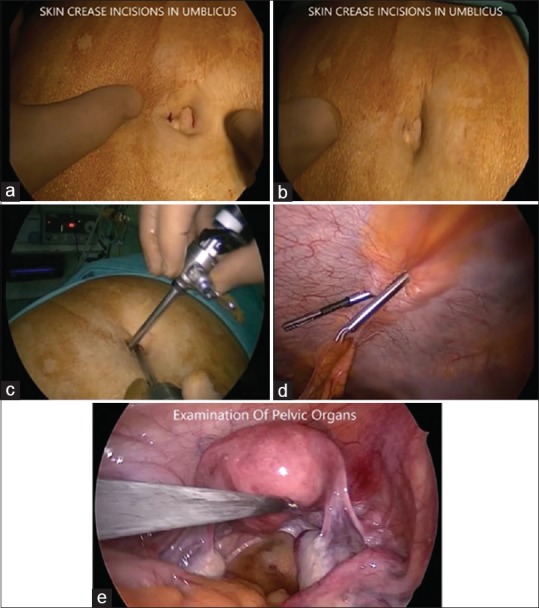
Surgical technique (abdominal part): (a and b) Skin incisions at umbilicus. (c) Abdominal ports of 5 mm through umbilicus. (d) Endoscopic view of umbilical ports. (e) Examination of pelvic cavity through umbilical port
Figure 2.
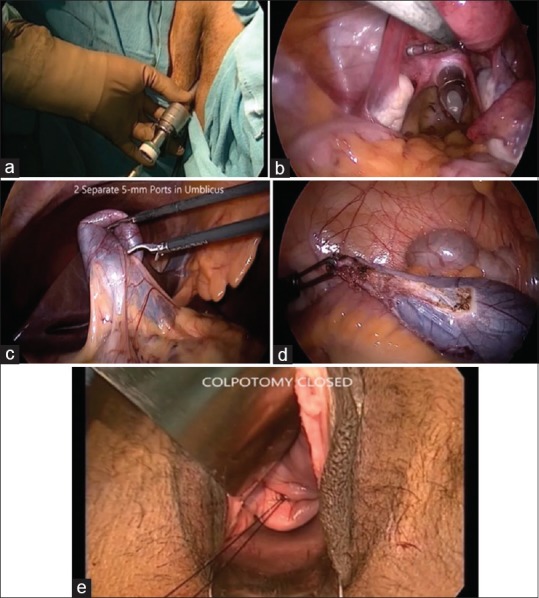
Surgical technique (vaginal part): (a) External view of vaginal 10 mm port. (b) Endoscopic view of vaginal 10 mm port. (c) Endoscopic view of gall bladder dissection through vaginal telescope. (d) Removal of gall bladder intact through vagina under vision from umbilical telescope. (e) Closure of port in the posterior vaginal fornix
Figure 3.
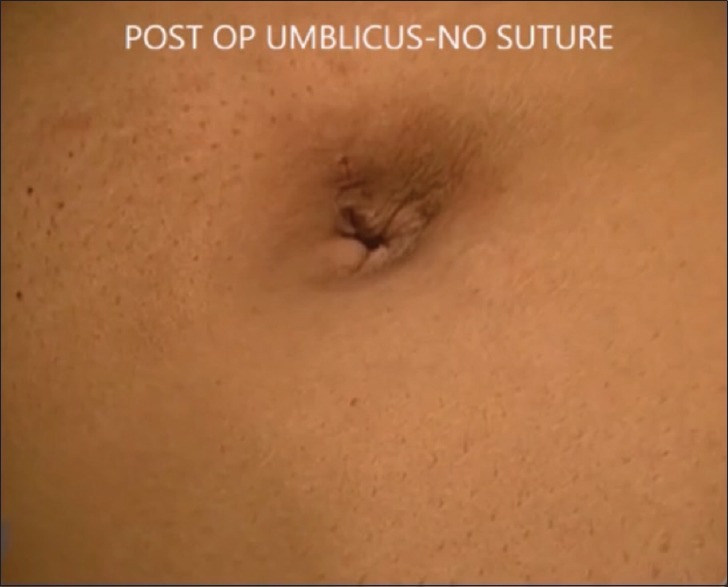
Post-operative skin incision site
Outcome
To see for complications, pain score and aesthetic score. Definition: Pain score: Visual analogue score (1–10) was used to measure pain intensity.[8] Aesthetic score: Harvard four point scale was used for assessing aesthetic outcome (0 - poor, 1 - fair, 2 - good, 3 - excellent).[9]
Statistical analysis
Data are expressed as number, percentages, mean and standard deviation. Statistical analysis was performed using GraphPad Prism (Version 6.0, Developer- GraphPad Software, Inc).
RESULTS
During the study, a total of 1100 cases underwent laparoscopic cholecystectomy, of which 257 cases underwent hybrid NOTES cholecystectomy. Four patients had mucocele of GB, 6 had acute mild cholecystitis. Six subjects underwent simultaneous laparoendoscopic single-site (LESS) hysterectomy at the same sitting. The mean age of the patients was 42.5 ± 8.9 (25–68) years. The mean BMI was 25.1 ± 2.4 (19.6–34) kg/m2. The indication for cholecystectomy was symptomatic cholelithiasis in all the cases. Two of the cases needed conversion to standard laparoscopic technique one due to presence of Endometriosis and another due to difficult visualisation of Calot's triangle.
Mean operative time was 31.5 ± 5.1 (25–40) min. None of the patients had any intraoperative complications. Post-operative course was uneventful in all the cases. None of the patients had biliary leak or required blood transfusion. None of the cases had any episode of pain abdomen or per-vaginal discharge on day 7. None of the patients had any port-site infection during the study. On extended follow-up of 1-month, none of the cases had any specific complaints, no visible scar or any hernia. Only seven patients had the complaint of occasional dull aching pain in the right hypochondrium. The duration of hospital stay was only a single day in all the cases. The mean pain score on day 1 and 2 was 3.6 ± 0.4 (3–4) and 1.0 ± 0.06 (1–2), respectively. The mean paracetamol (analgesic) dose requirement was 6.1 ± 0.6 (4–6.9) g. The aesthetic score was excellent in all the cases [Figure 3].
DISCUSSION
In the present prospective study, we report our technique of using hybrid NOTES in cholecystectomy and its outcome in terms of complications and cosmesis. None of the patients experienced any serious adverse event including low pain score with this technique and excellent aesthetic score was achieved in 100% of the cases.
Over the last few years, there has been a great deal of evolution on minimally invasive surgical techniques resulting in less pain, duration of hospital stay along with good cosmetic results. Kalloo et al. performed the first NOTES technique to do liver biopsies.[10] The approaches to peritoneum have been tried through vagina, colon, stomach and urinary bladder. The list of surgeries performed through NOTES technique includes cholecystectomy, appendectomy, ovarian cysts, tubal surgery, splenic surgery, hernia repair and nephrectomy.[11] The access of the peritoneal cavity through colon and stomach are associated with risk of intra-abdominal infection due to defective closure of the wall of the viscera. Transvaginal route for operative procedures such as hysterectomy or tubal ligation has been used for over 100 years. The transvaginal approach like the one used in the present study does not carry the risks of infection or defective wound closure as in transgastric/colonic approach. In addition to above-mentioned benefits, transvaginal approach provides a straight view of GB does not need the retroflection as in transgastric or colonic approach. In the transgastric/transcolic approach, the operative time is invariably >90 min, whereas this technique has the biggest advantage of much reduced operative time (25–40 min). This technique has lesser operative time than other NOTES as it does not include puncturing and passing sutures through GB for stabilisation and traction. NOTES surgery essentially removes the entire port site related complications such as infection, nerve injury, epigastric vessel injury, subcutaneous or intermuscular haematomas and post-operative infections and hernias. Even mini-laparoscopic ports are not fully immune to these complications.
In some NOTES technique, multi-channel ports are inserted through the vagina with or without an incision in the abdomen. We would appropriately like to call our technique as hybrid NOTES, as it includes an incision over the anterior abdominal wall at the umbilicus along with the telescope inserted through the vagina. The operative technique requires the expertise of both general surgeon and gynaecologist. The advantages of NOTES include, early recovery with reduced hospital stay, decrease in the incidence of adhesions, decrease in the incidence of hernia through abdominal wall and ideal cosmetic result after a surgery, in addition to significantly low pain scores. In the present study, the average pain score was <5, with only 2 cases having over 5 and 95% of the cases had a hospital of stay of only a single day. No Dyspareunia was reported post-operatively in the long-term follow-up. The cosmetic score was also excellent in 93% of the cases and none of the patients developed any major complication after using this technique. The results of the present study are similar to the results of the past by Bulian et al. and Brescia et al.[7,12] Brescia et al. evaluated the laparoscopic assisted TVC in 21 cases and reported very good cosmetic results, less post-operative pain, faster mobilisation and short hospital stay.[12] Bulian et al. carried out a matched-cohort study comparing 50 hybrid cholecystectomy and 50 classical laparoscopic cholecystectomy.[7] The authors observed that cases with hybrid NOTES had a significant less pain in early post-operative period with shorter hospital stay compared to standard technique.[7,12] Bulian et al. also randomised 100 cases to either needlescopic cholecystectomy (NC) (using 2–3 mm trocars) or umbilical-assisted TVC, patients randomised to TVC group had significantly better aesthetic, analgesic requirement and short term post-operative quality of life compared to those who underwent NC.[13] The technique reported by both the authors is similar to our technique in terms of utilising both transvaginal and abdominal route to perform cholecystectomy.
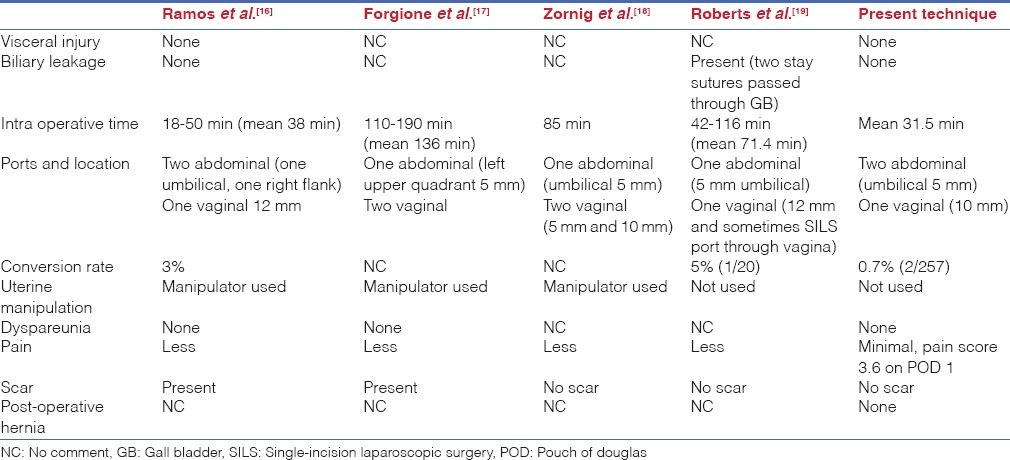
Hensel et al., Kilian et al., Bulian et al. and many other transvaginal NOTES studies have used ‘Zornig technique.’[14,15] However, the present study has used different operative technique ‘Dhillon technique,’ named after first author. The present study uses only one port with telescope through the vagina, different from other hybrid NOTES described by other authors where they use two ports or multi-portaccess devices through vagina, one for the telescope and one with grasper. While operating with two ports there can be friction between them and the bowel which gets collected in the pelvis in head up position can get injured due to the scissoring effect of two instruments which are not in the visual field. Furthermore, the manipulation of instruments through the vaginal end is difficult. Whereas, in the present technique, only one vaginal port with long cannula and telescope was used, which was inserted and removed under vision, so that there was no risk of bowel injury. As only one 10 mm trocar is used through vagina/POD the manoeuvrability in the small vaginal space is easy causing least vaginal/pelvic trauma, thereby avoiding post-operative dyspareunia, which none of our patients had. The present technique comparison with other hybrid NOTES technique has been shown in Table 1. The authors have evolved to this technique in time from standard laparoscopic cholecystectomy to single incision cholecystectomy to LESS surgery - scarless stitchless hysterectomy).[20] The experience in gynaecologic surgery was an added advantage to contribute in modifying to this technique.
Table 1.
Comparison of present technique with other hybrid natural orifice transluminal endoscopic surgery techniques
However, the technique has limitations in few settings like excessive abdominal obesity BMI >30 kg/m2 and in very tall patients, where standard laparoscopic surgery may be preferred over hybrid NOTES and also the study was not adequately powered to access the outcome and/or complications of the surgery. The present study involved no use of any special port access device in the vagina and used the standard straight laparoscopic instruments and delved on the philosophy of not puncturing the GB. The learning curve for this technique is not very long due to its simplicity.
CONCLUSIONS
Using the present technique of hybrid NOTES is beneficial in terms of cosmetic results, lesser need of analgesic and shorter hospital stay. Although the results are promising randomised trials are required to confirm the above findings and for further refinement and standardisation of the technique which is physiologically very friendly and avoids all port site complications such as hernias, pain and infection.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Meljnikov I, Radojcic B, Grebeldinger S, Radojcic N. History of surgical treatment of appendicitis. Med Pregl. 2009;62:489–92. [PubMed] [Google Scholar]
- 2.Litwin DE, Cahan MA. Laparoscopic cholecystectomy. Surg Clin North Am. 2008;88:1295–313, ix. doi: 10.1016/j.suc.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 3.Shea JA, Berlin JA, Bachwich DR, Staroscik RN, Malet PF, McGuckin M, et al. Indications for and outcomes of cholecystectomy: A comparison of the pre and postlaparoscopic eras. Ann Surg. 1998;227:343–50. doi: 10.1097/00000658-199803000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arulampalam T, Paterson-Brown S, Morris A. Association of Laparoscopic Surgeons of Great Britain and Ireland (ALSGBI); Association of Coloproctology of Great Britain and Ireland (ACPGBI); Association of Upper Gastro-intestinal Surgeons of Great Britain and Ireland (AUGIS); British Association of Urological Surgeons (BAUS); British Society of Gynaecological Endoscopy (BSGE); British Obesity and Metabolic Surgical Society (BOMSS); British Society of Gastroenterology (BSG). Natural orifice transluminal endoscopic surgery. Ann R Coll Surg Engl. 2009;91:456–9. [Google Scholar]
- 5.Delvaux G, Devroey P, De Waele B, Willems G. Transvaginal removal of gallbladders with large stones after laparoscopic cholecystectomy. Surg Laparosc Endosc. 1993;3:307–9. [PubMed] [Google Scholar]
- 6.Tsin DA, Sequeria RJ, Giannikas G. Culdolaparoscopic cholecystectomy during vaginal hysterectomy. JSLS. 2003;7:171–2. [PMC free article] [PubMed] [Google Scholar]
- 7.Bulian DR, Trump L, Knuth J, Siegel R, Sauerwald A, Ströhlein MA, et al. Less pain after transvaginal/transumbilical cholecystectomy than after the classical laparoscopic technique: short-term results of a matched-cohort study. Surg Endosc. 2013;27:580–6. doi: 10.1007/s00464-012-2490-2. [DOI] [PubMed] [Google Scholar]
- 8.Grant S, Aitchison T, Henderson E, Christie J, Zare S, McMurray J, et al. A comparison of the reproducibility and the sensitivity to change of visual analogue scales, Borg scales, and Likert scales in normal subjects during submaximal exercise. Chest. 1999;116:1208–17. doi: 10.1378/chest.116.5.1208. [DOI] [PubMed] [Google Scholar]
- 9.Haloua MH, Krekel NM, Jacobs GJ, Zonderhuis B, Bouman MB, Buncamper ME, et al. Cosmetic outcome assessment following breast-conserving therapy: A comparison between BCCT. core software and panel evaluation. Int J Breast Cancer 2014. 2014:716860. doi: 10.1155/2014/716860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kalloo AN, Singh VK, Jagannath SB, Niiyama H, Hill SL, Vaughn CA, et al. Flexible transgastric peritoneoscopy: A novel approach to diagnostic and therapeutic interventions in the peritoneal cavity. Gastrointest Endosc. 2004;60:114–7. doi: 10.1016/s0016-5107(04)01309-4. [DOI] [PubMed] [Google Scholar]
- 11.Rattner D, Kalloo A ASGE/SAGES Working Group. ASGE/SAGES working group on natural orifice translumenal endoscopic surgery. October 2005. Surg Endosc. 2006;20:329–33. doi: 10.1007/s00464-005-3006-0. [DOI] [PubMed] [Google Scholar]
- 12.Brescia A, Masoni L, Gasparrini M, Nigri G, Cosenza UM, Dall’Oglio A, et al. Laparoscopic assisted transvaginal cholecystectomy: single centre preliminary experience. Surgeon. 2013;11(Suppl 1):S1–5. doi: 10.1016/j.surge.2012.09.003. [DOI] [PubMed] [Google Scholar]
- 13.Bulian DR, Knuth J, Cerasani N, Sauerwald A, Lefering R, Heiss MM. Transvaginal/transumbilical hybrid – NOTES – versus 3-trocar needlescopic cholecystectomy: short-term results of a randomized clinical trial. Ann Surg. 2015;261:451–8. doi: 10.1097/SLA.0000000000000218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zornig C, Mofid H, Emmermann A, Alm M, von Waldenfels HA, Felixmüller C. Scarless cholecystectomy with combined transvaginal and transumbilical approach in a series of 20 patients. Surg Endosc. 2008;22:1427–9. doi: 10.1007/s00464-008-9891-2. [DOI] [PubMed] [Google Scholar]
- 15.Zornig C, Siemssen L, Emmermann A, Alm M, von Waldenfels HA, Felixmüller C, et al. NOTES cholecystectomy: matched-pair analysis comparing the transvaginal hybrid and conventional laparoscopic techniques in a series of 216 patients. Surg Endosc. 2011;25:1822–6. doi: 10.1007/s00464-010-1473-4. [DOI] [PubMed] [Google Scholar]
- 16.Ramos AC, Murakami A, Galvão Neto M, Galvão MS, Silva AC, Canseco EG, et al. NOTES transvaginal video-assisted cholecystectomy: First series. Endoscopy. 2008;40:572–5. doi: 10.1055/s-2008-1077398. [DOI] [PubMed] [Google Scholar]
- 17.Forgione A, Maggioni D, Sansonna F, Ferrari C, Di Lernia S, Citterio D, et al. Transvaginal endoscopic cholecystectomy in human beings: Preliminary results. J Laparoendosc Adv Surg Tech A. 2008;18:345–51. doi: 10.1089/lap.2007.0203. [DOI] [PubMed] [Google Scholar]
- 18.Zornig C, Emmermann A, von Waldenfels HA, Mofid H. Laparoscopic cholecystectomy without visible scar: Combined transvaginal and transumbilical approach. Endoscopy. 2007;39:913–5. doi: 10.1055/s-2007-966911. [DOI] [PubMed] [Google Scholar]
- 19.Roberts KE, Shetty S, Shariff AH, Silasi DA, Duffy AJ, Bell RL. Transvaginal NOTES hybrid cholecystectomy. Surg Innov. 2012;19:230–5. doi: 10.1177/1553350611427547. [DOI] [PubMed] [Google Scholar]
- 20.Awasthi D, Dhillon KS. Laparoendoscopic single-site surgery: Scarless stitchless hysterectomy. J Gynaecol Surg. 2015;31:144–7. [Google Scholar]


