Abstract
INTRODUCTION:
No previous study clearly focuses on laparoscopic technique to perform the second stage surgery (proctectomy with ileal pouch-anal anastomosis [IPAA]) after total colectomy for acute/severe ulcerative colitis (UC). We describe the procedural steps for a simple and rational minimally invasive second stage surgery, reporting intra- and short-term post-operative results.
PATIENTS AND METHODS:
During the period December 2014–December 2015, 10 consecutive patients (8 males and 2 females) with mean age of 48 years underwent laparoscopic proctectomy and IPAA adopting our novel approach. They were operated 3 months after the previous total colectomy which has been performed, respectively, for acute (three patients) or severe (seven patients) UC. Intraoperative data and post-operative complications, divided as minor and major, were recorded and analysed. A body image questionnaire was administered to all patients to evaluate the cosmetic results of the procedure.
RESULTS:
Overall mean surgical time was 235 ± 49 min. During the post-operative course, three patients required morphine for >48 h, no patient needed blood transfusion and bowel movements recovery happened as mean during the 2nd day. No early major complications happened. Two patients (20%) developed peri-ileostomic wound infection at the right flank. Only one patient (10%) suffered from ileal-anal anastomotic dehiscence, conservatively treated till resolution. The average length of hospital stay was 8 ± 2 days. The body image questionnaire showed in all patients an extreme satisfaction about the results obtained (mean value = 59/64 points).
CONCLUSIONS:
Through three standardised surgical steps easily reproducible, we describe an almost scar-less procedure able to optimise the intraoperative time with good post-operative results in terms of complications and cosmesis.
Keywords: Cosmesis, ileal pouch-anal anastomosis, laparoscopic surgery, restorative proctocolectomy, ulcerative colitis
INTRODUCTION
Surgery for ulcerative colitis (UC) has radically changed during the last four decades: In 1978, the introduction of restorative proctocolectomy with ileal pouch-anal anastomosis (IPAA) made the UC patients both ‘free’ from the disease and the need for a permanent stoma.[1] Since 1992, the increased use of minimally invasive surgery (wound sparing techniques) has left the UC patients almost free from scars too.[2] In fact, during the last years, many publications support the role of minimally invasive approach for the treatment of both elective[3,4,5,6,7,8,9] and emergency[10,11,12,13] UC surgeries. However, UC patients are often under high doses of steroids or immunosuppressive drugs, and because of their disease, they are frequently anaemic and characterised by a catabolic state, potentially at higher risk of minor or major septic complications than after oncological colorectal surgery.[14,15] Furthermore, a high percentage of UC patients has to be surgically treated with a three-stage approach: (1) total colectomy with terminal ileostomy; (2) proctectomy with IPAA and loop ileostomy; (3) loop ileostomy closure.
The aim of the present study is to describe a minimally invasive standardised laparoscopic technique to perform the second stage surgery (proctectomy and IPAA) in UC patients, analysing post-operative results in terms of complications and cosmetic satisfaction.
PATIENTS AND METHODS
From December 2014 to December 2015, ten consecutive patients underwent laparoscopic proctectomy and IPAA at the Department of Surgery and Translational Medicine of the University of Florence. The first stage surgery (total colectomy and ileostomy) had been performed, respectively, for acute (three patients) or severe (seven patients) UC. In nine of ten patients, the first stage surgery had been performed laparoscopically, removing the specimen from a mini-laparotomy performed at the right flank used at the end of the operation to carry out the terminal ileostomy too. Only one patient had undergone open total colectomy in the presence of a toxic megacolon. In all cases, the rectum had been stapled intraperitoneally at the level of the sacral promontorium, preserving the superior haemorrhoidal vessels and it was abandoned in the pelvis. Starting from post-operative day 3, topic therapy (5-aminosalicylic acid + steroid) was administered to control the rectal inflammation, and it was continued for a mean of 3 months, when the second stage surgery, adopting our newly described surgical steps, was performed. A computerised database was built prospectively recording all data about intra- and peri-operative course of this second stage surgery. Written informed consent was obtained from all the study participants, obtaining ethical approval from the local Experts Committee of Careggi Hospital. No UC patient undergoing the second stage surgery during the same period was excluded from the study. We evaluated post-operative complications dividing them as minor and major. At a mean of 1 month after surgery, all patients underwent X-ray contrasted anastomotic control (pouchography) to confirm the status of the IPAA and to program the ileostomy closure. During follow-up (as mean 3 months after the second stage), we administered all patients the already validated ‘body image questionnaire’ to evaluate the cosmetic results of the procedure.[16]
Surgical technique
During the first step of our approach, the terminal ileostomy is freed by the abdominal wall: An elliptical peri-stomal incision removing about 1 cm skin is performed (as mean about 5 cm in main diameter); the ileum is prepared reaching the anterior fascia of the right rectal muscle and the peritoneum. Every adhesion interesting the last ileal loop is cut during this first step.
The second surgical step is the J-pouch creation: The terminal ileum, freed by adhesions, is easily taken outside the abdomen from the same right flank incision. Usually, ileo-caecal vessels can be preserved without having any mesenterium traction. J-pouch is performed with 60 mm linear stapler cartridges after measuring the ileal loop to obtain a 15 cm long pouch as mean. The pouch is created stapling the small bowel from the opening of the previous terminal ileostomy. The anvil of a 25 or 28 mm circular stapler is put inside the pouch at its distal site. The proximal side of the pouch where the stapler had been introduced is sutured with a double layer of continuous 3/0 polydioxanone (PDS®; Ethicon) [Figure 1a]. The ileal pouch is gently pushed inside the abdomen, and the abdominal wall incision is used to create the pneumo-peritoneum through a 10 mm trocar (for the operator's right hand) put after positioning of LAP-DISC® device [Figure 1b].
Figure 1.
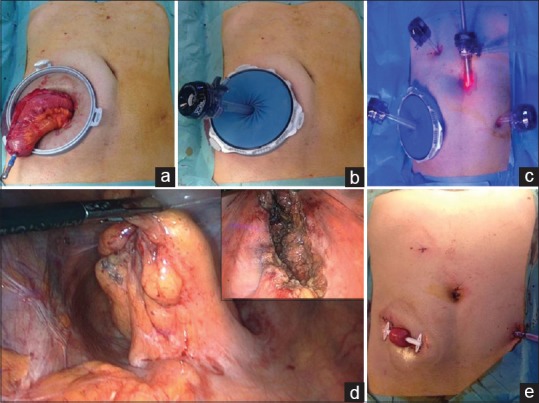
After the previous terminal ileostomy is freed by the abdominal wall, the ileal pouch is performed (a); the same abdominal wall incision is used to create the pneumo-peritoneum through a 10 mm trocar after positioning of LAP-DISC (b); trocar positions (c); the proctectomy is performed at the elevators muscles level stapling at the anal channel 2 cm above the dentate line (d and square). The loop ileostomy is created using the right flank incision and drainage is let in the pelvis using the 10 mm left flank trocar incision (e)
The third step is the laparoscopic proctectomy and the IPAA: Two additional 10 mm trocars and a 5 mm trocar are used. These are placed, respectively, in the left lower quadrant (retracting port, for the assistant's left hand), peri-umbilical (optical port) and right upper quadrant (for the operator's left hand) [Figure 1c]. The abandoned rectum is found and freed by eventual adhesions with the ileum or the omentum, and the inferior mesenteric artery, or its distal branch, cuts after clip positioning [Figure 1d]. The entire dissection is accomplished with a 5 mm laparoscopic high energy device.
The rectum is circumferentially prepared till the elevators muscles level and stapled with a laparoscopic linear stapler, introduced by the right flank 10 mm trocar, at the level of the anal canal 2 cm above the dentate line as mean [Figure 1d]. We prefer to perform trans-mesorectal proctectomy whenever not contraindicated. The specimen is delivered through the LAP-DISC, and the pneumo-peritoneum easily restored to perform the stapled IPAA and to check it with the pneumatic test.
At the end of the procedure, we prefer to create a loop ileostomy in all patients, using the right flank incision to let out the ileal loop (25 cm proximally from the pouch inlet as mean). In all cases, drainage is let in the pelvis using the 10 mm left flank trocar incision [Figure 1e].
Through these surgical steps, we are able to create an almost scar-less procedure, with a standardised technique easily reproducible.
RESULTS
Patients were consecutive 8 males and 2 females; their mean age was 48 years (range = 22–68); the mean body mass index was 22 (range = 18.9–29.2). Overall mean surgical time was 235 ± 49 min (range 155–310). Only three patients required morphine for more than 48 h in the post-operative course, and no patient needed post-operative blood transfusion. Bowel movements recovery (and consequently the solid oral re-feeding) happened in the 2nd post-operative day as mean. No early major complications happened. Two patients (20%) developed wound infection at the right flank (conservatively treated by draining); one patient (10%) had delayed gastric empty solved with medical therapy from post-operative day 6. Only one patient (10%) suffered ileal-anal anastomotic dehiscence conservatively treated till resolution (confirmed by a further pouchography). Because of the protective loop ileostomy we performed in all cases, the patient did not show any general sign of infection. The average length of hospital stay was 8 ± 2 days (range = 6–12). All patients answered the body image questionnaire reporting an extreme satisfaction (mean value = 59/64 points).
DISCUSSION
Despite advances in the medical treatment of UC, the surgical management is still required in up to 35% of patients and total proctocolectomy with IPAA is the gold standard procedure.[17]
A three-stage approach is preferred in acute or severe UC or debilitated patients. Several meta-analyses and review studies support the role of minimally invasive approach for the treatment of both elective[3,4,5,6,7,8,9] and emergency[10,11,12,13] UC surgery; however, to date, only one study describes in detail, in 18 patients, the laparoscopic IPAA surgical technique after the previous abdominal colectomy for acute-severe UC.[18] Taking into consideration that experience, we modified the surgical steps to obtain a simpler and time-saving minimally invasive laparoscopic approach to perform the second stage surgery (proctectomy and IPAA with loop ileostomy) in the same setting. Our approach differs because it is a standardised procedure performed through the same mini-laparotomy at the right flank. About the operative time, we evaluated the procedure in relationship to the time reported to perform the second stage procedure by Ouaïssi et al.:[18] Our approach seems to be time-saving (235 ± 48 vs. 286 ± 47 min); furthermore, we had lower rates of post-operative blood transfusions (0% vs. 17%), reoperations (0% vs. 11%) and anastomotic dehiscence (14% vs. 28%). We did not experience major complications, reporting only one case of anastomotic leak, conservatively treated. In this point of view, we prefer to preventively perform the loop ileostomy in patients undergoing IPAA. It is because of the high risk of ileal-anal anastomotic dehiscence reported in literature.[3,4,5,6,7,8,9,10,11,12,13,18] About minor post-operative complications, we observed one wound infection of the right flank around the ileostomy and one peri-stomal abscess, both conservatively treated: These values are similar to that reported in literature.[3,4,5,6,7,8,9,10,11,12,13,18]
Interestingly, in our series, no patients required conversion to laparotomy; meanwhile, one patient, previously undergone open total colectomy, was the candidate for laparoscopic IPAA adopting our new approach.
The length of post-operative stay was similar (9 ± 2 vs. 10 ± 2 days) to that reported by Ouaïssi et al.[18] To the best of our knowledge, in UC patients undergoing the second stage surgery, this is the first experience prospectively analysing both the post-operative pain control and the cosmetic results: Even considering the small sample size, we found an easily controlled post-operative pain: 4 patients (57.1%) required morphine for <24 h after surgery; it was extremely useful to obtain a prompt small bowel movements recovery (as mean during the 2nd post-operative day) and consequently to restore the oral re-feeding as soon as possible. About cosmesis, the body image questionnaire was extremely satisfactory for all patients (mean result 59/64) and it is to consider that one patient, undergone open surgery total colectomy, due to the presence of the first stage surgery abdominal scar, reported a lower grade of satisfaction at the questionnaire performed after the second stage surgery.
CONCLUSIONS
Our rationalisation of the second stage surgery in UC is safe and effective. It overcomes the complexity of the procedure providing a standardisation of the technique. In terms of operative time, hospital stay, post-operative pain control and cosmesis, our results are encouraging.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Parks AG, Nicholls RJ. Proctocolectomy without ileostomy for ulcerative colitis. Br Med J. 1978;2:85–8. doi: 10.1136/bmj.2.6130.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Peters WR. Laparoscopic total proctocolectomy with creation of ileostomy for ulcerative colitis: Report of two cases. J Laparoendosc Surg. 1992;2:175–8. doi: 10.1089/lps.1992.2.175. [DOI] [PubMed] [Google Scholar]
- 3.Thibault C, Poulin EC. Total laparoscopic proctocolectomy and laparoscopy-assisted proctocolectomy for inflammatory bowel disease: Operative technique and preliminary report. Surg Laparosc Endosc. 1995;5:472–6. [PubMed] [Google Scholar]
- 4.Ky AJ, Sonoda T, Milsom JW. One-stage laparoscopic restorative proctocolectomy: An alternative to the conventional approach? Dis Colon Rectum. 2002;45:207–10. doi: 10.1007/s10350-004-6149-5. [DOI] [PubMed] [Google Scholar]
- 5.Santoro E, Carlini M, Carboni F, Feroce A. Laparoscopic total proctocolectomy with ileal J pouch-anal anastomosis. Hepatogastroenterology. 1999;46:894–9. [PubMed] [Google Scholar]
- 6.Wexner SD, Johansen OB, Nogueras JJ, Jagelman DG. Laparoscopic total abdominal colectomy. A prospective trial. Dis Colon Rectum. 1992;35:651–5. doi: 10.1007/BF02053755. [DOI] [PubMed] [Google Scholar]
- 7.Fajardo AD, Dharmarajan S, George V, Hunt SR, Birnbaum EH, Fleshman JW, et al. Laparoscopic versus open 2-stage ileal pouch: Laparoscopic approach allows for faster restoration of intestinal continuity. J Am Coll Surg. 2010;211:377–83. doi: 10.1016/j.jamcollsurg.2010.05.018. [DOI] [PubMed] [Google Scholar]
- 8.Maartense S, Dunker MS, Slors JF, Cuesta MA, Gouma DJ, van Deventer SJ, et al. Hand-assisted laparoscopic versus open restorative proctocolectomy with ileal pouch anal anastomosis: A randomized trial. Ann Surg. 2004;240:984–91. doi: 10.1097/01.sla.0000145923.03130.1c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Seshadri PA, Poulin EC, Schlachta CM, Cadeddu MO, Mamazza J. Does a laparoscopic approach to total abdominal colectomy and proctocolectomy offer advantages? Surg Endosc. 2001;15:837–42. doi: 10.1007/s004640000356. [DOI] [PubMed] [Google Scholar]
- 10.Marceau C, Alves A, Ouaissi M, Bouhnik Y, Valleur P, Panis Y. Laparoscopic subtotal colectomy for acute or severe colitis complicating inflammatory bowel disease: A case-matched study in 88 patients. Surgery. 2007;141:640–4. doi: 10.1016/j.surg.2006.12.012. [DOI] [PubMed] [Google Scholar]
- 11.Bell RL, Seymour NE. Laparoscopic treatment of fulminant ulcerative colitis. Surg Endosc. 2002;16:1778–82. doi: 10.1007/s00464-001-8300-x. [DOI] [PubMed] [Google Scholar]
- 12.Marcello PW, Milsom JW, Wong SK, Brady K, Goormastic M, Fazio VW. Laparoscopic total colectomy for acute colitis: A case-control study. Dis Colon Rectum. 2001;44:1441–5. doi: 10.1007/BF02234595. [DOI] [PubMed] [Google Scholar]
- 13.Dunker MS, Bemelman WA, Slors JF, van Hogezand RA, Ringers J, Gouma DJ. Laparoscopic-assisted vs. open colectomy for severe acute colitis in patients with inflammatory bowel disease (IBD): A retrospective study in 42 patients. Surg Endosc. 2000;14:911–4. doi: 10.1007/s004640000262. [DOI] [PubMed] [Google Scholar]
- 14.Wexner SD, Reissman P, Pfeifer J, Bernstein M, Geron N. Laparoscopic colorectal surgery: Analysis of 140 cases. Surg Endosc. 1996;10:133–6. doi: 10.1007/BF00188358. [DOI] [PubMed] [Google Scholar]
- 15.Wexner SD, Cera SM. Laparoscopic surgery for ulcerative colitis. Surg Clin North Am. 2005;85:35–47, viii. doi: 10.1016/j.suc.2004.09.009. [DOI] [PubMed] [Google Scholar]
- 16.Dunker MS, Stiggelbout AM, van Hogezand RA, Ringers J, Griffioen G, Bemelman WA. Cosmesis and body image after laparoscopic-assisted and open ileocolic resection for Crohn's disease. Surg Endosc. 1998;12:1334–40. doi: 10.1007/s004649900851. [DOI] [PubMed] [Google Scholar]
- 17.Targownik LE, Singh H, Nugent Z, Bernstein CN. The epidemiology of colectomy in ulcerative colitis: Results from a population-based cohort. Am J Gastroenterol. 2012;107:1228–35. doi: 10.1038/ajg.2012.127. [DOI] [PubMed] [Google Scholar]
- 18.Ouaïssi M, Alves A, Bouhnik Y, Valleur P, Panis Y. Three-step ileal pouch-anal anastomosis under total laparoscopic approach for acute or severe colitis complicating inflammatory bowel disease. J Am Coll Surg. 2006;202:637–42. doi: 10.1016/j.jamcollsurg.2005.12.016. [DOI] [PubMed] [Google Scholar]


