Abstract
Approximately 60% of perioperative anaphylactic reactions are thought to be immunoglobulin IgE mediated, whereas 40% are thought to be non-IgE mediated hypersensitivity reactions (both considered non-dose-related type B adverse drug reactions). In both cases, symptoms are elicited by mast cell degranulation. Also, pharmacological reactions to drugs (type A, dose-related) may sometimes mimic symptoms triggered by mast cell degranulation. In case of hypotension, bronchospasm, or urticarial rash due to mast cell degranulation, identification of the responsible mechanism is complicated. However, determination of the type of the underlying adverse drug reaction is of paramount interest for the decision of whether the culprit drug may be re-administered. Neuromuscular blocking agents (NMBA) are among the most frequent cause of perioperative anaphylaxis. Recently, it has been shown that NMBA may activate mast cells independently from IgE antibodies via the human Mas-related G-protein-coupled receptor member X2 (MRGPRX2). In light of this new insight into the patho-mechanism of pseudo-allergic adverse drug reactions, in which as drug-receptor interaction results in anaphylaxis like symptoms, we critically reviewed the literature on NMBA-induced perioperative anaphylaxis. We challenge the dogma that NMBA mainly cause IgE-mediated anaphylaxis via an IgE-mediated mechanism, which is based on studies that consider positive skin test to be specific for IgE-mediated hypersensitivity. Finally, we discuss the question whether MRGPRX2 mediated pseudo-allergic reactions should be re-classified as type A adverse reactions.
Keywords: drug allergy, perioperative anaphylaxis, pseudo-allergy, adverse drug reaction, mast cell, histamine, Mas-related G-protein coupled receptor member X2
1. Introduction
The term “anaphylaxis” was previously used for IgE-mediated reactions only, whereas the term pseudo-allergic (or anaphylactoid) was used for similar clinical reactions, which occur via a non-IgE-dependent mechanism [1,2]. Both reactions may clinically present with hypotension, bronchospasm, and skin manifestations, typically urticaria [3,4]. The same symptoms might also be seen in cases of non-immune mediated pharmacological adverse drug reactions [5]. As it is not possible to distinguish anaphylactic from pseudo-allergic reactions clinically or by standard allergological investigations, a new definition has been suggested by the European Academy for Allergology and Clinical Immunology (EAACI). Thereby, all immediate-type adverse drug reactions are named anaphylaxis with a further subclassification into allergic or non-allergic [6].
The incidence of anaphylactic reactions during general anesthesia has been estimated at 1/4000 to 1/25,000, and about 1/5000 for Neuromuscular blocking agents (NMBA) [7]. The incidence varies according to geographical factors [8], indicating that environmental factors might have an effect on the risk of anaphylaxis during anesthesia. Isolated cutaneous symptoms seem to be more frequent in non-IgE-mediated anaphylaxis, whereas bronchospasm and cardiovascular symptoms are more often seen in IgE-mediated anaphylaxis [2]. However, it has been shown that the anesthetist was able to correctly identify the culprit drug in only one third of all peri-operative reactions [9].
Skin tests have so far been considered to be specific for IgE-mediated hypersensitivity, whereas pseudo-allergic reactions have been considered to yield negative results. However, the term “pseudo-allergy” has been too frequently used to describe any kind of immediate-type allergic-like reaction that is not IgE-mediated [10]. This is particularly the case for non-steroidal anti-inflammatory drug (NSAID) adverse reactions, where skin tests are typically negative due to the lack of mast cell involvement.
The recent identification of the Mas-related G-protein-coupled receptor member X2 (MRGPRX2), now allows for better classification of different types of non-IgE mediated allergic reactions [11]. According to the EAACI nomenclature, which has been published prior to the description of the MRGPRX2 receptor, these reactions should be classified into non-IgE mediated, allergic hypersensitivity reactions, considering the mast cell as belonging to the immune system [6]. Despite the proposal of the EAACI to abandon the term “pseudo-allergy”, this has been used to describe the reaction resulting from MRGPRX2 activation, and will be used in this review to differentiate this particular pathomechanism from other non-IgE mediated hypersensitivity reactions (Table 1). Especially, NMBA were described to elicit a pseudo-allergic reaction through activation of the MRGPRX2 receptor [11]. Whether this is relevant in human anaphylaxis to NMBA, remains hypothetical. However, this would explain why skin tests with NMBA may be positive in the absence of IgE-mediated hypersensitivity. Therefore, previously published data indicating that most reactions to NMBA are IgE-mediated based on positive skin test should be verified. An underlying pseudo-allergic mechanism would explain the high rate of anaphylactic reactions upon first exposure as well as the high rate of cross-sensitization, mainly demonstrated by positive skin test results to various NMBA [12,13].
Table 1.
Distinguishing features and proposed classification of different immediate type hypersensitivity reactions.
| Pseudo-Allergic (Mas-Related G-Protein-Coupled Receptor Member X2 (MRGPRX2) Activation) | Non-IgE Mediated, Immunologic Activation (IgG, rarely Described to be Involved in Immediate Type Reaction) | Non-IgE Mediated, Non Immunologic Activation (i.e., Opioid, Complement) | IgE Mediated | Non-Allergic (Immune System Not Primary Involved) | |
|---|---|---|---|---|---|
| Mast cell involvement | Yes | Yes | Yes | Yes | No |
| Skin test (immediate reading) | Positive | Negative | Positive | Positive | Negative |
| Specific IgE | Can be positive without clinical relevance | Can be positive without clinical relevance | Can be positive without clinical relevance | Presumably positive | Can be positive without clinical relevance |
| Basophil activation test (BAT) | Can be positive without clinical relevance | Presumably negative | For most negative | Presumably positive | Negative |
| Could explain reaction after first time exposure | Yes | No, except if previous sensitization by cross-reactivity | Yes | No, except if previous sensitization by cross-reactivity | Yes |
| Dose dependency | Yes | Probably | Yes | Classically no, marginally significant | Yes |
| Adverse drug reactions (ADR) Classification | New proposal: type A | Type B | Type B | Type B | Type A |
| Re-administration possible | Theoretically possible, with reduced speed or lower doses. No data available yet | Theoretically not recommended | Theoretically not recommended | Not recommended (consider desensitization protocol) | Yes, with reduced speed or lower doses if not pharmacologically contraindicated |
A better understanding of the underlying mechanism is of clinical relevance for deciding whether the culprit drug may be re-administered or has to be avoided. According to the still generally accepted and widely used classification of adverse drug reactions (ADR) that was developed in the 1970s [14], ADR can be classified into dose-related (“A” for Augmented, type A) or non-dose-related reactions (“B” for Bizarre, type B). The frequency of ADR type A is approximately 80%, whereas type B reactions are rarer [15]. According to this classification, non-IgE mediated hypersensitivity reactions represent type B reactions [16,17]. However, the highly predictable and dose-dependent mast cell degranulation found upon MRGPRX2 activation by NMBA [11] would argue in favor of a re-classification of pseudo-allergic reactions as type A adverse reactions. This would then allow for a more confident re-administration of a specific drug if needed.
2. Type A Adverse Drug Reactions Are Often Misinterpreted as Being “Allergic”
Type A ADR are pharmacological adverse reactions, which typically do not involve the immune system, and are therefore predictable. This means that the drug may be re-administered with a lower dose or reduced speed without re-eliciting the same adverse reaction. Examples of type A ADR are diarrhea after antibiotics, or gastric ulcers following prolonged NSAID treatment. Also, toxic reactions are typical type A reactions. The reason why some individuals suffer from type A ADR, whereas others do not, is often unknown. Identifying type A ADR is important, since this will have implications for the future management of the patient. An incorrect labeling as “allergic” may result in withholding optimal treatment for a subsequent illness, which can be deleterious in infectious disease and in anesthetic procedures [15].
3. Type B Adverse Drug Reaction Can Be Predictable and Dose Dependent
Type B reactions are ADR that are not predictable. They mainly include hypersensitivity reactions, which are mediated by the immune system and occur in a susceptible subgroup of patients. This susceptibility is classically considered to be due to environmental factors, in particular previous exposure during which the adaptive immune system develops hypersensitivity. However, it has been increasingly noted that some type B reactions that are highly predictable were not due to environmental factors, but to the genetic profile of the patient, linked to particular human leukocyte antigens (HLA). The reason for this is that the antigen presentation to T-cells is dependent on specific HLA haplotypes, for example in abacavir, carbamazepine and allopurinol ADR, which seem to be dose-dependent [18,19].
4. Mast Cells as Central Players in IgE-Mediated and Mas-Related G-Protein-Coupled Receptor Member X2-Mediated (MRGPRX2-Mediated) Anaphylactic Reactions
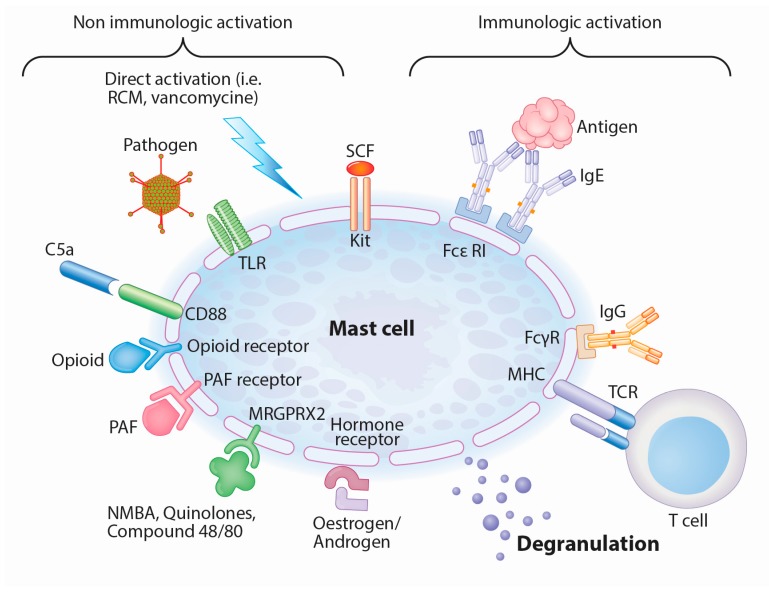
Mast cells can release preformed mediators (histamine, serotonin and proteoglycans, mainly heparin), newly formed lipid mediators (thromboxane, prostaglandin D2, leukotriene C4) and cytokines (e.g., tumor necrosis factor alpha, interleukin-4) during anaphylactic reactions. The clinical picture of IgE-mediated hypersensitivity, including hypotension, bronchospasm and urticaria, is mainly caused by these mediators, in particular histamine. However, mast cell degranulation can be also elicited by other mechanisms than IgE crosslinking, as these cells carry a variety of other receptors on their surface that can induce degranulation (Figure 1). Mast cells can be activated by Toll-like receptors (TLR), protease-activated receptors (PARs), opioid receptor, complement (particularly C5a), IgG and under certain circumstances even T-cells, depending on the localization and type of mast cell [20,21]. Whether mast cells are antigen presenting cells, is still matter of debate. Whereas all human mast cell types are activated via the aggregation of high affinity IgE receptors (FcεRI), a subset of mast cells found in the lungs and gut expressing only tryptase do not respond to complement components C3a, C5a and compound 48/80, a polymer used to promote mast cell degranulation [22]. Although TLR-mediated activation of mast cells does not lead to degranulation, but rather to cytokine, chemokine and lipid-mediator production, it is possible that TLR-mediated activation by pathogens may reduce the threshold required for degranulation by other stimuli [23].
Figure 1.
Immunologically and non-immunologically induced mast cell degranulation (adapted from Hannino et al. [20]). Abbreviations: RCM: radiocontrast media, TLR: Toll-like receptor, SCF: Stem cell factor, FcεRI: high affinity IgE receptor, FcγR: IgG receptor, TCR: T-cell receptor, NMBA: neuromuscular blocking agent, PAF: platelet activating factor, MHC: major histocompatibility complex.
5. Mast Cells Can Be Stimulated by Various Co-Factors and Mas-related G-Protein-Coupled Receptor Member X2 (MRGPRX2) Receptor Activation
Patients with chronic spontaneous urticaria often suffer from flares caused rather by a non-IgE mediated mechanism than by IgE-mediated allergy [24]. Different eliciting co-factors have been described as possible triggers such as body temperature, infections, hormonal factors, alcohol, or foods. NSAID, opiates, iodinated contrast media, vancomycin, local anesthetics and NMBA represent possible mast cell triggering agents, and should be avoided in patients with chronic urticaria or systemic mastocytosis if possible [1,3,5,25,26,27]. In the recent EAACI position paper on mastocytosis, concerning the use of general anesthetics, the authors state that in the current limited literature, there is conflicting information on both the tolerance of and reactions to different single drugs and drug groups [25]. Other authors suggest to avoid mivacurium and atracurium in particular [28].
The combination of different co-factors is thought to have a cumulative effect. This means that a single co-factor alone does not necessarily lead to a clinically apparent mast cell degranulation, but the simultaneous presence of several co-factors have the potential to trigger symptoms mediated by histamine release in these patients [24]. Nevertheless, it is widely accepted that the responsible mechanism does not involve adaptive immunity, and hence does not require sensitization [20]. Similarly, MRGPRX2 induced mast cell degranulation could be considered a co-factor and as such, depend on the presence of other co-factors to be clinically relevant. This mechanism could in turn at least partially explain why only a minority of patients react to NMBA.
6. Anaphylactic Reactions upon First Exposure Might Be due to IgE Cross-Sensitization or a Pseudo-Allergic Reaction
Therapeutically used monoclonal antibodies, as well as NMBA, have been described to induce anaphylactic reactions more frequently upon first exposure than subsequent re-exposure. The mechanism of these reactions remains unclear because previous sensitization to the drug is unlikely [29]. For decades, most NMBA were considered to cause non-specific histamine release from mast cells (benzylisoquinolines being more potent histamine releasers than aminosteroidal NMBA), and anesthetists believed that most of these reactions could be prevented by slow injection or pretreatment with antihistamines [30,31]. In recent years, newer studies from allergists, mainly considering positive skin test as a proof for IgE-mediated, type B ADR, indicated that for safety reasons, re-exposure to the culprit drug and to cross-reactive drugs needs to be avoided.
According to the current concept, a possible explanation for an IgE-mediated reaction upon first exposure could be cross-reactivity among different drugs, as shown in patients reacting to NMBA who have been previously exposed to pholcodine. Pholcodine is a non-prescription antitussive drug that contains a substituted ammonium ion (a moiety where the hydrogen atoms are substituted with other organic groups such as an alkyl group). Epidemiological studies have shown a correlation between the intake of pholcodine and the incidence of NMBA anaphylaxis. This is considered to be due to common substituted ammonium ions (tertiary and/or quaternary ammonium (QA) structures) which are found in a wide variety of chemical structures, including NMBA and pholcodine [8]. The main argument in favor of an IgE-mediated patho-mechanism in perioperative anaphylactic reactions due to NMBA is the reported decrease of the incidence of perioperative anaphylaxis after withdrawal of pholcodine from the market in Norway [32]. In this large cohort the total amount of NMBA exposure was not reported, instead official sales of NMBA in grams were used as indicator of exposure, showing a 12% decrease of NMBA exposure, and in particular a 28% decrease of succinylcholine exposure during the period studied [7]. Though the association between pholcodine exposure and NMBA anaphylaxis seems to be well established, the pathogenic mechanisms connecting these events remain yet to be elucidated [8]. In fact, it has been shown that pholcodine withdrawal was also associated with a decrease of total IgE levels [33], supporting the idea that pholcodine might be a potent “polysensitizer” (polyclonal IgE response) and may elicit NMBA sensitization by another mechanism than by sharing a common epitope. Precisely, mast cell responsiveness might be decreased due to lower circulating total IgE levels, as seen in patients after anti-IgE treatment. Based on this hypothesis, some authors considered the possibility that QA ions might be able to bind directly to immune receptors and stimulate cellular effectors in analogy to the “p-i concept” of drug interaction with majorhistocompatibility complex molecules and T-cell receptors in delayed hypersensitivity reactions [8].
7. The Supposed Involvement of the MRGPRX2 Receptor in Adverse Drug Reactions (ADR) to Neuromuscular Blocking Agent (NMBA) Leads to the Hypothesis of an Underlying “Innate Hypersensitivity”
Whereas severe cutaneous ADR associated with particular HLA-types are mainly delayed ADR, the recent identification of the MRGPRX2 receptor has introduced the concept of a genetical, possibly innate, predisposition to develop immediate-type pseudo-allergic ADR. Although environmental influence by epigenetic modification is certainly possible, genetic variants in the MRGPRX2 gene have already been reported [34,35]. This gene has undergone recent changes during evolution, and eleven haplotypes have been described so far [36]. Three of the four human-specific sequence substitutions are located in extra-cellular domains of the receptor. As extra-cellular receptor domains are usually involved in ligand recognition, the three human-specific amino acid substitutions may markedly modify the interaction between this receptor and its ligands. It is therefore probable that, similarly to several HLA-subtypes associated with drug reactions with eosinophilia and systemic symptoms (DRESS) syndrome or Lyell syndrome, mutations in the MRGPRX2 gene may be associated with an increased risk for pseudo-allergic ADR.
8. Perioperative Anaphylaxis due to NMBA Revised
NMBA are considered to be responsible for the majority of IgE-mediated reactions occurring during general anesthesia, followed by latex, antibiotics, hypnotics and opioids [37,38,39]. Opioids, like morphine, typically trigger non-IgE-mediated reactions [38]. Up to 85% of anaphylactic reactions occur in NMBA-naïve patients [40], and most of the NMBA-allergic patients show a high percentage of cross-reactivity, mostly based on skin tests results [41,42]. However, other authors reported a clinically lack of cross-reactivity between benzylisoquinolines and aminosteroids. Leysen et al. reported that, among 19 allergic patients to rocuronium, 15 were subsequently uneventfully exposed to a benzylisoquinoline [43]. Table 2 shows the most relevant studies indicating the mechanism of anaphylactic reactions to NMBA in chronological order. Most studies consider NMBA to mainly cause IgE-mediated reactions because positive skin tests were considered to prove the presence of IgE [2,43,44,45]. These studies should now be critically reviewed because we know that skin test can be positive in non-IgE mediated hypersensitivity.
Table 2.
Major clinical studies with data related to the prevalence and patho-mechanism of adverse drug reactions (ADR) to neuromuscular blocking agents (NMBA) (case series and case reports not considered).
| Title | Relevant Data and Remarks |
|---|---|
| Anaphylactic and anaphylactoid reactions occurring during anesthesia in France in 1999–2000 [2]. | Anaphylactic and anaphylactoid reactions were diagnosed in 518 cases (66%) and 271 cases (34%), respectively. The most common causes of anaphylaxis were NMBA (n = 306, 58.2%). Anaphylaxis was diagnosed on the basis of clinical history, skin tests, and/or specific immunoglobulin E assay. In case of negative tests, an anaphylactoid reaction was diagnosed. |
| Anaphylactic and anaphylactoid reactions occurring during anaesthesia in France. Seventh epidemiologic survey (January 2001–December 2002) [46]. | Anaphylactic and anaphylactoid reactions were diagnosed in 491 cases (69%) and 221 cases (31%), respectively. The most common causes of anaphylaxis were NMBA (n = 271, 55%). Anaphylaxis was diagnosed on the basis of clinical history if skin tests were positive or in case of elevated tryptase values and the presence of specific IgE. In case of negative tests, an anaphylactoid reaction was diagnosed. |
| Anaphylaxis during Anesthesia in Norway [47]. | Eighty-three cases were examined: IgE–mediated anaphylaxis was established in 71.1% of the cases, and NMBA were by far the most frequent culprit drug (93.2%). IgE-mediated anaphylaxis was identified based on a modified categorization grading of causality of the IgE-mediated reactions (investigated by skin prick test, intradermal test, histamine releasing test, specific IgE against morphine and P-aminophenyl phosphoryl choline) |
| Anaphylaxis during anesthesia: results of a 12-year survey at a French pediatric center [48]. | Out of 68 adverse reactions, IgE-mediated anaphylaxis was diagnosed in 51 children: 31 (60.8%) for NMBA, 14 (27%) for latex, seven (14%) for colloids, five (9%) for opioids and six (12%) for hypnotics. IgE-mediated anaphylaxis was diagnosed on the basis of the skin tests results concordant with the patients’ clinical history of adverse reactions and the anesthetic protocol. |
| Diagnosis of NMBA hypersensitivity reactions using cytofluorimetric analysis of basophils [49]. | In 47 NMBA allergic patients, cytofluorimetric analysis of basophils was positive in 17 subjects. The diagnosis of allergy to NMBA was established from a characteristic clinical history (urticaria, bronchospasm and/or anaphylactic shock a few minutes after the start of anesthesia) and the positivity of NMBA skin tests. |
| Anaphylaxis during general anaesthesia: one-year survey from a British allergy clinic [50]. | Out of the 23 patients who presented with anaphylaxis during anesthesia, 15 patients were found to have a positive skin test to at least one NMBA. |
| Evaluation of a new routine diagnostic test for IgE sensitization to NMBA [51]. | In 168 patients exposed to NMBA, quaternary ammonium (QA)-specific IgE was found in 84.2% of skin test-positive reactors. The frequency of QA-specific IgE positivity was significantly higher in skin test-negative reactors (24.6%) than in controls (9.3%), suggesting NMBA sensitivity. |
| Differentiating the cellular and humoral components of neuromuscular blocking agent-induced anaphylactic reactions in patients undergoing anaesthesia [52]. | On the basis of intradermal skin testing and clinical evaluation, allergy to NMBA was considered likely in 48 of 61 patients (79%). Correlation between skin test reactivity to rocuronium and IgE to rocuronium was low. In contrast, striking correlation between IgE to rocuronium and skin test reactivity to succinylcholine was found (p < 0.001). |
| IgE-sensitization to the cough suppressant pholcodine and the effects of its withdrawal from the Norwegian market [32]. | Methods used to identify NMBA induced anaphylaxis are not reported. Decrease of perioperative anaphylaxis after pholcodine withdrawal was noted. However, the total amount of NMBA usage was not reported. |
| Negative predictive value of skin tests to NMBA [53]. | 55 patients were diagnosed with an allergy to NMBA, confirmed by clinical history, presence of specific IgE and/or positive skin test. 19 of these 55 patients had a second general anesthesia, 13 without NMBA and 6 using an NMBA for which skin tests were negative. None had had a new reaction to the injected NMBA. |
| Hypersensitivity reactions during anesthesia. Results from the ninth French survey (2005–2007) [45]. | An IgE-mediated or non-IgE-mediated reaction was diagnosed in 786 cases (63%) and 467 cases (37%), respectively. The most common causes of anaphylaxis were NMBA (N = 373, 47.4%). Allergic or IgE-mediated anaphylaxis was diagnosed on the basis of skin test and/or IgE assay results consistent with the clinical history and the anesthetic protocol. |
| Perioperative allergic reactions: experience in a Flemish referral centre [54]. | Out of 119 patients, a diagnosis of IgE-mediated reaction was established by skin tests and/or specific IgE in 76 cases (63.9%). The most common agents were NMBA (61.8%). The remaining 43 cases (36.1%) were considered as non-IgE-mediated reactions. |
| Predictive value of allergy tests for NMBA: tackling an unmet need [43]. | 272 patients with a history of perioperative allergy who had received a NMBA were reported. From the 47 patients who were re-exposed to a NMBA, 19 were initially diagnosed with suspected NMBA allergy, 13 had another IgE-mediated allergy suspected, and in the remainder 15, no IgE-mediated allergy was identified (skin test, specific IgE and BAT were used). Negative skin test and negative BAT assisted the selection of alternative NMBA, which were well tolerated in all cases. |
| Multi-centre retrospective analysis of anaphylaxis during general anaesthesia in the United Kingdom: aetiology and diagnostic performance of acute serum tryptase [55]. | In 161 patients, an IgE-mediated cause was identified in 103 patients (64%); NMBA constituted the leading cause (38%). IgE-mediated reactions were diagnosed based on skin prick test [n = 25 (24%)], intradermal test (n = 68 (66%)), serum-specific IgE (n = 9 (9%)) and challenge tests (n = 3 (1%)). |
| Six years without pholcodine; Norwegians are significantly less IgE-sensitized and clinically more tolerant to NMBA [7]. | Five to 10 years after pholcodine withdrawal, very few, if any, individuals were IgE-sensitized to QA ion, and only one case of NMBA-related anaphylaxis per 1–2 years was reported. However, exposure decreased during time of observation and less suxamethonium and more rocuronium were used. |
8.1. Skin Tests to NMBA Have to Be Evaluated with Caution
Skin tests have been so far considered to have a high specificity for IgE-mediated reactions and to be negative in non-IgE mediated, immediate type reactions [2]. In NMBA induced anaphylaxis, this assumption was supported by the observation that most of the patients tolerate NMBA that were negative in skin test [56]. However, cases of a second anaphylactic reaction to a NMBA for which skin tests were negative, have been reported. In one case series, three patients among 192 who reacted to NMBA had a second anaphylactic reaction after re-administration of NMBA which resulted negative in skin test. Another patient had a minor hypersensitivity reaction to an NMBA for which skin tests were negative. Two other patients had additional reactions to NMBA for which they were not tested [42]. This ratio (6/192) is clearly higher than the incidence of anaphylactic reactions in NMBA-naïve patients (i.e., 1/5000), indicating an underlying increased risk of recurrence in these apparently predisposed patients, possibly linked to an underlying “innate” pseudo-allergic mechanism.
Moreover, patients with immediate type hypersensitivity against antibiotics, confirmed by positive skin test, have an increased risk for positive allergy skin tests for NMBA, independently from their atopic status [57]. This suggests a predisposition to positive skin tests to NMBA in a subgroup of patients without previously known NMBA exposure, possibly due to an underlying pseudo-allergic mechanism. Indeed, skin tests can be positive in patients with pseudo-allergic reactions, in particular when drugs are tested in so-called “irritative concentration” [41]. This seems in agreement with previous data from biopsies of positive skin test to NMBA, in which IgE did not appear to play any role [58]. The fact that most people do not react to non-irritative drug concentrations in skin tests, does not allow to assume that the patients which react have specific IgE against the drug. In a study investigating the cellular and humoral components of NMBA-induced anaphylactic reactions, the correlation between skin test reactivity to rocuronium and IgE to rocuronium was low. In contrast, striking correlation between IgE to rocuronium and skin test reactivity to succinylcholine was found (p < 0.001) [52]. This suggests that skin tests with rocuronium might not indicate IgE-mediated allergy, while skin tests to succinylcholine, a drug not acting on the MRGPRX2 receptor but sharing the QA epitope with rocuronium, could be more reliable for true NMBA IgE hypersensitivity. It also shows that IgE to rocuronium might be of lesser clinical relevance, as shown in other studies [43,52]. However, whether skin test with NMBA at correct concentrations may still be of value for IgE-mediated hypersensitivity, remains matter of debate. For rocuronium, a concentration 1/1000 (0.01 mg/mL) has been used in recent studies for intradermal testing and could increase specificity for IgE mediated hypersensitivity [59]. Also, it is not known if MRGPRX2 receptor on human mast cells might have a higher affinity to rocuronium than other NMBA, which could explain the higher rate of reactions to rocuronium than to other NMBA [59].
8.2. In Vitro Analysis of NMBA Anaphylaxis Shows Conflicting Results as to the Underlying Mechanism
Tryptase and histamine release are not specific for an IgE-mediated reaction [60,61]. Tryptase increase has been described to be more prominent in IgE-mediated reactions than in non-IgE mediated reactions, but these studies considered positive skin test to be diagnostic for IgE-mediated hypersensitivity [2,55]. Supposing that NMBA (except succinylcholine) might cause pseudo-allergic reactions, these data may be reinterpreted as follows: tryptase increase during the perioperative reaction is associated with an increased likelihood to have positive skin test, irrespective of whether this is mediated by IgE or not. This phenomenon is likely due to an increased propensity of degranulating mast cells during the perioperative reaction and during skin test.
As to other in vitro diagnostic tools, the value of specific IgE measurements for rocuronium, QA and morphine remains a matter of debate [8,43]. Although specific IgE against morphine appear to have the highest specificity for NMBA hypersensitivity, retrospective data confirm that an isolated positive result for morphine is not a reliable predictor for NMBA allergy [43,62,63]. In particular, specific IgE to morphine is not a good biomarker for sensitization to benzylisoquinolines [64]. In fact, IgE reactivity to tertiary and QA structures has been frequently found in the healthy general population [65]. Moreover, the overall rate of morphine sensitization is quite high, with a prevalence of 10% for patients with non-NMBA allergies and 5% for healthy blood donors in Norway [8]. Although the existence of specific IgE recognizing substituted ammonium ions has been demonstrated based on a radioimmunoassay using a sepharose-alcuronium complex [66], there is no conclusive evidence that conjugation of NMBA or their metabolites to endogenous proteins might form antigenic complexes [29]. Moreover, there is no evidence for any functional role of these antibodies in perioperative anaphylaxis to NMBA in vivo.
Basophil activation test (BAT) appears to be more reliable than measurement of specific IgE [43,44]. If the MRGPRX2 receptor is not expressed on basophils, as presumed by some authors [22], BAT could allow to differentiate true IgE-mediated hypersensitivity to NMBA from pseudo-allergic reaction. More precisely, if BAT would be positive, this would signal true IgE hypersensitivity, while negative BAT would indicate a MRGPRX2 mediated mechanism in a given patient with history of NMBA anaphylaxis. A recent study favored true IgE-mediated anaphylaxis as being responsible for atracurium-induced anaphylaxis because BAT was positive in 5/8 patients with positive skin tests [62]. In another study, BAT was positive in 11/12 patients who suffered from rocuronium-induced anaphylaxis and who had positive skin tests, and in 0/8 patients who tolerated rocuronium and had a negative skin test. This indicates that skin test and BAT results are often coherent and argue against an underlying pseudo-allergic mechanism [67]. However, recent data in literature calls these considerations into question: flow-cytometry studies of basophils recently showed that basophils express MRGPRX2 mainly intracellular [68], and further studies are required to determine this issue.
Atracurium ADR represents an exception among NMBA as the responsible epitope seems to be different than the ammonium ion in IgE-mediated reactions [69,70]. Moreover, taken together it seems that sensitization to atracurium occurs from different routes requiring a prior exposure. Whereas atracurium and mivacurium were already known to cause pseudo-allergic reactions [37], there is now evidence that members of all NMBA families except succinylcholine might cause pseudo-allergic reactions [11]. New data support previous study results showing the histamine releasing potential of several NMBA in healthy subjects, in particular of atracurium, mivacurium, tubocurarine, and to a lesser extent rocuronium [71].
9. Discussion
The recent discovery of the MRGPRX2 receptor gave important new insights into the patho-mechanism of pseudo-allergic ADR and questions a few old dogmas, in particular that skin tests are supposed to be specific for IgE-mediated reactions. Therefore, data in the literature reporting ADR based on positive skin tests have to be critically reviewed. Skin testing is not a formal proof for IgE-mediated reactions from the adaptive immune system. A positive skin test can mirror alternative activation pathways of cutaneous mast cell activation. Especially the assumption that anaphylaxis due to NMBA could be mainly IgE-mediated has to be questioned. On one hand the reported decreased incidence of anaphylaxis due to NMBA in Norway after pholcodine withdrawal and the often overlapping results of skin test and BAT, might argue in favor of an IgE-mediated reaction. On the other hand, as discussed in the previous chapters, these studies have several limitations and possible biases, and there are several facts that argue in favor of a pseudo-allergic mechanism: (1) most reactions occur upon first exposure, (2) there is a high rate of cross-sensitization to several NMBA, (3) specific IgE is present in non-allergic individuals without a clear causal link to the anaphylactic reaction, and (4) there is an increased risk of a second anaphylactic reactions to NMBA in skin test-negative patients with previous reaction to another NMBA compared to patients without previous reaction [42].
10. Conclusions
There is little doubt that IgE against the substituted ammonium ion might be induced by exposure to different chemical substances, i.e., pholcodine, that in turn puts the patient at risk for IgE-mediated anaphylaxis to succinylcholine due to cross-reactivity. However, the recent identification of the MRGPRX2 receptor indicates that other NMBA might induce mainly pseudo-allergic reactions. As mast cell degranulation mediated by MRGPRX2 was found to be dose-dependent and highly predictable [11], we propose that these pseudo-allergic reactions, differently than other non-IgE mediated allergic reactions in which skin test with immediate reading are negative (i.e., T-cell, IgG mediated, eosinophilic), should be reclassified as type A ADRs.
The hypothesis that most NMBA may cause pseudo-allergic rather than IgE-mediated reactions raises several new questions. (1) Supposing that NMBA reactions are due to non-IgE-mediated mast cell degranulation, why do some individuals react more easily than others? (2) Does the expression of MRGPRX2 vary in a single individual over time? Studies addressing the genetic variants and epigenetic modifications of MRGPRX2 are urgently needed to provide answers to these questions and gain more insight in the field of pseudo-allergic reactions.
Abbreviations
| NMBA | Neuromuscular blocking agents |
| NSAID | Non steroidal anti-inflammatory drugs |
| EAACI | European Academy for Allergology and Clinical Immunology |
| MRGPRX2 | Mas-related G-protein coupled receptor member X2 |
| ADR | Adverse drug reactions |
| TLR(s) | Toll-like receptors |
| PAR(s) | Protease-activated receptors |
| FcεRI | High affinity IgE receptors |
| QA | Quaternary ammonium |
| BAT | Basophil activation test |
| DRESS | Drug reaction with Eosinophilia and systemic symptoms |
| RCM | Radiocontrast media |
| SCF | Stem cell factor |
| FcγR | IgG receptor |
| TCR | T-cell receptor |
| PAF | Platelet activating factor |
| MHC | Major histocompatibility complex |
Author Contributions
David Spoerl reviewed the literature, David Spoerl and Thomas Harr drafted the manuscript, Christoph Czarnetzki and Haig Nigolian helped in drafting the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Ewan P.W., Dugué P., Mirakian R., Dixon T.A., Harper J.N., Nasser S.M. BSACI BSACI guidelines for the investigation of suspected anaphylaxis during general anaesthesia. Clin. Exp. Allergy J. Br. Soc. Allergy Clin. Immunol. 2010;40:15–31. doi: 10.1111/j.1365-2222.2009.03404.x. [DOI] [PubMed] [Google Scholar]
- 2.Mertes P.M., Laxenaire M.-C., Alla F. Groupe d’Etudes des Réactions Anaphylactoïdes Peranesthésiques Anaphylactic and anaphylactoid reactions occurring during anesthesia in France in 1999–2000. Anesthesiology. 2003;99:536–545. doi: 10.1097/00000542-200309000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Farnam K., Chang C., Teuber S., Gershwin M.E. Nonallergic drug hypersensitivity reactions. Int. Arch. Allergy Immunol. 2012;159:327–345. doi: 10.1159/000339690. [DOI] [PubMed] [Google Scholar]
- 4.Czech W., Schöpf E., Kapp A. Release of sulfidoleukotrienes in vitro: Its relevance in the diagnosis of pseudoallergy to acetylsalicylic acid. Inflamm. Res. Off. J. Eur. Histamine Res. Soc. 1995;44:291–295. doi: 10.1007/BF02032571. [DOI] [PubMed] [Google Scholar]
- 5.Mali S. Anaphylaxis during the perioperative period. Anesth. Essays Res. 2012;6:124–133. doi: 10.4103/0259-1162.108286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Johansson S.G., Hourihane J.O., Bousquet J., Bruijnzeel-Koomen C., Dreborg S., Haahtela T., Kowalski M.L., Mygind N., Ring J., van Cauwenberge P., et al. EAACI (the European Academy of Allergology and Cinical Immunology) nomenclature task force A revised nomenclature for allergy. An EAACI position statement from the EAACI nomenclature task force. Allergy. 2001;56:813–824. doi: 10.1034/j.1398-9995.2001.t01-1-00001.x. [DOI] [PubMed] [Google Scholar]
- 7.De Pater G.H., Florvaag E., Johansson S.G.O., Irgens Å., Petersen M.N.H., Guttormsen A.B. Six years without pholcodine; Norwegians are significantly less IgE-sensitized and clinically more tolerant to neuromuscular blocking agents. Allergy. 2016 doi: 10.1111/all.13081. [DOI] [PubMed] [Google Scholar]
- 8.Brusch A.M., Clarke R.C., Platt P.R., Phillips E.J. Exploring the link between pholcodine exposure and neuromuscular blocking agent anaphylaxis. Br. J. Clin. Pharmacol. 2014;78:14–23. doi: 10.1111/bcp.12290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Krøigaard M., Garvey L.H., Menné T., Husum B. Allergic reactions in anaesthesia: Are suspected causes confirmed on subsequent testing? Br. J. Anaesth. 2005;95:468–471. doi: 10.1093/bja/aei198. [DOI] [PubMed] [Google Scholar]
- 10.Celik G., Pichler W., Adkinson N.F. Drug Allergy. In: Adkinson N.F., Middleton E., editors. Middleton’s Allergy: Principles & Practice. Mosby/Elsevier; Philadelphia, PA, USA: 2009. [Google Scholar]
- 11.McNeil B.D., Pundir P., Meeker S., Han L., Undem B.J., Kulka M., Dong X. Identification of a mast-cell-specific receptor crucial for pseudo-allergic drug reactions. Nature. 2015;519:237–241. doi: 10.1038/nature14022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ebo D.G., Fisher M.M., Hagendorens M.M., Bridts C.H., Stevens W.J. Anaphylaxis during anaesthesia: Diagnostic approach. Allergy. 2007;62:471–487. doi: 10.1111/j.1398-9995.2007.01347.x. [DOI] [PubMed] [Google Scholar]
- 13.Dewachter P., Mouton-Faivre C., Emala C.W. Anaphylaxis and anesthesia: Controversies and new insights. Anesthesiology. 2009;111:1141–1150. doi: 10.1097/ALN.0b013e3181bbd443. [DOI] [PubMed] [Google Scholar]
- 14.Rawlins M., Thompson J. Pathogenesis of adverse drug reactions. In: Davies D.M., editor. Textbook of Adverse Drug Reactions. Oxford University Press; Oxford, UK: New York, NY, USA: 1977. [Google Scholar]
- 15.Waller D.G. Allergy, pseudo-allergy and non-allergy. Br. J. Clin. Pharmacol. 2011;71:637–638. doi: 10.1111/j.1365-2125.2011.03976.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Edwards I.R., Aronson J.K. Adverse drug reactions: Definitions, diagnosis, and management. Lancet Lond. Engl. 2000;356:1255–1259. doi: 10.1016/S0140-6736(00)02799-9. [DOI] [PubMed] [Google Scholar]
- 17.Pichler W. Drug allergy: Classification and clinical features. In: Adkinson N.F., Feldweg A.M., editors. UpToDate. UpToDate; Waltham, MA, USA: 2016. [Google Scholar]
- 18.Yun J., Mattsson J., Schnyder K., Fontana S., Largiadèr C.R., Pichler W.J., Yerly D. Allopurinol hypersensitivity is primarily mediated by dose-dependent oxypurinol-specific T cell response. Clin. Exp. Allergy. 2013;43:1246–1255. doi: 10.1111/cea.12184. [DOI] [PubMed] [Google Scholar]
- 19.Stamp L.K., Taylor W.J., Jones P.B., Dockerty J.L., Drake J., Frampton C., Dalbeth N. Starting dose is a risk factor for allopurinol hypersensitivity syndrome: A proposed safe starting dose of allopurinol. Arthritis Rheum. 2012;64:2529–2536. doi: 10.1002/art.34488. [DOI] [PubMed] [Google Scholar]
- 20.Hennino A., Bérard F., Guillot I., Saad N., Rozières A., Nicolas J.-F. Pathophysiology of urticaria. Clin. Rev. Allergy Immunol. 2006;30:3–11. doi: 10.1385/CRIAI:30:1:003. [DOI] [PubMed] [Google Scholar]
- 21.D’Andrea M.R., Rogahn C.J., Andrade-Gordon P. Localization of protease-activated receptors-1 and -2 in human mast cells: Indications for an amplified mast cell degranulation cascade. Biotech. Histochem. 2000;75:85–90. doi: 10.3109/10520290009064152. [DOI] [PubMed] [Google Scholar]
- 22.Subramanian H., Gupta K., Ali H. Roles of Mas-related G protein-coupled receptor X2 on mast cell-mediated host defense, pseudoallergic drug reactions, and chronic inflammatory diseases. J. Allergy Clin. Immunol. 2016;138:700–710. doi: 10.1016/j.jaci.2016.04.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Marshall J.S. Mast-cell responses to pathogens. Nat. Rev. Immunol. 2004;4:787–799. doi: 10.1038/nri1460. [DOI] [PubMed] [Google Scholar]
- 24.Zuberbier T., Pfrommer C., Specht K., Vieths S., Bastl-Borrmann R., Worm M., Henz B.M. Aromatic components of food as novel eliciting factors of pseudoallergic reactions in chronic urticaria. J. Allergy Clin. Immunol. 2002;109:343–348. doi: 10.1067/mai.2002.121309. [DOI] [PubMed] [Google Scholar]
- 25.Bonadonna P., Pagani M., Aberer W., Bilò M.B., Brockow K., Oude Elberink H., Garvey L., Mosbech H., Romano A., Zanotti R., et al. Drug hypersensitivity in clonal mast cell disorders: ENDA/EAACI position paper. Allergy. 2015;70:755–763. doi: 10.1111/all.12617. [DOI] [PubMed] [Google Scholar]
- 26.Zuberbier T., Asero R., Bindslev-Jensen C., Walter Canonica G., Church M.K., Giménez-Arnau A.M., Grattan C.E.H., Kapp A., Maurer M., Merk H.F., et al. Dermatology Section of the European Academy of Allergology and Clinical Immunology; Global Allergy and Asthma European Network; European Dermatology Forum; World Allergy Organization EAACI/GA (2) LEN/EDF/WAO guideline: Management of urticaria. Allergy. 2009;64:1427–1443. doi: 10.1111/j.1398-9995.2009.02178.x. [DOI] [PubMed] [Google Scholar]
- 27.Zuberbier T., Chantraine-Hess S., Hartmann K., Czarnetzki B.M. Pseudoallergen-free diet in the treatment of chronic urticaria. A prospective study. Acta Derm. Venereol. 1995;75:484–487. doi: 10.2340/0001555575484487. [DOI] [PubMed] [Google Scholar]
- 28.Dewachter P., Castells M.C., Hepner D.L., Mouton-Faivre C. Perioperative management of patients with mastocytosis. Anesthesiology. 2014;120:753–759. doi: 10.1097/ALN.0000000000000031. [DOI] [PubMed] [Google Scholar]
- 29.Baldo B.A., Fisher M.M., Pham N.H. On the origin and specificity of antibodies to neuromuscular blocking (muscle relaxant) drugs: An immunochemical perspective. Clin. Exp. Allergy. 2009;39:325–344. doi: 10.1111/j.1365-2222.2008.03171.x. [DOI] [PubMed] [Google Scholar]
- 30.Moss J. Muscle relaxants and histamine release. Acta Anaesthesiol. Scand. Suppl. 1995;106:7–12. doi: 10.1111/j.1399-6576.1995.tb04301.x. [DOI] [PubMed] [Google Scholar]
- 31.Claudius C., Garvey L.H., Viby-Mogensen J. The undesirable effects of neuromuscular blocking drugs. Anaesthesia. 2009;64(Suppl. S1):10–21. doi: 10.1111/j.1365-2044.2008.05866.x. [DOI] [PubMed] [Google Scholar]
- 32.Florvaag E., Johansson S.G.O., Irgens Å., de Pater G.H. IgE-sensitization to the cough suppressant pholcodine and the effects of its withdrawal from the Norwegian market. Allergy. 2011;66:955–960. doi: 10.1111/j.1398-9995.2010.02518.x. [DOI] [PubMed] [Google Scholar]
- 33.Florvaag E., Johansson S.G.O., Oman H., Harboe T., Nopp A. Pholcodine stimulates a dramatic increase of IgE in IgE-sensitized individuals. A pilot study. Allergy. 2006;61:49–55. doi: 10.1111/j.1398-9995.2005.00933.x. [DOI] [PubMed] [Google Scholar]
- 34.Kaminsky E.B., Kaul V., Paschall J., Church D.M., Bunke B., Kunig D., Moreno-De-Luca D., Moreno-De-Luca A., Mulle J.G., Warren S.T., et al. An evidence-based approach to establish the functional and clinical significance of copy number variants in intellectual and developmental disabilities. Genet. Med. 2011;13:777–784. doi: 10.1097/GIM.0b013e31822c79f9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Miller D.T., Adam M.P., Aradhya S., Biesecker L.G., Brothman A.R., Carter N.P., Church D.M., Crolla J.A., Eichler E.E., Epstein C.J., et al. Consensus statement: Chromosomal microarray is a first-tier clinical diagnostic test for individuals with developmental disabilities or congenital anomalies. Am. J. Hum. Genet. 2010;86:749–764. doi: 10.1016/j.ajhg.2010.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yang S., Liu Y., Lin A.A., Cavalli-Sforza L.L., Zhao Z., Su B. Adaptive evolution of MRGX2, a human sensory neuron specific gene involved in nociception. Gene. 2005;352:30–35. doi: 10.1016/j.gene.2005.03.001. [DOI] [PubMed] [Google Scholar]
- 37.Nel L., Eren E. Peri-operative anaphylaxis. Br. J. Clin. Pharmacol. 2011;71:647–658. doi: 10.1111/j.1365-2125.2011.03913.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Galvão V.R., Giavina-Bianchi P., Castells M. Perioperative anaphylaxis. Curr. Allergy Asthma Rep. 2014;14:452. doi: 10.1007/s11882-014-0452-6. [DOI] [PubMed] [Google Scholar]
- 39.Laxenaire M.C., Mertes P.M. Groupe d’Etudes des Réactions Anaphylactoïdes Peranesthésiques Anaphylaxis during anaesthesia. Results of a two-year survey in France. Br. J. Anaesth. 2001;87:549–558. doi: 10.1093/bja/87.4.549. [DOI] [PubMed] [Google Scholar]
- 40.Fisher M.M., Munro I. Life-threatening anaphylactoid reactions to muscle relaxants. Anesth. Anal. 1983;62:559–564. doi: 10.1213/00000539-198306000-00003. [DOI] [PubMed] [Google Scholar]
- 41.Spoerl D., D’Incau S., Roux-Lombard P., Harr T., Czarnetzki C. Non-IgE-Dependent Hypersensitivity to Rocuronium Reversed by Sugammadex: Report of Three Cases and Hypothesis on the Underlying Mechanism. Int. Arch. Allergy Immunol. 2016;169:256–262. doi: 10.1159/000446182. [DOI] [PubMed] [Google Scholar]
- 42.Fisher M.M., Merefield D., Baldo B. Failure to prevent an anaphylactic reaction to a second neuromuscular blocking drug during anaesthesia. Br. J. Anaesth. 1999;82:770–773. doi: 10.1093/bja/82.5.770. [DOI] [PubMed] [Google Scholar]
- 43.Leysen J., Uyttebroek A., Sabato V., Bridts C.H., de Clerck L.S., Ebo D.G. Predictive value of allergy tests for neuromuscular blocking agents: Tackling an unmet need. Clin. Exp. Allergy. 2014;44:1069–1075. doi: 10.1111/cea.12344. [DOI] [PubMed] [Google Scholar]
- 44.Hagau N., Gherman-Ionica N., Sfichi M., Petrisor C. Threshold for basophil activation test positivity in neuromuscular blocking agents hypersensitivity reactions. Allergy Asthma Clin. Immunol. 2013;9:42. doi: 10.1186/1710-1492-9-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dong S.W., Mertes P.M., Petitpain N., Hasdenteufel F., Malinovsky J.M. GERAP Hypersensitivity reactions during anesthesia. Results from the ninth French survey (2005–2007) Minerva Anestesiol. 2012;78:868–878. [PubMed] [Google Scholar]
- 46.Mertes P.-M., Laxenaire M.-C. GERAP (Anaphylactic and anaphylactoid reactions occurring during anaesthesia in France. Seventh epidemiologic survey (January 2001–December 2002)) Ann. Fr. Anesth. Reanim. 2004;23:1133–1143. doi: 10.1016/j.annfar.2004.10.013. [DOI] [PubMed] [Google Scholar]
- 47.Harboe T., Guttormsen A.B., Irgens A., Dybendal T., Florvaag E. Anaphylaxis during anesthesia in Norway: A 6-year single-center follow-up study. Anesthesiology. 2005;102:897–903. doi: 10.1097/00000542-200505000-00006. [DOI] [PubMed] [Google Scholar]
- 48.Karila C., Brunet-Langot D., Labbez F., Jacqmarcq O., Ponvert C., Paupe J., Scheinmann P., de Blic J. Anaphylaxis during anesthesia: Results of a 12-year survey at a French pediatric center. Allergy. 2005;60:828–834. doi: 10.1111/j.1398-9995.2005.00787.x. [DOI] [PubMed] [Google Scholar]
- 49.Kvedariene V., Kamey S., Ryckwaert Y., Rongier M., Bousquet J., Demoly P., Arnoux B. Diagnosis of neuromuscular blocking agent hypersensitivity reactions using cytofluorimetric analysis of basophils. Allergy. 2006;61:311–315. doi: 10.1111/j.1398-9995.2006.00978.x. [DOI] [PubMed] [Google Scholar]
- 50.Chong Y.Y., Caballero M.R., Lukawska J., Dugué P. Anaphylaxis during general anaesthesia: One-year survey from a British allergy clinic. Singap. Med. J. 2008;49:483–487. [PubMed] [Google Scholar]
- 51.Laroche D., Chollet-Martin S., Léturgie P., Malzac L., Vergnaud M.-C., Neukirch C., Venemalm L., Guéant J.-L., Roland P.N. Evaluation of a new routine diagnostic test for immunoglobulin E sensitization to neuromuscular blocking agents. Anesthesiology. 2011;114:91–97. doi: 10.1097/ALN.0b013e31820164d2. [DOI] [PubMed] [Google Scholar]
- 52.Aalberse R.C., Kleine Budde I., Mulder M., Stapel S.O., Paulij W., Leynadier F., Hollmann M.W. Differentiating the cellular and humoral components of neuromuscular blocking agent-induced anaphylactic reactions in patients undergoing anaesthesia. Br. J. Anaesth. 2011;106:665–674. doi: 10.1093/bja/aer028. [DOI] [PubMed] [Google Scholar]
- 53.Ramirez L.F., Pereira A., Chiriac A.M., Bonnet-Boyer M.-C., Demoly P. Negative predictive value of skin tests to neuromuscular blocking agents. Allergy. 2012;67:439–441. doi: 10.1111/j.1398-9995.2011.02753.x. [DOI] [PubMed] [Google Scholar]
- 54.Antunes J., Kochuyt A.-M., Ceuppens J.L. Perioperative allergic reactions: Experience in a Flemish referral centre. Allergol. Immunopathol. Madr. 2014;42:348–354. doi: 10.1016/j.aller.2013.08.001. [DOI] [PubMed] [Google Scholar]
- 55.Krishna M.T., York M., Chin T., Gnanakumaran G., Heslegrave J., Derbridge C., Huissoon A., Diwakar L., Eren E., Crossman R.J., et al. Multi-centre retrospective analysis of anaphylaxis during general anaesthesia in the United Kingdom: Aetiology and diagnostic performance of acute serum tryptase. Clin. Exp. Immunol. 2014;178:399–404. doi: 10.1111/cei.12424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Soetens F.M., Smolders F.J., Meeuwis H.C., Van der Donck A.G., van der Aa P.H., De Vel M.A., Vanhoof M.J., Soetens M.A. Intradermal skin testing in the investigation of suspected anaphylactic reactions during anaesthesia—A retrospective survey. Acta Anaesthesiol. Belg. 2003;54:59–63. [PubMed] [Google Scholar]
- 57.Hagau N., Gherman N., Cocis M., Petrisor C. Antibiotic-induced immediate type hypersensitivity is a risk factor for positive allergy skin tests for neuromuscular blocking agents. Allergol. Int. 2016;65:52–55. doi: 10.1016/j.alit.2015.07.007. [DOI] [PubMed] [Google Scholar]
- 58.Berg C.M., Heier T., Wilhelmsen V., Florvaag E. Rocuronium and cisatracurium-positive skin tests in non-allergic volunteers: Determination of drug concentration thresholds using a dilution titration technique. Acta Anaesthesiol. Scand. 2003;47:576–582. doi: 10.1034/j.1399-6576.2003.00093.x. [DOI] [PubMed] [Google Scholar]
- 59.Reddy J.I., Cooke P.J., van Schalkwyk J.M., Hannam J.A., Fitzharris P., Mitchell S.J. Anaphylaxis is more common with rocuronium and succinylcholine than with atracurium. Anesthesiology. 2015;122:39–45. doi: 10.1097/ALN.0000000000000512. [DOI] [PubMed] [Google Scholar]
- 60.Veien M., Szlam F., Holden J.T., Yamaguchi K., Denson D.D., Levy J.H. Mechanisms of nonimmunological histamine and tryptase release from human cutaneous mast cells. Anesthesiology. 2000;92:1074–1081. doi: 10.1097/00000542-200004000-00026. [DOI] [PubMed] [Google Scholar]
- 61.Marone G., Stellato C., Mastronardi P., Mazzarella B. Mechanisms of activation of human mast cells and basophils by general anesthetic drugs. Ann. Fr. Anesth. Reanim. 1993;12:116–125. doi: 10.1016/S0750-7658(05)81020-2. [DOI] [PubMed] [Google Scholar]
- 62.Uyttebroek A.P., Sabato V., Leysen J., Bridts C.H., De Clerck L.S., Ebo D.G. Flowcytometric diagnosis of atracurium-induced anaphylaxis. Allergy. 2014;69:1324–1332. doi: 10.1111/all.12468. [DOI] [PubMed] [Google Scholar]
- 63.Leysen J., de Witte L., Sabato V., Faber M., Hagendorens M., Bridts C., de Clerck L., Ebo D. IgE-mediated allergy to pholcodine and cross-reactivity to neuromuscular blocking agents: Lessons from flow cytometry. Cytom. B Clin. Cytom. 2013;84:65–70. doi: 10.1002/cyto.b.21074. [DOI] [PubMed] [Google Scholar]
- 64.Fisher M.M., Baldo B.A. Immunoassays in the diagnosis of anaphylaxis to neuromuscular blocking drugs: The value of morphine for the detection of IgE antibodies in allergic subjects. Anaesth. Intensive Care. 2000;28:167–170. doi: 10.1177/0310057X0002800207. [DOI] [PubMed] [Google Scholar]
- 65.Decuyper I.I., Ebo D.G., Uyttebroek A.P., Hagendorens M.M., Faber M.A., Bridts C.H., de Clerck L.S., Sabato V. Quantification of specific IgE antibodies in immediate drug hypersensitivity: More shortcomings than potentials? Clin. Chim. Acta. 2016;460:184–189. doi: 10.1016/j.cca.2016.06.043. [DOI] [PubMed] [Google Scholar]
- 66.Baldo B.A., Fisher M.M. Substituted ammonium ions as allergenic determinants in drug allergy. Nature. 1983;306:262–264. doi: 10.1038/306262a0. [DOI] [PubMed] [Google Scholar]
- 67.Ebo D.G., Bridts C.H., Hagendorens M.M., Mertens C.H., de Clerck L.S., Stevens W.J. Flow-assisted diagnostic management of anaphylaxis from rocuronium bromide. Allergy. 2006;61:935–939. doi: 10.1111/j.1398-9995.2006.01094.x. [DOI] [PubMed] [Google Scholar]
- 68.Sabato V., van Gasse A., Cop N., Claesen K., Decuyper I.I., Faber M.A., Bridts C., Mertens C., Hagendorens M., de Clerck L., et al. The Mas-Related G Protein-Coupled Receptor MRGPRX2 Is Expressed on Human Basophils and up-Regulated upon Activation; Proceedings of the AAAAI Conference; Atlanta, GA, USA. 3–6 March 2017; Abstract 536. [Google Scholar]
- 69.Johansson S.G.O., Oman H., Degerbeck F., Tunelli J., Florvaag E., Nopp A. Anaphylaxis to atracurium—A non-QAI-dependent reaction? Acta Anaesthesiol. Scand. 2012;56:262–263. doi: 10.1111/j.1399-6576.2011.02598.x. [DOI] [PubMed] [Google Scholar]
- 70.Uyttebroek A.P., Sabato V., Bridts C.H., De Clerck L.S., Ebo D.G. Immunoglobulin E antibodies to atracurium: A new diagnostic tool? Clin. Exp. Allergy J. Br. Soc. Allergy Clin. Immunol. 2015;45:485–487. doi: 10.1111/cea.12448. [DOI] [PubMed] [Google Scholar]
- 71.Naguib M., Samarkandi A.H., Bakhamees H.S., Magboul M.A., El-Bakry A.K. Histamine-release haemodynamic changes produced by rocuronium, vecuronium, mivacurium, atracurium and tubocurarine. Br. J. Anaesth. 1995;75:588–592. doi: 10.1093/bja/75.5.588. [DOI] [PubMed] [Google Scholar]