Abstract
The spleen plays an important role in coordinating both adaptive and innate immune responses. Here, the transcriptional response to T. gondii infection in the murine spleen was characterized concerning inflammasome sensors (two different models: seven days after oral or four weeks after intraperitoneal infection). Additionally, Tff1KO and Tff3KO mice were investigated because TFF genes are often upregulated during inflammation. The expression of the pattern-recognition receptors Nlrp3, Nlrp12, and Nlrp1a was significantly increased after infection. This increase was diminished in Tff1KO and Tff3KO mice pointing towards a positive regulation of the inflammatory response by Tff1 and Tff3. Furthermore, the transcription of Tff1 (encoding a motogenic lectin) and other secretory genes was analyzed, i.e., gastrokines (Gkn), IgG Fc binding protein (Fcgbp), and the mucin Muc2. The corresponding gene products belong to an interactome protecting mucous epithelia. Tff1 was significantly induced after infection, which might increase the motility of immune cells. In contrast, Gkn3, Fcgbp, and Muc2 were downregulated seven days after oral infection; whereas four weeks after i.p. infection only Gkn3 remained downregulated. This might be an indication that Gkn3, Fcgbp, and Muc2 are involved in the transient disruption of the splenic architecture and its reorganization, which is characteristic after T. gondii infection.
Keywords: inflammation, inflammasome, TFF1, trefoil factor, Toxoplasma gondii, gastrokine, IgG Fc binding protein, MUC2
1. Introduction
The spleen is the largest secondary lymphoid organ of the body with various functions, the immune function being the most important one [1,2]. Here, phagocytosis, T cell-mediated immunity, and B cell-mediated humoral immunity occur mainly in the white pulp and the marginal zone of the spleen. The red pulp of the spleen is a major blood filter, is also involved in phagocytosis, and is a key site for iron metabolism; the latter being also a prerequisite particularly for the oxidizing function of monocytes.
The spleen is also a rich source for endocrine secretions, e.g., it is a key player in the “cytokine storm” that develops after infection and trauma [3,4]. For example, tumor necrosis factor (TNF)-α is produced in the spleen in high amounts and individuals having undergone splenectomy are highly susceptible to infections [5,6]. Of note, vagus nerve stimulation inhibits TNF-α production in the spleen at the transcriptional level by signaling through the α7 nicotinic acetylcholine receptor subunit [5]. Calcitonin gene-related peptide and β-endorphin are other endocrine peptides of the spleen [7,8]. Furthermore, the spleen also participates in metabolic and immunological abnormalities described in obesity, and splenectomy attenuates the progression of obesity and decreases insulin hypersecretion [9].
Toxoplasma gondii is a pathogen that infects all types of warm-blooded vertebrates. The parasite spreads by migration across biological barriers such as the intestine, the blood-brain barrier, the blood-retina barrier, and the placenta [10]. The host immune system plays a critical role in the response to T. gondii infection [11,12,13]. Immune factors involved in controlling T. gondii infection are, e.g., interleukin (IL)-6, IL-10, IL-12, IL-33, and interferon (IFN)-γ [4]. In humans, infections are normally subclinical and severe complications occur in immunocompromised patients and because of congenital infection. Recently, cytokine expression in the murine spleen has been investigated after intraperitoneal (i.p.) or oral T. gondii infection [4,14]. Of note, all the differentially expressed chemokines were upregulated; whereas most of the differentially expressed chemokine receptors were downregulated [4]. Furthermore, T. gondii infection caused a changed miRNA regulation network in mouse spleen as well as transcriptional changes of splenocyte organelle components [15,16].
In the past, we could show that i.p. T. gondii infection caused a significant induction of pattern-recognition receptors (PRRs) in the brain, particularly members of the NOD-like receptors and of the HIN200 family [17]. These intracellular sensors are, together with procaspase-1 and the adaptor protein ASC, typical constituents of inflammasomes [18,19,20]. Inflammasome activation leads to maturation of caspase-1 and the processing of the proinflammatory cytokines, IL-1β and IL-18. Thus, T. gondii effectors are master regulators of the inflammatory response and the inflammasome pathway [13]. However, there are no reports systematically analyzing the expression of inflammasome sensors in the spleen. Thus, we present here first data describing the expression of inflammasome sensors in the murine spleen in two different models of T. gondii infection, i.e., after oral (established ileitis model) or i.p. infection (established encephalitis model).
The two mouse models have been described in previous studies, where trefoil factor family 3 (Tff3)-deficient (Tff3KO) mice were also investigated after oral T. gondii infection (ileitis model) and Tff1KO mice after i.p. T. gondii infection (encephalitis model), respectively [14,17]. In the present study, we continued our previous work and investigated the spleen of Tff3KO mice after oral T. gondii infection because Tff3 is known to be expressed also in the spleen [14,21,22]. Furthermore, we investigated the spleen of Tff1KO mice after i.p. T. gondii infection because Tff1 expression is known to be upregulated in the spleen after oral T. gondii infection [14]. Generally, TFF peptides (TFF1-3) are secretory lectins, which are expressed in mucous epithelia as well as the immune and the central nervous systems [21,23,24,25,26,27]. In the present study, other than inflammasome sensors, the splenic expression of Tff1 and diverse secretory genes associated with Tffs, such as gastrokines (Gkn), IgG Fc binding protein (Fcgbp), and the mucin Muc2, was investigated. The corresponding gene products belong to an interactome protecting mucous epithelia. Particularly interesting is the expression of TFF1 because it has been shown to be typically upregulated during various chronic inflammatory processes [14,17].
2. Results
2.1. Expression Profiling of Mouse Spleen after Oral T. gondii Infection
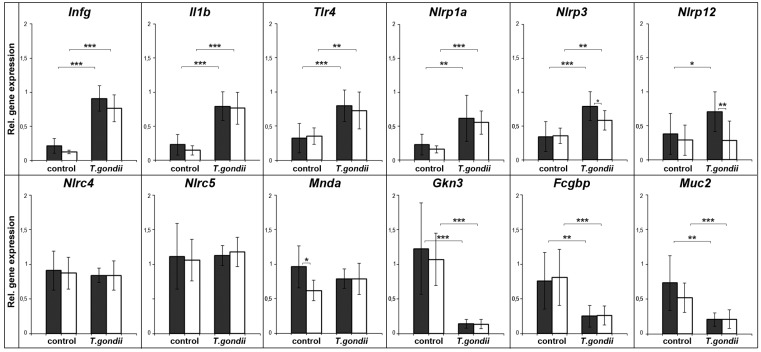
The expression of typical inflammatory marker genes was analyzed (validated by semi-quantitative evaluation) in wild type and in Tff3KO animals seven days after oral T. gondii infection (Figure 1). To monitor the inflammatory process, signature genes such as interferon γ (Ifnγ), Il1β, and Tlr4 were selected. As expected, these genes were significantly upregulated after T. gondii infection. The expression analysis of transcripts encoding the inflammasome constituents Nlrp1a, Nlrp3, Nlrp12, Nlrc4, Nlrc5, and Mnda revealed that Nlrp1a, Nlrp3, and Nlrp12 were significantly upregulated in T. gondii infected animals. Of note, Nlrp12 was only upregulated in wild type animals, but not in Tff3KO mice. In contrast, the expression of the inflammasome sensors—Nlrc4, Nlrc5, and Mnda—was not changed significantly after T. gondii infection.
Figure 1.
Semiquantitative RT-PCR analyses. Ifng (24×), Il1b (27×), Tlr4 (31×), Nlrp1a (33×), Nlrp3 (33×), Nlrp12 (35×), Nlrc4 (32×), Nlrc5 (32×), Mnda (32×), Gkn3 (35×), Fcgbp (35×), and Muc2 (35×) expression was monitored in the spleen seven days after oral T. gondii infection (ileitis model; 8 wild type and 11 Tff3KO mice, respectively). As a control, the spleens of non-infected animals (nine wild type and nine Tff3KO mice, respectively) were investigated. The relative gene expression levels were normalized against β-actin (Actb, 20×). The number of amplification cycles is given in parentheses. Significances are indicated by asterisks (*, p ≤ 0.05; **, p ≤ 0.01; ***, p ≤ 0.001). Wild type animals: black bars; Tff3KO animals: white bars.
Furthermore, the expression of genes associated with TFF peptides and mucous epithelia—such as Gkn3, Fcgbp, and Muc2—was analyzed. These three genes were significantly downregulated after T. gondii infection.
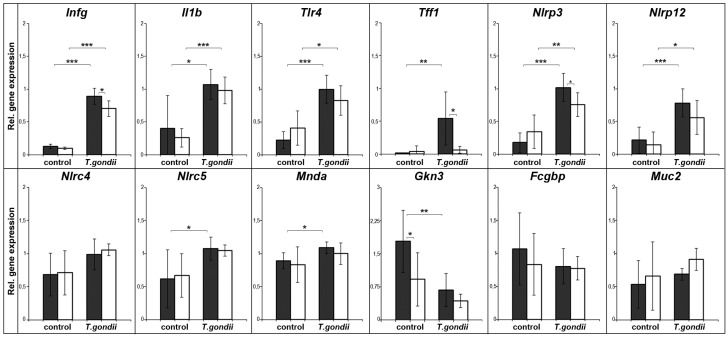
2.2. Expression Profiling of Mouse Spleen after Intraperitoneal T. gondii Infection
The expression of a similar set of genes was also analyzed in wild type and Tff1KO animals four weeks after intraperitoneal T. gondii infection (Figure 2). Again, the inflammatory markers Ifnγ, Il1β, and Tlr4 were significantly upregulated in the infected animals. Furthermore, Tff1 was significantly upregulated after T. gondii infection as well as expression of the inflammasome constituents Nlrp3 and Nlrp12; whereas the expression of the inflammasome sensor Nlrc4 did not show a significant change compared to the moderate upregulation of Nlrc5 and Mnda. In contrast to Fcgbp and Muc2, only Gkn3 was significantly downregulated in infected animals.
Figure 2.
Semiquantitative RT-PCR analyses. Ifng (30×), Il1b (27×), Tlr4 (32×), Tff1 (32×), Nlrp3 (33×), Nlrp12 (35×), Nlrc4 (33×), Nlrc5 (33×), Mnda (33×), Gkn3 (35×), Fcgbp (35×), and Muc2 (35×) expression was monitored in the spleen four weeks after i.p. T. gondii infection (encephalitis model; six wild type and six Tff1KO mice, respectively). As a control, the spleen of non-infected animals (six wild type and six Tff1KO mice, respectively) was investigated. The relative gene expression levels were normalized against β-actin (Actb, 22×). The number of amplification cycles is given in parentheses. Significances are indicated by asterisks (*, p ≤ 0.05; **, p ≤ 0.01; ***, p ≤ 0.001). Wild type animals: black bars; Tff1KO animals: white bars.
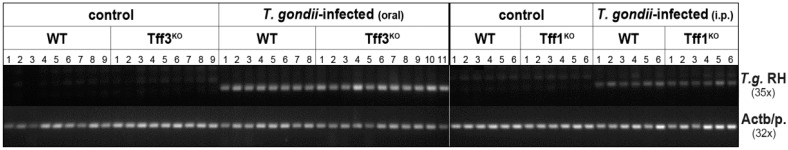
In order to confirm infection of the animals with T. gondii, the presence of the RH repeat region of T. gondii was monitored in the spleen in both infection models (Figure 3). Clearly, only the infected animals contained this DNA.
Figure 3.
PCR analyses of genomic DNA from the spleen for the T. gondii RH strain repeat region (T.g. RH). T. gondii DNA was monitored seven days after oral T. gondii infection and four weeks after i.p. infection, respectively. As a control, DNA from the β-actin promoter (Actb/p.) was amplified. The number of amplification cycles is given in parentheses.
3. Discussion
3.1. T. gondii Infection Induces the Expression of Specific Inflammasomes in the Spleen
In both experimental models, Ifnγ, Il1β, and Tlr4 were upregulated in the spleen (Figure 1 and Figure 2). This is in line with previous reports describing increased splenic expression of these genes after T. gondii infection [4,14,28,29,30]. In human monocytes, particularly the secreted GRA15 protein of T. gondii is responsible for IL-1β induction and the release of IL-1β is a direct consequence of inflammasome activation after infection [31]. Thus, these genes serve as positive controls indicating inflammatory processes in the spleen after T. gondii infection in our experimental studies presented here. Furthermore, also expression of the T. gondii RH repeat region confirms the infection of the spleen (Figure 3).
Expression of the inflammasome sensors Nlrp3 and Nlrp12 is significantly increased (p ≤ 0.001) in both models of T. gondii infection (wild type animals). Of note, the upregulation of Nlrp3 and Nlrp12 in infected Tff3KO and Tff1KO animals is reduced when compared to the corresponding wild type animals. This might be an indication that Tff1 and Tff3 positively regulate the inflammatory process. This view is supported by the observation that Tff3KO mice showed a reduced immune response in the ileum after oral T. gondii infection [14].
Furthermore, also Nlrp1a expression was significantly upregulated (p ≤ 0.001) seven days after oral T. gondii infection (animals with mixed 129/Sv and C57BL/6 background; Figure 1). In contrast, Nlrp1a expression was not detectable in the strains used for i.p. infection (129/Sv background). This is in line with previous reports that Nlrp1a and Nlrp1c expression is lacking in certain 129S1 mouse strains [17,32].
In contrast, Nlrc4 expression (and Nlrc5 and Mnda seven days after T. gondii infection) was not changed. Similar results were obtained for Nlrp6 and Aim2 (data not shown). Generally, the picture emerges that PRR expression after T. gondii infection is rather moderate, slow, and focal in the spleen, predominantly affecting Nlrp3 and Nlrp12. This is in contrast to the expression pattern in the brain four weeks after i.p. T. gondii infection, where at least Nlrp3, Nlrc4, Nlrc5, and Mnda were strongly upregulated (p ≤ 0.001) [17].
3.2. Splenic Tff1 Expression is Induced in Two Models of T. gondii Infection
Tff1 expression in the spleen was significantly induced (p ≤ 0.01) four weeks after i.p. T. gondii infection (Figure 2). This result is in agreement with a previous study showing significantly induced Tff1 expression in the spleen also seven days after oral T. gondii infection [14]. Thus, Tff1 is ectopically expressed in the inflamed spleen in two different models after T. gondii infection.
Taken together, this result is in line with ectopic TFF1 expression during various inflammatory processes, such as in the brain in an encephalitis model [17], in a murine ileitis model [14], during chronic intestinal ulceration [33], chronic pancreatitis [34], in the colon of infants with inflammatory bowel disease [35], in the porcine colon after infection with Salmonella typhimurium [36], and in a murine asthma model [37,38].
The upregulated Tff1 expression in the spleen after T. gondii infection is correlated with a complex inflammatory process. A primary response of the spleen is obviously the formation of inflammasomes (particularly Nlrp3 and Nlrp12) as shown in Figure 1 and Figure 2. Then, the release of IL1β and IL18 probably triggers NF-κB-dependent transcriptional events [19]. Induction of Tff1 expression as a consequence of TNF-α and IL1β stimulation and activation of NF-κB has been documented [39,40]. The specific upregulation of Tff1, but not of Tff2 and Tff3, could have been brought forth via FoxA (formerly: hepatocyte nuclear factor 3) and binding to motif IV [17,41,42,43]. Of note, FoxA expression is upregulated particularly by inflammatory cytokines [44].
Finally, the question arises concerning the biological function of ectopic TFF1 expression during inflammatory processes. TFF1 has been reported to have protective and healing effects to mucous epithelia and acts as a motogen (for reviews, see [21,23,24]); furthermore, it has a pH-dependent lectin activity [45]. Thus, Tff1 could influence, for example, the motility of certain immune cells. The reduced inflammatory response in Tff1KO animals (especially concerning the expression of Ifnγ and Nlrp3; Figure 2) after i.p. T. gondii infection points towards a positive regulation of the inflammatory response by Tff1 in order to protect the organ against invasion of pathogens. Of note, a similar effect has been observed in Tff3KO animals after oral T. gondii infection (particularly concerning Nlrp3, Nlrp12; Figure 1).
3.3. Changes of Other Secretory Genes in the Spleen after T. gondii Infection
Trefoil factor family (TFF) peptides are typical constituents of mucous gels and are also secreted from the central nervous system as well as the immune system [21,23,24,25,26,27]. In the spleen, particularly TFF2 and TFF3 are expressed [14,22,46,47]. The biosynthesis of TFF1 and TFF3 is complex; both are secretory peptides containing an odd number of cysteine residues and are able to form disulfide-linked heterodimers with GKN2 and FCGBP, respectively [48,49,50]. Thus, in the studies presented here the expression of secretory gastrokines, Fcgbp, and the gel-forming mucin Muc2—which are typically co-expressed in mucous epithelia—were monitored at the transcriptional level.
Surprisingly, Gkn3, Fcgbp, and Muc2 were significantly downregulated (p ≤ 0.001) seven days after oral T. gondii infection (Figure 1); whereas four weeks after i.p. T. gondii infection, only Gkn3 was downregulated (p ≤ 0.01). In contrast, the expression of Gkn1 and Gkn2 was hardly detectable in non-infected mice and rather increased little for Gkn2 after infection, particularly in Tff1KO mice (data not shown). Thus, the expression of Gkn3, Fcgbp, and Muc2 is contrary to that of inflammatory genes. Furthermore, it seems that their downregulation is a rather transient and quick response, because the effect is most prominent in the acute infection and seems to be attenuated in chronic infection after four weeks (only Gkn3 is still significantly downregulated; however, one has to consider that different T. gondii strains were used in the two experimental models). Currently, the function of these genes in the spleen is not known and this is the first description of their transcription in this organ. Gkn3 has been reported to inhibit gastric epithelial cell proliferation and probably marks a distinct neck cell precursor population [51]. Thus, Gkn3 could reduce the number of cell divisions, which is known to be very low in the spleen [52]. Of note, GKN3 function has been lost in humans [51]. Fcgbp is an IgG Fc binding protein, which is entirely different from Fcγ receptors, and is able to attach covalently to the mucin Muc2 [53,54]. Of special note, it has been postulated that Fcgbp traps HIV-1-antibody complexes at mucosal surfaces [55]. Thus, Fcgbp and Muc2 would be perfectly designed to establish an extracellular matrix with a barrier or adhesive function, particularly for immunoglobulins. Such a molecular function would be in agreement with the physiological role of the spleen. Furthermore, infection with T. gondii is known to induce a transient disruption of the splenic architecture [56]. As a consequence, the transiently reduced expression of Gkn3, Fcgbp, and Muc2 after T. gondii infection could well be a sign, that these genes are involved in the splenic reorganization.
Furthermore, the expression of ependymin related protein 1 (Epdr1, previously termed Merp2) was monitored, because it was downregulated in a murine asthma model [37]. Epdr1 probably encodes a lysosomal protein [57] homologous to human UCC1/MERP1 [58]. In both models, Epdr1 transcript levels did not significantly change after T. gondii infection (data not shown). This is comparable to a constant cerebral Epdr1 expression after i.p. T. gondii infection [17].
Analysis of the cellular localization of Tff1, Gkn3, Fcgbp, and Muc2 might be an interesting topic for further studies in order to gain more insights into the molecular functions of these new players in splenic function.
4. Materials and Methods
4.1. Murine T. gondii Infection Models
Two infection models described in detail previously [14,17] were applied for the studies presented here. First, corresponding wild type and Tff3KO animals (mixed 129/Sv and C57BL/6 background), respectively were orally infected with three cysts of a type II strain (ME49) per mouse (ileitis model) and seven days post-infection the spleen was collected as described [14]. Second, corresponding wild type and Tff1KO animals (129/Sv background) were i.p. infected with five cysts of the type II DX strain per mouse (encephalitis model) and, four weeks post-infection, the spleen was collected as reported [17]. Procedures concerning animal care and the generation of data from animal samples were according to legal regulations; T. gondii infection studies were approved by the responsible state authorities (No. 42502-2-1233 UniMD, 01/2014 and 12/2016; No. 42502-2-1004 UniMD, 09/2010, 11/2013, 03/2015; Landesverwaltungsamt Sachsen-Anhalt, Halle, Germany).
4.2. DNA and RNA Extraction, PCR Analysis
Genotyping the different mouse strains from tail clippings was as previously described [14,17]. Infection of the spleen with T. gondii was monitored by amplifying the T. gondii RH strain repeat region from 150 ng genomic DNA from the spleen. The specific primer pairs used have been published previously (Actb/promoter, MB1783/MB1784; [14]) or are listed in Table 1 (RH repeat region, MB2066/MB2067).
Table 1.
Oligonucleotides used for (RT)-PCR analysis and calculated size of the products.
| Genes | Accession No. | Primer No. | Primer Pairs | Nucleotide Positions | Tm | Size (bp) | Intron Spanning |
|---|---|---|---|---|---|---|---|
| Fcgbp | NM_001122603.1 | MB1516 | CCAAAACCTGGAGATGAGGA | 6215–6234 | 60 °C | 621 | Yes |
| MB1517 | CAGGCTACGGCAGAGATAGG | 6835–6816 | |||||
| Gkn3 | NM_026860.1 | MB2656 MB2657 |
TGGTCAGCATCCGAGACAAC CATGAGTCTGGGTCCATCGT |
270–289 612–593 |
60 °C | 343 | Yes |
| Muc2 | NM_023566.3 | MB2660 MB2661 |
GCTCTTTCTTCCTACGCCCG CATGAAGGTATGGTCAGGGC |
1913–1933 2141–2122 |
60 °C | 228 | Yes |
| Nlrp12 | NM_001033431.1 | MB2606 MB2607 |
CCCGTTACTTTGTCCCCCAT CACGCTGATTGGCTCTCAAAA |
184–203 536–516 |
60 °C | 353 | Yes |
| Tlr4 | NM_021297.3 | MB1687 | AGAAAATGCCAGGATGATGC | 269–288 | 60 °C | 417 | Yes |
| MB1688 | GTCTCCACAGCCACCAGATT | 685–666 | |||||
| T. g. RH repeat region | AF487550.1 | MB2066 MB2067 |
ACTACAGACGCGATGCCGCTC CTCTCCGCCATCACCACGAGGAA |
107–127 328–306 |
60 °C | 222 |
The isolation of total RNA of murine tissues as well as RT-PCR analysis and semi-quantitative evaluation of relative gene expression levels including statistical analysis have already been described in detail [14,17]. The specific primer pairs used in this RT-PCR study have been also published previously (Actb, MB1912/MB1913; Ifnγ, MB2054/MB2055; Il1β, MB2038/MB2039; Tff1, MD7/MD8; Nlrp1a, MB2576/MB2577; Nlrp3, MB2584/MB2585; Nlrc4, MB2382/MB2383; Nlrc5, MB2608/MB2609; Mnda, MB2600/MB2601; [14,17]) or are listed in Table 1 (Fcgbp, Gkn3, Muc2, Nlrp12, Toll-like receptor/Tlr4).
5. Conclusions
In two different models of T. gondii infection (oral and i.p., respectively), the splenic expression of specific inflammasome sensor genes (Nlrp3, Nlrp12) was upregulated together with typical inflammatory marker genes (Ifng, Il1b, Tlr4). Of note, the inflammatory response was diminished in Tff1KO and Tff3KO mice, which points towards a pro-inflammatory role of Tff1 and Tff3. Furthermore, Tff1 expression was also significantly upregulated after T. gondii infection. This established again Tff1 as a marker gene for inflammatory processes. In contrast, the splenic expression of certain mucus-associated genes (Gkn3, Fcgbp, Muc2) was downregulated particularly seven days after oral T. gondii infection. This might be a sign that these genes are involved in the transient disruption of the splenic architecture and its reorganization after T. gondii infection.
Acknowledgments
The authors thank Dr. Marie-Christine Rio and Dr. Catherine Tomasetto (both IGBMC, Illkirch, France) for providing the mice heterozygous for Tff1, Prof. Daniel K. Podolsky (Harvard Medical School) for providing the Tff3KO animals, Dr. Luisa Möhle for her help with the infection studies, Prof. Dirk Schlüter and Prof. Ildiko R. Dunay for continued support, Daniela Lorenz for her help with the illustrations, and PD Jonathan Lindquist for critically reading the manuscript.
Author Contributions
Eva B. Znalesniak performed the RT-PCR analyses and analyzed the data, Ting Fu and Franz Salm contributed materials, Ulrike Händel infected animals, and Werner Hoffmann conceived and designed the experiments. The manuscript was written by Werner Hoffmann and commented on by all authors.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Tarantino G., Savastano S., Capone D., Colao A. Spleen: A new role for an old player? World J. Gastroenterol. 2011;17:3776–3784. doi: 10.3748/wjg.v17.i33.3776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bronte V., Pittet M.J. The spleen in local and systemic regulation of immunity. Immunity. 2013;39:806–818. doi: 10.1016/j.immuni.2013.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gigliotti J.C., Okusa M.D. The spleen: The forgotten organ in acute kidney injury of critical illness. Nephron. Clin. Pract. 2014;127:153–157. doi: 10.1159/000363255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.He J.J., Ma J., Song H.Q., Zhou D.H., Wang J.L., Huang S.Y., Zhu X.Q. Transcriptomic analysis of global changes in cytokine expression in mouse spleens following acute Toxoplasma gondii infection. Parasitol. Res. 2016;115:703–712. doi: 10.1007/s00436-015-4792-5. [DOI] [PubMed] [Google Scholar]
- 5.Huston J.M., Ochani M., Rosas-Ballina M., Liao H., Ochani K., Pavlov V.A., Gallowitsch-Puerta M., Ashok M., Czura C.J., Foxwell B., et al. Splenectomy inactivates the cholinergic antiinflammatory pathway during lethal endotoxemia and polymicrobial sepsis. J. Exp. Med. 2006;203:1623–1628. doi: 10.1084/jem.20052362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Garraud O., Borhis G., Badr G., Degrelle S., Pozzetto B., Cognasse F., Richard Y. Revisiting the B-cell compartment in mouse and humans: More than one B-cell subset exists in the marginal zone and beyond. BMC Immunol. 2012;13:63. doi: 10.1186/1471-2172-13-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Martins J.M., Banks W.A., Kastin A.J. Transport of CRH from mouse brain directly affects peripheral production of β-endorphin by the spleen. Am. J. Physiol. 1997;273:E1083–E1089. doi: 10.1152/ajpendo.1997.273.6.E1083. [DOI] [PubMed] [Google Scholar]
- 8.Wang H., Xing L., Li W., Hou L., Guo J., Wang X. Production and secretion of calcitonin gene-related peptide from human lymphocytes. J. Neuroimmunol. 2002;130:155–162. doi: 10.1016/S0165-5728(02)00221-7. [DOI] [PubMed] [Google Scholar]
- 9.Leite Nde C., Montes E.G., Fisher S.V., Cancian C.R., de Oliveira J.C., Martins-Pinge M.C., Kanunfre C.C., Souza K.L., Grassiolli S. Splenectomy attenuates obesity and decreases insulin hypersecretion in hypothalamic obese rats. Metabolism. 2015;64:1122–1133. doi: 10.1016/j.metabol.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 10.Barragan A., Sibley L.D. Migration of Toxoplasma gondii across biological barriers. Trends Microbiol. 2003;11:426–430. doi: 10.1016/S0966-842X(03)00205-1. [DOI] [PubMed] [Google Scholar]
- 11.Kasper L., Courret N., Darche S., Luangsay S., Mennechet F., Minns L., Rachinel N., Ronet C., Buzoni-Gatel D. Toxoplasma gondii and mucosal immunity. Int. J. Parasitol. 2004;34:401–409. doi: 10.1016/j.ijpara.2003.11.023. [DOI] [PubMed] [Google Scholar]
- 12.Dunay I.R., Sibley L.D. Monocytes mediate mucosal immunity to Toxoplasma gondii. Curr. Opin. Immunol. 2010;22:461–466. doi: 10.1016/j.coi.2010.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Melo M.B., Jensen K.D.C., Saeij J.P.J. Toxoplasma gondii effectors are master regulators of the inflammatory response. Trends Parasitol. 2011;27:487–495. doi: 10.1016/j.pt.2011.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fu T., Znalesniak E.B., Kalinski T., Möhle L., Biswas A., Salm F., Dunay I.R., Hoffmann W. TFF peptides play a role in the immune response following oral infection of mice with Toxoplasma gondii. Eur. J. Microbiol. Immunol. 2015;5:221–231. doi: 10.1556/1886.2015.00028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.He J.J., Ma J., Wang J.L., Xu M.J., Zhu X.Q. Analysis of miRNA expression profiling in mouse spleen affected by acute Toxoplasma gondii infection. Infect. Genet. Evol. 2016;37:137–142. doi: 10.1016/j.meegid.2015.11.005. [DOI] [PubMed] [Google Scholar]
- 16.He J.J., Ma J., Li F.C., Song H.Q., Xu M.J., Zhu X.Q. Transcriptional changes of mouse splenocyte organelle components following acute infection with Toxoplasma gondii. Exp. Parasitol. 2016;167:7–16. doi: 10.1016/j.exppara.2016.04.019. [DOI] [PubMed] [Google Scholar]
- 17.Znalesniak E.B., Fu T., Guttek K., Händel U., Reinhold D., Hoffmann W. Increased cerebral TFF1 expression in two murine models of neuroinflammation. Cell Physiol. Biochem. 2016;39:2287–2296. doi: 10.1159/000447921. [DOI] [PubMed] [Google Scholar]
- 18.Schroder K., Tschopp J. The inflammasomes. Cell. 2010;140:821–832. doi: 10.1016/j.cell.2010.01.040. [DOI] [PubMed] [Google Scholar]
- 19.Lamkanfi M., Dixit V.M. Inflammasomes and their roles in health and disease. Annu. Rev. Cell Dev. Biol. 2012;28:137–161. doi: 10.1146/annurev-cellbio-101011-155745. [DOI] [PubMed] [Google Scholar]
- 20.De Zoete M.R., Palm N.W., Zhu S., Flavell R.A. Inflammasomes. Cold Spring Harb. Perspect. Biol. 2014;6:a016287. doi: 10.1101/cshperspect.a016287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hoffmann W. TFF peptides. In: Kastin A., editor. Handbook of Biologically Active Peptides. 2nd ed. Elsevier; San Diego, CA, USA: 2013. pp. 1338–1345. [Google Scholar]
- 22.Cook G.A., Familari M., Thim L., Giraud A.S. The trefoil peptides TFF2 and TFF3 are expressed in rat lymphoid tissues and participate in the immune response. FEBS Lett. 1999;456:155–159. doi: 10.1016/S0014-5793(99)00940-0. [DOI] [PubMed] [Google Scholar]
- 23.Hoffmann W., Jagla W. Cell type specific expression of secretory TFF peptides: colocalization with mucins and synthesis in the brain. Int. Rev. Cytol. 2002;213:147–181. doi: 10.1016/s0074-7696(02)13014-2. [DOI] [PubMed] [Google Scholar]
- 24.Tomasetto C., Rio M.-C. Pleiotropic effects of trefoil factor 1 deficiency. Cell. Mol. Life Sci. 2005;62:2916–2920. doi: 10.1007/s00018-005-5479-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kjellev S. The trefoil factor family—Small peptides with multiple functionalities. Cell. Mol. Life Sci. 2009;66:1350–1369. doi: 10.1007/s00018-008-8646-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hoffmann W. Trefoil factor family (TFF) peptides and chemokine receptors: A promising relationship. J. Med. Chem. 2009;52:6505–6510. doi: 10.1021/jm9008136. [DOI] [PubMed] [Google Scholar]
- 27.Hoffmann W. TFF2, a MUC6-binding lectin stabilizing the gastric mucus barrier and more. Int. J. Oncol. 2015;47:806–816. doi: 10.3892/ijo.2015.3090. [DOI] [PubMed] [Google Scholar]
- 28.Nam H.W., Ahn H.J., Yang H.J. Pro-inflammatory cytokine expression of spleen dendritic cells in mouse toxoplasmosis. Korean J. Parasitol. 2011;49:109–114. doi: 10.3347/kjp.2011.49.2.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Peng J., Lin X., Lin H., Chen S., Liu J., Guo Z., Liang Y., Huang S., Lu F. Upregulated TLR2 and TLR4 expressions in liver and spleen during acute murine T. gondii infection. Parasitol. Res. 2016;115:4681–4686. doi: 10.1007/s00436-016-5226-8. [DOI] [PubMed] [Google Scholar]
- 30.Zorgi N.E., Galisteo A.J., Jr., Sato M.N., do Nascimento N., de Andrade H.F., Jr. Immunity in the spleen and blood of mice immunized with irradiated Toxoplasma gondii tachyzoites. Med. Microbial. Immunol. 2016;205:297–314. doi: 10.1007/s00430-015-0447-5. [DOI] [PubMed] [Google Scholar]
- 31.Gov L., Karimzadeh A., Ueno N., Lodoen M.B. Human innate immunity to Toxoplasma gondii is mediated by host caspase-1 and ASC and parasite GRA15. mBio. 2013;4:e00255-13. doi: 10.1128/mBio.00255-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Boyden E.D., Dietrich W.F. Nalp1b controls mouse macrophage susceptibility to anthrax lethal toxin. Nat. Genet. 2006;38:240–244. doi: 10.1038/ng1724. [DOI] [PubMed] [Google Scholar]
- 33.Wright N.A., Poulsom R., Stamp G.W., Hall P.A., Jeffery R.E., Longcroft J.M., Rio M.C., Tomasetto C., Chambon P. Epidermal growth factor (EGF/URO) induces expression of regulatory peptides in damaged human gastrointestinal tissues. J. Pathol. 1990;162:279–284. doi: 10.1002/path.1711620402. [DOI] [PubMed] [Google Scholar]
- 34.Ebert M.P., Hoffmann J., Haeckel C., Rutkowski K., Schmid R.M., Wagner M., Adler G., Schulz H.U., Roessner A., Hoffmann W., et al. Induction of TFF1 gene expression in pancreas overexpressing transforming growth factor α. Gut. 1999;45:105–111. doi: 10.1136/gut.45.1.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shaoul R., Okada Y., Cutz E., Marcon M.A. Colonic expression of MUC2, MUC5AC, and TFF1 in inflammatory bowel disease in children. J. Pediatr. Gastroenterol. Nutr. 2004;38:488–493. doi: 10.1097/00005176-200405000-00006. [DOI] [PubMed] [Google Scholar]
- 36.Kim C.H., Oh Y., Ha Y., Ahn Q., Kim S.H., Cho K.D., Lee B.H., Chae C. Expression of mucins in the mucosal surface of small intestines in 1 week-old pigs. J. Vet. Med. Sci. 2010;72:245–247. doi: 10.1292/jvms.09-0308. [DOI] [PubMed] [Google Scholar]
- 37.Kouznetsova I., Chwieralski C.E., Balder R., Hinz M., Braun A., Krug N., Hoffmann W. Induced trefoil factor family 1 expression by trans-differentiating clara cells in a murine asthma model. Am. J. Respir. Cell. Mol. Biol. 2007;36:286–295. doi: 10.1165/rcmb.2006-0008OC. [DOI] [PubMed] [Google Scholar]
- 38.Hoffmann W. TFF (trefoil factor family) peptides and their potential roles for differentiation processes during airway remodeling. Curr. Med. Chem. 2007;14:2716–2719. doi: 10.2174/092986707782023226. [DOI] [PubMed] [Google Scholar]
- 39.Koike T., Shimada T., Fujii Y., Chen G., Tabei K., Namatame T., Yamagata M., Tajima A., Yoneda M., Terano A., et al. Upregulation of TFF1 (pS2) expression by TNF-α in gastric epithelial cells. J. Gastroenterol. Hepatol. 2007;22:936–942. doi: 10.1111/j.1440-1746.2007.04861.x. [DOI] [PubMed] [Google Scholar]
- 40.Hirota M., Awatsuji H., Furukawa Y., Hayashi K. Cytokine regulation of PS2 gene expression in mouse astrocytes. Biochem. Mol. Biol. Int. 1994;33:515–520. [PubMed] [Google Scholar]
- 41.Beck S., Sommer P., dos Santos Silva E., Blin N., Gott P. Hepatocyte nuclear factor 3 (winged helix domain) activates trefoil factor gene TFF1 through a binding motif adjacent to the TATAA box. DNA Cell. Biol. 1999;18:157–164. doi: 10.1089/104454999315547. [DOI] [PubMed] [Google Scholar]
- 42.Ribieras S., Lefebvre O., Tomasetto C., Rio M.C. Mouse trefoil factor genes: Genomic organization, sequences and methylation analyses. Gene. 2001;266:67–75. doi: 10.1016/S0378-1119(01)00380-8. [DOI] [PubMed] [Google Scholar]
- 43.Terada T., Sakagami R., Tabuchi Y., Maeda M. Characterization of the mouse TFF1 (pS2) gene promoter region. Biol. Pharm. Bull. 2001;24:135–139. doi: 10.1248/bpb.24.135. [DOI] [PubMed] [Google Scholar]
- 44.Hromas R., Costa R. The hepatocyte nuclear factor-3/forkhead transcription regulatory family in development, inflammation, and neoplasia. Crit. Rev. Oncol. Hematol. 1995;20:129–140. doi: 10.1016/1040-8428(94)00151-I. [DOI] [PubMed] [Google Scholar]
- 45.Reeves E.P., Ali T., Leonard P., Hearty S., O’Kennedy R., May F.E., Westley B.R., Josenhans C., Rust M., Suerbaum S., et al. Helicobacter pylori lipopolysaccharide interacts with TFF1 in a pH-dependent manner. Gastroenterology. 2008;135:2043–2054. doi: 10.1053/j.gastro.2008.08.049. [DOI] [PubMed] [Google Scholar]
- 46.Baus-Loncar M., Kayademir T., Takaishi S., Wang T. Trefoil factor family 2 deficiency and immune response. Cell. Mol. Life. Sci. 2005;62:2947–2955. doi: 10.1007/s00018-005-5483-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kurt-Jones E.A., Cao L., Sandor F., Rogers A.B., Whary M.T., Nambiar P.R., Cerny A., Bowen G., Yan J., Takaishi S., et al. Trefoil family factor 2 is expressed in murine gastric and immune cells and controls both gastrointestinal inflammation and systemic immune responses. Infect. Immun. 2007;75:471–480. doi: 10.1128/IAI.02039-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Westley B.R., Griffin S.M., May F.E. Interaction between TFF1, a gastric tumor suppressor trefoil protein, and TFIZ1, a brichos domain-containing protein with homology to SP-C. Biochemistry. 2005;44:7967–7975. doi: 10.1021/bi047287n. [DOI] [PubMed] [Google Scholar]
- 49.Kouznetsova I., Laubinger W., Kalbacher H., Kalinski T., Meyer F., Roessner A., Hoffmann W. Biosynthesis of gastrokine-2 in the human gastric mucosa: Restricted spatial expression along the antral gland axis and differential interaction with TFF1, TFF2 and mucins. Cell. Physiol. Biochem. 2007;20:899–908. doi: 10.1159/000110450. [DOI] [PubMed] [Google Scholar]
- 50.Albert T.K., Laubinger W., Muller S., Hanisch F.G., Kalinski T., Meyer F., Hoffmann W. Human intestinal TFF3 forms disulfide-linked heteromers with the mucus-associated FCGBP protein and is released by hydrogen sulfide. J. Proteome Res. 2010;9:3108–3117. doi: 10.1021/pr100020c. [DOI] [PubMed] [Google Scholar]
- 51.Menheniott T.R., Peterson A.J., O’Connor L., Lee K.S., Kalantzis A., Kondova I., Bontrop R.E., Bell K.M., Giraud A.S. A novel gastrokine, Gkn3, marks gastric atrophy and shows evidence of adaptive gene loss in humans. Gastroenterology. 2010;138:1823–1835. doi: 10.1053/j.gastro.2010.01.050. [DOI] [PubMed] [Google Scholar]
- 52.Mueller S.N., Ahmed R. Lymphoid stroma in the initiation and control of immune responses. Immunol. Rev. 2008;224:284–294. doi: 10.1111/j.1600-065X.2008.00657.x. [DOI] [PubMed] [Google Scholar]
- 53.Kobayashi K., Ogata H., Morikawa M., Iijima S., Harada N., Yoshida T., Brown W.R., Inoue N., Hamada Y., Ishii H., et al. Distribution and partial characterisation of IgG Fc binding protein in various mucin producing cells and body fluids. Gut. 2002;51:169–176. doi: 10.1136/gut.51.2.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Johansson M.E., Thomsson K.A., Hansson G.C. Proteomic analyses of the two mucus layers of the colon barrier reveal that their main component, the MUC2 mucin, is strongly bound to the FCGBP protein. J. Proteome Res. 2009;8:3549–3557. doi: 10.1021/pr9002504. [DOI] [PubMed] [Google Scholar]
- 55.Schwartz J.L. FCGBP—A potential viral trap in RV144. Open AIDS J. 2014;8:21–24. doi: 10.2174/1874613601408010021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zaretsky A.G., Silver J.S., Siwicki M., Durham A., Ware C.F., Hunter C.A. Infection with Toxoplasma gondii alters lymphotoxin expression associated with changes in splenic architecture. Infect. Immun. 2012;80:3602–3610. doi: 10.1128/IAI.00333-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Della Valle M.C., Sleat D.E., Sohar I., Wen T., Pintar J.E., Jadot M., Lobel P. Demonstration of lysosomal localization for the mammalian ependymin-related protein using classical approaches combined with a novel density shift method. J. Biol. Chem. 2006;281:35436–35445. doi: 10.1074/jbc.M606208200. [DOI] [PubMed] [Google Scholar]
- 58.Nimmrich I., Erdmann S., Melchers U., Chtarbova S., Finke U., Hentsch S., Hoffmann I., Oertel M., Hoffmann W., Müller O. The novel ependymin related gene UCC1 is highly expressed in colorectal tumor cells. Cancer Lett. 2001;165:71–79. doi: 10.1016/S0304-3835(01)00390-1. [DOI] [PubMed] [Google Scholar]