Abstract
Background: A low intake of fruits and vegetables (F&Vs) is a major risk factor for cardiovascular disease (CVD) in the United States. Both mass media campaigns (MMCs) and economic incentives may increase F&V consumption. Few data exist on their comparative effectiveness.
Objective: We estimated CVD mortality reductions potentially achievable by price reductions and MMC interventions targeting F&V intake in the US population.
Design: We developed a US IMPACT Food Policy Model to compare 3 policies targeting F&V intake across US adults from 2015 to 2030: national MMCs and national F&V price reductions of 10% and 30%. We accounted for differences in baseline diets, CVD rates, MMC coverage, MMC duration, and declining effects over time. Outcomes included cumulative CVD (coronary heart disease and stroke) deaths prevented or postponed and life-years gained (LYGs) over the study period, stratified by age, sex, and race.
Results: A 1-y MMC in 2015 would increase the average national F&V consumption by 7% for 1 y and prevent ∼18,600 CVD deaths (95% CI: 17,600, 19,500), gaining ∼280,100 LYGs by 2030. With a 15-y MMC, increased F&V consumption would be sustained, yielding a 3-fold larger reduction (56,100; 95% CI: 52,400, 57,700) in CVD deaths. In comparison, a 10% decrease in F&V prices would increase F&V consumption by ∼14%. This would prevent ∼153,300 deaths (95% CI: 146,400, 159,200), gaining ∼2.51 million LYGs. For a 30% price decrease, resulting in a 42% increase in F&V consumption, corresponding values would be 451,900 CVD deaths prevented or postponed (95% CI: 433,100, 467,500) and 7.3 million LYGs gained. Effects were similar by sex, with a smaller proportional effect and larger absolute effects at older ages. A 1-y MMC would be 35% less effective in preventing CVD deaths in non-Hispanic blacks than in whites. In comparison, price-reduction policies would have equitable proportional effects.
Conclusion: Both national MMCs and price-reduction policies could reduce US CVD mortality, with price reduction being more powerful and sustainable.
Keywords: cardiovascular disease, disparities, food policy, nutrition, fruits and vegetables
INTRODUCTION
Although US cardiovascular disease (CVD) mortality is declining (1, 2) because of decreases in population-level risk factors and increasing medical treatments (3), CVD remains the leading cause of mortality. Each year, CVD causes ∼800,000 deaths and 6 million hospital admissions (2). Coronary artery disease (CAD) alone accounts for ∼9% of all disability-adjusted life-years lost in the United States (4, 5). This large CVD burden has an associated economic burden, previously predicted to amount to ∼$820 billion by 2030 if current trends continue (6). Furthermore, this CVD burden is unequal by age, sex, and race (7). Despite declining mortality, race disparities have persisted and in some cases worsened (8). With such vast health, economic, and equity burdens, CVD remains a challenge and priority for innovative preventive policies.
Suboptimal diet is the leading risk factor for cardiovascular mortality and morbidity in the United States and globally (9). Appropriately, many leading organizations, including the Institute of Medicine and WHO, have called for governments to adopt and implement evidence-based policies to improve diet (10), in particular intake of fruits and vegetables (F&Vs) because of their low consumption amounts and large, associated CVD burdens (11–13). However, the optimal methods to increase population F&V consumption remain unclear. Potential policy options range from the provision of general information, such as via mass media campaigns (MMCs), to direct economic incentives, such as subsidies or price reductions for healthy foods.
Estimates of potential reductions in US CVD mortality and possible effects on disparities of dietary policies are limited (14), and quantification of potential health gains of such policies by age, sex, and race are also sparse. Direct comparisons of the health and equity gains of MMCs and price-reduction policies by age, sex, and race are sparser still. Such studies are valuable to understand their potential effectiveness, determine potential varying efficacy, and help inform policy makers facing the large health, economic, and equity burdens of CVD.
We therefore aimed to estimate the CVD mortality reductions, life-years gained (LYGs), and subsequent effects on race disparities that are potentially achievable through MMCs and price-reduction interventions in the US population from 2015 to 2030 using the US IMPACT Food Policy model.
METHODS
We modeled the comparative effects on CAD, stroke, and total CVD mortality, LYGs, and race disparities through increased F&V consumption by means of a nationwide MMC or price reduction (10% and 30%) from 2015 to 2030. Outputs were stratified by age, sex, and race.
Data sources
The US population was stratified by age (10-y age groups, 25 to ≥85 y) and sex by using Surveillance, Epidemiology and End Results Program single-year population estimates (15). Population projections were sourced from the United States Census Bureau 2012 National Population Projections (16). We obtained data on the number of annual CVD deaths (International Classification of Disease codes: I00-09, I11, I13, I20-I51, I60-69) from 1979 to 2012 from the National Vital Statistics System (17), whereas baseline mortality projections to 2030 with the use of this data were taken from recent work by our group as described below (8). Baseline F&V intake data by age, sex, and race were obtained from the nationally representative NHANES 2009–2012 (18) by using the average of 2 consecutive 24-h dietary recalls, and projected intake forecasts were derived from NHANES data from 1999 to 2012 (19). Briefly, for each stratum we fitted a survey-weighted linear regression model with the survey year as the independent variable and F&V intake as the dependent variable. Estimated intakes for 2015–2030 were then estimated for each stratum based on this model by using the Stata “margins” command. The SE of the predicted intakes became less precise the further out-of-sample the prediction occurred (20), consistent with the out-of-sample prediction in any regression context. Sensitivity analyses were conducted carrying forward the most recent estimates. For no strata was there evidence of nonlinear trends.
Policy scenarios modeled
We modeled 3 potential policies that could increase F&V consumption in the United States. Our comparator was future consumption continuing on current trends through the model described above (19). Although the effect of F&V consumption on CVD mortality is stratified by age and sex (21), the effect size of the policy scenarios below (price reduction and MMC) on F&V consumption are aggregate estimates only, but we do include coverage estimates (explained below) to MMC effect size.
Price reduction
A recent meta-analysis by Afshin et al. (22) investigated and quantified the effect of change in food price on dietary habits, including F&V consumption. The strength of this meta analyses over previous studies is that it included interventional or prospective observational studies only. The meta-analysis concluded that for every 10% reduction in the price of F&Vs, consumption increased by 14% (95% CI: 11, 17%), broadly consistent with other published estimates (10, 23). This estimate is valid from a 10% to 50% change in price.
To model the effect of an increased consumption of F&Vs due to a reduction in the price of F&Vs, we used the effect size from the recent meta-analysis of interventional and prospective studies (22) discussed above. We applied this effect size to the baseline intake data to estimate the resulting intake of F&Vs. From this point, we ran the model as described below to calculate deaths prevented or postponed (DPPs). We assumed that the effect size applied to all subgroups similarly. Throughout this study, we refer to “coverage” as the differing effect size of the policy by age, sex, and race. The time-lag from the price-reduction policy being implemented to the subsequent effect on F&V consumption was assumed to be <1 y; hence, no time lag is modeled. Finally, we assumed a sustained impact of the policy throughout the 15-y period, i.e., no decaying impact of the policy efficacy.
We modeled 2 F&V price-reduction scenarios: 1) 10% price reduction at the point of purchase—a conservative scenario; and 2) 30% price reduction at the point of purchase—the price reduction achieved through the pilot Supplemental Nutrition Assistance Program in Massachusetts (24, 25).
MMC
An update of a further meta-analysis that updated previous provisional results (26) investigated and quantified the prospective effect of MMCs on dietary habits, again including F&Vs. This suggested that MMCs might increase F&V intake ∼7% (95% CI: 4%, 9%). The methodology to model the effect of MMCs on F&V consumption was the same as described above for the price-reduction scenarios. Using data from the “5 a day campaign” (27), we incorporated policy “coverage” estimates stratified by age, sex, and race (Supplemental Table 1). Here we used the full effect size 7% (95% CI: 4%, 9%) for the age, sex, and race groups with the largest effect size measured in the “5 a day campaign” and apportioned the reduced effect size to each other age, sex, and race group according to the proportional lower observed effect size. Further, we included policy “decaying impact” estimates by assuming that the MMCs would run for a 1-y duration (2015) with a 20% residual effect (minimum 5%, maximum 40%) 5 y later in 2020 (this estimate is further explained in the Supplemental Methods). We modeled linear reduction in effect size from the end of year 1–5 and the residual effect (20%) to persist to 2030. For completeness, we also modeled a less realistic scenario whereby the full effect of the MMCs persisted for a 15-y duration termed “sustained effect” model, assuming that the campaign would continue to operate at the same intensity over the entire time horizon of the analysis. These results are presented in full in the supplemental results (Supplemental Table 2).
The IMPACT Food Policy model
The IMPACT Food Policy model is an extension and adaptation of the CAD IMPACT model (28), deployed to the US population in 2007 (3), and the IMPACT Food Policy model previously used for modeling potential health gains through adapting healthier food policies in the United Kingdom (29, 30), Ireland (31), and the United States (32). Full details of the validated IMPACT methodology to calculate DPPs and LYGs have been described (33). Briefly, using mortality trends (1979–2012) we estimated baseline mortality projections for each year from 2015 to 2030 for CAD and stroke (8) to provide the number of expected stroke and CAD deaths each year, stratified by age, sex, and race. This estimation is crucial, given the steadily declining CVD mortality rates in the United States, to avoid substantial overestimation of potential benefits of any preventive intervention (8). The IMPACT Food Policy model calculates the expected change in numbers of CAD and stroke deaths attributable to changes in risk factors and treatments. In our analysis, we first estimated the effect of each given policy scenario on F&V intake. We then used the best evidence of effect size on CAD and stroke for both F&Vs separately (21) stratified by age and sex. This provided the policy scenario effect on CAD and stroke mortality and, hence, the number of deaths in each intervention year. This served as the “intervention expected number of deaths.” The difference between the baseline and intervention expected deaths provided the cumulative DPPs from 2015 to 2030. Then using 2012 life expectancy data for each age and sex group (17) (Supplemental Table 3) we calculated LYGs by multiplying this stratum-specific life expectancy data by the generated DPPs.
Probabilistic sensitivity analyses
We used probabilistic sensitivity analysis to estimate the effect of uncertainty in key model parameters with given input probability distributions. For each policy scenario we performed 10,000 iterations of the full model in R, version 3.2.2 (34) providing 95% CIs. The key parameters included were the effect size of MMC and price reductions on F&V intake, respectively, consumption of F&Vs, effect size of F&V consumption on CVD mortality, baseline CVD mortality, ratio of ischemic to hemorrhagic strokes, and years of life lost. Details on the parameters and chosen distributions for the Monte Carlo simulation are available in Supplemental Table 4.
RESULTS
Effects of policies on diet
The change in consumption of F&Vs varies substantially across the 3 policy scenarios and by age, sex, and race. A 10% price reduction resulted in an increase of 21.2 g (14% above baseline) fruit consumption/d in men aged 55–64 y (Table 1), compared with a larger 63.6-g (42%) increase in fruit consumption/d with a 30% price decrease in the same subgroup. The MMC resulted in just a 0.9-g (0.6%) increase in fruit consumption/d in this subgroup. Similar relative increases were observed in vegetable consumption. There was a larger range of increased consumption of F&V across subgroups under the MMC scenario. For example, young men (aged 25–34 y) observed a 1.5% (2-g/d) increase in fruit consumption, more than double the relative increase in middle-aged men outlined above.
TABLE 1.
Baseline consumption of fruits and vegetables in 2015 and 2030 (current trends) and achieved consumption associated with modeled policy options stratified by age and sex1
| 2015 baseline, g/d | 2030 baseline, g/d | 2030 price decrease by 10%, g/d | 2030 price decrease by 30%, g/d | 2030 MMC decaying impact, g/d | |
| Fruits | |||||
| Men, y | |||||
| 25–34 | 102.3 (86.0, 121.5) | 136.1 (99.2, 182.9) | 155.2 (112.3, 210.7) | 193.3 (139.2, 261.9) | 138.1 (100.7, 183.9) |
| 35–44 | 82.2 (66.0, 101.0) | 83.0 (47.6, 129.6) | 94.6 (54.1, 158.6) | 117.9 (65.0, 192.1) | 84.0 (48.8, 139.1) |
| 45–54 | 126.6 (100.7, 158.9) | 150.7 (92.5, 223.7) | 171.8 (106.3, 262.2) | 214.0 (130.9, 325.3) | 152.1 (94.0, 230.5) |
| 55–64 | 130.3 (109.7, 152.2) | 151.3 (103.0, 215.0) | 172.5 (119.5, 235.2) | 214.9 (150.2, 294.1) | 152.2 (103.1, 209.7) |
| 65–74 | 120.2 (97.6, 149.1) | 110.6 (62.7, 175.7) | 126.1 (72.7, 200.9) | 157.0 (88.5, 261.5) | 112.0 (60.8, 189.5) |
| ≥75 | 129.4 (112.1, 150.7) | 115.9 (77.1, 170.7) | 132.2 (84.1, 194.9) | 164.6 (104.6, 242.7) | 117.4 (74.1, 176.7) |
| Women, y | |||||
| 25–34 | 115.6 (99.6, 132.0) | 153.0 (114.2, 198.3) | 174.5 (132.7, 229.0) | 217.3 (163.3, 280.5) | 154.8 (118.3, 198.8) |
| 35–44 | 107.8 (86.7, 130.1) | 129.9 (85.1, 190.4) | 148.1 (97.9, 215.0) | 184.4 (117.5, 280.1) | 131.2 (84.7, 195.8) |
| 45–54 | 123.8 (107.2, 143.1) | 139.9 (98.2, 195.0) | 159.4 (112.3, 222.3) | 198.6 (142.9, 266.6) | 140.9 (104.5, 193.1) |
| 55–64 | 143.8 (124.9, 164.5) | 164.4 (111.4, 223.5) | 187.4 (131.8, 257.6) | 233.4 (161.1, 318.7) | 165.2 (115.3, 230.6) |
| 65–74 | 151.7 (128.9, 177.1) | 162.4 (111.3, 232.4) | 185.1 (123.3, 264.3) | 230.6 (161.3, 323.9) | 164.1 (111.1, 239.9) |
| ≥75 | 140.6 (124.2, 159.5) | 139.7 (96.8, 197.1) | 159.3 (112.0, 228.4) | 198.4 (136.8, 292.6) | 141.2 (97.2, 199.9) |
| Vegetables | |||||
| Men, y | |||||
| 25–34 | 163.9 (148.3, 180.4) | 167.7 (128.5, 215.4) | 191.2 (146.3, 244.6) | 238.1 (181.0, 303.4) | 170.0 (133.4, 217.6) |
| 35–44 | 179.0 (162.8, 196.9) | 185.2 (142.8, 230.8) | 211.2 (162.8, 273.9) | 263.0 (205.9, 334.7) | 187.5 (148.0, 234.6) |
| 45–54 | 174.5 (152.9, 200.5) | 175.6 (120.1, 250.5) | 200.2 (140.0, 280.7) | 249.4 (176.3, 343.2) | 177.3 (124.3, 244.1) |
| 55–64 | 180.0 (163.6, 197.0) | 184.8 (146.3, 228.9) | 210.7 (165.1, 260.5) | 262.5 (208.2, 330.2) | 185.9 (149.7, 229.9) |
| 65–74 | 191.1 (164.3, 219.4) | 192.8 (135.2, 257.4) | 219.8 (156.2, 300.8) | 273.8 (190.3, 375.7) | 195.2 (141.2, 261.1) |
| ≥75 | 169.9 (150.0, 193.6) | 167.0 (120.1, 224.3) | 190.4 (136.8, 258.3) | 237.1 (165.0, 326.7) | 169.1 (122.3, 224.1) |
| Women, y | |||||
| 25–34 | 173.5 (152.7, 196.7) | 163.6 (117.1, 225.6) | 186.4 (132.9, 264.6) | 232.2 (161.0, 334.6) | 165.5 (117.7, 231.1) |
| 35–44 | 180.1 (157.2, 202.5) | 177.1 (126.0, 243.5) | 201.9 (143.3, 278.6) | 251.5 (180.5, 341.2) | 178.9 (129.5, 241.8) |
| 45–54 | 212.4 (185.3, 238.4) | 221.9 (166.8, 288.3) | 253.0 (187.5, 331.8) | 315.1 (233.4, 402.6) | 223.6 (167.1, 288.3) |
| 55–64 | 212.9 (185.4, 239.5) | 211.4 (158.2, 283.0) | 241.0 (176.8, 319.4) | 300.2 (216.0, 392.9) | 212.5 (157.2, 279.0) |
| 65–74 | 202.7 (183.5, 224.6) | 190.2 (144.1, 251.5) | 216.9 (163.9, 283.7) | 270.1 (204.1, 357.7) | 192.2 (142.2, 252.8) |
| ≥75 | 169.8 (151.9, 188.1) | 159.0 (115.6, 210.9) | 181.3 (135.9, 234.8) | 225.8 (170.2, 292.6) | 160.7 (120.4, 211.8) |
Values are numbers (95% CIs). MMC “decaying impact” models refer to a 1-y MMC. Consumption is reported as grams per day. MMC, mass media campaign.
Mortality outcomes
All 3 policy scenarios would reduce deaths against the baseline of no intervention between 2015 and 2030. Price-reduction scenarios would save a substantially larger number of deaths than an MMC would. A 30% price decrease in F&Vs to the entire US population would yield the greatest mortality savings, reducing total CVD deaths by ∼6.4% representing ∼451,900 deaths (95% CI: 433,100, 467,500 deaths) over the period of 2015–2030 (Table 2). This would comprise ∼236,800 (95% CI: 225,400, 247,200) CAD and 215,100 (95% CI: 200,800, 229,000) stroke deaths. Prevented CVD deaths would generate 7.3 million LYGs (95% CI: 7,000,600, 7,471,500 LYGs) (Table 3). A smaller price decrease in F&Vs of 10% would still substantially reduce deaths but would be approximately one-third as effective as a 30% price reduction. This scenario would reduce total CVD deaths by 2.2%, ∼153,300 (95% CI: 146,400, 159,200) deaths from 2015 to 2030 comprising ∼79,700 (95% CI: 75,900, 83,600) CAD and 73,200 (95% CI: 68,600, 78,400) stroke deaths. This would generate 2.5 million LYGs (95% CI: 2,371,600, 2,551,100 LYGs) (Table 3). The efficacy of a MMC would vary substantially depending on whether it is a 1-y (decaying impact) or 15-y (sustained effect) campaign. However, both scenarios would yield substantially fewer DPPs than the price-reduction scenarios. A nationwide MMC would reduce total CVD deaths by between 0.3% and 0.8%, representing 18,600 (95% CI: 17,600, 19,500) to 56,100 (95% CI: 52,400, 57,700) deaths in the 1- and 15-y MMC, respectively (Table 2, Supplemental Table 2). A 1-y MMC would generate ∼280,100 LYGs (95% CI: 266,900, 291,100 LYGs) (Table 3).
TABLE 2.
Total cumulative expected deaths from CVD for 2015–2030 and reductions associated with each policy scenario1
| Baseline | Price decreased by 10% | Price decreased by 30% | MMC decaying impact | MMC sustained effect | |
| CAD | 5,051,300 (4,930,100, 5,187,800)2 | 79,700 (75,900, 83,600) [1.6]3 | 236,800 (225,400, 247,200) [4.7] | 9600 (9000, 10,200) [0.2] | 28,700 (26,700, 29,500) [0.6] |
| Men | 2,900,600 (2,823,000, 2,995,200) | 47,100 (44,200, 50,000) [1.6] | 139,800 (131,100, 147,600) [4.8] | 6000 (5500, 6500) [0.2] | 17 ,900 (16,300, 18,700) [0.6] |
| Women | 2,150,800 (2,055,800, 2,253,300) | 32,600 (30,200, 35,100) [1.5] | 97,000 (90,700, 104,400) [4.5] | 3700 (3300, 4100) [0.2] | 10,900 (9800, 11,500) [0.5] |
| Stroke | 2,011,600 (1,900,300, 2,135,100) | 73,200 (68,600, 78,400) [3.6] | 215,100 (200,800, 229,000) [10.7] | 9000 (8300, 9600) [0.4] | 27,300 (24,700, 29,100) [1.4] |
| Men | 862,400 (773,700, 970,400) | 32,000 (28,400, 36,200) [3.7] | 93,800 (83,400, 105,400) [10.9] | 4200 (3800, 4700) [0.5] | 12,900 (11,100, 14,500) [1.5] |
| Women | 1,149,200 (1,085,500, 1,214,100) | 41,300 (37,900, 44,600) [3.6] | 121,200 (111,500, 130,700) [10.5] | 4700 (4300, 5200) [0.4] | 14,400 (12,900, 15,500) [1.3] |
| CVD | 7,062,900 (6,890,400, 7,244,100) | 153,000 (146,400, 159,200) [2.2] | 451,900 (433,100, 467,500) [6.4] | 18,600 (17,600, 19,500) [0.3] | 56,100 (52,400, 57,700) [0.8] |
| Men | 3,762,900 (3,636,400, 3,908,800) | 79,000 (74,600, 84,200) [2.1] | 233,700 (219,500, 246,200) [6.2] | 10,200 (9500, 10,800) [0.3] | 30,800 (28,200, 32,400) [0.8] |
| Women | 3,300,000 (3,189,300, 3,410,500) | 73,900 (69,800, 78,000) [2.2] | 218,300 (206,100, 230,100) [6.6] | 8400 (7800, 9100) [0.3] | 25,300 (23,200, 26,400) [0.8] |
Baseline numbers of deaths are cumulative from 2015 to 2030. MMC “decaying impact” models refer to a 1-y MMC; “sustained effect” models refer to a 15-y MMC. Data are stratified by CVD subtype and sex. Results are rounded to the nearest 100. CAD, coronary artery disease; CVD, cardiovascular disease; MMC, mass media campaign.
Number of baseline expected deaths; 95% CI in parentheses (all such values).
Reduction in the number of deaths; 95% CI in parentheses; percentage of reduction in CVD mortality in brackets (all such values).
TABLE 3.
Cumulative life-years gained for 2015–2030 with each policy option1
| Price decreased by 10% | Price decreased by 30% | MMC decaying impact | |
| CAD | 1,363,900 (1,301,000, 1,424,600) | 4,044,500 (3,869,400, 4,197,000) | 152,800 (143,900, 161,500) |
| Men | 823,200 (776,000, 871,200) | 2,440,900 (2,297,100, 2,571,200) | 97,200 (89,600, 104,400) |
| Women | 540,700 (507,500, 579,300) | 1,603,600 (1,504,500, 1,699,600) | 55,600 (50,800, 60,500) |
| Stroke | 1,099,500 (1,038,000, 1,160,800) | 3,214,500 (3,026,500, 3,377,100) | 127,300 (118,700, 135,400) |
| Men | 484,000 (438,200, 538,400) | 1,414,700 (1,285,900, 1,559,100) | 60,400 (54,400, 66,100) |
| Women | 615,600 (573,900, 653,700) | 1,799,900 (1,677,000, 1,918,600) | 66,900 (61,200, 72,600) |
| CVD | 2,463,400 (2,371,600, 2,551,100) | 7,259,000 (7,000,600, 7,471,500) | 280,100 (266,900, 291,100) |
| Men | 1,307,200 (1,240,300, 1,378,600) | 3,855,500 (3,652,600, 4,045,100) | 157,600 (147,900, 166,700) |
| Women | 1,156,300 (1,100,200, 1,208,800) | 3,403,400 (3,241,900, 3,554,900) | 122,500 (114,600, 130,100) |
Values are numbers (95% CIs). Numbers of life-years gained are cumulative from 2015 to 2030. MMC “decaying impact” models refer to a 1-y MMC. Data are stratified by CVD subtype and sex. Results are rounded to the nearest 100. CAD, coronary artery disease; CVD, cardiovascular disease; MMC, mass media campaign.
Deaths prevented or postponed by age and sex
Although the relative increase in consumption of F&Vs due to price change would be equal, absolute changes in consumption would be unequal because of differential baseline consumption. For example, although vegetable consumption in men aged 65–74 and ≥75 y rose by 14% uniformly in the 10% price-reduction scenario, this resulted in a 27-g/d (i.e., from 191.1 g/d in 2015 to 219.8 g/d in 2030) and a 23.4-g/d (i.e., from 169.9 g/d in 2015 to 190.4 g/d in 2030) absolute increase in consumption, respectively, in 2030 (Table 1). The largest residual increase in fruit consumption compared with the 2030 baseline intake would be 1.5% (2.0 g/d) in young men (aged 25–34 y). This was ∼2.5 times larger than the modest increase (0.6%, 0.9 g/d) in consumption seen in middle-aged men (aged 55–64 y) (Table 1). This difference between the policy scenarios is consistent with the variation of efficacy of each policy by subgroup highlighted in the methods.
The variation in absolute change in F&V consumption, combined with baseline mortality, resulted in varying absolute and relative reductions in deaths by age and sex (Table 4). Generally, DPPs would increase with age and are greater in men than in women. Across all 3 policies, the largest absolute mortality gains would be seen in the oldest age group (≥75 y) of women over the period 2015–2030 (Table 4) where ∼120,900 (95% CI: 110,200, 131,600) deaths would be averted with a 30% F&V price decrease representing a reduction of ∼5.1% compared with 4.2% in the same age group in men. The largest relative reductions in CVD mortality, however, would be seen in younger groups in the 30% F&V price-reduction scenario. Young women (25–34 y old) would observe a reduction in mortality of ∼16.1%, and 35- to 44-y-old women would see a similar reduction of 13.8%, representing ∼4400 (95% CI: 3900, 4800) deaths. A similar pattern was seen in the 10% price-reduction scenario. Although mortality reductions in the MMC scenario would be substantially lower, the largest relative gains would be in the young age groups (men and women, 25–34 y old) who are most receptive to the MMC. These groups would see a reduction in CVD mortality of ∼0.7–0.8%, representing just 130 (95% CI: 110–150) and 59 (51–68) deaths in men and women, respectively. If the MMC were sustained over the 15-y period, this would prevent 3 times as many deaths (∼18,600) than the model assuming a decay in impact (Table 2, Supplemental Table 2).
TABLE 4.
Expected deaths from CVD from 2015 to 2030 and cumulative absolute deaths prevented or postponed from 2015 to 2030 associated with each policy option by age and sex1
| Baseline | Price decreased by 10% | Price decreased by 30% | MMC decaying impact | |
| Men, y | ||||
| 25–34 | 18,600 (17,300, 20,100)2 | 810 (700, 950) [4.4]3 | 2400 (2100, 2800) [12.8] | 130 (110, 150) [0.7] |
| 35–44 | 87,400 (82,600, 92,600) | 3000 (2700, 3400) [3.4] | 8800 (7800, 9900) [10.1] | 420 (360, 470) [0.5] |
| 45–54 | 239,600 (227,900, 251,500) | 8400 (7600, 9300) [3.5] | 24,700 (22,100, 27,400) [10.3] | 930 (810, 1060) [0.4] |
| 55–64 | 518,200 (495,700, 541,800) | 16,200 (14,500, 17,800) [3.1] | 47,800 (42,900, 52,900) [9.2] | 1200 (1000, 1400) [0.2] |
| 65–74 | 854,700 (811,400, 908,100) | 21,400 (19,100, 24,300) [2.5] | 63,200 (56,400, 70,600) [7.4] | 3200 (2800, 3600) [0.4] |
| ≥75 | 2,044,600 (1,938,300, 2,173,700) | 29,200 (25,900, 33,000) [1.4] | 86,900 (77,000, 97,900) [4.2] | 4400 (3900, 4900) [0.2] |
| Women, y | ||||
| 25–34 | 7900 (7400, 8600) | 440 (390, 490) [5.6] | 1300 (1100, 1400) [16.1] | 59 (51, 68) [0.8] |
| 35–44 | 32,000 (30,400, 34,000) | 1500 (1400, 1700) [4.7] | 4400 (3900, 4800) [13.8] | 180 (150, 200) [0.6] |
| 45–54 | 99,500 (94,800, 104,700) | 4400 (4000, 4800) [4.4] | 12,800 (11,600, 14,000) [12.9] | 410 (360, 460) [0.4] |
| 55–64 | 266,300 (253,400, 280,600) | 10,300 (9300, 11,200) [3.8] | 30,100 (27,400, 32,800) [11.3] | 620 (540, 700) [0.2] |
| 65–74 | 517,500 (489,800, 548,400) | 16,600 (15,000, 18,300) [3.2] | 48,900 (44,500, 53,300) [9.4] | 2000 (1800, 2200) [0.4] |
| ≥75 | 2,376,700 (2,265,500, 2,486,000) | 40,700 (37,300, 44,400) [1.7] | 120,900 (110,200, 131,600) [5.1] | 5100 (4600, 5800) [0.2] |
Baseline number of deaths are cumulative from 2015 to 2030. MMC “decaying impact” models refer to a 1-y MMC; “sustained effect” models refer to a 15-y MMC. Results are rounded to the nearest 100, rounded to the nearest 10 (<1000), or not rounded (<100). CVD, cardiovascular disease; MMC, mass media campaign.
Number of baseline expected deaths; 95% CI in parentheses (all such values).
Reduction in the number of deaths; 95% CI in parentheses; percentage of reduction in CVD mortality in brackets (all such values).
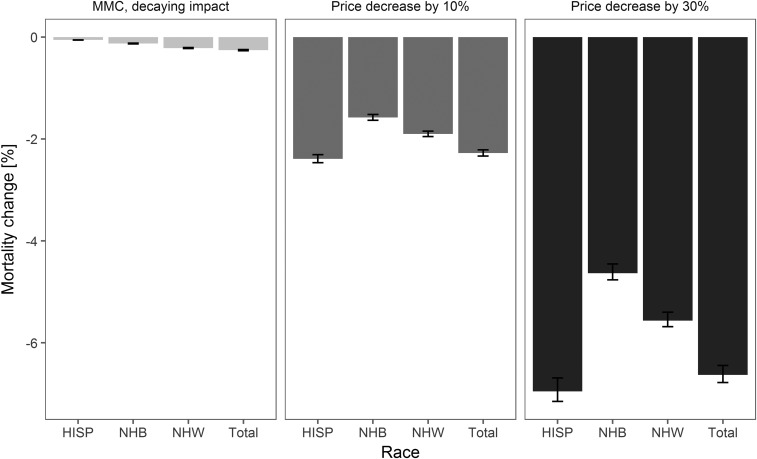
Effects on race disparities
Potential averted deaths due to MMCs or price-reduction policies (10% and 30%) would vary significantly by race (Figure 1). A 10% price decrease would be approximately equitable across race groups, with non-Hispanic whites observing a 1.86% reduction in CVD mortality over the 15-y period compared with a 1.83% reduction, just 1.6% less, in non-Hispanic blacks. A 30% price reduction in F&Vs would be similarly equitable, resulting in CVD mortality reductions of 5.51% and 5.41% in non-Hispanic whites and non-Hispanic blacks, respectively. In contrast, an MMC would be one-twentieth as equitable. The MMC would result in a 0.23% reduction in CVD mortality in non-Hispanic whites compared with just 0.15% in non-Hispanic blacks. Much of this 35% reduced effectiveness in non-Hispanic blacks was attributed to lower coverage and receptiveness to the campaign (Supplemental Table 1). Hispanic groups would observe larger reductions in CVD mortality in both price-reduction scenarios (2.35% and 6.90% in 10% and 30% price reduction, respectively) but a ∼75% lower reduction (0.06%) in CVD mortality in the MMC scenario when compared with non-Hispanic whites.
FIGURE 1.
Relative reduction in cardiovascular disease mortality by 2030 through a 15-y MMC and 10% and 30% price decreases in fruits and vegetables stratified by race. Values are medians (95% CIs). HISP, Hispanic; MMC, mass media campaign; NHB, non-Hispanic black; NHW, non-Hispanic white.
DISCUSSION
This is the first study, to our knowledge, to compare the potential effects on cardiovascular mortality of F&V MMCs and price-reduction policies from 2015 to 2030 stratified by age, sex, and race in the United States. Policies effectively increasing F&V consumption could powerfully reduce CVD mortality in the United States. Although all 3 policies would result in reductions in deaths by 2030, the magnitude and rate of such reductions differed substantially. A 30% price reduction in F&Vs alone could reduce CVD mortality from 2015 to 2030 by ∼6.4%, saving ∼451,900 deaths during this period. These gains could be >20 times greater than mortality savings from national MMCs.
One key contributor to the magnitude of the differential mortality reduction between these different approaches is the decaying impact of MMCs. In this modeling study, we assumed (not unreasonably) that a year-long media campaign might see a subsequent decline in effectiveness over time, with perhaps just a 20% residual effect 5 y later. If the effect were sustained, however, this would be ∼3 times as effective in reducing mortality over the 15-y period. Regardless of the MMC duration, price-reduction policies were more powerful and equitable.
Our study suggests that population-wide fiscal policies would be more effective over a longer period. Price-reduction policies might be more equitable than MMCs among race groups, based on data describing varying coverage estimates from previous nationwide campaigns (27) to model differential efficacy of the media campaign on age, sex, and race groups; however, further research is needed to confirm the equitability of price-reduction policies in F&Vs specifically. These potential differences become even larger when examining age and sex more closely. In the price-reduction scenarios, much of the difference in reduced CVD mortality was due to variance in the baseline F&V consumption; assuming a uniform proportional increase in consumption would therefore widen the disparity between those consuming the most and the least F&Vs. A poor intake of F&Vs is a strong risk factor for CAD, stroke, and common cancers, and intake is often lowest in the most deprived groups in society, thus widening disparities. Public health strategies can aim to improve the environment (structural policies) or facilitate behavior change in individuals (“agentic” policies) (35). The findings of our study are consistent with this notion, with nationwide price-reduction policies potentially being more equitable than the MMC attempting to change individual behavior.
F&V consumption has increased in the United States over the past decade (18) and is projected to increase further (19). However, consumption remains substantially below the recommended numbers of 2.5 vegetable (cups) and 2 fruit (cups) servings/d (36). The findings of this study have important implications for crafting specific price and incentive policy approaches to increase F&V access. F&Vs have high production costs because they have limited storage time, they often have to be transported with temperature control, they typically have to be hand-picked or cannot have a completely mechanized harvest, and certain crops are especially susceptible to adverse weather (37). The ultimate price that consumers pay for F&Vs is affected by policies and practices that have impacts across the entire food production system (38), including international trade agreements, immigration law, imports and exports, and the technology that is used to harvest and transport fragile crops across the globe. Embedding pricing incentives systematically within government food programs, such as the Supplemental Nutrition Assistance Program, could increase the purchase and consumption of F&Vs within low-income populations. These benefits could be extended if Electronic Benefits Transfer was integrated into all farmers’ markets, allowing recipients to authorize transfer of their government benefits to the retailers through retail channels of all sizes (from local farmers’ markets all the way up to large-scale retailers). Other pricing-related policy approaches could extend to growers, providing them with more accessible crop insurance, some agricultural subsidies for growing specialty crops, or offering government incentives to diversify crops across base acres of land. Thus, a system-wide approach to price strategies might be necessary to effectively increase broader access to F&Vs (39).
This study has strengths. To our knowledge, this is the first study to quantify and compare the potential health gains of F&V MMCs and price-reduction policies, which could be of great use to policy makers. We used nationally representative data sets encompassing the US adult (≥25 y old) population (15, 17, 40). Further, we used comprehensive meta-analyses (21) for effect sizes of F&Vs on CVD mortality and of each given policy on F&V intake within the US population (22, 26). Stratifying potential policy effects on race disparities in the United States of these policies is an additional strength. Further, our health outcomes analysis assumes continuing recent declines in CVD mortality (8) rather than more conventional methods that simply use a static baseline. If future mortality plateaus or even increases, mortality savings through the modeled policy scenarios would be even greater.
This study also has limitations. Both the effect of F&Vs on CAD and stroke mortality, alongside the effect on consumption of each given policy, are taken from comprehensive meta-analyses and thus are imperfect estimates (14, 21, 22, 26) The meta-analyses that we use (22) provide the same elasticity for F&Vs; however, other estimates find differences in their respective elasticities (10). Further, although this meta-analysis did not find heterogeneity by age or assess by sex or race, the relatively small number of studies included means we cannot conclude that there is no heterogeneity, just that none was found in this study. Our method of projecting dietary trends is based on 14 y of data, and this might not be enough to detect potential nonlinearity in the trend; however, we incorporated the uncertainty in the trend estimation into the probabilistic sensitivity analysis. When calculating LYGs, using disease subgroup-specific (CAD subgroup, stroke) median survivals is desirable, similar to previous work in the United Kingdom (33, 41). However, the age-specific life expectancy data used in our study offer a reasonable proxy. We assumed a short lag time between policy implementation and reductions in CVD mortality. However, evidence consistently supports this assumption (42). Although we incorporated coverage estimations by age, sex, and race for the MMC using data from the nationwide “5 a day campaign” (27), scarce data exist regarding decaying impact of MMCs. We therefore approximated a 20% residual effect after 5 y with wide uncertainty parameters (5–40%) included potential mortality savings of a “prolonged” 15-y media campaign in a sensitivity analysis. We did not account for differing price elasticity of demand for F&Vs by age, sex, and race, which could underestimate the effects of such policies on reducing disparities. Similarly, we did not account for a substitution effect of increasing F&V consumption. However, the meta-analyses deriving model parameters present observed effects, accounting for average actual population substitutes and compliments. Focused efforts to encourage specific substitutions could make such interventions even more effective. Further research addressing the cost-effectiveness of such potential food policies is therefore warranted.
In conclusion, increasing the consumption of F&Vs is an achievable and important target for public health policy, one that could substantially reduce US CVD mortality. Furthermore, compared with national MMCs, price-reduction policies of 10% or 30% would be far more powerful and sustainable. Decisive action is now indicated, prioritizing the most effective and cost-effective policy options.
Acknowledgments
The authors’ responsibilities were as follows—SC, MO, and DM: conceived the idea of the study; JP-S and PB: led the analysis with supervision by MO; JP-S: generated the results and drafted and finalized the paper with input from all authors; MO: was the guarantor and affirmed that the manuscript is an honest, accurate and transparent account of the study being reported; and all authors: contributed to the analysis, intellectual content, and critical revisions to the drafts of the paper and read and approved the final version. LW serves as the Director of Policy Research for the American Heart Association. CDR has consulted for the Almond Board of California and the Bell Institute of Health and Nutrition. DM has received honoraria for one-time scientific presentations and/or reviews on diet from Haas Avocado Board and Pollock Communications; has done ad-hoc consulting for Life Sciences Research Organization, Astra Zeneca, Boston Heart Diagnostics, GOED, and DSM; was on the scientific advisory board for Unilever North America until 2014; has received royalties from UpToDate for online chapters on fish oil and dietary fat; and is listed on Patent US8889739 B2 to Harvard University as a co-inventor, for use of trans-palmitoleic acid in identifying and treating metabolic disease. None of the remaining authors reported a conflict of interest related to the study.
Footnotes
Abbreviations used: CAD, coronary artery disease; CVD, cardiovascular disease; DPP, death prevented or postponed; F&V, fruit and vegetable; LYG, life-year gained; MMC, mass media campaign.
REFERENCES
- 1.National Heart, Lung and Blood Institute. Morbidity and mortality: 2012 chart book on cardiovascular, lung and blood diseases. Bethesda (MD): National Heart, Lung and Blood Institute; 2012. [Google Scholar]
- 2.Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, et al. Heart disease and stroke statistics–2012 update: a report from the American Heart Association. Circulation 2012;125:e2–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ford ES, Ajani UA, Croft JB, Critchley JA, Labarthe DR, Kottke TE, Giles WH, Capewell S. Explaining the decrease in U.S. deaths from coronary disease, 1980-2000. N Engl J Med 2007;356:2388–98. [DOI] [PubMed] [Google Scholar]
- 4.Global Burden of Disease Health Data. Citation for GBD compare visualizations [Internet]. 2015 [cited 2016 Jan 27]. Available from: https://www.healthdata.org/sites/default/files/files/Data_viz/Help_Cite_GBD_Compare_Visualization.pdf.
- 5.Forouzanfar MH, Alexander L, Anderson HR, Bachman VF, Biryukov S, Brauer M, Burnett R, Casey D, Coates MM, Cohen A, et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;386:2287–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, Finkelstein EA, Hong Y, Johnston SC, Khera A, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation 2011;123:933–44. [DOI] [PubMed] [Google Scholar]
- 7.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de Ferranti S, Després JP, Fullerton HJ, et al. Heart disease and stroke statistics-2016 update: a report from the American Heart Association. Circulation 2016;133:e38–360. [DOI] [PubMed] [Google Scholar]
- 8.Pearson-Stuttard J, Guzman-Castillo M, Penalvo JL, Rehm CD, Afshin A, Danaei G, Kypridemos C, Gaziano T, Mozaffarian D, Capewell S, et al. Modeling future cardiovascular disease mortality in the United States: national trends and racial and ethnic disparities. Circulation 2016;133:967–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. UN. Political declaration of the high-level meeting of the general assembly on the prevention and control of non-communicable diseases [Internet]. 2011 [cited 2015 May 20]. Available from: http://www.who.int/nmh/events/un_ncd_summit2011/political_declaration_en.pdf. [Google Scholar]
- 10.Andreyeva T, Long MW, Brownell KD. The impact of food prices on consumption: a systematic review of research on the price elasticity of demand for food. Am J Public Health 2010;100:216–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic impact goal through 2020 and beyond. Circulation 2010;121:586–613. [DOI] [PubMed] [Google Scholar]
- 12.GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;385:117–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Roth GA, Huffman MD, Moran AE, Feigin V, Mensah GA, Naghavi M, Murray CJ. Global and regional patterns in cardiovascular mortality from 1990 to 2013. Circulation 2015;132:1667–78. [DOI] [PubMed] [Google Scholar]
- 14.Afshin A, Penalvo J, Del Gobbo L, Kashaf M, Micha R, Morrish K, Pearson-Stuttard J, Rehm C, Shangguan S, Smith JD, et al. CVD prevention through policy: a review of mass media, food/menu labeling, taxation/subsidies, built environment, school procurement, worksite wellness, and marketing standards to improve diet. Curr Cardiol Rep 2015;17:98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Cancer Institute. Surveillance, Epidemiology, and End Results Program. Single year of age county population estimates 1969-2015 [Internet]. Bethesda (MD): National Cancer Institute; 2015 [cited 2015 May 22]. Available from: http://seer.Cancer.Gov/popdata/singleages.html.
- 16.US Census Bureau. Population projections. 2012 national population projections: summary tables [Internet]. Washington (DC): US Census Bureau; 2015 [cited 2015 May 15]. Available from: http://www.census.gov/population/projections/data/national/2012/summarytables.html.
- 17.Murphy SL, Kochanek KD, Xu J, Heron M. Deaths: final data for 2012. Natl Vital Stat Rep. 2015;63:1–117. [PubMed] [Google Scholar]
- 18.CDC. NHANES 2009–2010 dietary data [Internet]. Atlanta (GA): CDC; 2015. [cited 2015 May 22]. Available from: http://wwwn.cdc.gov/nchs/nhanes/search/datapage.aspx?Component=dietary&CycleBeginYear=2009.
- 19.Rehm CD, Peñalvo JL, Afshin A, Mozaffarian D. Dietary intake among us adults, 1999-2012. JAMA 2016;315:2542–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Korn EL, Graubard BI. Analysis of health surveys. New York: Wiley; 1999. [Google Scholar]
- 21.Micha R, Penalvo JL, Cudhea F, Imamura F, Rehm CD, Mozaffarian D. Association between dietary factors and mortality from heart disease, stroke, and type 2 diabetes in the United States. JAMA 2017;317:912–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Afshin A, Penalvo JL, Del Gobbo L, Silva J, Michaelson M, O’Flaherty M, Capewell S, Spiegelman D, Danaei G, Mozaffarian D. The prospective impact of food pricing on improving dietary consumption: a systematic review and meta-analysis. PLoS One 2017;12:e0172277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Green R, Cornelsen L, Dangour AD, Turner R, Shankar B, Mazzocchi M, Smith RD. The effect of rising food prices on food consumption: systematic review with meta-regression. BMJ 2013;346:f3703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bartlett S, Klerman J, Olsho L. Evaluation of the Healthy Incentives Pilot (HIP): final report. Cambridge (MA): Abt Associates for the USDA, Food and Nutrition Service; 2014. [Google Scholar]
- 25.Olsho LE, Klerman JA, Wilde PE, Bartlett S. Financial incentives increase fruit and vegetable intake among supplemental nutrition assistance program participants: a randomized controlled trial of the USDA healthy incentives pilot. Am J Clin Nutr 2016;104:423–35. [DOI] [PubMed] [Google Scholar]
- 26.Afshin A, Abioye AI, Ajala ON, Nguyen AB, See KC, Mozaffarian D. Effectiveness of mass media campaigns for improving dietary behaviors: a systematic review and meta-analysis. Circulation 2013;127:AP087. [Google Scholar]
- 27.Potter JD, Finnegan JR, Guinard J, Huerta E, Kelder SH, Kristal AR, Kumanyika S, Lin R, Motsinger B, Prendergast F, et al. 5 A Day for Better Health program evaluation report. NIH Publication No. 01-4904. Bethesda (MD): NIH; 2000.
- 28.Capewell S, Morrison CE, McMurray JJ. Contribution of modern cardiovascular treatment and risk factor changes to the decline in coronary heart disease mortality in Scotland between 1975 and 1994. Heart 1999;81:380–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.O’Flaherty M, Flores-Mateo G, Nnoaham K, Lloyd-Williams F, Capewell S. Potential cardiovascular mortality reductions with stricter food policies in the United Kingdom of Great Britain and Northern Ireland. Bull World Health Organ 2012;90:522–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Allen K, Pearson-Stuttard J, Hooton W, Diggle P, Capewell S, O’Flaherty M. Potential of trans fats policies to reduce socioeconomic inequalities in mortality from coronary heart disease in England: cost effectiveness modelling study. BMJ 2015;351:h4583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.O’Keeffe C, Kabir Z, O’Flaherty M, Walton J, Capewell S, Perry IJ. Modelling the impact of specific food policy options on coronary heart disease and stroke deaths in Ireland. BMJ Open 2013;3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pearson-Stuttard J, Bandosz P, Rehm C, Penalvo J, Whitsel L, Gaziano T, Conrad Z, Wilde P, Micha R, Lloyd-Williams F, et al. Reducing US cardiovascular disease burden and disparities through national and targeted dietary policies: a modelling study. PLoS Med 2017;14:e1002311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Unal B, Critchley JA, Fidan D, Capewell S. Life-years gained from modern cardiological treatments and population risk factor changes in England and Wales, 1981-2000. Am J Public Health 2005;95:103–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.R Development Core Team. R: a language and environment for statistical computing [Internet]. c2014 [cited 2017 May 2]. Available from: http://www.R-project.org/.
- 35.McLaren L, McIntyre L, Kirkpatrick S. Rose’s population strategy of prevention need not increase social inequalities in health. Int J Epidemiol 2010;39:372–7. [DOI] [PubMed] [Google Scholar]
- 36.US Department of Health and Human Services and USDA. Dietary guidelines for Americans 2015 – 2020 [Internet]. 8th ed. 2015. [cited 2016 Jan 29]. Available from: http://health.gov/dietaryguidelines/2015/guidelines/appendix-3/.
- 37.Calvin L, Martin P. The U.S. produce industry and labor: facing the future in a global economy [Internet]. Washington (DC): USDA; 2010 [cited 2017 May 2]. Available from: https://arefiles.ucdavis.edu//uploads/filer_public/2014/06/19/calvin-martinusdaerr106.pdf.
- 38.Drewnowski A, Darmon N. The economics of obesity: dietary energy density and energy cost. Am J Clin Nutr 2005;82(1 Suppl):265S–73S. [DOI] [PubMed] [Google Scholar]
- 39.Hawkes C. Food policies for healthy populations and healthy economies. BMJ 2012;344:e2801. [DOI] [PubMed] [Google Scholar]
- 40.CDC. National Vital Statistics System Report [Internet]. 2015. [cited 2015 May 22]. Available from: http://www.cdc.gov/nchs/deaths.html.
- 41.Pearson-Stuttard J, Critchley J, Capewell S, O’Flaherty M. Quantifying the socio-economic benefits of reducing industrial dietary trans fats: modelling study. PLoS One 2015;10:e0132524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Capewell S, O’Flaherty M. Rapid mortality falls after risk-factor changes in populations. Lancet 2011;378:752–3. [DOI] [PubMed] [Google Scholar]