Abstract
Context
Therapeutic hypothermia is used for patients following both out-of-hospital and in-hospital cardiac arrest. However, randomized trials on its efficacy for the in-hospital setting do not exist, and comparativeness effectiveness data are limited.
Objective
To evaluate the association between therapeutic hypothermia and survival after in-hospital cardiac arrest.
Design, Setting, Patients
Within the national Get-With-The-Guidelines-Resuscitation registry, 26,183 patients successfully resuscitated from an in-hospital cardiac arrest between March 1, 2002 and December 31, 2014 following introduction of therapeutic hypothermia treatment at 355 U.S. hospitals were identified. Follow-up ended February 4, 2015.
Exposure
Induction of therapeutic hypothermia
Main Outcome Measures
Primary outcome of survival to hospital discharge. Secondary outcome of favorable neurological survival, defined as a cerebral performance category score ≤ 2 (i.e., without severe neurological disability). Comparisons were performed using a matched propensity score analysis and examined for all arrests, and separately for nonshockable (asystole and pulseless electrical activity) and shockable cardiac arrests (ventricular fibrillation and pulseless ventricular tachycardia).
Results
Overall, 1568 (6.0%) patients with in-hospital cardiac arrest were treated with therapeutic hypothermia, and 1524 patients were matched by propensity score to 3714 non-hypothermia-treated patients. Mean age of the propensity score-matched cohort was 62.0 ± 17.5 years, 57.5% were men, and 68.0% were white. After adjustment, therapeutic hypothermia was associated with lower in-hospital survival (27.4% vs. 29.2%; Relative Risk, 0.88 [95% CI, 0.80–0.97]; Risk Difference, −3.6% [−6.3%, −0.9%]; P=0.01), and these associations were similar (interaction P=0.74) for non-shockable (22.2% vs. 24.5%; Relative Risk, 0.87 [0.76–0.99]; Risk Difference, −3.2% [−6.2%, −0.3%]) and shockable cardiac arrest rhythms (41.3% vs. 44.1%; Relative Risk, 0.90 [0.77, 1.05]; Risk Difference, −4.6% [−10.9%, 1.7%]). Therapeutic hypothermia was also associated with lower rates of favorable neurological survival for the overall cohort (hypothermia group, 17.0% [246/1443]; non-hypothermia group, 20.5% [725/3529]; Relative Risk, 0.79 [0.69, 0.90]; Risk Difference, −4.4% [−6.8%, −2.0%]; P<0.001) and for both rhythm types (interaction P=0.88).
Conclusion
Among patients with in-hospital cardiac arrest, use of therapeutic hypothermia compared with usual care was associated with a lower likelihood of survival to hospital discharge and a lower likelihood of favorable neurological survival. These observational findings warrant a randomized clinical trial to assess efficacy of therapeutic hypothermia for in-hospital cardiac arrest.
Introduction
Therapeutic hypothermia, or targeted temperature management, is recommended for comatose patients following both out-of-hospital and in-hospital cardiac arrest.1 Nevertheless, therapeutic hypothermia has only been shown to improve overall survival and rates of favorable neurological survival in patients with out-of-hospital cardiac arrest due to ventricular fibrillation.2, 3 Whether this treatment improves survival for patients with in-hospital cardiac arrest—in which response times, comorbidity burden, and cardiac arrest etiology differ markedly from the out-of-hospital setting—is unknown.
To our knowledge, there have been no randomized trials conducted in the in-hospital setting. Two small observational studies (comprising a total of 231 treated patients) have not shown a survival benefit,4, 5 and a third contained only 42 treated patients with in-hospital cardiac arrest.6 In addition, greater than 80% of in-hospital cardiac arrests have initial rhythms of asystole or pulseless electrical activity (PEA)—cardiac arrest rhythms for which the evidence base for therapeutic hypothermia is unclear, even for the out-of-hospital setting.7 As in-hospital cardiac arrest affects ~200,000 individuals annually in the U.S.8, there is a need to understand whether therapeutic hypothermia is associated with improved survival for these patients.
To address this gap in knowledge, this study was designed to evaluate the association of therapeutic hypothermia with survival to hospital discharge, and with favorable neurological survival at hospital discharge among patients with in-hospital cardiac arrest, by leveraging data from the Get with the Guidelines (GTWG)–Resuscitation registry. In addition, by linking this registry with Medicare files, the association between hypothermia treatment and 1-year survival was evaluated.
Methods
The institutional review board of the Mid America Heart Institute waived the requirement for informed consent as data were de-identified.
Data Sources
GWTG-Resuscitation® is a large, prospective, national quality-improvement registry of in-hospital cardiac arrest sponsored by the American Heart Association. Its design has been previously described.9 In brief, trained hospital personnel attempt to identify all patients without do-not-resuscitate orders with a cardiac arrest (defined as absence of a palpable central pulse, apnea, and unresponsiveness) who undergo cardiopulmonary resuscitation. Cases are identified by hospital research staff through multiple methods, including centralized collection of cardiac arrest flow sheets, reviews of hospital paging system logs, and routine checks of code carts and pharmacy tracer drug records.9 Standardized Utstein-style definitions are used for all patient variables and outcomes to facilitate uniform reporting across hospitals.10, 11 Data accuracy in GWTG-Resuscitation is supported by certification of research staff, use of case-study methods for newly enrolled hospitals to enhance operational definition compliance prior to data acceptance, use of standardized software with data checks for completeness and accuracy, and a periodic re-abstraction process, which has been demonstrated to have a mean error rate of 2.4%.9
For patients 65 years of age and older, GWTG-Resuscitation data has been previously linked with Medicare inpatient files.12, 13 For each linked patient, Medicare denominator and inpatient files were obtained. For this study, as newer years of Medicare files were available, the deterministic linkage was repeated for Medicare data through 2012. This linkage was successful in 66.5% of Medicare-eligible GWTG-Resuscitation patients, similar to the prior rate of 68.6%.13
Study Population
The study included patients enrolled in GWTG-Resuscitation between March 1, 2002 (after publication of hypothermia trials for out-of-hospital cardiac arrest)2, 3 and December 31, 2014. As this study evaluated therapeutic hypothermia, only patients with return of spontaneous circulation after an index in-hospital cardiac arrest were included. For those 65 and older, patients who were not linked to Medicare inpatient files (no unique match or enrolled after 2012) were excluded to enable examination of post-discharge survival. To ascertain that hypothermia was available at each hospital, patients from hospitals with no cases of therapeutic hypothermia were excluded. Moreover, only cases occurring after the first documented use of therapeutic hypothermia for in-hospital cardiac arrest at each hospital were included. As therapeutic hypothermia is considered in comatose patients, the cohort was restricted to patients on mechanical ventilation at the time of cardiac arrest (as documented by GWTG-Resuscitation) or after cardiac arrest (as documented by a Medicare ICD-9-CM procedure code for mechanical ventilation [96.7X] among those 65 or older). Patients with missing information on survival to discharge and comorbidities for model adjustment were excluded. Furthermore, patients with an initial out-of-hospital cardiac arrest followed by an in-hospital cardiac arrest were excluded.
Independent Variable and Study Outcomes
The independent exposure variable was active induction of therapeutic hypothermia, as documented within GWTG-Resuscitation. The primary outcome was in-hospital survival, (i.e., to hospital discharge). The secondary outcome was favorable neurological survival, defined as survival to hospital discharge with a cerebral performance category score of 1 or 2 (i.e., without severe neurological disability).14 Additionally, among patients 65 or older, cumulative survival (i.e., area under the survival curve) over the first year and one-year survival were examined using Medicare denominator files. The last follow-up date was February 4, 2015 for survival to discharge and favorable neurological survival and December 31, 2012 for one-year outcomes.
Statistical Analysis
Baseline differences between patients treated and not treated with therapeutic hypothermia were evaluated using X2 tests for categorical variables and Student’s t-tests for continuous variables.
To evaluate the association between therapeutic hypothermia treatment and survival outcomes, propensity score analyses were conducted. A multivariable logistic regression model was constructed to estimate a patient’s likelihood of being treated with therapeutic hypothermia after in-hospital cardiac arrest. This model included the hospital site and the following variables from GWTG-Resuscitation: age, sex, self-identified race by patients or families (which is known to affect survival15 and was categorized as white, black, and other), initial cardiac arrest rhythm (asystole, PEA, ventricular fibrillation, pulseless ventricular tachycardia), location of cardiac arrest, comorbid conditions (prior heart failure or myocardial infarction; index admission heart failure or myocardial infarction, diabetes mellitus, baseline depression in central nervous system function, acute stroke, pneumonia, and metastatic or hematologic malignancy), medical conditions present within 24 hours of cardiac arrest (renal insufficiency, hepatic insufficiency, respiratory insufficiency, hypotension, septicemia, and metabolic or electrolyte abnormality) and interventions in place at the time of cardiac arrest (continuous intravenous vasopressor, implantable cardioverter-defibrillator, and hemodialysis). The model also adjusted for duration of acute cardiopulmonary resuscitation, the time of day (work hours [7:00 am to 10:59 pm] vs. after hours [11:00 pm to 6:59 am]), and day of the week (weekday vs. weekend) of the cardiac arrest.16
After deriving a propensity score for each patient, variable optimal matching for each hypothermia-treated patient was performed, with up to 4 controls without replacement for each treated patient, using an algorithm match with a caliper width no greater than 0.2 times the standard deviation of the logit of the propensity score.17 Besides matching by propensity score, hypothermia and non-hypothermia-treated patients were additionally matched on 3 other criteria: cardiac arrest ± 365 days of treated patients, initial cardiac arrest rhythm, and duration of acute cardiopulmonary resuscitation (in 5 minute categories [e.g., 6–10, 11–15, 16–20, etc]). Matched patients were compared to assess balance in covariates (i.e., standardized differences for each covariate were <10%).18 After confirming this, the associations between therapeutic hypothermia and survival to discharge and favorable neurological survival were assessed by constructing binomial models using a log link, stratified by matched sets, to estimate relative risks, and an identity link to estimate risk differences.19
Interaction analyses were conducted between therapeutic hypothermia and cardiac arrest rhythm to assess whether the association between therapeutic hypothermia and survival outcomes differed for patients with shockable (ventricular fibrillation and pulseless ventricular tachycardia) and non-shockable cardiac arrest rhythms (asystole and PEA). For 1-year survival, a separate propensity score model was derived for patients 65 years of age or older. Cumulative survival over the first year was compared between the propensity score-matched patients. In addition, a binomial model using a log link, stratified by matched sets, assessed overall rates of 1-year survival.
Although use of a propensity score balances measured covariates between treatment groups, indication bias due to unmeasured confounding may exist. To address this, a sensitivity analysis was conducted whereby all patients who died within the first 24 hours were excluded. If there was indication bias against therapeutic hypothermia treatment (whereby sicker patients were more likely to receive therapeutic hypothermia), this analysis, from 24 hours onward, would result in a stronger survival benefit for therapeutic hypothermia treatment, as a greater proportion of patients treated with hypothermia would have died during the first 24 hours. This sensitivity analysis was conducted after deriving new propensity scores for this cohort and re-performing the previous analyses.
For each analysis, the null hypothesis was evaluated at a 2-sided significance level of 0.05 and calculated 95% confidence intervals (CIs) using robust standard errors. All analyses were performed using SAS version 9.2 (SAS Institute, Cary, North Carolina) and R version 2.10.0 (R Foundation for Statistical Computing, Vienna, Austria).20
Results
An initial 117,005 in-hospital cardiac arrest patients with return of spontaneous circulation from 674 hospitals were identified (Figure 1). Excluded were 31,565 patients not linked with Medicare data, 15,012 patients from hospitals without hypothermia cases, 17,117 patients with an in-hospital cardiac arrest prior to the first patient treated with therapeutic hypothermia at their hospital, 26,429 patients not on mechanical ventilation, 69 patients and 28 patients with missing data on survival and comorbidities, respectively, and 602 patients with an initial out-of-hospital cardiac arrest. The final cohort included 26,183 patients from 355 hospitals who were successfully resuscitated after in-hospital cardiac arrest.
Figure 1. Derivation of the Study Cohort.
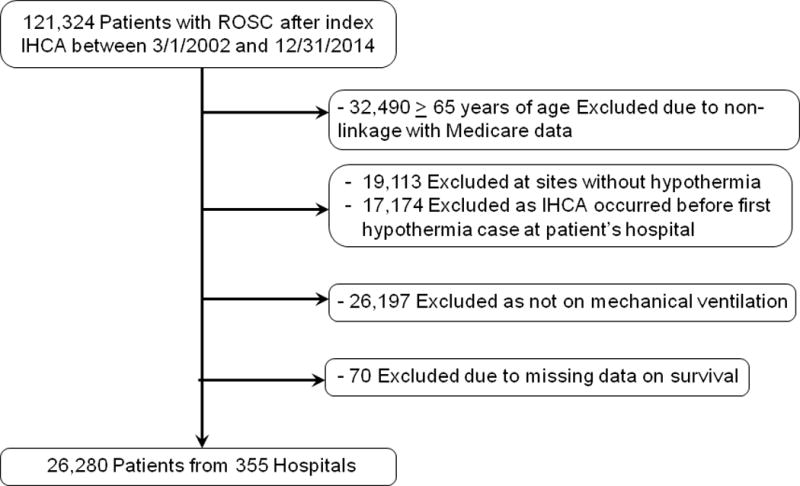
IHCA, in-hospital cardiac arrest; PS, propensity score; ROSC, return of spontaneous circulation.
Overall, 1568 (6.0%) were treated with therapeutic hypothermia. Patients treated with hypothermia were younger, less likely to have a cardiac arrest in the intensive care unit, and more likely to have an initial cardiac arrest rhythm of ventricular fibrillation (Table 1). The duration of resuscitation before return of spontaneous circulation was similar between patients treated with and without hypothermia, but patients initiated on therapeutic hypothermia were more likely to have a myocardial infarction prior to their cardiac arrest and less likely to have hypotension, respiratory insufficiency, renal insufficiency, hepatic insufficiency, pneumonia, acute stroke, and metastatic or hematologic malignancy at the time of their arrest.
Table 1. Comparison of Hypothermia-treated and Non-Hypothermia-treated Patients Before and After Propensity Score Matching.
Patient and cardiac arrest factors were well-balanced (i.e., standardized differences <10%) after propensity score matching
| BEFORE PROPENSITY SCORE MATCHING
|
AFTER PROPENSITY SCORE MATCHING
|
|||||
|---|---|---|---|---|---|---|
| Hypothermia (n = 1568) |
Non-Hypothermia (n = 24,615) |
P value | Hypothermia (n = 1524) |
Non-Hypothermia (n =3714) |
Standardized Differences, % |
|
| DEMOGRAPHICS | ||||||
| Age, mean ± SD | 61.5 ± 16.2 | 63.9 ± 16.9 | <0.001 | 61.6 ± 16.2 | 62.2 ± 17.5 | 3.2 |
| Male sex | 908 (57.9%) | 13,750 (55.9%) | 0.11 | 892 (58.5%) | 2120 (57.1%) | 1.7 |
| Race | 0.07 | 5.0 | ||||
| White | 1044 (66.6%) | 17,184 (69.8%) | 1015 (66.6%) | 2548 (68.6%) | ||
| Black | 377 (24.0%) | 5315 (21.6%) | 366 (24.0%) | 870 (23.4%) | ||
| Other | 147 (9.4%) | 2116 (8.6%) | 143 (9.4%) | 296 (8.0%) | ||
| CARDIAC ARREST FACTORS | ||||||
| CPR duration (minutes), mean ± SD | 16.5 ± 18.7 | 16.3 ± 19.0 | 0.78 | 16.5 ± 18.7 | 16.3 ± 18.8 | 2.7 |
| CPR duration (minutes), median (IQR) | 11.0 (8.0, 22.0) | 10.0 (8.0, 21.0) | 0.09 | 11.0 (8.0, 22.0) | 11.0 (8.0, 21.0) | NA¶ |
| Location of arrest | <0.001 | 8.3 | ||||
| Intensive care unit | 852 (54.3%) | 15,908 (64.6%) | 830 (54.5%) | 2208 (59.5%) | ||
| Telemetry unit | 126 (8.0%) | 2495 (10.1%) | 126 (8.3%) | 330 (8.9%) | ||
| Non-monitored hospital unit | 152 (9.7%) | 2248 (9.1%) | 149 (9.8%) | 347 (9.3%) | ||
| Emergency room | 254 (16.2%) | 2046 (8.3%) | 248 (16.3%) | 475 (12,8%) | ||
| Procedural area | 165 (10.5%) | 1737 (7.1%) | 154 (10.1%) | 319 (8.6%) | ||
| Other | 19 (1.2%) | 181 (0.7%) | 17 (1.1%) | 35 (0.9%) | ||
| Time of Arrest | ||||||
| Night (11 PM to 6:59 AM) | 451 (28.8%) | 7693 (31.3%) | 0.04 | 436 (28.6%) | 1101 (29.6%) | 1.3 |
| Weekend | 492 (31.4%) | 7846 (31.9%) | 0.68 | 481 (31.6%) | 1171 (31.5%) | 0.1 |
| Initial Cardiac Arrest Rhythm | <0.001 | 2.7 | ||||
| Asystole | 407 (26.0%) | 7016 (28.5%) | 397 (26.0%) | 1000 (26.9%) | ||
| Pulseless Electrical Activity | 735 (46.9%) | 12,785 (51.9%) | 715 (46.9%) | 1832 (49.3%) | ||
| Ventricular Fibrillation | 263 (16.8%) | 2548 (10.4%) | 254 (16.7%) | 500 (13.5%) | ||
| Pulseless Ventricular Tachycardia | 163 (10.4%) | 2266 (9.2%) | 158 (10.4%) | 382 (10.3%) | ||
| PRE-EXISTING CONDITIONS | ||||||
| Heart failure this admission | 250 (15.9%) | 4423 (18.0%) | 0.04 | 244 (16.0%) | 581 (15.6%) | 0.3 |
| Heart failure prior to admission | 310 (19.8%) | 5030 (20.4%) | 0.53 | 304 (19.9%) | 717 (19.3%) | 1.5 |
| MI this admission | 346 (22.1%) | 3804 (15.5%) | <0.001 | 338 (22.2%) | 728 (19.6%) | 5.2 |
| MI prior to admission | 252 (16.1%) | 3600 (14.6%) | 0.12 | 248 (16.3%) | 570 (15.3%) | 2.0 |
| Hypotension* | 494 (31.5%) | 8817 (35.8%) | <0.001 | 473 (31.0%) | 1239 (33.4%) | 3.9 |
| Respiratory insufficiency* | 818 (52.2%) | 13,828 (56.2%) | 0.001 | 797 (52.3%) | 2015 (54.3%) | 2.3 |
| Renal insufficiency* | 514 (32.8%) | 9289 (37.7%) | <0.001 | 502 (32.9%) | 1248 (33.6%) | 0.7 |
| Hepatic insufficiency* | 106 (6.8%) | 2300 (9.3%) | <0.001 | 103 (6.8%) | 307 (8.3%) | 4.5 |
| Metabolic or electrolyte abnormality* | 310 (19.2%) | 5197 (21.1%) | 0.07 | 291 (19.1%) | 740 (19.9%) | 1.3 |
| Diabetes mellitus | 475 (30.3%) | 7545 (30.7%) | 0.77 | 462 (30.3%) | 1062 (28.6%) | 2.4 |
| Baseline depression in CNS function | 216 (13.8%) | 3341 (13.6%) | 0.82 | 211 (13.8%) | 495 (13.3%) | 0.1 |
| Major trauma | 71 (4.5%) | 1702 (6.9%) | <0.001 | 68 (4.5%) | 215 (5.8%) | 5.4 |
| Acute stroke | 50 (3.2%) | 1125 (4.6%) | 0.01 | 49 (3.2%) | 133 (3.6%) | 2.1 |
| Pneumonia | 227 (14.5%) | 4304 (17.5%) | 0.002 | 225 (14.8%) | 607 (16.3%) | 5.0 |
| Septicemia* | 263 (16.8%) | 5404 (22.0%) | <0.001 | 258 (16.9%) | 716 (19.3%) | 4.6 |
| Metastatic or hematologic malignancy | 122 (7.8%) | 2784 (11.3%) | <0.001 | 119 (7.8%) | 355 (9.6%) | 5.5 |
| INTERVENTIONS IN PLACE AT TIME OF ARREST | ||||||
| Continuous intravenous vasopressor | 572 (36.5%) | 9157 (37.2%) | 0.57 | 554 (36.4%) | 1371 (36.9%) | 1.1 |
| Dialysis/extracorporeal filtration | 53 (3.4%) | 1144 (4.6%) | 0.02 | 52 (3.4%) | 126 (3.4%) | 0.1 |
| Pre-existing ICD | 31 (2.0%) | 444 (1.8%) | 0.62 | 30 (2.0%) | 75 (2.0%) | 0.0 |
Abbreviations: CNS, central nervous system; CPR, cardiopulmonary resuscitation; ICD, implantable cardioverter-defibrillator; IQR, interquartile range; MI, myocardial infarction; NA, not applicable; SD, standard deviation
Denotes conditions which were present within 24 hours of cardiac arrest
Standardized difference cannot be calculated for a comparison of medians
The propensity score for the overall cohort had good discrimination (c-statistic of 0.783) and led to the successful matching of 1524 patients treated with hypothermia to 3714 patients not treated with hypothermia. Mean age of the propensity score-matched cohort was 62.0 ± 17.5 years, 57.5% were men, and 68.0% were of white race. Prior differences in age, sex, race, initial cardiac arrest rhythm, location of arrest, and comorbidities were well balanced after matching for the overall cohort (see Table 1) and by rhythm type (Supplementary Appendix eTable 1). Temperature data (optional data element) was available for 364 (23.9%) hypothermia and 607 (16.3%) non-hypothermia matched patients. The median lowest achieved temperature was 33.1C (IQR: 32.3C–35.7C) in hypothermia-treated patients (with 76 [20.9%] below the recommended nadir of 32C) and 36.3C (IQR: 35.6, 36.8) in non-hypothermia-treated patients (P<0.001).
Survival to Discharge
In the overall propensity-score matched cohort, 417 (27.4%) patients treated with therapeutic hypothermia survived to hospital discharge, as compared with 1084 (29.2%) non-hypothermia-treated patients. Therapeutic hypothermia was associated with a lower likelihood of in-hospital survival (Relative Risk, 0.88 [95% CI, 0.80, 0.97]; Risk Difference, −3.6% [−6.3%, −0.9%]; P=0.01), and this association was similar (interaction P=0.74) for non-shockable and shockable cardiac arrest rhythms (Table 2).
Table 2. In-Hospital Outcomes and Model Results.
Both relative risks and absolute risk differences are reported for propensity score-matched cohorts.
| Hypothermia | No Hypothermia | Relative Risk With Hypothermia (95% CI) |
Risk Difference With Hypothermia (95% CI) |
P* |
P for Interaction** |
|
|---|---|---|---|---|---|---|
| Survival to Discharge | ||||||
| All cardiac arrests | 417/1524 (27.4%) | 1084/3714 (29.2%) | 0.88 (0.80, 0.97) | −3.6% (−6.3%, −0.9%) | 0.01 | |
| Non-shockable cardiac arrests | 247/1112 (22.2%) | 695/2832 (24.5%) | 0.87 (0.76, 0.99) | −3.2% (−6.2%, −0.3%) | 0.74 | |
| Shockable cardiac arrests | 170/412 (41.3%) | 389/882 (44.1%) | 0.90 (0.77, 1.05) | −4.6% (−10.9%, 1.7%) | ||
|
| ||||||
| Favorable Neurological Survival¶ | ||||||
| All cardiac arrests | 246/1443 (17.0%) | 725/3529 (20.5%) | 0.79 (0.69, 0.90) | −4.4% (−6.8%, −2.0%,) | <0.001 | |
| Non-shockable cardiac arrests | 137/1054 (13.0%) | 446/2723 (16.4%) | 0.78 (0.64, 0.93) | −3.7% (−6.2%, −1.1%) | 0.88 | |
| Shockable cardiac arrests | 109/389 (28.0%) | 279/806 (34.6%) | 0.79 (0.65, 0.97) | −7.3% (−13.3%, −1.3%) | ||
Abbreviation: CI, confidence interval
For comparison of outcomes in the overall cohort
Interaction between hypothermia and initial cardiac arrest rhythm tests whether the estimates of effect were different in the shockable and non-shockable rhythm subgroups
Information on neurological status was not available for 81 hypothermia-treated patients and 185 non-hypothermia-treated patients
A lower proportion of patients in the hypothermia group died during the first day than in the non-hypothermia group (29.1% vs. 45.0%; P<0.001). In sensitivity analysis, wherein the study cohort was restricted to the 3124 (59.6%) propensity score-matched patients who survived the first 24 hours after cardiac arrest, all associations between therapeutic hypothermia and survival persisted (Supplementary Appendix eTable 2). In addition, survival results were not due to higher rates of de novo do-not-resuscitate orders in the hypothermia group after achieving return of spontaneous circulation (Supplementary Appendix eTable 3).
Favorable Neurological Survival
Information on favorable neurological survival was missing on 81 [5.3%] hypothermia-treated patients and 185 [5.0%] non-hypothermia-treated patients. After excluding these patients, therapeutic hypothermia was associated with a lower likelihood of favorable neurological survival for all rhythms (17.0% vs. 20.5%; Relative Risk, 0.76 [0.64, 0.90]; Risk Difference, −4.4% [−6.8%, −2.0%]; P=0.001), with similar patterns in patients with non-shockable and shockable rhythms (interaction P=0.88; Table 2). These results did not change when the analyses were restricted to propensity score-matched patients who survived the first 24 hours after cardiac arrest (see eTable 2).
One-Year Survival
Among 2741 propensity score-matched patients successfully linked to Medicare inpatient files, 706 patients treated with therapeutic hypothermia were matched to 2035 non-hypothermia controls. Cumulative survival throughout the first year was similar between the two groups (2.21 months vs. 2.20 months; P=0.92) (Table 3 and Supplementary Appendix eFigure 1). At one year, 100 (14.2%) hypothermia-treated patients and 286 (14.1%) non-hypothermia-treated patients were alive, and there were no differences in 1-year survival between the two groups overall (Relative Risk, 1.00 [0.96, 1.03; P=0.94) and by rhythm type (see Table 3).
Table 3. One-Year Outcomes and Model Results.
Results reported for mean cumulative survival over the first year and whether patients were alive at 1 year. Cumulative 1-year survival quantifies the area under the survival curve during the first year of follow-up.
| Hypothermia | No Hypothermia |
PROPENSITY SCORE MODEL RESULTS |
P for interaction** | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Cumulative Survival Over First Year (months) | Alive at 1 Year | ||||||||
| Hypothermia | No Hypothermia |
P | Relative Risk With Hypothermia |
Risk Difference With Hypothermia |
P* | ||||
| Crude 1-Year Survival | |||||||||
| All cardiac arrests | 100/706 (14.2%) | 286/2035 (14.1%) | 2.21 | 2.20 | 0.92 | 1.00 (0.96, 1.03) | −0.1% (−3.1%, 2.9%) | 0.94 | |
| Non-shockable arrests | 60/537 (11.2%) | 184/1587 (11.6%) | 1.83 | 1.84 | 0.93 | 1.01 (0.97, 1.04) | 0.5% (−2.7%, 3.6%) | 0.53 | |
| Shockable arrests | 40/169 (23.7%) | 102/448 (22.8%) | 3.44 | 3.44 | 0.99 | 0.97 (0.88, 107) | −2.2% (−9.7%, 5.4%) | ||
For comparison of outcomes in the overall cohort
Interaction between hypothermia and initial cardiac arrest rhythm tests whether the estimates of effect were different in the shockable and non-shockable rhythm subgroups
Discussion
In a large national registry, treatment with therapeutic hypothermia was not associated with higher rates of survival to discharge or favorable neurological survival in patients with in-hospital cardiac arrest and was associated with potential harm. These associations were similar for both shockable and non-shockable cardiac arrest rhythms. When follow-up was extended to one year, there remained no survival advantage with therapeutic hypothermia treatment. Collectively, these findings do not support current use of therapeutic hypothermia for patients with in-hospital cardiac arrest.
To our knowledge, there are no randomized trials of therapeutic hypothermia for in-hospital cardiac arrest, and observational studies are scant and have been underpowered. Kory et al. found no difference in rates of survival to discharge between 17 hypothermia-treated patients (24%) and 16 non-hypothermia-treated patients (31%; P=0.62).4 An early study within GWTG-Resuscitation found no difference in rates of favorable neurological survival between 214 hypothermia-treated patients (18.7%) vs. 8102 non-hypothermia-treated patients (20.1%), but that study involved few patients treated with hypothermia and did not restrict analyses to sites with hypothermia capability.5 A more recent study6 reported improved survival among 42 hypothermia-treated patients, but this study used a limited propensity score derived from 5 factors unrelated to in-hospital cardiac arrest.21 This current study extends the findings of prior studies by including a large study sample, restricting the analyses to hospitals with therapeutic hypothermia capability, requiring all study patients to be on mechanical ventilation, using a robust propensity score, examining outcomes for both shockable and non-shockable cardiac arrest rhythms, and evaluating both in-hospital and one-year survival.
A particular focus of this study was to assess whether unmeasured factors leading to indication bias (e.g., initiating hypothermia in those with a worse prognosis) influenced study results. To address this, a sensitivity analysis that excluded patients who died within the first 24 hours after return of spontaneous circulation was conducted and found that a lower proportion of patients treated with hypothermia died within the first day. This suggests that either therapeutic hypothermia was protective during the first 24 hours after return of spontaneous circulation but not effective overall, or that any indication bias was in favor of patients treated with hypothermia.
Another potential concern is that GWTG-Resuscitation does not collect information on comatose status among patients resuscitated from an in-hospital cardiac arrest. To overcome this limitation, patients were required to be on mechanical ventilation at the time of, or after, cardiac arrest as a surrogate for comatose status. Given a mean duration of cardiopulmonary resuscitation of 16 minutes in both groups and the additional requirement of mechanical ventilation, it is likely that only a few non-comatose patients were included in the study cohort, and any misclassification would be expected to be non-differential. Nonetheless, potential indication bias and misclassification of comatose status further suggest that this study’s findings warrant confirmation with a randomized clinical trial.
The finding that therapeutic hypothermia was not associated with better survival outcomes may raise questions about plausibility. However, clinical trials have found that therapeutic hypothermia leads to worse survival outcomes for other conditions, such as traumatic brain injury22, 23 and bacterial meningitis.24 To date, the only randomized trials to examine therapeutic hypothermia versus no temperature management have been for out-of-hospital cardiac arrest.2, 3 Yet, in-hospital cardiac arrest is a different condition with faster response times (median times of <1 minute to cardiopulmonary resuscitation, 1 minute to first defibrillation,25 and 3 minutes to first epinephrine dose26), potentially limiting the theorized benefit of therapeutic hypothermia to reduce free radical mediated reperfusion injury from anoxic brain injury.27 Moreover, 4 in 5 patients with in-hospital cardiac arrest have an initial rhythm of asystole or PEA—cardiac arrest rhythms for which randomized trials of therapeutic hypothermia do not exist. Additionally, although patients treated with hypothermia in this study achieved, on average, a median lowest temperature of 33.1C, which is consistent with recent trials of therapeutic hypothermia,28 21% of patients treated with hypothermia achieved temperatures below the recommended nadir of 32C. These factors may explain why therapeutic hypothermia for in-hospital cardiac arrest in this registry was not associated with improved short-term or long-term survival, and was possibly harmful. Since therapeutic hypothermia is not without costs, national registries such as GWTG-Resuscitation have a unique opportunity to conduct low-cost, large-scale, pragmatic trials of therapeutic hypothermia treatment in order to establish its efficacy for in-hospital cardiac arrest.29
This study should be interpreted in the context of the following limitations. First, although data available in GWTG-Resuscitation enabled a propensity score analysis which adjusted for a number of key variables that have been linked to survival after cardiac arrest, the possibility of residual confounding remains. Second, GWTG-Resuscitation did not collect detailed data on therapeutic hypothermia protocols and treatments for each patient; therefore, this study reflects outcomes of community implementation of hypothermia treatment. Moreover, temperature data was an optional data field and was not available for most patients. The possibility remains that the null findings for therapeutic hypothermia seen in this study may reflect poor implementation (e.g., insufficient duration of hypothermia), even though the median lowest achieved temperature was 33.1C among patients treated with hypothermia for whom temperature data were available. Also, since the Targeted Management Trial for out-of-hospital cardiac arrest was not published until December of 201328 (a year before the study period ended), the proportion of non-hypothermia-treated patients managed with targeted temperature management of 36C is likely small. Third, there is the possibility that this study may have included some patients who were not comatose post-cardiac arrest. Any misclassification would be expected to be non-differential, but differential misclassification favoring the non-hypothermia group could have influenced the study results. Fourth, results for favorable neurological survival should be interpreted with some caution as variability in assessing neurological status exists30 and some patients were missing data on this outcome. And fifth, although GWTG-Resuscitation is a quality improvement registry that collects cardiac arrest data from a diverse population of U.S. hospitals, findings may be different in nonparticipating hospitals.
Conclusions
Among patients with in-hospital cardiac arrest, use of therapeutic hypothermia compared with usual care was associated with a lower likelihood of survival to hospital discharge and a lower likelihood of favorable neurological survival. These observational findings warrant a randomized clinical trial to assess efficacy of therapeutic hypothermia for in-hospital cardiac arrest.
Supplementary Material
KEY POINTS.
Question
Is therapeutic hypothermia associated with better survival outcomes for patients with in-hospital cardiac arrest?
Findings
In a US national registry, survival outcomes were compared for 26,183 patients who were vs. those who were not treated with therapeutic hypothermia after surviving an in-hospital cardiac arrest. Compared with untreated patients, those treated with therapeutic hypothermia had significantly lower rates of in-hospital survival (27.4% vs. 29.2%), as well as lower rates of survival to discharge with favorable neurological status.
Meaning
Therapeutic hypothermia was not associated with improved survival or better neurological outcomes and was potentially harmful. Current use of therapeutic hypothermia for in-hospital cardiac arrest may warrant reconsideration.
Acknowledgments
Funding/Support:
Dr. Chan is supported by funding (R01HL123980) from the National Heart Lung and Blood Institute.
Footnotes
Disclosures:
Dr. Chan has served as a consultant for the American Heart Association. None of the other authors has any conflicts of interest or financial interests to disclose.
GWTG-Resuscitation is sponsored by the American Heart Association, which had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. The manuscript was reviewed and approved by the GWTG-Resuscitation research and publications committee prior to journal submission.
Authorship: Dr. Chan had full access to all of the data in the study, and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study Concept and design: Chan, Spertus
Acquisition of Data: Chan, Tang
Statistical Analysis: Tang
Analysis and interpretation of data: Chan, Berg, Tang, Curtis,
Drafting of the manuscript: Chan
Critical revision of the manuscript for important intellectual content: Chan, Berg, Tang, Curtis, Spertus
Study Supervision: Chan
References
- 1.Callaway CW, Donnino MW, Fink EL, et al. Part 8: Post-Cardiac Arrest Care: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015;132:S465–482. doi: 10.1161/CIR.0000000000000262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bernard SA, Gray TW, Buist MD, et al. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med. 2002;346:557–563. doi: 10.1056/NEJMoa003289. [DOI] [PubMed] [Google Scholar]
- 3.Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002;346:549–556. doi: 10.1056/NEJMoa012689. [DOI] [PubMed] [Google Scholar]
- 4.Kory P, Fukunaga M, Mathew JP, et al. Outcomes of mild therapeutic hypothermia after in-hospital cardiac arrest. Neurocrit Care. 2012;16:406–412. doi: 10.1007/s12028-011-9664-y. [DOI] [PubMed] [Google Scholar]
- 5.Nichol G, Huszti E, Kim F, et al. Does induction of hypothermia improve outcomes after in-hospital cardiac arrest? Resuscitation. 2013;84:620–625. doi: 10.1016/j.resuscitation.2012.12.009. [DOI] [PubMed] [Google Scholar]
- 6.Perman SM, Grossestreuer AV, Wiebe DJ, Carr BG, Abella BS, Gaieski DF. The Utility of Therapeutic Hypothermia for Post-Cardiac Arrest Syndrome Patients With an Initial Non-Shockable Rhythm. Circulation. 2015;132:2146–2151. doi: 10.1161/CIRCULATIONAHA.115.016317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim YM, Yim HW, Jeong SH, Klem ML, Callaway CW. Does therapeutic hypothermia benefit adult cardiac arrest patients presenting with non-shockable initial rhythms?: A systematic review and meta-analysis of randomized and non-randomized studies. Resuscitation. 2012;83:188–196. doi: 10.1016/j.resuscitation.2011.07.031. [DOI] [PubMed] [Google Scholar]
- 8.Strategies to Improve Cardiac Arrest Survivial: A Time to Act. Institute of Medicine; Washington, D.C.: 2015. [Google Scholar]
- 9.Peberdy MA, Kaye W, Ornato JP, et al. Cardiopulmonary resuscitation of adults in the hospital: a report of 14720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003;58:297–308. doi: 10.1016/s0300-9572(03)00215-6. [DOI] [PubMed] [Google Scholar]
- 10.Cummins RO, Chamberlain D, Hazinski MF, et al. Recommended guidelines for reviewing, reporting, and conducting research on in-hospital resuscitation: the in-hospital ‘Utstein style’. American Heart Association. Circulation. 1997;95:2213–2239. doi: 10.1161/01.cir.95.8.2213. [DOI] [PubMed] [Google Scholar]
- 11.Jacobs I, Nadkarni V, Bahr J, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa) Circulation. 2004;110:3385–3397. doi: 10.1161/01.CIR.0000147236.85306.15. [DOI] [PubMed] [Google Scholar]
- 12.Hammill BG, Hernandez AF, Peterson ED, Fonarow GC, Schulman KA, Curtis LH. Linking inpatient clinical registry data to Medicare claims data using indirect identifiers. Am Heart J. 2009;157:995–1000. doi: 10.1016/j.ahj.2009.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chan PS, Nallamothu BK, Krumholz HM, et al. Long-term outcomes in elderly survivors of in-hospital cardiac arrest. N Engl J Med. 2013;368:1019–1026. doi: 10.1056/NEJMoa1200657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet. 1975;1:480–484. doi: 10.1016/s0140-6736(75)92830-5. [DOI] [PubMed] [Google Scholar]
- 15.Chan PS, Nichol G, Krumholz HM, et al. Racial differences in survival after in-hospital cardiac arrest. JAMA. 2009;302:1195–1201. doi: 10.1001/jama.2009.1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Peberdy MA, Ornato JP, Larkin GL, et al. Survival from in-hospital cardiac arrest during nights and weekends. JAMA. 2008;299:785–792. doi: 10.1001/jama.299.7.785. [DOI] [PubMed] [Google Scholar]
- 17.Rosenbaum PR, Rubin DB. Constructing a control group using multivariate matched sampling methods that incorporate propensity scores. The American Statistician. 1985;39:33–38. [Google Scholar]
- 18.Normand ST, Landrum MB, Guadagnoli E, et al. Validating recommendations for coronary angiography following acute myocardial infarction in the elderly: a matched analysis using propensity scores. Journal of clinical epidemiology. 2001;54:387–398. doi: 10.1016/s0895-4356(00)00321-8. [DOI] [PubMed] [Google Scholar]
- 19.Walker GA. Common Statistical Methods for Clinical Research with SAS® Examples. Cary NC: 2002. Second Edition. [Google Scholar]
- 20.R Development Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing V; Austria; 2008. URL http://www.R-project.org. [Google Scholar]
- 21.Chan PS. Letter to the Editor regarding ‘The Utility of Therapeutic Hypothermia for Post-Cardiac Arrest Syndrome Patients with an Initial Nonshockable Rhythm’. Circulation. 2016 doi: 10.1161/CIRCULATIONAHA.115.020725. In Press for April 26, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Andrews PJ, Sinclair HL, Rodriguez A, et al. Hypothermia for Intracranial Hypertension after Traumatic Brain Injury. N Engl J Med. 2015;373:2403–2412. doi: 10.1056/NEJMoa1507581. [DOI] [PubMed] [Google Scholar]
- 23.Gentilello LM, Jurkovich GJ, Stark MS, Hassantash SA, O’Keefe GE. Is hypothermia in the victim of major trauma protective or harmful? A randomized, prospective study. Annals of surgery. 1997;226:439–447. doi: 10.1097/00000658-199710000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mourvillier B, Tubach F, van de Beek D, et al. Induced hypothermia in severe bacterial meningitis: a randomized clinical trial. JAMA. 2013;310:2174–2183. doi: 10.1001/jama.2013.280506. [DOI] [PubMed] [Google Scholar]
- 25.Chan PS, Krumholz HM, Nichol G, Nallamothu BK. Delayed time to defibrillation after in-hospital cardiac arrest. N Engl J Med. 2008;358:9–17. doi: 10.1056/NEJMoa0706467. [DOI] [PubMed] [Google Scholar]
- 26.Donnino MW, Salciccioli JD, Howell MD, et al. Time to administration of epinephrine and outcome after in-hospital cardiac arrest with non-shockable rhythms: retrospective analysis of large in-hospital data registry. BMJ. 2014;348:g3028. doi: 10.1136/bmj.g3028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Leonov Y, Sterz F, Safar P, et al. Mild cerebral hypothermia during and after cardiac arrest improves neurologic outcome in dogs. J Cereb Blood Flow Metab. 1990;10:57–70. doi: 10.1038/jcbfm.1990.8. [DOI] [PubMed] [Google Scholar]
- 28.Nielsen N, Wetterslev J, Cronberg T, et al. Targeted temperature management at 33 degrees C versus 36 degrees C after cardiac arrest. N Engl J Med. 2013;369:2197–2206. doi: 10.1056/NEJMoa1310519. [DOI] [PubMed] [Google Scholar]
- 29.Lauer MS, D’Agostino RB., Sr The randomized registry trial–the next disruptive technology in clinical research? N Engl J Med. 2013;369:1579–1581. doi: 10.1056/NEJMp1310102. [DOI] [PubMed] [Google Scholar]
- 30.Ajam K, Gold LS, Beck SS, Damon S, Phelps R, Rea TD. Reliability of the Cerebral Performance Category to classify neurological status among survivors of ventricular fibrillation arrest: a cohort study. Scand J Trauma Resusc Emerg Med. 2011;19:38. doi: 10.1186/1757-7241-19-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


