Abstract
Purpose
A large body of evidence clearly shows that cancer patients experience significant health benefits with smoking cessation. Cancer Care Ontario, the provincial agency responsible for the quality of cancer services in Ontario, has undertaken a province-wide smoking cessation initiative. The strategies used, the results achieved, and the lessons learned are the subject of the present article.
Methods
Evidence related to the health benefits of smoking cessation in cancer patients was reviewed. A steering committee developed a vision statement for the initiative, created a framework for implementation, and made recommendations for the key elements of the initiative and for smoking cessation best practices.
Results
New ambulatory cancer patients are being screened for their smoking status in each of Ontario’s 14 regional cancer centres. Current or recent smokers are advised of the benefits of cessation and are directed to smoking cessation resources as appropriate. Performance metrics are captured and used to drive improvement through quarterly performance reviews and provincial rankings of the regional cancer centres.
Conclusions
Regional smoking cessation champions, commitment from Cancer Care Ontario senior leadership, a provincial secretariat, and guidance from smoking cessation experts have been important enablers of early success. Data capture has been difficult because of the variety of information systems in use and non-standardized administrative and clinical processes. Numerous challenges remain, including increasing physician engagement; obtaining funding for key program elements, including in-house resources to support smoking cessation; and overcoming financial barriers to access nicotine replacement therapy. Future efforts will focus on standardizing processes to the extent possible, while tailoring the approaches to the populations served and the resources available within the individual regional cancer programs.
Keywords: Smoking cessation, program implementation
BACKGROUND
Cancer Care Ontario (cco) oversees the quality of cancer services in the province of Ontario. It develops standards and guidelines through the Program in Evidence-Based Care at McMaster University (https://www.cancercare.on.ca/toolbox/qualityguidelines); maps best practices through a disease pathway management initiative (https://www.cancercare.on.ca/ocs/qpi/dispathmgmt); and uses funding models, quality metrics, and performance management to drive change. However, until recently, an important component of quality care—an initiative supporting newly diagnosed cancer patients to quit smoking—was absent. Patients were not routinely assessed for their smoking or tobacco use status, and they were not offered assistance in making a quit attempt, despite strong evidence of benefit1,2. The 2014 report from the U.S. Surgeon General identified that continued smoking after a diagnosis of cancer can increase all-cause mortality, lead to greater toxicity from therapeutic interventions, and increase the incidence of second malignancies2. The report also suggested that the risk of dying from cancer could be lowered by 30%–40% by smoking cessation at the time of diagnosis2. Here, we describe the steps taken and the lessons learned by cco in implementing a province-wide smoking cessation initiative in its regional cancer programs (rcps).
METHODS
Planning
In 2011, data about the potentially large survival benefits of smoking cessation in patients receiving treatment for lung and head-and-neck cancer were presented to cco leaders3,4. That presentation resulted in the formation of a steering committee on smoking cessation that was tasked with developing an implementation framework for the rcp smoking cessation initiative (“the initiative”). The committee included experts in smoking cessation from the University of Ottawa Heart Institute, the Centre for Addiction and Mental Health, the Registered Nurses’ Association of Ontario, and the Canadian Cancer Society, among others. The committee produced a framework, a set of recommendations for action, and a vision statement: “By systematically offering a smoking cessation intervention to every ambulatory cancer patient, the Regional Cancer Program smoking cessation initiative will help to ensure that cancer patients in Ontario achieve the best possible health benefits from their cancer treatments.”
The Smoking Cessation Framework
The geographic size, population density, and target population size for smoking cessation in each of the 14 health regions in Ontario varies considerably. The resources available to support the initiative also varied considerably between the rcps. For those reasons, the committee developed a smoking cessation framework (“the framework”) that could be adapted to individual regional circumstances.
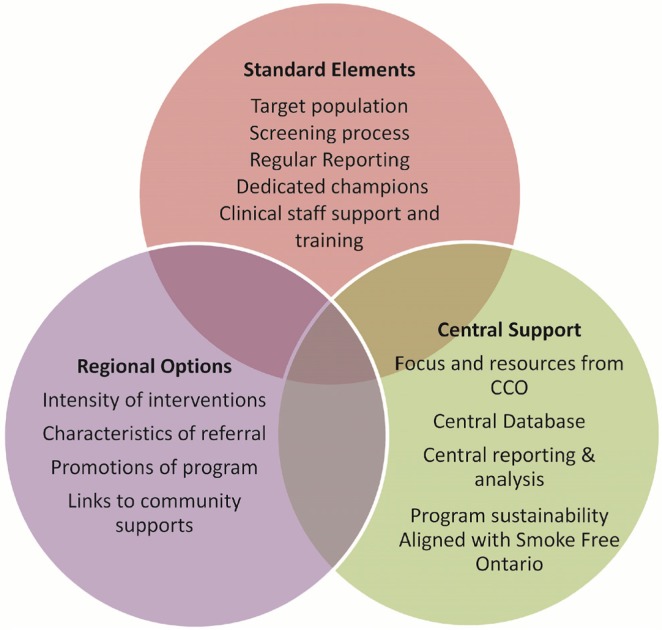
The framework consisted of three components (Figure 1): a set of standard program elements, regional options, and central administrative support. The standard elements were the target population to be screened for tobacco use (new ambulatory cancer patients), standard screening questions, identification of current and recent smokers (those who had smoked in the preceding 6 months), a smoking cessation champion, training of health care providers, and regular reports of performance metrics to cco.
FIGURE 1.
Framework components of the smoking cessation initiative. CCO = Cancer Care Ontario.
The regional options were items that could be tailored to the rcp’s specific conditions, such as the intensity of the smoking cessation intervention (brief to intensive), the referral type (referral within the regional cancer centre or hospital, or to an external community partner), the agencies with which to partner in the local community, how to promote the initiative, and risk mitigation strategies.
Central administrative support included a dedicated team at cco, a central database with reporting and analytics, guidance from experts in smoking cessation, and alignment with the provincial government’s Smoke-Free Ontario strategy.
Implementation Recommendations
The steering committee made 6 implementation recommendations:
-
■ Recommendation 1 Screen all new ambulatory cancer patients for smoking status.
New ambulatory cancer patients should be screened for tobacco use, preferably by a nurse or physician, at the time of initial consultation for surgery, radiation, or chemotherapy.
-
■ Recommendation 2 Standardize the screening question, referral questions, and data collection.
For comparability of reported data, a standardized question should be used to capture smoking status. The recommended screening question was “Have you used tobacco products, such as cigarettes, pipes, cigars or chewing tobacco, in the past 6 months?” Six months was used to identify patients who might have quit smoking before their cancer diagnosis, but who still remain susceptible to relapse.
-
■ Recommendation 3 Monitor the effectiveness of the smoking cessation initiative.
It was recommended that metrics be developed and reported back to the rcps and be used for performance management. Data were to be captured electronically in a central database, analyzed centrally, and reported according to a documented methodology.
-
■ Recommendation 4 Develop and maintain an inventory of smoking cessation services within each region.
An inventory of regional smoking cessation resources should be developed by each region and kept current. Information on services such as the Canadian Cancer Society’s government-funded telephone quit line (Smokers’ Helpline), trained community-based pharmacists, and hospital- and community-based smoking cessation clinics should be made available to staff, patients, and their families.
-
■ Recommendation 5 Establish partnerships.
Partnerships between rcps and local smoking cessation services should be developed and fostered to assist in making referrals of patients to smoking cessation clinics that are close to the cancer centre or to the patient’s residence. Potential partners could include government and non-governmental organizations such as the cco Aboriginal Tobacco Program, the Canadian Cancer Society, public health units, and Tobacco Control Area Networks.
-
■ Recommendation 6 Take steps to minimize the risks to implementation and sustainability.
Mitigation strategies to address perceived threats to implementation and sustainability should be addressed to the extent possible at both the regional and provincial level, including lack of infrastructure (internal and external), limited funding, level of staff buy-in and training, patient motivation, and the cost of smoking cessation pharmacotherapy.
Implementation
Senior-Level Commitment and Infrastructure Support
Senior leadership at both the provincial and regional levels of cco recognized the need to demonstrate commitment and to provide administrative support for the initiative. Executives and regional vice-presidents at cco endorsed the initiative through the cco Provincial Leadership Council, supported the establishment of a provincial secretariat, and agreed to the steering committee’s framework recommendations. The steering committee was replaced by an advisory committee to provide ongoing expert guidance on refinements to the implementation process, evaluation of the framework, and future expansion of the initiative.
Regional “smoking cessation champions” were appointed at each of the 14 rcps to advance the initiative within each unique regional setting. Champions were selected for their enthusiasm to lead, their communication skills, and their knowledge of smoking cessation. Champions were accountable to their regional vice-president for implementation of the initiative.
A smoking cessation secretariat at cco was established under the vice-president of Prevention and Cancer Control. The secretariat organized regular meetings of the advisory committee and the smoking cessation champions; communicated the goals of the initiative; developed, captured, analyzed, and reported on the smoking cessation performance metrics (described later in this article); and developed patient-facing materials about the health benefits of smoking cessation. Monthly teleconference and Web meetings with the champions allowed for information exchange about effective practices to engage health care providers and patients. An in-person meeting of the champions has been held annually to review the status of the initiative and to showcase best practices.
Implementation Processes
Cancer centres were encouraged to adopt the 5 As (Ask, Advise, Assess, Assist, Arrange) model of smoking cessation5; however, a specific approach for screening patients was not prescribed, nor was the methodology for documentation standardized. Furthermore, the rollout of the initiative varied across the province, with some centres launching the initiative across all treatment programs at the same time and others piloting it selectively for specific disease sites such as lung cancer, where smoking rates are high. Most regional cancer centres had health care providers screen patients for smoking status during the first clinical consultation; however, a few screened patients at registration using a history form that was self-administered or completed with clerical staff.
The various information systems used by the regional cancer centres posed an implementation problem. Some systems could be readily modified to capture and submit data to cco. However, a standalone secure file transfer system had to be set up at a few centres to enable quarterly reporting. In the early months of the program, the volume and quality of the data submitted varied considerably. Data on smoking cessation activities is now captured in cco’s Activity Level Reporting file, which is submitted monthly together with the other metrics routinely reported to cco by the rcps.
Historically, only a small amount of government funding ($35,000) had been incorporated into the rcp annual budgets for prevention activities. With provincial implementation of the initiative, centres were directed to commit those funds to smoking cessation. In addition, the provincial Ministry of Health and Long-Term Care provided a similar amount of funding to be used over 3 fiscal years. Funds were used to support the smoking cessation counsellor, education and marketing activities, and purchase of nicotine replacement therapy.
Communicating the Rationale for the Initiative and Motivating Health Care Providers
Evidence about the health benefits of smoking cessation for cancer patients from the American Association for Cancer Research policy statement1 and the U.S. Surgeon General’s 2014 report2 were presented at rounds in most of the province’s regional cancer centres. Compared with mid-day rounds (which often conflicted with clinics), evening dinner meetings appeared to be the most successful in attracting physician attendance. A common reaction from the physicians was one of surprise at the magnitude of the benefit possible with smoking cessation.
Despite the evidence, many oncologists still questioned the utility of recommending smoking cessation to patients with advanced disease. They also expressed concern about an increased workload. The education sessions emphasized brief physician interventions using a script that informed patients of the importance of smoking cessation to achieve the best results from their cancer treatment. Oncologists were encouraged to refer patients to appropriate smoking cessation services within the cancer centre, hospital, or community, and to be firm and directive when speaking with the patient about the importance of smoking cessation.
Evaluation and Ongoing Monitoring
Five key performance metrics have been used to monitor the initiative:
■ The proportion of ambulatory cancer patients screened for their smoking status
■ The proportion of those screened who were current or recent smokers
■ The proportion of current or recent smokers who were advised about the benefits of quitting smoking
■ The proportion of those advised to quit smoking who were recommended for referral to smoking cessation services
■ The proportion of those offered a referral who accepted it (If a referral was accepted, the type of referral was also captured and was measured as the proportion who accepted a referral to an internal cancer centre resource, an external resource, or both.)
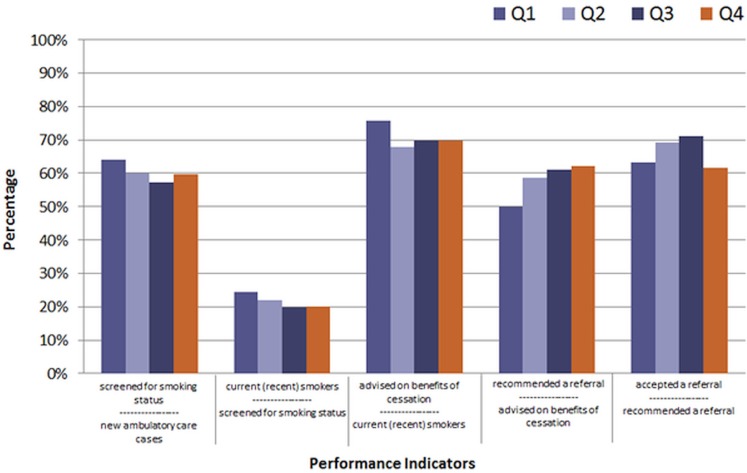
Figure 2 shows the indicators for 2014–2015. Although the data during fiscal year 2014–2015 were of variable quality, they did show that approximately 60% of new ambulatory cancer patients attending cancer centres in the province of Ontario were screened for their smoking status. The screening rate varied from a low of 26.0% to a high of 97.3%. Approximately 20% of those screened were current or recent smokers. Of patients who were recommended for referral, approximately 65% were receptive (Figure 2).
FIGURE 2.
Smoking cessation performance indicators, Ontario average (14 regional cancer centres), fiscal year 2014–2015.
A preliminary evaluation of the initiative was conducted in 2015 to better understand implementation barriers and to provide recommendations for improvement. Three evaluation methods were used:
■ A process flow review focused on how the initiative had been implemented and the data reported.
■ An online survey was conducted.
■ A key-informant interview with the smoking cessation champion was held.
The evaluation identified significant variability in regional processes. For example, when patients were screened for their smoking status and smokers were advised on the benefits of quitting, a health care provider (nurse, radiation therapist, or oncologist) conducted the interaction at most rcps. However, at 2 centres, a registration clerk asked the questions, and at 1 site, the patient completed a paper form before interacting with a health care provider. The latter site reported a 100% “advised” rate (assuming that all smokers read the advice on the form), and so although the performance metric appeared strong, their approach could not be considered a best practice.
Documentation issues were repeatedly raised as a major challenge. Centres differed concerning the method used to capture data, with some sites using direct-entry electronic medical record systems with mandatory fields. That choice improved compliance and facilitated data extraction and reporting. In contrast, other sites used paper or paper–electronic hybrid systems, which commonly resulted in incomplete data.
The rcps also differed in the types of cessation services offered. A few sites had a dedicated in-house cessation specialist—a choice that facilitated referrals and improved patient acceptance. In contrast, other sites were able to offer a referral only to a telephone helpline. A key data issue was that “acceptance” of a referral did not necessarily lead to actual contact with a smoking cessation service.
LEARNINGS AND NEXT STEPS
The preliminary evaluation led to several recommendations to refine the implementation model, including creation of a cancer-specific best practice guideline for smoking cessation in oncology settings and a tailored action plan for each rcp.
In view of a perception of resistance among clinicians, continuing education must be a priority to reach all health care providers in the cancer system, as well as communitybased primary care providers. Despite presentations in most regional cancer centres on the topic of the health benefits of smoking cessation for cancer patients (up to three annual presentations having been made at some centres), it appears that a substantial number of oncologists have not yet heard the message. An ongoing effort of further in-person presentations, use of Ontario’s telemedicine network, contributions to professional association and hospital newsletters, and collaboration with cco’s regional primary care leads will be required.
Key messages pertaining to the benefits of smoking cessation in the oncology setting have to reach all physicians and other health care providers caring for cancer patients. Providers such as radiation therapists and chemotherapy suite nurses have regular contact with patients and develop trusting relationships that can be used to influence patients to quit smoking. A planned survey of health care providers will help to determine the extent to which knowledge of the health benefits of smoking cessation has been heard and actioned.
Persistence is needed to change the culture of the cancer system from one that accepts continued smoking by cancer patients as one of their few pleasures or views it as being “too late” to help the patient to quit, to one that recognizes that cancer patients who stop smoking can gain significant health benefits.
The advisory committee recently suggested that the approach for new patients could be simplified to a 2 As, 1 R model: Ask, Advise, and Refer patients to a smoking cessation service. Patients have to stop smoking as quickly as possible and before starting anticancer therapy, which makes it unrealistic to assess their willingness to quit. The diagnosis of cancer has to be used as a teachable moment that leads directly to a recommendation for referral to cessation services.
Into the future, the two key metrics to be monitored will be the proportion of all new ambulatory cancer patients who are screened for their smoking status, and the proportion of current smokers who accept a referral for smoking cessation services. The first of those metrics (“tobacco use screening”) has been incorporated into cco’s quarterly performance reviews with the rcps and into the regional scorecard. The second metric (“referral acceptance”) is also reported in the quarterly reviews and will be included in the 2017–2018 scorecard. Regional vice-presidents are expected to develop action plans to improve declining or poor performance. The provincial scorecard measures rcp performance against provincial targets and determines the ranking of the regional cancer centre within the provincial cancer system—a strong incentive for improvement, which has been demonstrated to drive change.
This cco initiative has attracted broad interest and resulted in the Canadian Partnership Against Cancer issuing a request for proposals to all of the provincial and territorial cancer agencies to compete for funding to help plan, implement, or evaluate smoking cessation initiatives. Cancer Care Ontario has obtained funding to further refine the implementation model. It is now clear that certain processes, such as screening and data reporting, will need to be standardized according to best practices. In particular, screening accompanied by advice to quit is most effective when provided by a health care provider, such as the consultant oncologist or clinic nurse.
SUMMARY
This cco smoking cessation initiative has had considerable province-wide implementation success because of the commitment of senior leadership, the guidance of smoking cessation experts, and the enthusiastic efforts of the regional smoking cessation champions. The initiative has been enabled by a secretariat at cco that supports the efforts of the regional champions and collects and analyzes smoking cessation data. Collaboration with other agencies, including the Canadian Cancer Society, has resulted in the development of standardized patient information materials about why it is important for cancer patients to stop smoking after a diagnosis of cancer and about how they can quit.
However, the initiative is not as robust as it could be because of several factors: lack of funding for dedicated smoking cessation champions and the financial barriers affecting access to nicotine replacement therapy in Ontario. The current environment of fiscal constraint has reduced the funds that hospitals can commit to smoking cessation interventions, which in turn affects the regional cancer centres and their programming. The cco smoking cessation initiative is limited to new ambulatory cancer patients, but it ideally should be extended to all cancer patients, their caregivers, and those attending Ontario’s cancer screening programs. As low-dose computed tomography screening for the high-risk lung cancer population is introduced in Ontario, smoking cessation will have to be incorporated to maximize the benefits of the program. Finally, Ontario’s primary care providers have to be informed about the health benefits of smoking cessation for cancer patients so that the advice provided in the cancer centres is reinforced in the primary care setting.
CONFLICT OF INTEREST DISCLOSURES
We have read and understood Current Oncology’s policy on disclosing conflicts of interest, and we declare that we have none.
REFERENCES
- 1.Toll BA, Brandon TH, Gritz ER, Warren GW, Herbst RS, on behalf of the aacr Subcommittee on Tobacco and Cancer Assessing tobacco use by cancer patients and facilitating cessation: an American Association for Cancer Research policy statement. Clin Cancer Res. 2013;19:1941–8. doi: 10.1158/1078-0432.CCR-13-0666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.United States, Department of Health and Human Services, Centers for Disease Control and Prevention (cdc), National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health . The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Atlanta, GA: CDC; 2014. [Available online at: http://www.surgeongeneral.gov/library/reports/50-years-of-progress; cited 15 January 2016] [Google Scholar]
- 3.Parsons A, Daley A, Begh R, Aveyard P. Influence of smoking cessation after diagnosis of early stage lung cancer on prognosis: systematic review of observational studies with meta-analysis. BMJ. 2010;340:b5569. doi: 10.1136/bmj.b5569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Browman GP, Wong G, Hodson I, et al. Influence of cigarette smoking on the efficacy of radiation therapy in head and neck cancer. N Engl J Med. 1993;328:159–63. doi: 10.1056/NEJM199301213280302. [DOI] [PubMed] [Google Scholar]
- 5.Clinical practice guideline treating tobacco use and dependence 2008 update panel, liaisons, and staff A clinical practice guideline for treating tobacco use and dependence: 2008 update. A U.S. Public Health Service report. Am J Prev Med. 2008;35:158–76. doi: 10.1016/j.amepre.2008.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]