Abstract
Background
The Odette Cancer Centre’s recent implementation of a rapid diagnostic unit (rdu) for breast lesions has significantly decreased wait times to diagnosis. However, the economic impact of the unit remains unknown. This project defined the development and implementation costs and the operational costs of a breast rdu in a tertiary care facility.
Methods
From an institutional perspective, a budget impact analysis identified the direct costs associated with the breast rdu. A base-case model was also used to calculate the cost per patient to achieve a diagnosis. Sensitivity analyses computed costs based on variations in key components. Costs are adjusted to 2015 valuations using health care–specific consumer price indices and are reported in Canadian dollars.
Results
Initiation cost for the rdu was $366,243. The annual operational cost for support staff was $111,803. The average per-patient clinical cost for achieving a diagnosis was $770. Sensitivity analyses revealed that, if running at maximal institutional capacity, the total annual clinical cost for achieving a diagnosis could range between $136,080 and $702,675.
Conclusions
Establishment and maintenance of a breast rdu requires significant investment to achieve reductions in time to diagnosis. Expenditures ought to be interpreted in the context of institutional patient volumes and trade-offs in patient-centred outcomes, including lessened patient anxiety and possibly shorter times to definitive treatment. Our study can be used as a resource-planning tool for future rdus in health care systems wishing to improve diagnostic efficiency.
Keywords: Diagnostics, costs, breast cancer
INTRODUCTION
Breast cancer is the most common cancer in women, and diagnostic delays have been shown to increase the related morbidity and mortality1–5. Furthermore, the diagnostic phase of breast cancer is an anxiety-provoking and stressful experience for the patient and the family6. Although published guidelines outline the appropriate diagnostic algorithms for breast cancer, few recommendations have addressed standardizing the timeliness with which such investigations should occur7,8.
Analyses of breast cancer diagnostic times in Canada have shown a general increase in wait time since the end of the 1990s7,9. That increase is attributed to an increased demand for services without a parallel rise in resources. Concerns about diagnostic delay, particularly in the context of a publicly funded health care system, have spurred the need for fast-track cancer referral routes7.
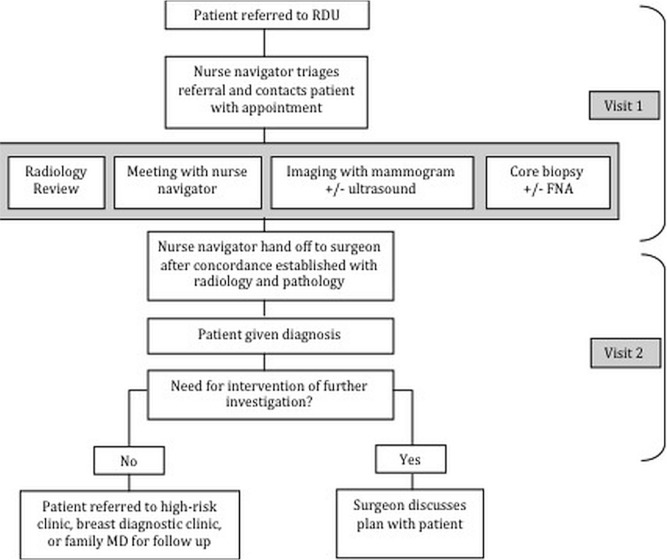
In 2011, a multidisciplinary team of breast cancer specialists at our centre implemented a rapid diagnostic unit (rdu) to improve the efficiency of the diagnostic process for women with highly suspicious breast lesions. The rdu primarily made use of the pre-existing physical infrastructure at our institution (for example, clinical space and diagnostic equipment), but changed the process and philosophy, enabling us to significantly lower the wait time to a definitive diagnosis10. Moreover, the addition of support staff allowed the diagnostic process to be streamlined as illustrated in Figure 1. With the rdu initiative, the wait time from referral to diagnosis decreased, on average, to 2 days from 16 days. Decreases in the wait time have been shown to positively affect patient-reported outcomes8. However, the economic impact of implementing a rdu remains unknown. The goals of the present study were
■ to perform a budget impact analysis (bia) in which the short-term costs associated with the development and ongoing operation of an institutional breast rdu were defined from the hospital’s perspective, and
■ to calculate the average cost per patient and the overall cost burden of achieving a definitive diagnosis.
FIGURE 1.
Patient flow through the breast rapid diagnostic unit (RDU). FNA = fine-needle aspiration.
METHODS
Study Design
Using a bia, we identified all direct costs associated with implementation of our institution’s breast rdu and also its annual operational costs. The purpose of a bia is to address the expected short-term undiscounted changes in the expenditure of a health care system after adoption of a new intervention or process11. In addition, we created a base-case model to calculate the average cost per patient needed to achieve a definitive diagnosis. The study was approved by our institution’s research ethics board.
Patient Population and Base-Case Definition
The Odette Cancer Centre at Sunnybrook Health Sciences Centre is the 6th largest comprehensive cancer centre in North America. The breast rdu was implemented with the goal of providing rapid assessment and diagnosis delivery for individuals with a suspicious abnormality detected on mammography, breast ultrasonography, or clinical examination. With a streamlined design, a dedicated nurse navigator, and a triage coordinator, the rdu aims to reduce not only the time a patient waits for results, but also the number of outpatient appointments required to obtain a diagnosis (Figure 1). Any physician within the province can refer a patient to the rdu. Before implementation of the rdu, patients with suspicious breast lesions were referred to individual clinicians and often required multiple visits to complete their diagnostic assessment.
The base case was modelled in view of a typical rdu patient with a highly suspicious lesion who requires
■ an initial radiology consultation and review of diagnostic images from the past or from the referring institution;
■ bilateral mammography with at least 2 additional cone or magnification views;
■ unilateral breast ultrasonography;
■ ultrasonography-guided or stereotactic core biopsy (with radiography of the biopsy specimen to ensure retrieval of microcalcifications from the biopsy and site concordance);
■ pathology analysis of the core biopsy specimen; and
■ a surgical oncology consultation. (At our institution, the surgical oncology team oversees the diagnostic process and discloses results to the patients.)
Time Horizon and Perspective
A bia takes the payer’s or the budget holder’s perspective. In our health care system, implementation of an rdu affects the institutional (hospital) budget. The time horizon for ongoing operational costs is 1 year. We also report the total annual costs for achieving patient diagnoses (the product of cost per patient and anticipated patient volume).
Costs
Cost categories were the rdu initiation costs, the ongoing operational costs, and the average cost per patient to achieve diagnosis. Initiation and operational costs are reported from the perspective of the institution, and the cost per patient reflects the overall cost burden to achieve a diagnosis. The clinic infrastructure was already in place in the pre-rdu era, and therefore major overhead costs related to operating a breast oncology clinic were not included in the present analysis. Similarly, capital expenditures related to pre-existing equipment (for example, mammography and sonography machines) are also not included. Rather, we focus on the incremental costs associated with the rdu (when compared with a non-rdu clinical program).
The initiation costs are the direct costs associated with planning and implementing the rdu, including fees for consultants, personnel training, and the purchase of two rapid tissue processors (required to expedite the pathology analysis of biopsied breast specimens), as well as the costs related to continuous quality control and validation of the rapid tissue processor results. The American Society of Clinical Oncology and the American College of Pathologists recommend that any change in pre-analytical variables such as fixation time and tissue processing protocols be fully validated before tests for hormone receptors and her2 (the human epidermal growth factor receptor) can be reliably performed12,13. Personnel training consisted of teaching all staff involved in the rdu (pathologists, surgeons, radiologists, nurses, technologists and technicians, and other support staff) the new clinic processes, in keeping with the “lean” philosophy. Training was conducted by a third-party private consulting service. The lean approach is a customer-centric quality improvement methodology widely used in industry and applied in health care to continuously improve processes through reduction of waste and a focus on increasing efficiency and maximizing valuebased activities14–17.
Ongoing operational costs included clerical and administrative support (rdu triage coordinator), and a full-time-equivalent nurse navigator. The nurse navigator and triage coordinator’s salaries met the provincial standardized unionized rates, with benefits included. Although a full-time-equivalent nurse navigator is budgeted, the position functionally includes the part-time contributions of several people. As such, many individuals with interchangeable training and skills are able, as a team, to manage the role.
The cost per patient for achieving a diagnosis was determined using physician billing claims and invoices from the pathology laboratory. The costs of physician billing claims are standardized and published by the province of Ontario18 and were used to determine the costs of diagnostic breast image interpretation and image-guided biopsies, and the consultation fees for surgeons, radiologists, and pathologists. Invoices from the pathology laboratory were used to determine the costs of processing and analyzing the biopsied or aspirated specimens, including gross specimen handling, tissue processing, block embedding, slide preparation, hematoxylin and eosin staining, immunohistochemistry for diagnosis and biomarkers, fluorescence in situ hybridization for her2 results that were equivocal on immunohistochemistry, and cytology analysis of fine-needle aspirate samples when accompanying a surgical specimen.
All costs are reported in adjusted 2015 Canadian dollars using health care–specific consumer price indices to account for inflation19.
Analysis
Summative costs were generated for the three cost categories of interest: rdu initiation costs, annual operational costs, and cost per patient to achieve a diagnosis. Cost per patient entails only the costs required to achieve a diagnosis, using the base-case model. Additional tests required after diagnosis or the costs associated with treatment of breast cancer are not included (for example, staging tests or magnetic resonance imaging); they are beyond the scope and purpose of the rdu and this analysis.
Sensitivity analyses were performed to compute costs based on feasible variations in the cost-per-patient needed to achieve a diagnosis. We determined the least and greatest cost-per-patient scenarios by varying the investigations required in the base case to achieve a diagnosis. The least costly cost-per-patient scenario occurs when imaging and physician consultation suffice to make a definitive diagnosis (that is, no biopsy needed). The most costly diagnostic scenario for an individual patient occurs when, in addition to the standard tests, requirements extend to bilateral breast ultrasonography, additional mammographic cone views, repeat or bilateral breast biopsies, a fine-needle aspirate of a suspicious lymph node for cytology analysis, fluorescence in situ hybridization for biomarkers to resolve equivocal immunohistochemistry results, and repeat surgical assessment (additional required visit). Our previous work showed that approximately 30% of rdu patients with invasive breast carcinoma require fluorescence in situ hybridization analysis10. Approximately 10% of patients require more than 1 core biopsy, and fewer than one quarter of referred patients require fine-needle aspiration to achieve a diagnosis10.
To account for variations in referral and the annual patient volume, we determined the range of annual operational costs if the rdu were to be running at maximal capacity. Based on the number of allotted rdu slots or appointments available in the radiology suite, the rdu’s maximal capacity is 405 patients per year (9 slots per week for 45 weeks).
RESULTS
The initiation cost of the rdu was $366,243 (Table i). Given that most of the infrastructure was already in place before implementation of the rdu, the most substantial cost was the purchase of two rapid tissue processors to allow for pathology diagnoses within 24 hours. The second-largest cost consisted of quality control or validation of the rapid tissue processors by repeat pathology testing using standard processing on all biopsy specimens. The third-largest cost was training of physicians, technologists, support staff, nurses, and allied health members.
TABLE I.
Initiation costs for the breast rapid diagnostic unit
| Item | Cost (2015 CA$) |
|---|---|
| Rapid tissue processorsa (n = 2) | 280,396 |
| Quality control and validation of tissue processors | 40,331 |
| Staff training (Lean event) | 32,589 |
| Lean consultant | 12,410 |
| Printer | 517 |
| TOTAL | 366,243 |
15-Year lifespan.
The annual operational expenditure is $111,803 (Table ii), which includes ongoing compensation for a nurse navigator and a triage coordinator.
TABLE II.
Annual operations costs for the breast rapid diagnostic unit (RDU)
| Item | Cost (2015 CA$) |
|---|---|
| RDU nurse navigator (1 full-time equivalent) | 103,414 |
| Triage coordinator and clerical support (0.15 full-time equivalent) | 8,389 |
| TOTAL | 111,803 |
Table iii depicts the cost of achieving a diagnosis in the modelled base case, representative of a typical patient referred to the rdu.
TABLE III.
Cost of achieving a diagnosis in a modelled base-case patient
| Item | Cost (2015 CA$) |
|---|---|
| Initial radiology consultation | 50 |
| Interpretation of ... | |
| Bilateral mammograms | 64 |
| Additional cone views | 22 |
| Unilateral ultrasonography images | 40 |
| Image-guided core biopsy and radiography of biopsy specimen | 94 |
| Pathology analysisa | 340 |
| Surgical consultation | 160 |
| TOTAL | 770 |
Cost includes tissue processing and block embedding, preparation of slides, immunohistochemistry for biomarkers (estrogen, progesterone, and HER2 receptors), and professional fee for technicians and pathologist to review the case.
Sensitivity analyses revealed that, if the rdu were to run at maximal institutional capacity (n = 405), the total clinical cost for achieving a definitive diagnosis could range from $136,080 to $702,675 annually. The least costly trajectory for a referred patient is $336 (Table iv), when biopsy is not indicated after appropriate review of diagnostic images by a breast radiologist (because of benign appearance on imaging). The most costly trajectory for a patient referred to the rdu is estimated to be $1735 for those requiring repeat biopsies and additional tests to achieve diagnostic certainty (Table iv). In sum, the cost per patient can range anywhere from $336 to $1735 dollars, depending on clinician decisions and patient needs. In Canada, payment to achieve a definitive diagnosis derives from two major sources: the institution, which provides personnel and equipment for testing, and the government, which provides physician compensation. Here, however, both are combined in the cost-per-case calculation (Tables iii and iv) to illustrate the overall economic burden of diagnostic testing for breast patients.
TABLE IV.
Sensitivity analyses demonstrating variations in cost-per-patient needed to achieve a diagnosis
| Item | Cost (2015 CA$) | |
|---|---|---|
|
| ||
| Least | Most | |
| Initial radiology consultation | 50 | 50 |
| Interpretation of ... | ||
| Bilateral mammograms | 64 | 64 |
| Additional cone views | 22 | 22 |
| Ultrasonography images | 40 (unilateral) | 80 (bilateral) |
| Surgical consultation | 160 | 160 |
| Image-guided core biopsy and radiography of biopsy specimen | NA | 94 |
| Pathology analysisa | NA | 340 |
| Fluorescence in situ hybridization | NA | 334 |
| Aspiration biopsy by radiology for FNA | NA | 79 |
| FNA (cytology analysis and interpretation) | NA | 20 |
| Repeat stereotactic core biopsy and radiography of biopsy specimen | NA | 94 |
| Repeat pathology analysis | NA | 340 |
| Repeat surgical assessment | NA | 58 |
| TOTAL | 336 | 1735 |
Cost includes tissue processing and block embedding, preparation of slides, immunohistochemistry for biomarkers (estrogen, progesterone, and HER2 receptors), and professional fee for technicians and pathologist to review the case.
NA = not applicable; FNA = fine-needle aspiration.
DISCUSSION
Our bia is the first of its kind, portraying the expected expenditure related to rdu implementation for suspicious breast lesions in a tertiary health care centre. After an initial investment of $366,243, annual operational costs are $111,803. The annual costs for achieving a diagnosis can range from $136,080 to $702,675, depending on institutional case mix (based on our maximal capacity of 405 cases annually).
The rdu has been shown to lower patient wait times to definitive diagnosis—a result achieved by changing system-level processes10. Similarly, at other institutions, the cost of streamlining and expediting the diagnostic journey has shown to be a valuable investment, reducing delays in breast cancer diagnosis20,21. Cancer Care Ontario has mandated that wait times for cancer care be decreased, and thus rdus are strategically in line with health care goals22,23. To date, the price for expedited cancer care remains unknown. Given the financial restraints experienced in the current health care system, bias are crucial for resource planning and allocation; they provide the basis for future cost-effectiveness analyses.
Thus far, no other studies have looked at the incremental costs associated with rdus. Arnaout et al.6 described the experience with their Rapid Diagnosis and Support breast clinic initiative. As at our institution, their new clinical model significantly lowered diagnostic wait times while improving patient satisfaction6,10. However, the only costs they reported were the incremental nursing salary ($20,731) and the increased cost for the required radiology technologist time and equipment after the addition of 10 biopsy days ($6100)6. Albeit not the primary purpose of their study, that economic assessment is limited and did not capture all the direct costs associated with implementing and operationalizing a rdu.
To our knowledge, our bia is the first related to a cancer rdu. Other health care systems have adopted rdu models for a variety of diseases. In a systematic review, Gupta and colleagues24 evaluated the effectiveness of European quick diagnosis units for the diagnostic evaluation of patients with potentially severe disease. The investigators showed that such units are cost-effective and that they lower the number of inpatient hospitalizations. However, none of the studies included in their systematic review were specific to suspicious breast lesions or compared two outpatient programs head-to-head (that is, an outpatient rdu vs. an outpatient non-rdu).
One of the limitations to the utility of our paper is that it does not measure cost against an effectiveness outcome. Such an evaluation was neither the intent nor the vision of our bia. However, even a cost-effectiveness study would not be able to capture all the indirect costs and benefits of a rdu. For instance, decreasing patient wait time to diagnosis leads to less patient anxiety and increased patient access to support services, both of which are challenging to quantify economically6,10,25. Thus, to truly determine whether incremental costs lead to improved patient-centred outcomes or even possibly long-term savings, a cost-effectiveness analysis examining implementation of a rdu, if desired, has to be assessed from the societal perspective.
Another limitation of our bia pertains to its external validity. Our costing data are most relevant for an institution with a similar practice model (tertiary referral centre in a universal health care system). However, given that the funding of health care and the delivery of health services are highly variable, and that clinical decision-making and testing can also be variable between institutions, the purpose of our bia is not to give a single cost estimate. Rather, using transparent and well-documented assumptions, the goal is to provide an economic analysis that reflects our institutional experience and that can be extrapolated for the use of others as applicable. Thus, we did not perform a micro-costing analysis.
Lastly, an ostensive limitation of our study might be that we did not include the capital costs of ultrasonography or digital mammography machines, or the purchase or rental cost of the physical space in which the rdu resides. Additionally, the costs of creating and maintaining a patient-tracking database for research or quality control were not included. Our objective was primarily to determine the cost of implementing a change to a current or pre-existing system in which diagnostic infrastructure is already in place. Our reported initiation costs and operational costs therefore take account only of the items that reflect a change in process. However, recognizing that infrastructure costs could be relevant to other institutions, current estimates show that mammography machines are priced at approximately $134,000 (2016 estimate, Canadian dollars) and ultrasonography machines at $250,000, both of which will depreciate over a decade26,27. Based on our own experience, the creation and annual maintenance costs of a prospective patient database are $17,451 and $3702 respectively (Canadian dollars). Maintenance includes personnel costs for data input, daily system backup, maintenance of user account software, and development of custom reports.
CONCLUSIONS
Establishment and maintenance of a breast rdu requires meaningful investment to achieve reductions in time to diagnosis. Future steps will be to measure patient-centred outcomes, including reduction in patient anxiety and possibly shorter times to definitive treatment. The present study can be used as a resource-planning tool for future rdus in health care systems wishing to improve diagnostic efficiency.
ACKNOWLEDGMENTS
This paper was presented as a poster at the Annual Scientific Meeting of the American Society of Breast Surgeons; Dallas, TX, U.S.A.; 13–17 April 2016.
CONFLICT OF INTEREST DISCLOSURES
We have read and understood Current Oncology’s policy on disclosing conflicts of interest, and we declare that we have none.
REFERENCES
- 1.Becker S. A historic and scientific review of breast cancer: the next global healthcare challenge. Int J Gynaecol Obstet. 2015;131(suppl 1):S36–9. doi: 10.1016/j.ijgo.2015.03.015. [DOI] [PubMed] [Google Scholar]
- 2.Toriola AT, Colditz GA. Trends in breast cancer incidence and mortality in the United States: implications for prevention. Breast Cancer Res Treat. 2013;138:665–73. doi: 10.1007/s10549-013-2500-7. [DOI] [PubMed] [Google Scholar]
- 3.El Saghir NS, Anderson BO. Breast cancer early detection and resources: where in the world do we start? Breast. 2012;21:423–5. doi: 10.1016/j.breast.2012.06.007. [DOI] [PubMed] [Google Scholar]
- 4.Hansen RP, Vedsted P, Sokolowski I, Søndergaard J, Olesen F. General practitioner characteristics and delay in cancer diagnosis. a population-based cohort study. BMC Fam Pract. 2011;12:100. doi: 10.1186/1471-2296-12-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jassem J, Ozmen V, Bacanu F, et al. Delays in diagnosis and treatment of breast cancer: a multinational analysis. Eur J Public Health. 2014;24:761–7. doi: 10.1093/eurpub/ckt131. [DOI] [PubMed] [Google Scholar]
- 6.Arnaout A, Smylie J, Seely J, et al. Improving breast diagnostic services with a Rapid Access Diagnostic and Support (rads) program. Ann Surg Oncol. 2013;20:3335–40. doi: 10.1245/s10434-013-3120-5. [DOI] [PubMed] [Google Scholar]
- 7.Emery JD, Shaw K, Williams B, et al. The role of primary care in early detection and follow-up of cancer. Nat Rev Clin Oncol. 2014;11:38–48. doi: 10.1038/nrclinonc.2013.212. [DOI] [PubMed] [Google Scholar]
- 8.Masood S. Rapid assessment breast clinic: how to offer the same day diagnosis? Breast J. 2012;18:101–2. doi: 10.1111/j.1524-4741.2012.01225.x. [DOI] [PubMed] [Google Scholar]
- 9.Reed AD, Williams RJ, Wall PA, Hasselback P. Waiting time for breast cancer treatment in Alberta. Can J Public Health. 2004;95:341–5. doi: 10.1007/BF03405142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Racz JM, Holloway CMB, Huang W, Look Hong N. Improving patient flow and timeliness in the diagnosis and management of breast abnormalities: the impact of a rapid diagnostic unit at a large, tertiary care cancer center. Cur Oncol. 2016;23:260. doi: 10.3747/co.23.3017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sullivan SD, Mauskopf JA, Augustovski F, et al. Budget impact analysis-principles of good practice: report of the ispor 2012 Budget Impact Analysis Good Practice ii Task Force. Value Health. 2014;17:5–14. doi: 10.1016/j.jval.2013.08.2291. [DOI] [PubMed] [Google Scholar]
- 12.Wolff AC, Hammond ME, Hicks DG, et al. on behalf of the American Society of Clinical Oncology and the College of American Pathologists Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline update. J Clin Oncol. 2013;31:3997–4013. doi: 10.1200/JCO.2013.50.9984. [DOI] [PubMed] [Google Scholar]
- 13.Fitzgibbons PL, Murphy DA, Hammond ME, Allred DC, Valenstein PN. Recommendations for validating estrogen and progesterone receptor immunohistochemistry assays. Arch Pathol Lab Med. 2010;134:930–5. doi: 10.5858/134.6.930. [DOI] [PubMed] [Google Scholar]
- 14.Shah CJ, Sullivan JR, Gonyo MB, Wadhwa A, DuBois MS. Practice policy and quality initiatives: using lean principles to improve screening mammography workflow. Radiographics. 2013;33:1505–17. doi: 10.1148/rg.335135017. [DOI] [PubMed] [Google Scholar]
- 15.D’Andreamatteo A, Ianni L, Lega F, Sargiacomo M. Lean in healthcare: a comprehensive review. Health Policy. 2015;119:1197–209. doi: 10.1016/j.healthpol.2015.02.002. [DOI] [PubMed] [Google Scholar]
- 16.Hwang P, Hwang D, Hong P. Lean practices for quality results: a case illustration. Int J Health Care Qual Assur. 2014;27:729–41. doi: 10.1108/IJHCQA-03-2014-0024. [DOI] [PubMed] [Google Scholar]
- 17.Kruskal JB, Reedy A, Pascal L, Rosen MP, Boiselle PM. Quality initiatives: lean approach to improving performance and efficiency in a radiology department. Radiographics. 2012;32:573–87. doi: 10.1148/rg.322115128. [DOI] [PubMed] [Google Scholar]
- 18.Ontario Health Insurance Plan (ohip) Schedule of Benefits and Fees. Toronto, ON: OHIP; 2015. [Google Scholar]
- 19.Statistics Canada . Consumer Price Index. Ottawa, ON: Statistics Canada; CANSIM Table 326-0021. Catalogue nos. 62-001-X and 62-010-X. n.d. [Current version available online at: http://www5.statcan.gc.ca/cansim/a26?id=3260021; cited 1 May 2017] [Google Scholar]
- 20.Hoffman HJ, LaVerda NL, Young HA, et al. Patient navigation significantly reduces delays in breast cancer diagnosis in the District of Columbia. Cancer Epidemiol Biomarkers Prev. 2012;21:1655–63. doi: 10.1158/1055-9965.EPI-12-0479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Baliski C, McGahan CE, Liberto CM, et al. Influence of nurse navigation on wait times for breast cancer care in a Canadian regional cancer center. Am J Surg. 2014;207:686–91. doi: 10.1016/j.amjsurg.2014.01.002. [DOI] [PubMed] [Google Scholar]
- 22.Brouwers M, Oliver TK, Crawford J, et al. Cancer diagnostic assessment programs: standards for the organization of care in Ontario. Curr Oncol. 2009;16:29–41. doi: 10.3747/co.v16i6.400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gilbert JE, Dobrow MJ, Kaan M, et al. Creation of a diagnostic wait times measurement framework based on evidence and consensus. J Oncol Pract. 2014;10:e373–9. doi: 10.1200/JOP.2013.001320. [DOI] [PubMed] [Google Scholar]
- 24.Gupta S, Sukhal S, Agarwal R, Das K. Quick diagnosis units—an effective alternative to hospitalization for diagnostic workup: a systematic review. J Hosp Med. 2014;9:54–9. doi: 10.1002/jhm.2129. [DOI] [PubMed] [Google Scholar]
- 25.Lefresne S, Berthelet E, Cashman R, et al. The Vancouver rapid access clinic for palliative lung radiation, providing more than just rapid access. Support Care Cancer. 2015;23:125–32. doi: 10.1007/s00520-014-2345-6. [DOI] [PubMed] [Google Scholar]
- 26.Hiatt MD, Carr JJ, Manning RL. The length of time necessary to break even after converting to digital mammography. J Telemed Telecare. 2000;6:222–4. doi: 10.1258/1357633001935392. [DOI] [PubMed] [Google Scholar]
- 27.Health Quality Ontario Ultrasound as an adjunct to mammography for breast cancer screening: a health technology assessment. Ont Health Technol Assess Ser. 2016;16:1–71. [PMC free article] [PubMed] [Google Scholar]