Abstract
Objective: The objective of the study is to examine the Champlain. BASETM (Building Access to Specialists through eConsultation) eConsult service’s impact on access to care for older persons. Methods: We conducted a cross-sectional analysis of all eConsult cases submitted between April 15, 2011, and July 31, 2015, in which the patient was above the age of 65 years. Study data consisted of utilization data collected automatically by the service and responses to surveys completed by primary care providers at the conclusion of all eConsult cases. Results: A total of 1,796 cases were submitted for older persons between April 15, 2011, and July 31, 2015, accounting for 21.3% of all cases submitted during the study period. Specialists responded to cases in a median of 0.8 days. In 94% of cases, providers rated eConsult as having great or excellent value for themselves and their patients. Sixty-eight percent of eConsults did not require a face-to-face visit; only 28% of all cases resulted in a referral. Discussion: As they suffer from higher than average rates of comorbid disease and mobility issues, older persons stand to benefit from shorter wait times and better access to care, which the eConsult service can provide.
Keywords: access to care, health services research, primary care, electronic consultation, elderly
Introduction
Limited access to specialist care is a major barrier to health care. Recently, the Commonwealth Fund found that 41% of Canadian patients waited for more than 2 months for their specialist appointment (Schoen & Osborn, 2010). In the United States, 39% of individuals with below average incomes reported cost related access problems, the highest proportion among all countries surveyed (Schoen & Osborn, 2010).
Although excessive wait times are a concern for patients of all ages, older individuals face particular challenges in accessing specialist care. Older persons are often frail and frequently struggle with mobility issues, raising further barriers to their ability to access timely specialist care (Grant et al., 2011). They are also more likely than younger patients to have multiple chronic conditions (Schoen, Osborn, How, Doty, & Peugh, 2009), resulting in more frequent use of health services and greater costs for the health care system (Lehnert et al., 2011). Among patients in the United States with multiple chronic conditions, 60.4% of older patients reported they needed to see a specialist in the last year regarding their care (Soni, 2015). In addition, many older persons experience conditions such as chronic pain that require multiple medications, resulting in frequent appointments and challenges in safely reducing dosages or curtailing the use of medications that are no longer needed (Ramage-Morin, 2008). Reduced access to specialist care exacerbates these issues, leading to poor health outcomes, low levels of satisfaction, and increased mortality (Canadian Institute for Health Information, 2012; Day, 2013).
Electronic consultation (eConsult) allows primary care providers (PCPs) to communicate asynchronously with specialists. In many cases, these services can allow PCPs to treat patients without referring them for a face-to-face specialist visit (Kim-Hwang et al., 2010; Liddy, Rowan, Afkham, Maranger, & Keely, 2013; Stoves et al., 2010). A number of studies have demonstrated the ability of eConsult services to reduce wait times for patients, foster improved communication between PCPs and specialists, and provide better access to specialist care (Callahan, Malone, Estroff, & Person, 2005; Straus, Chen, Yee, Kushel, & Bell, 2011; Wootton, Menzies, & Ferguson, 2009).
One such program, called the Champlain BASE™ (Building Access to Specialists through eConsultation) eConsult service, was launched as a proof-of-concept in Ottawa, Ontario in 2010 (Liddy et al., 2013). The service has now enrolled 1,040 PCPs as users (879 of whom are family doctors and 160 nurse practitioners) and provides access to 86 specialty groups, the largest menu of specialties available from such services worldwide. The eConsult service has had a substantial impact on wait times, and has been received positively by PCPs and specialists alike (Keely, Drosinis, Afkham, & Liddy, 2015; Keely, Liddy, & Afkham, 2013; Liddy, Afkham, Drosinis, Joschko, & Keely, 2015).
Little work has been done to understand the impact of eConsult services for older persons. Studies of real-time telemedicine services have shown high satisfaction among patients and providers when used for treating dementia (Azad, Amos, Milne, & Power, 2012), and such systems have been identified as an economically feasible approach to provide geriatric care to patients in rural areas (Versleijen, Martin-Khan, Whitty, Smith, & Gray, 2015). However, eConsult systems differ from real-time platforms as the communication between providers happens asynchronously, thus limiting comparability between the two delivery models. To our knowledge, no work has been done to understand the impact of eConsult services for older persons.
We have collected utilization data from the eConsult service over the past 5 years, providing a unique opportunity to explore the service’s impact on older persons. The objectives of this study are to better understand the impact of eConsult on (a) access to specialist care, (b) value of the service to patients and providers, and (c) the ability of eConsult to deliver efficient care.
As more eConsult systems continue to be implemented, the findings of the study will be useful in further understanding the potential benefits of eConsult specifically for older persons.
Method
Design
Our study consisted of a cross-sectional analysis of all eConsult cases that PCPs submitted on behalf of patients above the age of 65 years.
Setting
The Champlain Local Health Integration Network (LHIN) is a regional health district located in eastern Ontario, Canada. More than 16,000 km2 in size, the region has a population of 1.2 million (Champlain LHIN, 2014). Approximately half of the Champlain LHIN’s residents live in the city of Ottawa, with the other half residing in the surrounding towns and rural areas. As the region’s urban center, Ottawa houses the majority of specialists practicing in the Champlain LHIN. Individuals residing outside of the city who require specialist consultations may have to travel as much as 2 hr by car to attend face-to-face appointments.
Participants
All PCPs practicing in the Champlain LHIN are eligible to sign up for the eConsult service. In addition, select groups of PCPs from outside our health region are able to access the service through ongoing research projects. The Champlain BASE™ team used provider engagement strategies to recruit initial users. Once the service became more established, PCPs began seeking out opportunities to join the service. Consequently, subsequent recruitment of PCPs has been driven primarily by self-selection.
For this study, we analyzed only those eConsults submitted by PCPs between April 15, 2011, and July 31, 2015 for patients above the age of 65 years. Participants included PCPs working in community practices and long-term care facilities.
The eConsult Service
The eConsult service’s secure web-based platform allows PCPs to submit questions on patients’ care to one of 86 specialty groups. Questions are entered into an online form that allows for the attachment of additional files such as digital images, test results, or health histories. Once the question is submitted, a designated case assigner receives an e-mail letting them know a case is waiting to be assigned. The case is then assigned to a specialist based either on their availability or by a rotation schedule. The specialist receives an e-mail notifying them they have an eConsult pending their review and prompts the specialist to log-into the eConsult site to reply to the case. Replies are expected to be sent within 1 week, and specialists have the option to (a) provide advice regarding the patient’s treatment, (b) request additional information on the case before providing a response, or (c) a recommend a face-to-face referral. Specialists are paid CDN$200/hr for answering eConsults, prorated to their self-reported time to complete the eConsult.
Data Collection and Analysis
For each case completed by the eConsult service, the system collects a variety of usage data, including the number of eConsults the PCP has previously submitted, the specialty group referred to, response time, and outcome of the case. The service also maintains a complete log of all exchanges between providers, which the PCP and specialist can access. We ascertained rurality of the PCP by using their practices’ postal code and the Ontario Medical Association’s Rurality Index of Ontario score (Kralj, 2005).
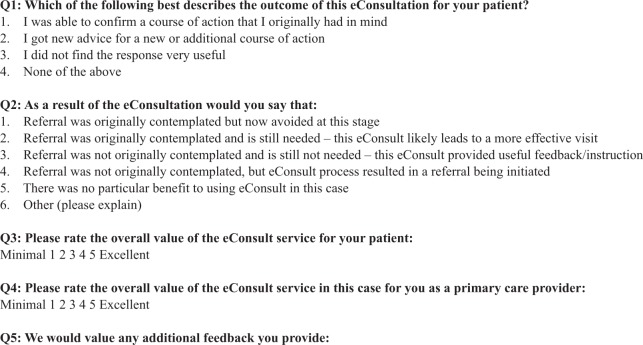
Additional data for our study were drawn from a mandatory survey that PCPs complete at the conclusion of each eConsult case (Figure 1). The survey contains five questions. For Question 1, PCPs select a response that best describes the outcome of the eConsult. The four options are as follows: (a) The specialist confirmed the PCP’s originally chosen course of action, (b) the specialist recommended a new/additional course of action, (c) the response was not very useful, or (d) none of the above. For Question 2, PCPs choose from a number of set responses identifying whether or not they (a) had originally contemplated a referral, and (b) ultimately chose to refer the patient based on the specialist’s advice. For the purposes of this study, we were interested in whether each eConsult resulted in the patient not having to attend a face-to-face specialist visit. We therefore coded the responses into a three-level categorical variable as “referral not needed,” “referral needed,” and “other,” with the latter category including any cases where the PCP did not indicate whether or not a referral was needed. For Question 3, PCPs use a 5-point Likert-type scale to rank the value of the eConsult for their patients, with one being minimal and five excellent. For Question 4, PCPs use the same scale to rank the value of the eConsult service for themselves. For Question 5, PCPs are given an optional open-text field where they may provide any additional feedback.
Figure 1.
Close-out survey administered upon completion of each eConsult.
Responses to Question 2 of the closeout survey were calculated separately for each specialty group, to identify which specialties showed the highest proportion of a referral not needed. We calculated median and interquartile ranges (IQRs) for response times for all eConsult cases included in the study. For all other outcomes, we tabulated counts and averages, as appropriate. Responses to question five contained only open-text data, and are not included in this study.
Results
A total of 338 PCPs (including 295 family doctors and 43 nurse practitioners) submitted 1,796 cases for patients above 65 years of age between April 15, 2011, and July 31, 2015. This amounted to 21.3% of all eConsults submitted during the study period. Cases were directed to 70 specialists practicing in 41 specialty groups. Patients included in the sample had an average age of 76 years (SD = 7.7), and the majority of patients were female (62%) and treated by family doctors (92%). In 14.4% (n = 259) of cases, eConsults were submitted by PCPs who practice in a rural area (Table 1).
Table 1.
Provider, Utilization, and Patient Characteristics for eConsults Submitted for Older Persons, All Other Patients, and All eConsults Completed Between April 15, 2011, and July 31, 2015.
| Patients aged 65+ (n = 1,796) | Patients under the age of 65 (n = 6,649) | All patients (n = 8,445) | |
|---|---|---|---|
| Provider and utilization characteristics | |||
| Provider type | |||
| Family doctor | 91.7% | 86.3% | 87.5% |
| Nurse practitioner | 8.3% | 13.7% | 12.5% |
| Practice location | |||
| Urban | 85.6% | 87.4% | 87% |
| Rural | 14.4% | 12.6% | 13% |
| Specialist time to complete | |||
| Fewer than 10 min | 51.6% | 52.0% | 51.9% |
| 10-15 min | 30.5% | 30.9% | 30.8% |
| 15-20 min | 14.1% | 13.6% | 13.7% |
| 20+ min | 3.8% | 3.5% | 3.6% |
| Patient characteristics | |||
| Gender | |||
| Male | 38.2% | 37.7% | 37.8% |
| Female | 61.8% | 62.3% | 62.2% |
Response Time and Specialty Group
The median time between PCPs sending a question and receiving an initial specialist response was 0.8 days (IQR: 0.16-3.1). In more than half of all cases, specialists reported taking fewer than 10 min to complete their response. Only 4% of cases took specialists more than 20 min to complete (Table 1). The most popular specialty groups for eConsult for older persons were dermatology (14%), cardiology (11%), endocrinology (10%), hematology (10%), and neurology (7%).
Survey Responses
In response to Question 1, 38% of eConsult cases confirmed the PCP’s course of action, whereas 59% of cases provided PCPs with a new or additional course of action.
In response to Question 2, 68% of all eConsults did not require a face-to-face specialist visit; only 28% of all cases resulted in a referral (Table 2). The percentage of cases that resulted in a referral varied between specialty groups. Nineteen specialty groups received more than 20 eConsults during the study period. Within these specialty groups, the proportion of eConsults that did not require a face-to-face visit varied from 37% (respirology) to 89% (thrombosis).
Table 2.
The Impact of eConsult on the Need for a Face-to-Face Referral Needed for Patients Over the Age of 65, Reported Across Specialty Groups.
| Specialty | Referral not needed | Referral needed | Othera |
|---|---|---|---|
| Respirology (n = 27) | 37% | 59% | 4% |
| Urology (n = 81) | 51% | 48% | 1% |
| Pain medicine (n = 38) | 53% | 39% | 8% |
| Neurology (n = 124) | 57% | 37% | 6% |
| Hematology (n = 178) | 59% | 37% | 4% |
| Radiology (n = 42) | 60% | 40% | 0% |
| Orthopedics (n = 57) | 63% | 30% | 7% |
| Rheumatology (n = 111) | 65% | 32% | 4% |
| Psychiatry (n = 24) | 67% | 29% | 4% |
| Gastroenterology (n = 56) | 68% | 29% | 4% |
| Average (n = 1,796) | 68% | 28% | 4% |
| Infectious diseases (n = 66) | 70% | 26% | 5% |
| ENT (n = 21) | 71% | 29% | 0% |
| Dermatology (n = 256) | 71% | 23% | 5% |
| Cardiology (n = 209) | 74% | 22% | 3% |
| Internal medicine (n = 82) | 74% | 21% | 5% |
| Nephrology (n = 84) | 76% | 20% | 4% |
| OBS/GYN (n = 49) | 78% | 18% | 4% |
| Endocrinology (n = 178) | 80% | 19% | 2% |
| Thrombosis (n = 46) | 89% | 11% | 0% |
Note. ENT = ear, nose, and throat; OBS/GYN = obstetrics and gynecology.
Other refers to responses in which the primary care provider did not indicate whether or not a referral was needed in their closeout survey.
For Question 3, 94% of PCPs rated the value of the eConsult to their patients as four (18%) or five (76%) out of five, indicating great and excellent value, respectively.
For Question 4, which used the same scale as above, 94% of PCPs also rated the value of the eConsult for themselves as four (15%) or five (79%) out of five. The average rating across all included cases was 4.7 out of five for both patients and providers.
Long-Term Care
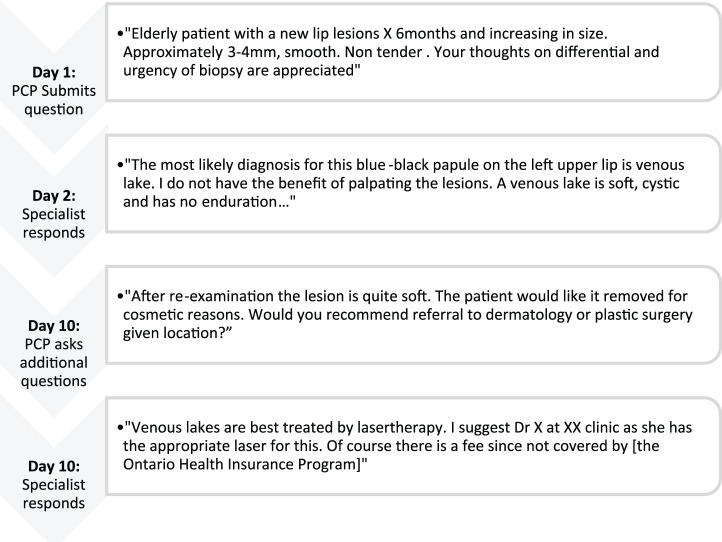
Among the 338 PCPs who submitted eConsults during the study period, four practice in long-term care homes. These four PCPs submitted a total of 23 eConsults during the study period, with the most popular specialty groups being dermatology (n = 11) and infectious diseases (n = 4). The remaining eConsults were directed to internal medicine (n = 2), gastroenterology (n = 1), hematology (n = 1), neurology (n = 1), radiology (n = 1), orthopedics (n = 1), and palliative care (n = 1). The appendix illustrates an example case submitted through the eConsult service for an older person.
Discussion
The implementation of the Champlain BASE™ eConsult service has greatly improved timely access to specialist care for the aging population in our health region. We have shown that there is high value to the service from the patient and provider perspective in terms of access to care, greater efficiency of care delivery, integrated care, education, and capacity building.
Few studies have examined the specialist referral patterns of older adults. Shadd et al. calculated specialist referral rates from an electronic health record and reported the highest referral rates for general surgery (61 referrals per 1,000 patients per year), obstetrics/gynecology (41/1,000), orthopedic surgery (41/1,000), dermatology (35/1,000), and otolaryngology (33/1,000) (2011). Although the authors did not report patterns of referral specifically for older persons, referral rates were found to increase with patient age (Shadd, Ryan, Maddocks, & Thind, 2011). Other studies have also found that referral rates increase with patient age (Chan & Austin, 2003; Sullivan, Omar, Ambler, & Majeed, 2005).
Although not specifically designed for older persons, eConsult is particularly beneficial to this patient population due to its ability to reduce unnecessary referrals. Older persons suffer disproportionately from multiple chronic conditions; while only 13% of patients between the ages of 20 and 39 years reported having at least one chronic condition, this jumps to 71% for patients between 60 and 79 years (Broemeling, Watson, & Prebtani, 2007). Furthermore, a growing percentage of older patients suffer from Alzheimer’s disease and other dementias, complex health issues, and physical frailty (Canadian Institute for Health Information, 2009, 2013). As a result of these issues, older patients often face significant challenges to attend a specialist appointment. Many will require some assistance to get to the appointment, whether from a family member or a caregiver, who may need to take time off work or school. Patients and their caregivers often have to travel some distance to attend the appointment, an issue of particular concern for patients living in rural areas. In addition, time constraints and poor weather conditions can complicate patients’ ability to attend specialist appointments. Finally, those living on a fixed income may face a greater impact of out of pocket expenses including parking, gas, and meal costs. When considering these factors, avoiding even just one referral can have a significant positive impact on patients.
One sector that may stand to benefit from eConsult is residential long-term care homes. In the province of Ontario, approximately one in four individuals will reside in a long-term care home during their last year of life. Since 2008, long-term care residents have shown an increased prevalence of heart/circulation diseases (an 8.9% increase from 2008/2009 to 2013/2014), hypertension (12.3%), dementias including Alzheimer’s (5.7%), arthritis (8.7%), and psychiatric/mood diseases (5.8%), with 93% of residents having two or more chronic diseases (Canadian Institute for Health Information, 2009, 2013). The staff at long-term care facilities often lack the clinical skills and medical technology required to support these complex conditions on-site, necessitating burdensome and costly referrals and transfers (Ontario Long-Term Care Association, 2014). The eConsult service is well positioned to reduce this burden by allowing long-term care clinicians to eliminate a number of unnecessary referrals, thereby improving access to care. Subsequent research may explore the implementation of the eConsult service in long-term care and evaluate the service’s impact on residents’ health outcomes.
Limitations
We did not have access to data on the total number of referrals for patients above 65 years of age in our health region. Consequently, our analysis does not examine the eConsult service’s impact on a population level. In addition, no patient identification information is collected through the service. This prevented us from characterizing patients by the presence of chronic conditions or medical history.
Conclusion
The eConsult service resulted in quicker access to specialist care for older persons. Cases submitted using the service received replies in a median time of 0.8 days. The rate of eConsults not requiring a face-to-face visit ranged from 37% to 89% of cases depending on specialty type, and providers expressed nearly universal satisfaction with the service. With high frequencies of multimorbidities and mobility issues, older persons stand to benefit from shorter wait times and better access to care, which the eConsult service is well positioned to provide.
Acknowledgments
The authors wish to thank the primary care providers (PCPs) and specialists who participated in the service, and the Winchester District Memorial Hospital for hosting the servers and providing technical support.
Appendix
Example case submitted to dermatology from a PCP through eConsult.
Note. PCP = primary care provider.
Footnotes
Authors’ Note: This study was approved by the Ottawa Health Science Network Research Ethics Board (Protocol 2009848-01H).
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Ministry of Health and Long-Term Care, The Ottawa Hospital Academic Medical Organization Innovation Fund, e-Health Ontario, and the Champlain Local Health Integration Network.
References
- Azad N., Amos S., Milne K., Power B. (2012). Telemedicine in a rural memory disorder clinic—Remote management of patients with dementia. Canadian Geriatrics Journal, 15, 96-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broemeling A. M., Watson D. E., Prebtani F. (2007). Population patterns of chronic health conditions, co-morbidity and healthcare use in Canada: Implications for policy and practice. Healthcare Quarterly, 11, 70-76. [DOI] [PubMed] [Google Scholar]
- Callahan C. W., Malone F., Estroff D., Person D. A. (2005). Effectiveness of an Internet-based store-and-forward telemedicine system for pediatric subspecialty consultation. Archives of Pediatrics & Adolescent Medicine, 159, 389-393. [DOI] [PubMed] [Google Scholar]
- Canadian Institute for Health Information. (2009). CCRS continuing care reporting system: Profile of residents in continuing care facilities 2008-2009. Retrieved from http://www.cihi.ca/CIHI-ext-portal/internet/EN/Quick_Stats/quick+stats/quick_stats_main?xTopic=Community%20Care&;pageNumber=1&resultCount=10
- Canadian Institute for Health Information. (2012). Health care in Canada, 2012: A focus on wait times. Retrieved from https://secure.cihi.ca/free_products/HCIC2012-FullReport-ENweb.pdf
- Canadian Institute for Health Information. (2013). CCRS continuing care reporting system: Profile of residents in continuing care facilities 2012-2013. Retrieved from http://www.cihi.ca/CIHI-ext-portal/internet/EN/Quick_Stats/quick+stats/quick_stats_main?xTopic=Community%20Care&;pageNumber=1&resultCount=10
- Champlain LHIN. (2014). Population characteristics for Champlain health link areas. Retrieved from http://www.champlainlhin.on.ca/~/media/sites/champlain/Accountability/Integration/HL%20Docs/201410ChHLAsPopCharEN.pdf?la=en
- Chan B. T., Austin P. C. (2003). Patient, physician, and community factors affecting referrals to specialists in Ontario, Canada: A population-based, multi-level modelling approach. Medical Care, 41, 500-511. [DOI] [PubMed] [Google Scholar]
- Day B. (2013). The consequences of waiting. In Globerman S. (Ed.), Reducing wait times for health care: What Canada can learn from theory and international experience (pp. 45-76). Vancouver, British Columbia, Canada: Fraser Institute. [Google Scholar]
- Grant R. W., Ashburner J. M., Hong C. S., Chang Y., Barry M. J., Atlas S. J. (2011). Defining patient complexity from the primary care physician’s perspective: A Cohort study. Annals of Internal Medicine, 155, 797-804. [DOI] [PubMed] [Google Scholar]
- Keely E., Drosinis P., Afkham A., Liddy C. (2015). Perspectives of Champlain BASE specialist physicians: Their motivation, experiences and recommendations for providing eConsultations to primary care providers. Studies in Health Technology and Informatics, 209, 38-45. [PubMed] [Google Scholar]
- Keely E., Liddy C., Afkham A. (2013). Utilization, benefits, and impact of an e-Consultation service across diverse specialties and primary care providers. Telemedicine Journal and e-Health, 19, 733-738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim-Hwang J. E., Chen A. H., Bell D. S., Guzman D., Yee H. F., Jr., Kushel M. B. (2010). Evaluating electronic referrals for specialty care at a public hospital. Journal of General Internal Medicine, 25, 1123-1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kralj B. (2005). Measuring “rurality” for purposes of health care planning: An empirical measure for Ontario. Retrieved from https://www.oma.org/Resources/Documents/2008RIO-FullTechnicalPaper.pdf
- Lehnert T., Heider D., Leicht H., Heinrich S., Corrieri S., Luppa M., . . . König H. H. (2011). Review: Health care utilization and costs of elderly persons with multiple chronic conditions. Medical Care Research and Review, 68, 387-420. [DOI] [PubMed] [Google Scholar]
- Liddy C., Afkham A., Drosinis P., Joschko J., Keely E. (2015). Impact and satisfaction with a new eConsult service: A mixed methods study of primary care providers. Journal of the American Board of Family Medicine, 28, 394-403. [DOI] [PubMed] [Google Scholar]
- Liddy C., Rowan M. S., Afkham A., Maranger J., Keely E. (2013). Building access to specialist care through e-consultation. Open Medicine, 7, e1-e8. [PMC free article] [PubMed] [Google Scholar]
- Ontario Long-Term Care Association. (2014). This is Long-Term Care 2014. Markham, Ontario, Canada: Author. [Google Scholar]
- Ramage-Morin P. L. (2008). Chronic pain in Canadian seniors. Ottawa, Ontario: Health Reports, Statistics Canada. [PubMed] [Google Scholar]
- Schoen C., Osborn R. (2010). The commonwealth fund 2010 international health policy survey in eleven countries. Retrieved from http://www.commonwealthfund.org/~/media/files/publications/chartbook/2010/pdf_2010_ihp_survey_chartpack_full_12022010.pdf
- Schoen C., Osborn R., How S. K., Doty M. M., Peugh J. (2009). In chronic condition: Experiences of patients with complex health care needs, in eight countries, 2008. Health Affairs, 28, w1-w16. [DOI] [PubMed] [Google Scholar]
- Shadd J., Ryan B. L., Maddocks H., Thind A. (2011). Patterns of referral in a Canadian primary care Electronic health record database: Retrospective cross-sectional analysis. Informatics in Primary Care, 19, 217-223. [DOI] [PubMed] [Google Scholar]
- Soni A. (2015). Specialist need and access among adults with multiple chronic conditions, U.S. civilian noninstitutionalized population, 2012 (Statistical Brief No. 482). Rockville, MD: Agency for Healthcare Research and Quality. [PubMed] [Google Scholar]
- Stoves J., Connolly J., Cheung C. K., Grange A., Rhodes P., O’Donoghue D., Wright J. (2010). Electronic consultation as an alternative to hospital referral for patients with chronic kidney disease: A novel application for networked electronic health records to improve the accessibility and efficiency of healthcare. Quality & Safety in Health Care, 19, Article e54. [DOI] [PubMed] [Google Scholar]
- Straus S. G., Chen A. H., Yee H., Jr., Kushel M. B., Bell D. S. (2011). Implementation of an electronic referral system for outpatient specialty care. AMIA Annual Symposeum Proceedings, 2011, 1337-1346. [PMC free article] [PubMed] [Google Scholar]
- Sullivan C. O., Omar R. Z., Ambler G., Majeed A. (2005). Case-mix and variation in specialist referrals in general practice. British Journal of General Practice, 55, 529-533. [PMC free article] [PubMed] [Google Scholar]
- Versleijen M., Martin-Khan M. G., Whitty J. A., Smith A. C., Gray L. C. (2015). A telegeriatric service in a small rural hospital: A case study and cost analysis. Journal of Telemedicine and Telecare, 21, 459-468. [DOI] [PubMed] [Google Scholar]
- Wootton R., Menzies J., Ferguson P. (2009). Follow-up data for patients managed by store and forward telemedicine in developing countries. Journal of Telemedicine and Telecare, 15, 83-88. [DOI] [PubMed] [Google Scholar]