Abstract
Purpose
Breast cancer-related lymphedema (BCRL) is a debilitating condition. The recommended treatment is based on decongestive lymphedema therapy (DLT) with two separate phases: a short-term intensive phase to reduce lymphedema volume and a long-term maintenance phase to stabilize it. Optimizing compression therapy and compliance during maintenance phase are key factors for long-term control of lymphedema. The primary objective of this pilot prospective open-label randomized study was to assess the benefit of a new auto-adjustable nighttime arm sleeve (MOBIDERM® Autofit) on lymphedema volume during the maintenance phase after the intensive phase.
Methods
Forty women with BRCL were consecutively enrolled and randomized (D0) for 1 month in 1:1 ratio either in night-use group: with MOBIDERM® Autofit (on top of a daytime compression hosiery), or in no night-use group: without MOBIDERM® Autofit (daytime hosiery alone). From Day 31 to Day 90, all patients were fitted with MOBIDERM® Autofit. Primary endpoint was lymphedema volume variation between Day 0 and Day 30. Secondary endpoints were compliance, quality of life (LYMQOL arm questionnaire), functional symptoms (heaviness, limb use limitation, pain), sleep quality, and safety.
Results
In ITT population, between Day 0 and Day 30, mean lymphedema volume increase was higher in no night-use group with 92.9 mL (i.e., 3.2%) than in night-use group with 46.7 mL (i.e., 1.80%), p = 0.757. Between Day 30 and Day 90, all patients fitted with MOBIDERM® Autofit, lymphedema volume remained stable in both groups. The device improved functional symptoms and function domain of the LYMQOL arm questionnaire. MOBIDERM® Autofit was worn overnight almost 85% of the nights. It was well accepted by the patients and no adverse reaction leading to permanent device discontinuation occurred.
Conclusions
Our results suggest that MOBIDERM® Autofit offers clinical benefits during maintenance phase of lymphedema treatment and enhances patient’s self-management.
Keywords: Self-management, Lymphedema, Breast cancer, Volume, Compression, Maintenance
Introduction
Breast cancer-related lymphedema (BCRL) is a common and debilitating complication [1–3]. Despite modern treatment modalities, it remains a major health problem. As edema progress, the disease can lead to pain, infection, decreased function, reduced quality of life, body image disturbance and anxiety [4, 5].
The recommended treatment of lymphedema is based on a decongestive lymphedema therapy (DLT) which is composed of 2 phases: an intensive phase which combines manual lymphatic drainage (MLD), multilayer bandages, skin cares, and physical exercises, to reduce as much as possible lymphedema volume in a few days period of time and a maintenance phase which consists in helping the patient to preserve lymphedema volume achieved during intensive phase, as long as possible [6, 7]. In spite of self-care management, it is common to observe an increase of lymphedema volume after intensive phase also called “maintenance phase failure”. There is no existing consensus on the definition of treatment failure in lymphedema, but in the long-term trial of Vignes et al. [8], the stringent definition of treatment failure, i.e., a lymphedema volume increase of ≥50% of the total reduction obtained with the first intensive decongestive physiotherapy, was selected to estimate a prolonged benefit. With this end-point criterion, the risk of failure was estimated to 38.1, 53.1, and 64.8% after 1, 2, and 4 years, respectively. In the POLIT study [9], the first large observational study measuring the effects of DLT in 12 French lymphology reference centers, Quéré et al. [9] showed that even if intensive phase permitted to reduce lymphedema volume by 30%, the effect was partially reversed 6 months later. Therefore, optimizing maintenance phase treatment seems to be crucial for long term management of lymphedema.
Compression is largely described as the key component in the treatment of lymphedema in the updated best practice guidelines of International Lymphedema Framework (ILF) [10]. In France, the Haute Autorité de Santé (HAS) recommends to use high-pressure compression garments (up to 15 mmHg with the need to apply the higher pressure tolerated by patient) during the day and if needed, low stretched bandages during the night without any pressure specifications [11]. More recently, Damstra and Partsch [12] showed that applying too much pressure under low-stretch bandages may be counterproductive and recommends levels of 20–30 mmHg for the upper limb. Self-management and patient compliance to treatment are crucial in the maintenance phase. Among the 306 patients observed in POLIT study [8], maintenance therapy was applied in most patients by means of daytime hosiery (95.8%) and/or bandages (12.3%) meaning some patients used both day devices. At night, 21.1% of the patients did not use any night compression therapy. Among the rest, 45.2% of the patients reported night compression therapy using bandaging and 46% with made to measure hosieries.
In practice, during maintenance phase, the bandages are not easy to put on and require assistance and/or specific patient’s education. Composed of several layers of inelastic and short-stretch materials, these bulky bandages do not favor patient’s compliance and quality of life. Custom made short-stretch arm sleeve, designed to apply a low rest pressure, are easier to put on but can be quickly unsuitable if patient’s measurements vary over time. The challenge is to provide BCRL patients with an easy to use, safe and effective low-stretch night device as an add-on treatment to their daytime compression hosiery in order to optimize their maintenance treatment and increase their autonomy and compliance.
This study was conducted to assess the interest of nighttime MOBIDERM® Autofit arm sleeve on lymphedema volume during maintenance phase in patients with BCRL.
Patients and methods
Patient’s selection
This pilot prospective open-label randomized controlled trial had been conducted between September 2014 and February 2015 in the vascular medicine ward of the Saint-Eloi Hospital, Montpellier, France. Forty women were consecutively screened and included. Eligible patients were women aged ≥18 years, with unilateral secondary upper limb lymphedema of stage II or III according to the ISL classification, with evident pitting sign (assessed as ++ or +++). Patients had to have undergone an intensive phase treatment with a decrease of lymphedema volume at least of 10% prior to study entry. Exclusion criteria were active cellulitis, lymphedema associated with active cancer requiring chemotherapy, motor and/or sensitive neurological deficiency, postoperative edema (i.e., acute edema occurring in the days following breast cancer-related surgery), active skin lesions on the arm, and pregnant or breastfeeding female.
The study was conducted in accordance with the Declaration of Helsinki and the International Conference on Harmonization Good Clinical Practice Guidelines (ICH-GCP). Prior to study start, the protocol received approval from health authorities and ethics committee. Written informed consent was obtained from each patient prior to study enrolment.
Compression arm modalities
At the end of the intensive phase of the DLT (D0), patients fulfilling the study entry criteria were randomized in a 1:1 ratio to:
The night-use group (Group I), fitted during the first 30 days with MOBIDERM® Autofit device additionally to their daytime elastic hosiery.
The no night-use group (Group II), fitted only with the day time elastic hosiery.
The daytime elastic hosiery was standardized. It was a circular made to measure knitted garment applying a level of pressure of 15–20 mmHg (French class 2) or 20–36 mmHg (French class 3) on investigator’s demand from THUASNE company (THUASNE Lymphology®).
Then, from Day 31 to Day 90, all patients in both groups used both day and night time devices.
Description of the medical device tested
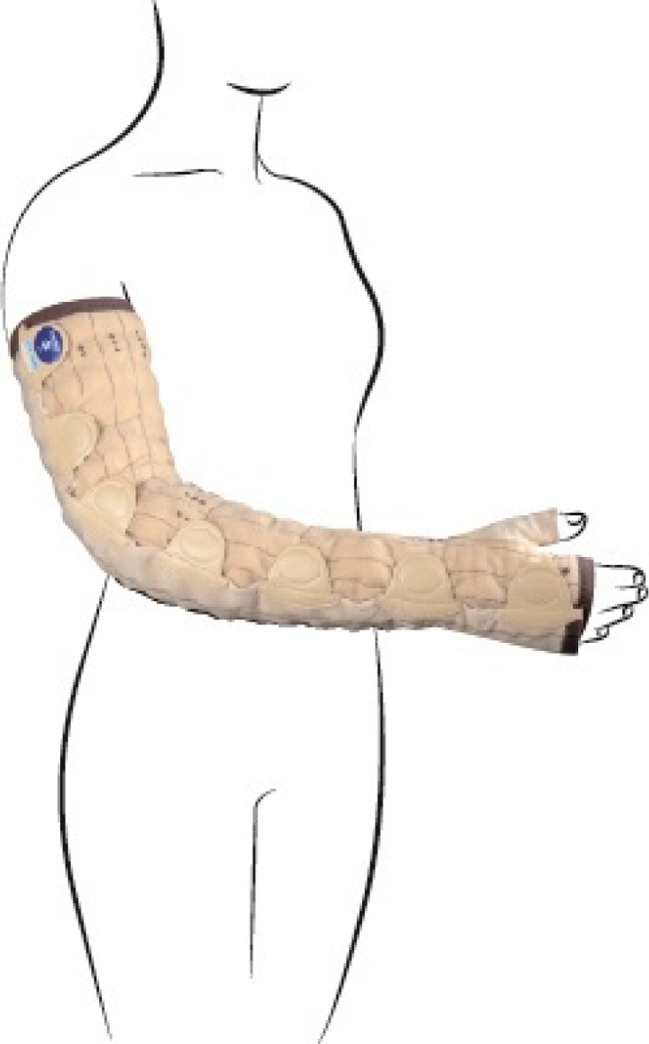
The nighttime MOBIDERM® Autofit was a standard low-stretch garment designed to apply a pressure of 15 mmHg. It is an auto-adjustable semi-open sleeve (Thuasne, Saint-Etienne, FRANCE) available in six sizes, two lengths, left/right arm (Fig. 1) with several semi-rigid straps used to adjust the device to each patient’s morphology or volumes changes. This garment uses the patented MOBIDERM® technology composed of foam blocks in soft adherent webbing. It creates, on and under the skin, zones of differentiated pressure between the foam blocks and their perimeter allowing a local mobilization to facilitate edema fluid evacuation.
Fig. 1.
Auto-adjustable MOBIDERM® Autofit
Statistical analysis
The primary endpoint was the volume excess (also called lymphedema volume) variation, defined as the volumetric difference of the affected limb compared to the contralateral upper limb, between Day 0 and Day 30. Volumes were calculated after taking patients measurements every 5 cm, above (4 measurements) and below (4 measurements) the fold of the elbow (start point) and using the truncated cone formula: H × (C 2 + C × c + c 2)/12π, H = cone height, C = cone top circumference, and c = cone base circumference. This method demonstrated excellent inter- and intra-observer reproducibility in comparison to water displacement, which is considered the gold standard [13, 14].
The comparison of the volume excess variation (mL, %) from Day 0 to Day 30 between the two randomization groups was performed using a bilateral Wilcoxon-Mann-Whitney test on the ITT population. All secondary endpoints and PP analysis were provided only descriptively: functional symptoms at Day 30 and Day 90 vs. baseline, QOL based on LYMQOL ARM questionnaire [15] at each study visits and patient’s satisfaction with self-reported questionnaires, compliance of the treatment evaluated by patient diary between Day 0 and Day 30 and by questioning the patients at D90 regarding the study period between Day 30 and Day 90.
Safety and tolerance data were assessed by numbers and percentages of patients with at least one reported adverse event (AE) tabulated by system organ class and preferred term.
As there is no previous specific published trial on night garment in maintenance phase of lymphedema, sample size calculation was not possible for this a proof of concept study.
Results
Patient disposition and baseline characteristics
Figure 2 displays patient’s disposal in the study. Forty patients were randomized and included in the ITT and safety populations. Five patients were excluded from the per protocol (PP) population for major protocol violation; 3 patients in no night-use Group did not present any decrease of lymphedema volume after DLT, one patient in night-use Group did not wear the daytime hosiery and the nighttime hosiery for at least 75% of time and one patient in no night-use Group applied a night or day different compression device from the allocated one in the study.
Fig. 2.
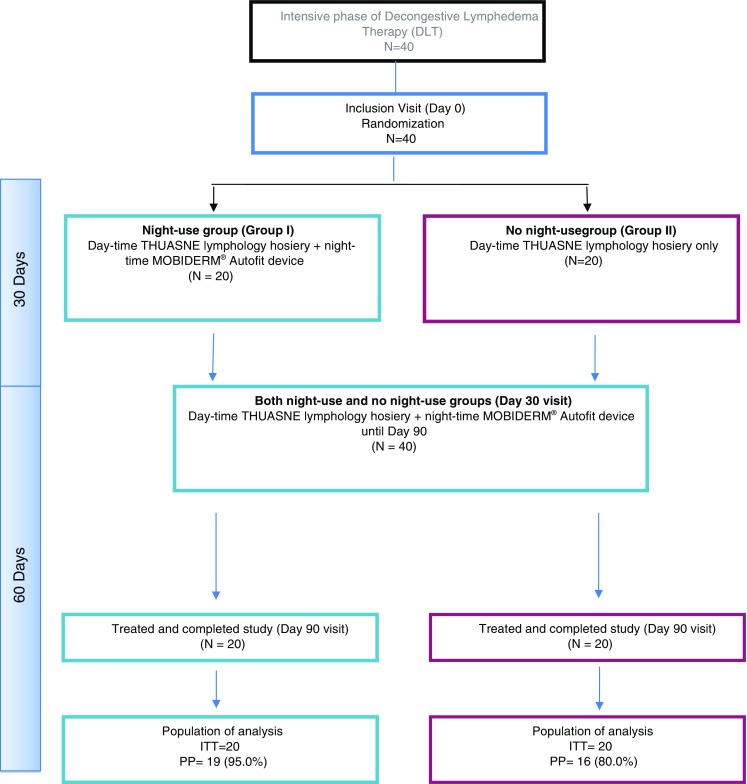
Disposition of patients in the study
Table 1 displays the baseline characteristics of the patients and lymphedema. Overall, the mean age of the ITT population was 67.0 years old [45.3; 89.9] and the mean body mass index (BMI) was 28.5 kg/m2 [19.8; 44.0]. Disease characteristics were well balanced between the two groups. Mean time from diagnosis of lymphedema to inclusion was 8.3 years [0.5; 28.7].
Table 1.
Patient’s demographics and lymphedema characteristics
| Group I (night-use) N = 20 |
Group II (no night-use) N = 20 |
Total N = 40 | ||
|---|---|---|---|---|
| Age at inclusion (years) | N | 20 | 20 | 40 |
| Mean ± SD | 65.11 ± 8.62 | 68.87 ± 11.79 | 66.99 ± 10.37 | |
| Median | 64.47 | 72.01 | 66.31 | |
| Min; max | 50.5; 84.5 | 45.3; 89.9 | 45.3; 89.9 | |
| Body mass index (kg m−2) at day 0[b] | N | 20 | 20 | 40 |
| Mean ± SD | 27.44 ± 4.54 | 29.63 ± 6.53 | 28.53 ± 5.66 | |
| Median | 28.09 | 29.08 | 28.81 | |
| Min ; Max | 20.4; 34.3 | 19.8; 44.0 | 19.8; 44.0 | |
| Time since diagnosis of breast cancer (years) | N | 20 | 20 | 40 |
| Mean ± SD | 12.72 ± 9.87 | 15.40 ± 11.21 | 14.06 ± 10.51 | |
| Prior therapies for breast cancer | N | 20 | 20 | 40 |
| Surgery | 20 (100.0%) | 20 (100.0%) | 40 (100.0%) | |
| Time since latest surgery (years) | Mean ± SD | 10.78 ± 8.80 | 12.44 ± 9.39 | 11.61 ± 9.02 |
| Type of surgery | ||||
| Tumorectomy | 5 (25.0%) | 7 (35.0%) | 12 (30.0%) | |
| Tumorectomy + sentinel lymph node removal and/or entire lymph node removal | 5 (25.0%) | 7 (35.0%) | 12 (60%) | |
| Mastectomy | 3 (15.0%) | 3 (15.0%) | 6 (15.0%) | |
| Mastectomy + entire lymph node removal or entire lymph node removal | 7 (35.0%) | 3 (15.0%) | 10 (50.0%) | |
| Sentinel lymph node removal | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | |
| Radiotherapy | 20 (100.0%) | 20 (100.0%) | 40 (100.0%) | |
| Chemotherapy | 12 (60.0%) | 12 (60.0%) | 24 (60.0%) | |
| Hormone therapy | N | 7 (35.0%) | 7 (35.0%) | 14 (35.0%) |
| Time since lymphedema diagnosis (years) | N | 20 | 20 | 40 |
| Mean ± SD | 7.08 ± 5.52 | 9.62 ± 7.98 | 8.35 ± 6.90 | |
| Median | 7.00 | 7.13 | 7.00 | |
| Min; Max | 0.5; 20.5 | 0.5; 28.7 | 0.5; 28.7 | |
| Lymphedema stage | N | 20 | 20 | 40 |
| Stage II | 20 (100.0%) | 17 (85.0%) | 37 (92.5%) | |
| Stage III | 0 (0.0%) | 3 (15.0%) | 3 (7.5%) | |
| Pitting signs | N | 20 | 20 | 40 |
| Absent | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | |
| + | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | |
| ++ | 18 (90.0%) | 17 (85.0%) | 35 (87.5%) | |
| +++ | 2 (10.0%) | 3 (15.0%) | 5 (12.5%) | |
| ++++ | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | |
The majority of the patients (92.2%) presented stage II lymphedema with a pitting sign distributed between ++ (87.5%) and +++ (12.5%).
Efficacy results
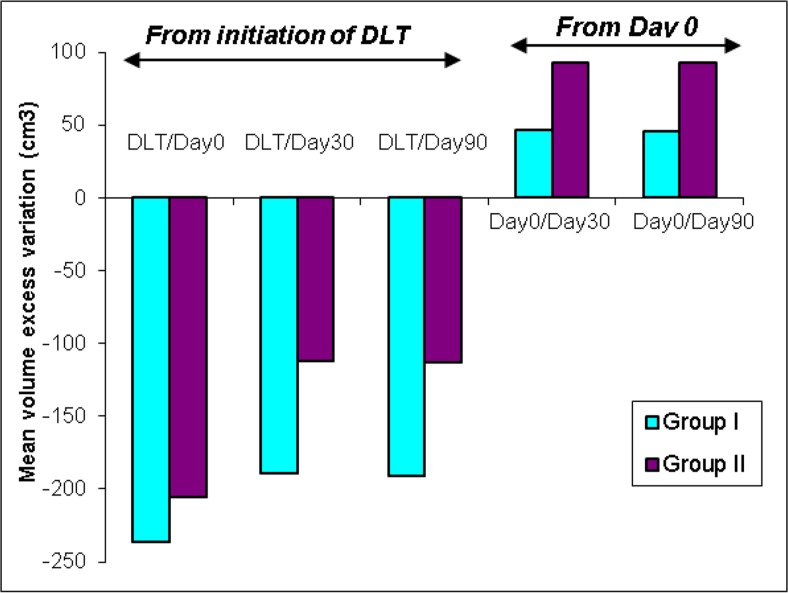
Lymphedema volume variation for each time period analysis (Day 0–Day 30–Day 90 and also according to the initiation of intensive phase (DLT initiation)) is displayed in Fig. 3. At D0, mean lymphedema volume variation was 436.9 mL ± 392.7 (range −0.5 to 1443.5) in the night-use group and 585.5 mL ± 397.7 (range −262.2 to 1493.1) in the no night-use group. As shown in the figure, in the intent-to-treat (ITT) population, the mean lymphedema volume variation at Day 30 (primary efficacy endpoint) was 46.7 mL ± 99.00 [0.41; 93.07] (i.e., median increase 1.8%) in the night-use group and was two times higher in the no night-use group, 92.9 mL ± 196.77 [0.77; 184.95] (i.e., median increase 3.2%), (p = 0.757). In the PP population (n = 35), the in-between group difference was slightly more important with, at Day 30, 51.36 mL ± 99.26 [3.72; 99.41] (i.e., median increase 2.2%) in the night-use group vs. 108.27 mL ± 212.11 [−4.75; 221.30] (i.e., median increase 6.32%) in the no night-use group.
Fig. 3.
Volume excess variation–ITT set. The figure displays the mean volume excess variations (mL) calculated using with circumferential method in the two treatment groups at each time point (Day 30 and Day 90) compared to Day 0 (baseline) and to the initiation of intensive phase (DLT initiation)
From Day 30 to Day 90, when all patients were fitted with MOBIDERM® Autofit, a stabilization of the lymphedema volume was obtained in both groups (−1.2 mL in night-use group vs. −0.3 mL in no night-use group).
During the intensive phase of DLT (before study period), the mean lymphedema volume reduction was more important in night-use group than in no night-use group (−236.2 mL vs − 205.2 mL, respectively). From the initiation of the intensive phase of the DLT to Day 30 of the maintenance phase, mean lymphedema volume decreased by −189.5 mL in night-use group and 112.3 mL in no night-use group and by −190.7 mL in night-use group and −112.6 mL in no night-use group at Day 90.
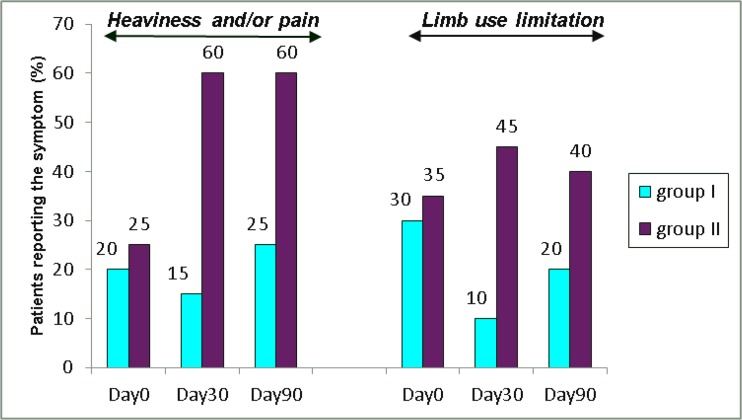
Functional symptoms at baseline were well balanced between groups (Fig. 4). At Day 30, a higher proportion of patients in no night-use group complained with functional symptoms (60 vs. 15% reported heaviness and/or pain, and 45% vs. 10% reported limb use limitation in no night-use group vs. night-use group, respectively). The same trend was observed until Day 90 with always 60% (n = 12/20) in no night-use group having reported heaviness and /or pain symptoms vs. 25% (n = 5/20) in night-use group. Limb use limitation was reported in 20% (n = 4/20) of the patients in night-use group vs. 40% (n = 8/20) in no night-use group at the end of the study period.
Fig. 4.
Functional symptoms evolution legend: the figure shows the evolution of functional symptoms (namely, heaviness and/or pain, and limb use limitation) at each study time points (Day 0, Day 30 and Day 90) in both treatment groups
Treatment exposure and compliance to the medical devices
During the first month (Day 0–Day 30), the daytime hosiery was worn all day long for a mean of 79 and 93% of the days by night-use group and no night-use group patients, respectively. The MOBIDERM® Autofit was worn all night long for a mean of 84.5% of the nights.
Between Day 30 and D90, 94.7% (n = 18/19) wore the daytime arm sleeve every day in night-use group and 90% (18/20) in no night-use group. The MOBIDERM® Autofit was worn every night by 79% (n = 15/19) and 95% (n = 19/20) of the patients in night-use group and no night-use group, respectively.
Safety and local tolerability
Overall, a total of 31 patients (77.5%) experienced at least one AE for a total of 64 events (36 in night-use group and 28 in no night-use group), of which 11 events (n = 8 patients i.e., 40% of night-use group patients) were considered as device-related. Most frequently related AEs to MOBIDERM® Autofit arm sleeve were erythema (n = 5) and pruritis (n = 4), but none of them were severe. No discontinuation related to AE was observed in the trial. Two serious adverse events (SAEs) occurred during the study, none was related to the study device.
Assessment of skin tolerability showed that the most frequent cutaneous reactions were skin compression marks (n = 15, 8 in night-use group and 7 in no night-use group), related to day compression sleeve by clinicians and rapidly decreasing redness (n = 5). No feeling of heat was reported. No significant variation of the hand’s volume, assessed at Day 30 and Day 90 as compared to Day 0, was observed, suggesting absence of the lymphedema migration to the hand.
Quality of life, sleep quality and patient satisfaction
Overall QoL and by specific domains (symptoms, appearance, mood, and function) were assessed over the study period. In line with symptoms, function domain was improved in night-use group (−0.4 pts) vs. no night-use group (+0.1 pts). Others domains remained quite stable in both groups over the study period. Sleep-related issues showed no alteration of sleep throughout the study with the same sleep quality score in both groups.
A total of 82% patients were globally satisfied by the auto-adjustable MOBIDERM® Autofit. For 70% of the patients, the device was considered easy or very easy to wear. Almost three quarters of the patients reported that they did not have any trouble sleeping with. The arm sleeve was assessed as comfortable or very comfortable by more than 90% of the patients. The pressure on the arm during the night was bearable for 87.2% of the patients.
Discussion
This is the first study evaluating the effects of the nighttime auto-adjustable MOBIDERM® Autofit arm sleeve in women with BCRL who had just completed intensive phase of DLT. We observed a different variation of lymphedema volume between the two groups in favor of the night-use group. In the ITT population, the lymphedema volume variation from Day 0 to Day 30 (relative median, primary efficacy endpoint) was lower in patients fitted with MOBIDERM® Autofit (night use group) vs. the no night-use group (1.8 vs. 3.2%, respectively). The introduction during the first 30 nights of Autofit in night-use group patients, a critical period following intensive phase of DLT associated with high risk of lymphedema volume increase, should have limited maintenance phase failure, as compared to no night-use group patients treated without night device.
From Day 30 to Day 90, when all patients were fitted with the auto-adjustable MOBIDERM® Autofit arm sleeve during the night, the lymphedema volume remained stable in both groups, suggesting that the device allowed stabilization of the lymphedema volume as soon as it is putted on. Interestingly, this stabilization observed in night-use group is associated with improvement of the functional symptoms as well as the function as assessed by the patients.
High quality compressive garments are important to maintain and optimize the volume reduction achieved during the intensive phase of DLT. Long term and consistent use of garments or bandages during the night are encouraged by ILF [10]. Vignes et al. [8] showed that women who wore a daytime compression sleeve associated with nighttime low-stretch compression bandages had a significantly reduced risk of relapse in arm lymphedema volume. However, self-bandaging remain a difficult process for patients, especially for arm. In addition, multilayers bandages composition varies widely (number of layers, type of material, number of overlaps) and the final quality is operator-dependent. Our results showed that MOBIDERM® Autofit night sleeve can stabilize lymphedema volume during the first 3 months of the maintenance phase and improve some domains of quality of life and functional symptoms as an add-on treatment.
Patient’s adherence to the therapy is an important factor in the long-term management of lymphedema. It has been shown that the persistence of reduced lymphedema volume is associated with good patient’s compliance [16]. In our study, during the first month, MOBIDERM® Autofit was worn all night long for a mean of 84.5% of the nights. The same levels of compliance are observed from D30 to D90 in both groups, confirming the high acceptability of the device by patients. This result is in accordance to the great satisfaction reported by patients who especially liked the speed to put it on and the auto-adjustable nature of the product giving patients autonomy and opportunity to take part of their own treatment. Our data also proved that this device has a good safety profile, which could be a contributing factor to the observed good compliance.
This original proof of concept study shows that night arm-sleeve MOBIDERM® Autofit can be a useful device to stabilize lymphedema volume during maintenance phase treatment. The benefit seems to be greater in case of early treatment initiation after DLT intensive phase. Moreover, the study shows that it is a well-accepted device that enhances patient’s autonomy. Consecutive inclusion over a short period in a single site limited the selection bias; also it is worth noting that, the study population and lymphedema characteristics is representative of the population of patients with BCRL.
The limit of the study is the small sample size to show the statistical significance. As there are very few articles dealing precisely on the maintenance phase of lymphedema therapy and specifically on night garment effect, it was difficult to initially hypothesis the treatment effects. The results need to be confirmed in an appropriately powered study.
Conclusion
The results of this study suggest that auto-adjustable MOBIDERM® Autofit night sleeve, on top of daily compression, offer benefit to patients during maintenance phase of lymphedema treatment and enhances patient’s autonomy.
Acknowledgments
We thank all the patients who took their time to participate in the study and all the team of the unit of lymphology, Montpellier University Hospital that allowed this study to be achieved in the best conditions, especially our caregivers Véronique Bouys, physiotherapist; Florence Delseny, physiotherapist; Fabienne Mourgues, nurse; and Hélène Pourquier, physiotherapist. And also Daniel Pontal, clinical research associate;
Stéphanie Badouaille, secretary; and the patients’ association AVML « Vivre mieux le lymphoedeme ».
Compliance with ethical standards
The study was conducted in accordance with the Declaration of Helsinki and the International Conference on Harmonization Good Clinical Practice Guidelines (ICH-GCP). Prior to study start, the protocol received approval from health authorities and ethics committee. Written informed consent was obtained from each patient prior to study enrolment.
Role of funding source
The sponsor participated in the design of the study, had oversight on the conduct of the study, and participated in interpretation of data and the decision to publish the results. The corresponding author had full access to all of the data and the final responsibility to submit for publication.
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Petrek JA, Heelan MC. Incidence of breast carcinoma-related lymphedema. Cancer. 1998;83:2776–1781. doi: 10.1002/(SICI)1097-0142(19981215)83:12B+<2776::AID-CNCR25>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 2.Meric F, Buchholz TA, Mirza NQ, Vlastos G, Ames FC, Ross MI, et al. Long-term complications associated with breast-conservation surgery and radiotherapy. Ann Surg Oncol. 2002;9(6):543–549. doi: 10.1007/BF02573889. [DOI] [PubMed] [Google Scholar]
- 3.Clark B, Sitzia J, Harlow W. Incidence and risk of arm oedema following treatment for breast cancer: a three-year follow-up study. QJM. 2005;98(5):343–348. doi: 10.1093/qjmed/hci053. [DOI] [PubMed] [Google Scholar]
- 4.Campbell KL, Pusic AL, Zucker DS, McNeely ML, Binkley JM, Cheville AL, Harwood KJ. A prospective model of care for breast cancer rehabilitation: function. Cancer. 2012;118(8 Suppl):2300–2311. doi: 10.1002/cncr.27464. [DOI] [PubMed] [Google Scholar]
- 5.Paskett ED, Dean JA, Oliveri JM, Harrop JP. Cancer-related lymphedema risk factors, diagnosis, treatment, and impact: a review. J Clin Oncol. 2012;30(30):3726–3733. doi: 10.1200/JCO.2012.41.8574. [DOI] [PubMed] [Google Scholar]
- 6.Cheville AL, McGarvey CL, Petrek JA, Russo SA, Taylor ME, Thiadens SR. Lymphedema management. Semin Radiat Oncol. 2003;13(3):290–301. doi: 10.1016/S1053-4296(03)00035-3. [DOI] [PubMed] [Google Scholar]
- 7.Lymphoedema Framework. Best practice for the management of lymphoedema–International Consensus, 2006. Available at: http://www.woundsinternational.com/media/issues/210/files/content_175.pdf
- 8.Vignes S, Porcher R, Arrault M, Dupuy A. Factors influencing breast cancer-related lymphedema volume after intensive decongestive physiotherapy. Support Care Cancer. 2011;19(7):935–940. doi: 10.1007/s00520-010-0906-x. [DOI] [PubMed] [Google Scholar]
- 9.Quéré I, Presles E, Coupe M, Vignes S, Vaillant L, Eveno D, et al. Prospective multicentre observational study of lymphedema therapy: POLIT study. J Mal Vasc. 2014;39(4):256–263. doi: 10.1016/j.jmv.2014.05.004. [DOI] [PubMed] [Google Scholar]
- 10.The International Lymphoedema Framework. Best Practice for the management of lymphoedema - Second edition, 2012.
- 11.Haute Autorité de Santé 2010. Dispositifs de compression médicale à usage individuel. Utilisation en pathologies vasculaires. Available at: http://www.has-sante.fr/portail/upload/docs/application/pdf/2010-12/synthese_rapport_compression_medicale_vf.pdf
- 12.Damstra RJ, Partsch H. Compression therapy in breast cancer-related lymphedema: A randomized, controlled comparative study of relation between volume and interface pressure changes. J Vasc Surg. 2009;49(5):1256–1263. doi: 10.1016/j.jvs.2008.12.018. [DOI] [PubMed] [Google Scholar]
- 13.Megens AM, Harris SR, Kim-Sing C, McKenzie DC. Measurementof upper extremity volume in women after axillary dissectionfor breast cancer. Arch Phys Med Rehabil. 2001;82:1639–1644. doi: 10.1053/apmr.2001.26822. [DOI] [PubMed] [Google Scholar]
- 14.Galland C, Auvert JF, Flahault A, Vayssairat M. Why and how post-mastectomy edema should be quantified in patients withbreast cancer. Breast Cancer Res Treat. 2002;75:87–89. doi: 10.1023/A:1016522319282. [DOI] [PubMed] [Google Scholar]
- 15.Keeley V, Crooks S, Locke J, Veigas D, Riches K, Hilliam R. A quality of life measure for limb lymphoedema (LYMQOL) Journal of Lymphoedema. 2010;5(1):26–37. [Google Scholar]
- 17.Boris M, Weindorf S, Lasinkski S. Persistence of lymphedema reduction after noninvasive complex lymphedema therapy. Oncology (Williston Park) 1997;11(1):99–109. [PubMed] [Google Scholar]