Abstract
Summary
This case report describes a 38-year-old woman, who presented with bilateral femoral stress fractures and osteoporosis after years of excessive levothyroxine treatment. Her bone health was restored rapidly and long-lasting with the reduction of levothyroxine dosage. No bone-active treatment was warranted.
Introduction
Hyperthyroidism is a known risk factor for osteoporosis and fractures. Recent studies on patients with serum thyrotropin-suppressive therapy have not, however, indicated adverse effects on bone during long-term follow-up.
Methods
This case report describes long-term follow-up data of a clinically euthyreoid patient, who developed symptomatic osteoporosis due to excessive levothyroxine treatment.
Results
After correction of levothyroxine dosage, her bone mineral density (BMD) and previously elevated serum osteocalcin levels normalized rapidly and she remained free from fractures during 23 years of follow-up over menopause.
Conclusion
Excessive TSH suppression contributed to the secondary osteoporosis in this patient; BMD normalized after dose reduction of levothyroxine and no fractures occurred during 23 years’ follow-up. Some patients develop severe osteoporosis if they are over-substituted with levothyroxine, and decent follow-up of patients with levothyroxine supplementation is mandatory.
Keywords: Bone mineral density, Fracture, Levothyroxine, Secondary osteoporosis
Introduction
Hyperthyroidism is a known cause of accelerated bone turnover and bone loss and increases the risk of osteoporosis and fragility fractures. Also, subclinical hyperthyroidism, and even serum thyrotropin (S-TSH) levels within the low-normal range in euthyroid elderly women, has been shown to increase the risk of low bone mineral density (BMD) and fractures [1–3]. When examining patients with long-term levothyroxine treatment, both high and low S-TSH levels have been indicated to increase the risk of fragility fractures [4]. Study results are, however, conflicting. In recent studies neither young nor elderly women receiving TSH-suppressive therapy after treatment for thyroid cancer exhibited adverse effects on BMD or fracture rates during at least 10 years of follow-up [5, 6].
In this case report, we present the severe consequence of excessive levothyroxine therapy in an otherwise healthy woman and the complete remission with correction of dosage. The presentation includes long-term follow-up extending over menopause.
Case report
A 38-year-old non-smoking woman was referred to the endocrine out-patient clinic in 1993 for assessment due to stress fractures. She had undergone thyroidectomy at the age of 12 years due to a papillary thyroid adenoma and had thereafter received levothyroxine replacement therapy. Her postoperative serum calcium levels had been normal. The follow-up in the primary health care had been insufficient, however, and she had used a daily dose of 0.3 mg (300 μg) levothyroxine since her teens. An extensive biochemical assessment including screening for other hormone disturbances and chronical illnesses was normal.
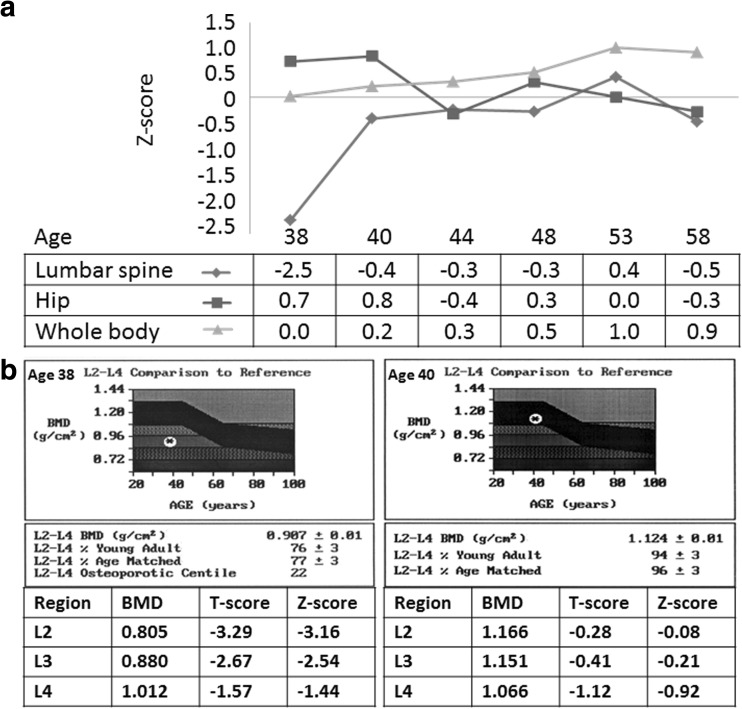
She trained excessively, running 10–20 km 5–6 times a week, and had recently experienced debilitating pain in both thighs caused by bilateral femoral stress fractures, which was confirmed by bone scintigraphy in October 1992. She also had a recent history of one low-impact forearm fracture and eight rib fractures at separate occasions, e.g., from lifting a heavy object. Her anterior-posterior lumbar BMD Z-score (L1-L4) was −2.5, and the lowest Z-score was −3.2 in L2, and similarly at the lateral spine projection. Her hip BMD Z-score was normal; +0.7 (Fig. 1a, b left panel). At the time of the first bone scintigraphy in 1992, she had a transiently elevated serum calcium level (2.68 mmol/L; reference range 2.15–2.50) but normal serum alkaline phosphatase (3.1 μkat/L; reference range 0–5.0). At first assessment at our clinic, she was clinically euthyroid with a heart rate of 78 beats/min and normal blood pressure. She was of normal build, her menstrual cycle was regular, and she had two healthy children. She experienced no tremor, excessive perspiration, or palpitations. Biochemical analyses revealed a high serum free T4 (37 ng/L; reference range 10–22 ng/L), an undetectable TSH, an elevated osteocalcin level, but normal levels of other bone markers and 25-hydroxyvitamin D. Biochemical markers at first assessment in February 1993 and during follow-up are presented in Table 1.
Fig. 1.
Bone mineral density (BMD) changes pictured over time in a woman with years of excessive levothyroxine dosage. The dosage was reduced at age 38, and she experienced menopause at age 55. a. Z-scores during 20 years of follow-up. b. Left panel: lumbar spine BMD at age 38 years. Right panel: lumbar spine BMD at age 40 years
Table 1.
Patient and biochemical variables during follow-up. The reference ranges are marked in parentheses; the reference ranges which have changed during follow-up are marked with an asterisk
| 1993 | 1994 | 1996 | 2000 | 2016 | |
|---|---|---|---|---|---|
| Height, cm | 172 | 172 | 171 | 170 | 169 |
| Body weight, kg | 60 | 59 | 61 | 60 | 62 |
| BMI, kg/m2 | 20.3 | 19.9 | 20.9 | 20.8 | 21.7 |
| Levothyroxine, average daily dose (μg) | 300 | 125 | 100 | 112.5 | 107 |
| Free T4, pmol/L (10–22) | 37 | 15 | 15 | 12 | 24 |
| T3, nmol/L (1.3–3.1) | 2.6 | 2.4 | 1.6 | ||
| TSH, mU/L (0.2–4.2) | 0.0001 | 0.015 | 0.03 | 0.28 | 0.06 |
| Osteocalcin, μg/L (3.0–7.5)(5.4–59)* | 9.6 | 6.8 | 7.0 | 6.0 | 19* |
| PTH, ng/L (10–64)(1.6–6.9 pmol/L)* | 31.8 | 41.2 | 53 | 3.77* | |
| Calcium, mmol/L (2.15–2.5) | 2.39 | 2.37 | 2.36 | 2.34 | 2.5 |
| Ionized calcium, mmol/L(1.18–1.31) | 1.30 | 1.27 | 1.21 | 1.23 |
The levothyroxine dose was successively lowered to 0.1 mg (100 μg) daily, and 6 months later, her femoral pain had subsided, her resting heart rate had dropped to 60 beats/min, and her weight was unaltered. A bone scintigraphy in 1993 showed diminished isotope uptake in affected femoral regions, and she was at the time still running 5–10 km 3–4 times a week. She experienced that her physical condition had improved substantially with the lowering of the resting heart rate and of the maximum pulse rate during exercise. She soon thereafter increased her training to previous levels and continued competing in long-distance running for several years. Her lumbar spine BMD normalized within 2 years without any bone-specific treatments or supplements (Fig. 1a, b right panel). During follow-up for over 20 years, her BMD remained normal past menopause, and she has not experienced fractures or bone pain despite continuing her active running regime. The last 10 years, she has mainly participated in public running happenings and no longer at elite level.
Conclusions
Our patient suffered severe symptoms from her osteoporosis and her condition was rapidly reversed with a lowering of levothyroxine dosage. During the most painful phase, before the stress fractures started healing, she trained by cycling, but resumed running only 2 months later. Long-distance runners are known to have lower spine BMD, and her temporary rest may have contributed to the fast improvement of spine BMD [7]. On the other hand, she resumed her excessive training soon thereafter and no decrease in spine BMD could be detected. Her bone health has since remained normal during 20 years and past menopause. At the time of diagnosis, our patient had an elevated level of serum osteocalcin and normal serum alkaline phosphatase. In 1993, no other bone turnover markers could be analyzed at our hospital. Osteocalcin levels are known to rise with increasing triiodothyronine levels, and bone resorption markers to decline with treatment for hyperthyreosis [8, 9]. The association between a hyperactive thyroid, high-turnover bone loss, and increased risk for fractures is well-established, and reversal of osteoporosis after thyreostatic treatment has been documented previously [10–12]. The molecular and cellular mechanism behind hyperthyreosis-induced osteoporosis is not completely understood. Due to the physiological reciprocal correlation between thyroid hormones and TSH, it is difficult to clinically discriminate which hormone alteration is the cause of bone loss. Some results indicate that TSH induces a direct effect on bone cells through TSH receptors, and low TSH receptor activation may enhance osteoclast function and downregulate osteoblast differentiation inducing a state of high-turnover bone metabolism, while other studies show that T3 controls bone cells through activating thyroid hormone receptor α1 [13–15]. While clarification of the molecular and cellular functions could aid in the development of future remedies for osteoporosis, the treatment of our and similar patients is quite straight-forward. The goal is to normalize the hypothalamic-pituitary-thyroid axis and thereby bone health is restored.
For patient groups in need of TSH-suppressive therapy, e.g., after thyroid malignancy, the issue of bone health is more complicated. Based on recent studies, low levels of TSH increase the risk for low BMD and fractures, particularly in postmenopausal women, but since prospective studies on fracture risk in young women and men are scarce, the risk of TSH-suppressive therapy is difficult to assess properly [2, 3, 14, 16]. Our patient suffered significantly from her hyperthyroid bone condition, but on the other hand, she had used a higher levothyroxine dose than normally prescribed in TSH-suppressive therapy (5.0 vs 2–3 μg/kg/day) [6]. This may explain why her bone status was more severely affected than in other premenopausal women in presented studies [5, 6]. Other factors, such as heredity and nutrient intake, can also affect the tendency for bone loss in an individual. The reason why only her spinal BMD had decreased may be due to the fact that trabecular bone is more sensitive to high-turnover states than the weight-bearing cortical bone, as has been seen previously in TSH-suppressed patients [16, 17]. Her long-distance running may also have influenced the severity of her symptoms. However, as she continued the long-distance running fairly soon, within 2 months, after the fractures, we believe that the normalized BMD was due to the reduction of the levothyroxine dose which the patient complied with. Hence, only one of the two possible contributing factors to the secondary osteoporosis was treated and the result was excellent.
The conclusion is that even though levothyroxine supplementation in the hypothyroid patient may seem like a routine matter for many physicians, we have the responsibility to monitor our patients regularly to avoid unnecessary side-effects. Serum free T4 and TSH should be kept within the reference range for the usual regimen of levothyroxine replacement in hypothyroidism. The levothyroxine dosage to achieve TSH suppression after thyroid cancer should be titrated to the smallest possible dose as to avoid complications. For patients with thyroid cancer, reference guidelines regarding TSH suppression take into account the severity of the malignancy as well as treatment response. Patients with low-grade malignancy and a structural and biochemical complete response to treatment should be substituted to a TSH level of 0.5 to 2.0 mU/L; patients with incomplete biochemical response or increased risk of relapse to a TSH level of 0.1 to 0.5 mU/L and patients with a high risk of relapse to a TSH level below 0.1 mU/L [18]. Bone-active treatment was not given to our patient and was unwarranted in this case of evident secondary osteoporosis.
Compliance with ethical standards
Conflicts of interest
None.
Footnotes
The abstract was presented orally by Kerstin Landin-Wilhelmsen at the Master Clinician Session at The Endocrine Society Annual Meeting in San Francisco, CA, USA 2013.
References
- 1.Taylor PN, Razvi S, Pearce SH, Dayan CM. Clinical review: a review of the clinical consequences of variation in thyroid function within the reference range. J Clin Endocrinol Metab. 2013;98(9):3562–3571. doi: 10.1210/jc.2013-1315. [DOI] [PubMed] [Google Scholar]
- 2.Leader A, Ayzenfeld RH, Lishner M, Cohen E, Segev D, Hermoni D. Thyrotropin levels within the lower normal range are associated with an increased risk of hip fractures in euthyroid women, but not men, over the age of 65 years. J Clin Endocrinol Metab. 2014;99(8):2665–2673. doi: 10.1210/jc.2013-2474. [DOI] [PubMed] [Google Scholar]
- 3.Noh HM, Park YS, Lee J, Lee W. A cross-sectional study to examine the correlation between serum TSH levels and the osteoporosis of the lumbar spine in healthy women with normal thyroid function. Osteoporos Int. 2015;26(3):997–1003. doi: 10.1007/s00198-014-2906-z. [DOI] [PubMed] [Google Scholar]
- 4.Flynn RW, Bonellie SR, Jung RT, MacDonald TM, Morris AD, Leese GP. Serum thyroid-stimulating hormone concentration and morbidity from cardiovascular disease and fractures in patients on long-term thyroxine therapy. J Clin Endocrinol Metab. 2010;95(1):186–193. doi: 10.1210/jc.2009-1625. [DOI] [PubMed] [Google Scholar]
- 5.Lee MY, Park JH, Bae KS, Jee YG, Ko AN, Han YJ, Shin JY, Lim JS, Chung CH, Kang SJ. Bone mineral density and bone turnover markers in patients on long-term suppressive levothyroxine therapy for differentiated thyroid cancer. Ann Surg Treat Res. 2014;86(2):55–60. doi: 10.4174/astr.2014.86.2.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leonova TA, Drozd VM, Saenko VA, Mine M, Biko J, Rogounovitch TI, Takamura N, Reiners C, Yamashita S. Bone mineral density in treated at a young age for differentiated thyroid cancer after Chernobyl female patients on TSH-suppressive therapy receiving or not calcium-D3 supplementation. Endocr J. 2015;62(2):173–182. doi: 10.1507/endocrj.EJ14-0408. [DOI] [PubMed] [Google Scholar]
- 7.Hind K, Zanker C, Truscott J. Five-year follow-up investigation of bone mineral density by age in premenopausal elite-level long-distance runners. Clin J Sport Med. 2011;21(6):521–529. doi: 10.1097/JSM.0b013e3182377257. [DOI] [PubMed] [Google Scholar]
- 8.Kobe N, Takamatsu J, Ito M, Sakane S, Ohsawa N. Acute and early effects of triiodothyronine administration on serum markers of bone and mineral metabolism. Endocrine. 1999;10(1):53–56. doi: 10.1385/ENDO:10:1:53. [DOI] [PubMed] [Google Scholar]
- 9.Yoshihara A, Yoshimura Noh J, Mukasa K, Watanabe N, Iwaku K, Ohye H, Suzuki M, Matsumoto M, Kunii Y, Suzuki N, Endo K, Suzuki R, Hattori N, Sugino K, Ito K (2016) The characteristics of osteoporotic patients in Graves’ disease patients newly diagnosed after menopause: a prospective observational study. Endocr J [DOI] [PubMed]
- 10.Cummings SR, Nevitt MC, Browner WS, Stone K, Fox KM, Ensrud KE, Cauley J, Black D, Vogt TM. Risk factors for hip fracture in white women. Study of osteoporotic fractures research group. N Engl J Med. 1995;332(12):767–773. doi: 10.1056/NEJM199503233321202. [DOI] [PubMed] [Google Scholar]
- 11.Vestergaard P, Mosekilde L. Hyperthyroidism, bone mineral, and fracture risk—a meta-analysis. Thyroid. 2003;13(6):585–593. doi: 10.1089/105072503322238854. [DOI] [PubMed] [Google Scholar]
- 12.Abrahamsen B, Jorgensen HL, Laulund AS, Nybo M, Brix TH, Hegedus L. Low serum thyrotropin level and duration of suppression as a predictor of major osteoporotic fractures—the OPENTHYRO register cohort. J Bone Miner Res. 2014;29(9):2040–2050. doi: 10.1002/jbmr.2244. [DOI] [PubMed] [Google Scholar]
- 13.Abe E, Marians RC, Yu W, Wu XB, Ando T, Li Y, Iqbal J, Eldeiry L, Rajendren G, Blair HC, Davies TF, Zaidi M. TSH is a negative regulator of skeletal remodeling. Cell. 2003;115(2):151–162. doi: 10.1016/S0092-8674(03)00771-2. [DOI] [PubMed] [Google Scholar]
- 14.Nicholls JJ, Brassill MJ, Williams GR, Bassett JH. The skeletal consequences of thyrotoxicosis. J Endocrinol. 2012;213(3):209–221. doi: 10.1530/JOE-12-0059. [DOI] [PubMed] [Google Scholar]
- 15.Baliram R, Sun L, Cao J, Li J, Latif R, Huber AK, Yuen T, Blair HC, Zaidi M, Davies TF. Hyperthyroid-associated osteoporosis is exacerbated by the loss of TSH signaling. J Clin Invest. 2012;122(10):3737–3741. doi: 10.1172/JCI63948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tournis S, Antoniou JD, Liakou CG, Christodoulou J, Papakitsou E, Galanos A, Makris K, Marketos H, Nikopoulou S, Tzavara I, Triantafyllopoulos IK, Dontas I, Papaioannou N, Lyritis GP, Alevizaki M. Volumetric bone mineral density and bone geometry assessed by peripheral quantitative computed tomography in women with differentiated thyroid cancer under TSH suppression. Clin Endocrinol. 2015;82(2):197–204. doi: 10.1111/cen.12560. [DOI] [PubMed] [Google Scholar]
- 17.Jodar E, Munoz-Torres M, Escobar-Jimenez F, Quesada-Charneco M, Lund del Castillo JD. Bone loss in hyperthyroid patients and in former hyperthyroid patients controlled on medical therapy: influence of aetiology and menopause. Clin Endocrinol. 1997;47(3):279–285. doi: 10.1046/j.1365-2265.1997.2261041.x. [DOI] [PubMed] [Google Scholar]
- 18.Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, Pacini F, Randolph GW, Sawka AM, Schlumberger M, Schuff KG, Sherman SI, Sosa JA, Steward DL, Tuttle RM, Wartofsky L. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016;26(1):1–133. doi: 10.1089/thy.2015.0020. [DOI] [PMC free article] [PubMed] [Google Scholar]