Abstract
Background
Among those with opioid use disorder, heroin use is associated with poorer prognosis relative to use of prescription opioids alone. However, relatively little is known about distinguishing features between those who use heroin relative to those who use prescription opioids. In the present study we evaluated differences in delay discounting in those with opioid use disorder based on primary opioid of use. Delay discounting is associated with a range of negative outcomes and is an important therapeutic target in this population.
Methods
Treatment-seeking adults with opioid dependence completed self-report measures including past-month opioid use and the Monetary Choice Questionnaire (Kirby and Marakovic, 1996; Kirby et al., 1999), a measure of delay discounting. Participants were divided into two groups based on whether they used any heroin in the past 30 days or only prescription opioids, and delay discounting scores were compared between the groups. Group differences in sociodemographic or clinical variables were included in the analysis as covariates.
Results
Results from a forward stepwise linear regression indicated that heroin use was associated with significantly higher delay discounting (B = −0.99, SEB = 0.34, t = −2.88, p = .005), even when considering covariates.
Conclusions
Adults with opioid dependence who exclusively used prescription opioids had lower delay discounting relative to those who used heroin. This finding contributes further to the literature suggesting that heroin use is associated with greater clinical severity among those with opioid use disorder.
Keywords: opioid use disorder, prescription opioids, heroin, delay discounting, impulsivity, addiction
1. INTRODUCTION
The prevalence of heroin use and heroin use disorders has risen sharply in recent years, with the rate of past-year heroin use disorders almost doubling between 2002 and 2013 in the U.S. (Jones, 2013; Jones et al., 2015). Following years of increases in prescription opioid misuse, many new heroin users report having initiated opioid use with opioid analgesic medications (Cerda et al., 2015; Jones, 2013; Novak et al., 2016). The initiation of heroin use in this population is associated with a significantly poorer prognosis (Brands et al., 2004; Moore et al., 2007; Potter et al., 2013; Rosenblum et al., 2007; Sigmon, 2006; Weiss et al., 2011). However, little is known about mechanisms that might explain differences between prescription opioid and heroin users, or facilitate the transition from prescription opioids to heroin.
One major difference between prescription opioids and heroin is that prescription opioids can be obtained legally for medical purposes. This may foster the belief that prescription opioids are less risky than heroin (Daniulaityte et al., 2012; Lord et al., 2011). Accordingly, greater impulsivity may be a distinguishing feature of those who use heroin relative to those who use only prescription opioids. Those who are more impulsive perceive risky behaviors to be less harmful (Arria et al., 2008; Doran et al., 2011; Robbins and Bryan, 2004), and may be more likely to engage in such behaviors, even adjusting for perceived risk (Ryb et al., 2006).
The tendency to over-value immediate relative to delayed reward, i.e., delay discounting, is a common feature of substance use and other addictive disorders (Bickel et al., 2014; MacKillop et al., 2011; Reynolds, 2006). Those with higher delay discounting act quickly on current needs, while devaluing future needs. This facet of impulsivity is particularly notable in opioid use disorder; heroin users not only show a dramatically larger preference for immediate rewards relative to healthy comparison samples (Kirby et al., 1999; Madden et al., 1997), but also have higher discounting rates compared to people who abuse alcohol, and rates similar to those who abuse cocaine (Kirby and Petry, 2004). Delay discounting has also been associated with negative treatment outcome in a variety of substance use disorder populations (MacKillop and Kahler, 2009; Stanger et al., 2012; Washio et al., 2011). However, only one published study has examined delay discounting among those who are dependent upon prescription opioids (Yi et al., 2007). To date, no published studies have examined differences in delay discounting between those with opioid use disorder who use prescription opioids vs. heroin.
The objective of the present study was to compare levels of delay discounting in a sample of adults with opioid use disorder, based on the type of opioid abused in the past month. We hypothesized that heroin users would show elevated delay discounting relative to prescription opioid users.
2. METHODS
2.1. Participants
A sample of 151 participants seeking treatment for opioid use disorder was recruited from an inpatient detoxification unit as part of a larger study. In this sample, 139 participants completed the delay discounting measure. Eligible participants were 18 years or older, met Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (American Psychiatric Association, 2000) criteria for opioid dependence, and were undergoing a buprenorphine stabilization and taper protocol as part of medical detoxification at the time of study participation. Exclusion criteria included presence of an acute psychiatric or medical disorder or cognitive impairment that would impede the ability to perform study procedures. Those with co-occurring substance use disorders and/or other non-acute psychiatric disorders were eligible to participate; no specific disorders were excluded.
2.2. Procedure
All procedures were approved by the local Institutional Review Board. Participants who provided written informed consent completed a battery of self-report questionnaires during one 30-minute session.
Participants were categorized into one of three groups: 1) heroin users (heroin use on ≥4 days in the 30 days prior to hospitalization, with <4 days of prescription opioid use during that time), 2) prescription opioid users (prescription opioid use on ≥4 of the 30 days prior to hospitalization, with <4 days of heroin use during that time), or 3) combined heroin and prescription opioid users ( ≥4 days of both heroin and prescription opioid use in the 30 days prior to hospitalization).
2.3. Measures
Participants self-reported demographic information. Substance use disorder and other psychiatric diagnoses were extracted from participants’ medical records.
The 17-item Brief Addiction Monitor (BAM; Cacciola et al., 2013) was used to collect information about past-month substance use. The BAM has shown good test-retest reliability as well as strong predictive validity (Cacciola et al., 2013).
The Monetary Choice Questionnaire (MCQ; Kirby and Marakovic, 1996; Kirby et al., 1999) is a 27-item self-report measure that was used to characterize participants’ rates of delay discounting. Each item presents a choice between two monetary rewards—one smaller, immediate reward and one larger, delayed reward (e.g., “Would you prefer $19 today or $25 in 53 days?”). “Discounting rates,” or k values, represent the rates at which individuals devalue rewards based on their delay, and can be inferred from individuals’ patterns of choices across items. Estimation of k values was performed according to standardized scoring procedures that utilize Excel-based software (Kirby, 2000; Kirby et al., 1999). Inconsistencies in the data, such as nonsystematic discounting, are accounted for by estimating k using a participant’s observed pattern of choices rather than his or her performance on a single item (Kirby, 2000). These procedures result in the k value that most likely gave rise to the observed data; these values can range from 0.00016 to 0.25, with higher k values indicating a stronger preference for smaller, immediate rewards and thus a more impulsive decision-making style. Consistent with previous literature (Kirby et al., 1999), k scores were log-transformed to approximate a normal distribution. The MCQ has demonstrated strong retest reliability (Kirby, 2009).
2.4. Data Analysis
The three groups of study participants were compared on sociodemographic and drug use variables using univariate analysis of variance (ANOVA) for continuous variables and chi-square tests for categorical variables. Variables for which differences were statistically significant were added to the main study analysis.
These groups were then collapsed into two groups: prescription opioid use only and any heroin use. We then conducted a forward stepwise regression examining the association between opioid type and delay discounting (log-transformed k score). This approach was used to account for the potential confounding effects of covariates, while also mitigating concern about high overlap among independent variables.
3. RESULTS
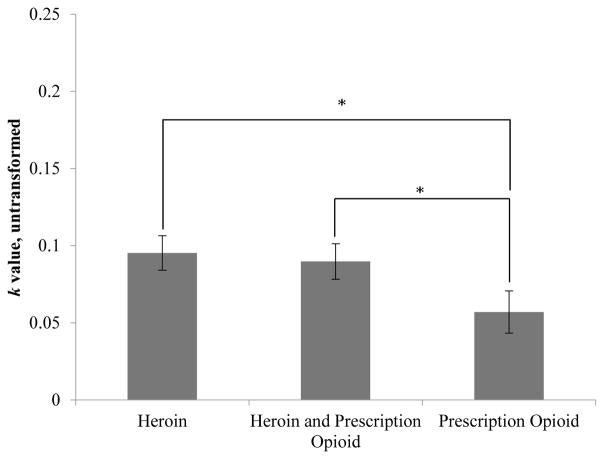
Descriptive statistics for sociodemographic and drug use variables are presented in Table 1. Based on self-reported opioid use in the 30 days prior to hospital admission, 60 participants (43.2%) were defined as heroin users, 33 (23.7%) were defined as prescription opioid users, and 46 (33.1%) were defined as combined users. The groups differed significantly with respect to age, education, current cigarette smoking, and diagnosis of a stimulant use disorder (see Table 1). Mean k scores for heroin users, combined users, and prescription opioid users were .095, .090, and .060, respectively; higher k scores denote greater delay discounting (see Figure 1).
Table 1.
Participant Characteristics by Primary Opioid
| Primary opioid (N=139) | F/χ2 | p-value | |||
|---|---|---|---|---|---|
|
| |||||
| Prescription opioid (n= 33) | Heroin (n= 60) | Combined (n= 46) | |||
| Sociodemographic | |||||
|
| |||||
| Age (years) | 38.3 (14.8) | 26.1 (5.4) | 28.0 (8.4) | 19.01 | <.001 |
| Female, % | 27.3 | 26.7 | 19.6 | 0.90 | .639 |
|
| |||||
| Caucasian, % (n=138) | 90.9 | 93.2 | 97.8 | ----- | -----a |
| Hispanic, % (n=126) | 0.0 | 0.0 | 10.0 | ----- | -----a |
|
| |||||
| Beyond high school, % | 90.9 | 63.3 | 58.7 | 10.44 | .005 |
| Employed, % (n=133) | 50.0 | 41.4 | 35.6 | 1.55 | .461 |
|
| |||||
| Past month opioid use, days | |||||
| Heroin use | 0.0 (0.0) | 24.7 (7.1) | 24.9 (7.8) | 183.60 | <.001 |
| Prescription opioid use | 24.0 (7.9) | 0.4 (0.8) | 13.0 (9.4) | 140.49 | <.001 |
| Other substance use disordersb, % | |||||
|
| |||||
| Alcohol | 30.3 | 23.3 | 19.6 | 1.23 | .540 |
| Benzodiazepines/other sedatives | 15.2 | 15.0 | 26.1 | 2.46 | .292 |
| Cocaine/other stimulants | 3.0 | 25.0 | 17.4 | 7.19 | .027 |
| Cannabis | 18.2 | 20.0 | 30.4 | 2.17 | .338 |
|
| |||||
| Current smoking status, % | 45.5 | 86.7 | 82.2 | 21.17 | <.001 |
| Axis I psychiatric comorbidity, % | 63.6 | 60.0 | 67.4 | 0.61 | .736 |
Sample was 94% Caucasian and 88% non-Hispanic; statistics were not computed for these variables due to low prevalence.
No participants met criteria for hallucinogen or inhalant use disorders
Figure 1.
Delay Discounting Scores by Primary Opioid. *p<.05; significance tests reflect univariate ANOVA comparing the natural log of k scores among the 3 groups
Because the heroin and combined users were similar in relation to both opioid use and sociodemographic characteristics, we collapsed these groups to reflect a single heroin-user group. This group was compared with the prescription opioid users, controlling for age, education, cigarette smoking, and diagnosis of a stimulant use disorder. The results of the regression indicated that only opioid group was associated with delay discounting (B = −0.99, SEB = 0.34, t = −2.88, p = .005); all other variables were excluded from the model (ps ranged from .52 to .74). Specifically, delay discounting was significantly higher among those who used heroin relative to those who exclusively used prescription opioids.
4. DISCUSSION
In a sample of adults hospitalized for opioid use disorder, we found that those who used heroin (whether with or without prescription opioids) exhibited greater delay discounting than those who exclusively used prescription opioids. These differences remained statistically significant after controlling for sociodemographic and drug use variables that differed between groups. Delay discounting is of significant clinical concern in substance-using populations due to its association with the initiation of use, addiction severity, increased risk of relapse, and risky behaviors (for review, see Bickel et al., 2014).
This finding adds to the growing literature showing clinically meaningful differences among those with opioid use disorder who use heroin vs. prescription opioids only. A recurring theme in this literature is that heroin use is associated with more severe baseline presentation and a more negative treatment outcome relative to prescription opioid use (Brands et al., 2004; Moore et al., 2007; Nielsen et al., 2015; Potter et al., 2013; Rosenblum et al., 2007; Sigmon, 2006).
Although our cross-sectional design cannot rule out the possibility that heroin use itself led to increases in delay discounting, there is some support in the literature that delay discounting precedes substance use. Audrain-McGovern et al. (2009) found that delay discounting is a trait-like characteristic across adolescence to young adulthood, and that greater delay discounting promotes acquisition of cigarette smoking. Longitudinal research examining this association in opioid users is needed to investigate whether these differences in delay discounting precede heroin use among nonmedical prescription opioid users.
The current findings suggest the potential relevance of targeting delay discounting in the treatment of heroin users, which could entail use of medication or behavioral interventions targeting impulsivity. Several studies have supported the benefits of contingency management for the treatment of opioid use disorders (Everly et al., 2011; Petry and Carroll, 2013; Petry and Martin, 2002), and this treatment appears to be associated with significant decreases in delay discounting (Landes et al., 2012). Other novel strategies for reducing delay discounting, such as the use of cognitive rehabilitation strategies (i.e., working memory training), have shown initial promise for other substances of abuse and are potential candidates for application with opioid use disorder (Bickel et al., 2011). Longitudinal research will help to identify whether such intervention is appropriate for preventing the initiation of heroin use in nonmedical prescription opioid users, for reducing relapse among those with current heroin use, or both.
This study has several limitations. The study was cross-sectional, so we are unable to determine the temporal relationships between heroin use and rates of delay discounting. Second, we do not have lifetime opioid use histories for our participants, and thus do not know whether opioid use was initiated with heroin or a prescription opioid, how long participants had been using opioids, or whether the prescription opioid users had a lifetime history of heroin use. Future research that investigates the lifetime course of opioid use disorder and accounts for the duration of opioid use is necessary to understand the impact of delay discounting across participants’ opioid use trajectories. Third, although groups did not differ with respect to prevalence of psychiatric disorders generally, we cannot rule out the possibility that co-occurring disorders affected the findings. Fourth, in our delay discounting task, monetary choices were hypothetical and not related to any actual monetary reward outcome. However, a number of studies that investigated real versus hypothetical rewards in delay discounting procedures found no effect of reward type (Lagorio and Madden, 2005; Madden et al., 2003, 2004), somewhat mitigating this concern. Finally, although the brevity of the MCQ is a strength, longer measures may afford more precision in estimating delay discounting (Epstein et al., 2003). Future studies also considering other impulsivity measures will help to clarify the link between impulsivity and heroin use. Other future directions may include consideration of the impact of factors such as the quantity and frequency of opioid use.
This study found statistically significant differences in delay discounting between those who used a substantial amount (≥4 days in the past month) of heroin relative to those who exclusively used prescription opioids. This finding provides further evidence for meaningful differences between those who misuse heroin vs. prescription opioids. Identifying risk factors for the initiation of heroin use is critical to early intervention to mitigate the significant hazards of heroin use.
Highlights.
Delay discounting is the tendency to overvalue immediate vs. delayed reward.
Adults with opioid use disorder completed a measure of delay discounting.
Prescription opioid (PO) users had lower delay discounting vs. heroin users.
Any use of heroin was associated with greater delay discounting than POs alone.
Heroin use is associated with a more impulsive style of decision-making.
Acknowledgments
Role of Funding Source
This work was supported by National Institute on Drug Abuse (NIDA) grants K23 DA035297 (Dr. McHugh) and K24 DA022288 (Dr. Weiss). NIDA had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Footnotes
Conflict of Interest
Dr. Weiss is has served as a consultant to Indivior, U.S. WorldMeds, and GW Pharmaceuticals. All other authors declare they have no conflicts of interest.
Contributors
Drs. Weiss, McHugh, and Griffin designed the original study. Dr. McHugh and Ms. Karakula designed this secondary analysis. Ms. Karakula and Dr. McHugh undertook the statistical analysis, and wrote the first draft of the manuscript. Dr. Weiss, Dr. Griffin, Ms. Borges, and Mr. Bailey contributed to the interpretation and presentation of study findings. All authors contributed to and have approved the final manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV-TR. American Psychiatric Association; Washington, DC: 2000. [Google Scholar]
- Arria AM, Caldeira KM, Vincent KB, O’Grady KE, Wish ED. Perceived harmfulness predicts nonmedical use of prescription drugs among college students: interactions with sensation-seeking. Prev Sci. 2008;9:191–201. doi: 10.1007/s11121-008-0095-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Audrain-McGovern J, Rodriguez D, Epstein LH, Cuevas J, Rodgers K, Wileyto EP. Does delay discounting play an etiological role in smoking or is it a consequence of smoking? Drug Alcohol Depend. 2009;103:99–106. doi: 10.1016/j.drugalcdep.2008.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, Koffarnus MN, Moody L, Wilson AG. The behavioral- and neuroeconomic process of temporal discounting: a candidate behavioral marker of addiction. Neuropharmacology. 2014;76(Pt. B):518–527. doi: 10.1016/j.neuropharm.2013.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, Yi R, Landes RD, Hill PF, Baxter C. Remember the future: working memory training decreases delay discounting among stimulant addicts. Biol Psychiatry. 2011;69:260–265. doi: 10.1016/j.biopsych.2010.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brands B, Blake J, Sproule B, Gourlay D, Busto U. Prescription opioid abuse in patients presenting for methadone maintenance treatment. Drug Alcohol Depend. 2004;73:199–207. doi: 10.1016/j.drugalcdep.2003.10.012. [DOI] [PubMed] [Google Scholar]
- Cacciola JS, Alterman AI, Dephilippis D, Drapkin ML, Valadez C, Jr, Fala NC, Oslin D, McKay JR. Development and initial evaluation of the Brief Addiction Monitor (BAM) J Subst Abuse Treat. 2013;44:256–263. doi: 10.1016/j.jsat.2012.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerda M, Santaella J, Marshall BD, Kim JH, Martins SS. nonmedical prescription opioid use in childhood and early adolescence predicts transitions to heroin use in young adulthood: a national study. J Pediatr. 2015;167:605–612. e601–602. doi: 10.1016/j.jpeds.2015.04.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daniulaityte R, Falck R, Carlson RG. I’m not afraid of those ones just ‘cause they’ve been prescribed”: perceptions of risk among illicit users of pharmaceutical opioids. Int J Drug Policy. 2012;23:374–384. doi: 10.1016/j.drugpo.2012.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doran N, Sanders PE, Bekman NM, Worley MJ, Monreal TK, McGee E, Cummins K, Brown SA. Mediating influences of negative affect and risk perception on the relationship between sensation seeking and adolescent cigarette smoking. Nicotine Tob Res. 2011;13:457–465. doi: 10.1093/ntr/ntr025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein LH, Richards JB, Saad FG, Paluch RA, Roemmich JN, Lerman C. Comparison between two measures of delay discounting in smokers. Exp Clin Psychopharmacol. 2003;11:131–138. doi: 10.1037/1064-1297.11.2.131. [DOI] [PubMed] [Google Scholar]
- Everly JJ, DeFulio A, Koffarnus MN, Leoutsakos JM, Donlin WD, Aklin WM, Umbricht A, Fingerhood M, Bigelow GE, Silverman K. Employment-based reinforcement of adherence to depot naltrexone in unemployed opioid-dependent adults: a randomized controlled trial. Addiction. 2011;106:1309–1318. doi: 10.1111/j.1360-0443.2011.03400.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones CM. Heroin use and heroin use risk behaviors among nonmedical users of prescription opioid pain relievers - United States, 2002–2004 and 2008–2010. Drug Alcohol Depend. 2013;132:95–100. doi: 10.1016/j.drugalcdep.2013.01.007. [DOI] [PubMed] [Google Scholar]
- Jones CM, Logan J, Gladden RM, Bohm MK. Vital signs: demographic and substance use trends among heroin users - United States, 2002–2013. MMWR. 2015;64:719–725. [PMC free article] [PubMed] [Google Scholar]
- Kirby KN. Instructions For Inferring Discount Rates From Choices Between Immediate And Delayed Rewards. Williams College; Williamstown, MA, USA: 2000. [Google Scholar]
- Kirby KN. One-year temporal stability of delay-discount rates. Psychon Bull Rev. 2009;16:457–462. doi: 10.3758/PBR.16.3.457. [DOI] [PubMed] [Google Scholar]
- Kirby KN, Marakovic NN. Delay-discounting probabilistic rewards: rates decrease as amounts increase. Psychon Bull Rev. 1996;3:100–104. doi: 10.3758/BF03210748. [DOI] [PubMed] [Google Scholar]
- Kirby KN, Petry NM. Heroin and cocaine abusers have higher discount rates for delayed rewards than alcoholics or non-drug-using controls. Addiction. 2004;99:461–471. doi: 10.1111/j.1360-0443.2003.00669.x. [DOI] [PubMed] [Google Scholar]
- Kirby KN, Petry NM, Bickel WK. Heroin addicts have higher discount rates for delayed rewards than non-drug-using controls. J Exp Psychol Gen. 1999;128:78–87. doi: 10.1037//0096-3445.128.1.78. [DOI] [PubMed] [Google Scholar]
- Lagorio CH, Madden GJ. Delay discounting of real and hypothetical rewards III: steady-state assessments, forced-choice trials, and all real rewards. Behav Processes. 2005;69:173–187. doi: 10.1016/j.beproc.2005.02.003. [DOI] [PubMed] [Google Scholar]
- Landes RD, Christensen DR, Bickel WK. Delay discounting decreases in those completing treatment for opioid dependence. Exp Clin Psychopharmacol. 2012;20:302–309. doi: 10.1037/a0027391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord S, Brevard J, Budman S. Connecting to young adults: an online social network survey of beliefs and attitudes associated with prescription opioid misuse among college students. Subst Use Misuse. 2011;46:66–76. doi: 10.3109/10826084.2011.521371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J, Amlung MT, Few LR, Ray LA, Sweet LH, Munafo MR. Delayed reward discounting and addictive behavior: a meta-analysis. Psychopharmacology (Berl) 2011;216:305–321. doi: 10.1007/s00213-011-2229-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J, Kahler CW. Delayed reward discounting predicts treatment response for heavy drinkers receiving smoking cessation treatment. Drug Alcohol Depend. 2009;104:197–203. doi: 10.1016/j.drugalcdep.2009.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madden GJ, Begotka AM, Raiff BR, Kastern LL. Delay discounting of real and hypothetical rewards. Exp Clin Psychopharmacol. 2003;11:139–145. doi: 10.1037/1064-1297.11.2.139. [DOI] [PubMed] [Google Scholar]
- Madden GJ, Petry NM, Badger GJ, Bickel WK. Impulsive and self-control choices in opioid-dependent patients and non-drug-using control participants: drug and monetary rewards. Exp Clin Psychopharmacol. 1997;5:256–262. doi: 10.1037//1064-1297.5.3.256. [DOI] [PubMed] [Google Scholar]
- Madden GJ, Raiff BR, Lagorio CH, Begotka AM, Mueller AM, Hehli DJ, Wegener AA. Delay discounting of potentially real and hypothetical rewards: II. Between-and within-subject comparisons. Exp Clin Psychopharmacol. 2004;12:251–261. doi: 10.1037/1064-1297.12.4.251. [DOI] [PubMed] [Google Scholar]
- Moore BA, Fiellin DA, Barry DT, Sullivan LE, Chawarski MC, O’Connor PG, Schottenfeld RS. Primary care office-based buprenorphine treatment: comparison of heroin and prescription opioid dependent patients. J Gen Intern Med. 2007;22:527–530. doi: 10.1007/s11606-007-0129-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nielsen S, Hillhouse M, Mooney L, Ang A, Ling W. Buprenorphine pharmacotherapy and behavioral treatment: comparison of outcomes among prescription opioid users, heroin users and combination users. J Subst Abuse Treat. 2015;48:70–76. doi: 10.1016/j.jsat.2014.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Novak SP, Bluthenthal R, Wenger L, Chu D, Kral AH. Initiation of heroin and prescription opioid pain relievers by birth cohort. Am J Public Health. 2016;106:298–300. doi: 10.2105/AJPH.2015.302972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry NM, Carroll KM. Contingency management is efficacious in opioid-dependent outpatients not maintained on agonist pharmacotherapy. Psychol Addict Behav. 2013;27:1036–1043. doi: 10.1037/a0032175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry NM, Martin B. Low-cost contingency management for treating cocaine- and opioid-abusing methadone patients. J Consult Clin Psychol. 2002;70:398–405. doi: 10.1037//0022-006x.70.2.398. [DOI] [PubMed] [Google Scholar]
- Potter JS, Marino EN, Hillhouse MP, Nielsen S, Wiest K, Canamar CP, Martin JA, Ang A, Baker R, Saxon AJ, Ling W. Buprenorphine/naloxone and methadone maintenance treatment outcomes for opioid analgesic, heroin, and combined users: findings from starting treatment with agonist replacement therapies (START) J Stud Alcohol Drugs. 2013;74:605–613. doi: 10.15288/jsad.2013.74.605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds B. A review of delay-discounting research with humans: relations to drug use and gambling. Behav Pharmacol. 2006;17:651–667. doi: 10.1097/FBP.0b013e3280115f99. [DOI] [PubMed] [Google Scholar]
- Robbins RN, Bryan A. Relationships between future orientation, impulsive sensation seeking, and risk behavior among adjudicated adolescents. J Adolesc Res. 2004;19:428–445. doi: 10.1177/0743558403258860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenblum A, Parrino M, Schnoll SH, Fong C, Maxwell C, Cleland CM, Magura S, Haddox JD. Prescription opioid abuse among enrollees into methadone maintenance treatment. Drug Alcohol Depend. 2007;90:64–71. doi: 10.1016/j.drugalcdep.2007.02.012. [DOI] [PubMed] [Google Scholar]
- Ryb GE, Dischinger PC, Kufera JA, Read KM. Risk perception and impulsivity: association with risky behaviors and substance abuse disorders. Accid Anal Prev. 2006;38:567–573. doi: 10.1016/j.aap.2005.12.001. [DOI] [PubMed] [Google Scholar]
- Sigmon SC. Characterizing the emerging population of prescription opioid abusers. Am J Addict. 2006;15:208–212. doi: 10.1080/10550490600625624. [DOI] [PubMed] [Google Scholar]
- Stanger C, Ryan SR, Fu H, Landes RD, Jones BA, Bickel WK, Budney AJ. Delay discounting predicts adolescent substance abuse treatment outcome. Exp Clin Psychopharmacol. 2012;20:205–212. doi: 10.1037/a0026543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Washio Y, Higgins ST, Heil SH, McKerchar TL, Badger GJ, Skelly JM, Dantona RL. Delay discounting is associated with treatment response among cocaine-dependent outpatients. Exp Clin Psychopharmacol. 2011;19:243–248. doi: 10.1037/a0023617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss RD, Potter JS, Fiellin DA, Byrne M, Connery HS, Dickinson W, Gardin J, Griffin ML, Gourevitch MN, Haller DL, Hasson AL, Huang Z, Jacobs P, Kosinski AS, Lindblad R, McCance-Katz EF, Provost SE, Selzer J, Somoza EC, Sonne SC, Ling W. Adjunctive counseling during brief and extended buprenorphine-naloxone treatment for prescription opioid dependence: a 2-phase randomized controlled trial. Arch Gen Psychiatry. 2011;68:1238–1246. doi: 10.1001/archgenpsychiatry.2011.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yi R, Buchhalter AR, Gatchalian KM, Bickel WK. The relationship between temporal discounting and the prisoner’s dilemma game in intranasal abusers of prescription opioids. Drug Alcohol Depend. 2007;87:94–97. doi: 10.1016/j.drugalcdep.2006.07.007. [DOI] [PubMed] [Google Scholar]