Routinely collected hospital episode statistics data can be used to calculate hospital standardised mortality ratios and adjusted death rates for various diagnoses and procedures.w1 Providing this information to hospitals can prove a stimulus to the introduction of a range of improvements in hospital care, mainly with the aim of reducing avoidable deaths. The subsequent changes in mortality can be monitored. We report the experience of Walsall Hospitals NHS Trust.
The bottom line
In 2000 Walsall Hospitals NHS Trust had an HSMR of 130, the highest of all main acute hospitals in England
After the HSMR data were published Walsall set up seven clinical governance groups to identify where improvements could be implemented
The hospital's mortality data were monitored over the next four years, and by September 2004 the HSMR had dropped to 92.8
Hospital medical care has become more complex than it was in the days when there were few effective treatments available. Now many more healthcare professionals may be involved in the increasingly complex care of an individual patient, but the possibilities for error have increased. The Bristol Inquiry,w2 Harvard medical practice study,w3 and the Institute of Medicine's report To Err Is Humanw4 have all drawn attention to the level of adverse events in hospitals and the need to avoid unnecessary deaths.
Since January 2001 Dr Foster has published hospital standardised mortality ratios (HSMRs) based on routinely collected hospital episode statistics (HES) for the major acute hospitals in England. In 2000 Walsall Hospitals NHS Trust had an HSMR of 130, the highest of all main acute hospitals in England (30% above the value for England as a whole, which is 100). Its medical director and others formed seven clinical governance groups to implement changes in clinical disease areas: heart, malignant, gastrointestinal, respiratory, renal, diabetes, other vascular groups, trauma and orthopaedics, anaesthetics, resuscitation, accident and emergency, critical care, outpatients, dietetics, children, and elderly care. Similarly, changes were initiated in management areas: audit department, clinical risk, continuing professional development unit, bed management, information services and performance management, research and development, education, discharge liaison team, workforce development, integrated care pathway development, national confidential inquiries, NICE guidelines, NSF update reports, clinical governance structure, and the primary care trust Evercare project.
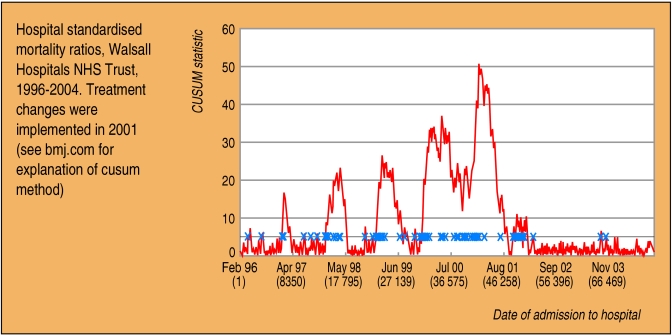
We used risk adjusted statistical process control methodsw5 to follow the changes in death rates at Walsall Hospitals NHS Trust from February 1996 to September 2004 (figure). The chart crosses the alarm threshold many times between 1996 and 2001 (implying that the risk of death at Walsall often rose to at least twice the national average during that period) but after early 2002 crossed only twice. With indirect standardisation, the HSMR at Walsall dropped from 130.0 in 2000 to 92.8 by September 2004 (see figure on bmj.com). For the diagnoses leading to 80% of all deaths, the overall reduction in the number of observed minus expected deaths was 295 (27% of observed deaths in 2001). The largest reductions were in circulatory diseases (44%) and respiratory diseases (30%). This works out at 0.14 fewer observed minus expected deaths per bed for 100% of diagnoses per year. Part of the reduction in HSMR could be due to chance, regression to the mean, better coding, different discharge policies, or referral of more complicated cases to other hospitals but, as the reductions coincided with an extensive effort to implement improvement policies, they are probably associated with improved quality of care. The number of hospital doctors per bed is the best predictor of HSMRs (lower HSMRs being associated with more doctors per bed)w1: from 1999 to 2003 Walsall's ratio of doctors per bed increased from 0.226 to 0.305.
Figure 1.
The basic figures
In year 2000 Walsall Hospitals NHS Trust had 8734 admissions for the 80 diagnoses that lead to 80% of all hospital deaths
For these diagnoses Walsall had 1080 deaths during year 2000, compared with 830.7 that would be expected using England death rates by age, sex, admission method, multiple deprivation score, and diagnosis as standard, giving an HSMR of 130 (1080/830.7×100).
After a wide range of improvements in care were introduced, starting in 2001, the adjusted fall in observed minus expected deaths at Walsall was 295 by September 2004 for the diagnoses that lead to 80% of all deaths
Supplementary Material
 This month's Dr Foster's case notes were compiled by Brian Jarman, Alex Bottle, and Paul Aylin at the Dr Foster Unit at Imperial College and Mike Browne at Walsall Hospitals NHS Trust. Dr Foster is an independent research and publishing organisation created to examine measures of clinical performance.
This month's Dr Foster's case notes were compiled by Brian Jarman, Alex Bottle, and Paul Aylin at the Dr Foster Unit at Imperial College and Mike Browne at Walsall Hospitals NHS Trust. Dr Foster is an independent research and publishing organisation created to examine measures of clinical performance.
 References, methodology, tables, and a figure are on bmj.com
References, methodology, tables, and a figure are on bmj.com
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.