Abstract
We present the case of a 43-year-old Italian woman with a left undiagnosed pleural effusion, which in subsequent months presented a clinically unexpected evolution with the appearance at first of a right wrist tenosynovitis and subsequently a bilateral lung involvement caused by M. Tuberculosis.
With this case report, we would like to underline the importance of making a correct diagnosis of any pleural effusion as soon as possible by at least a thoracocentesis. If untreated, tuberculosis may easily disseminate to other organs. Some considerations and suggestions for antibiotic treatment of pleural effusion will also be given, since many antibiotics have some anti-tuberculosis effect and may delay the diagnosis of this infectious disease.
Keywords: Pleural effusion (PE), Tuberculous tenosynovitis, Pleural tuberculosis (PT), TB- NAAT=Tuberculosis nucleic acid amplification test
1. Introduction
Extrapulmonary tuberculosis involvement of the musculoskeletal system is uncommon, accounting for only 1% to 5% of cases [1]. Even less common in musculoskeletal TB is the involvement of the joint tendons, producing tuberculous tenosynovitis [2], [3]; involvement of the wrist is uncommon, occurring in less than 1% of cases [4].
Tuberculous tenosynovitis of the wrist has been recognized as a clinical sequela to pulmonary tuberculosis for the past century [5]. Nevertheless, it is of the utmost importance to recognize combined pulmonary-extrapulmonary manifestations of tuberculosis in order to start early treatment.
2. Case report
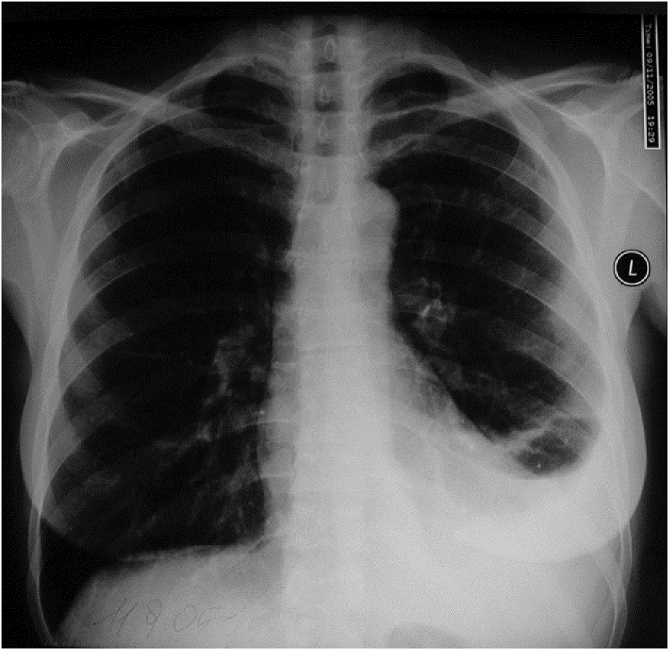
A 43-year-old Italian woman, a non-smoker, was referred to another clinic where she was treated by a pulmonologist for fever, cough and left chest pain. The chest X-ray (Fig. 1) showed a moderate left pleural effusion; she reported no comorbidity.
Fig. 1.
Left pleural effusion.
She underwent neither blood tests nor thoracentesis, as the pulmonologist did not consider these as being necessary for such a small effusion. She started treatment with 500 mg levofloxacin bis in die per os for 2 weeks.
After 2 weeks a chest X-ray showed improvement in the left pleural effusion; she had no fever (it had disappeared after 3 days of treatment), but chest pain persisted.
Two months later the patient was well, without fever, albeit with very slight thoracic pain during deep inspiration; a chest X-ray showed no parenchymal lesions, but only an occlusion of the left costophrenic sinus. CT scan was normal at that time.
At this stage, the patient asked us to intervene because she was not satisfied with her treatment by the other doctor; we decided to follow the patient up at our clinic with no other treatments or examinations since she was well and because of the complete resolution shown by the chest X-ray picture.
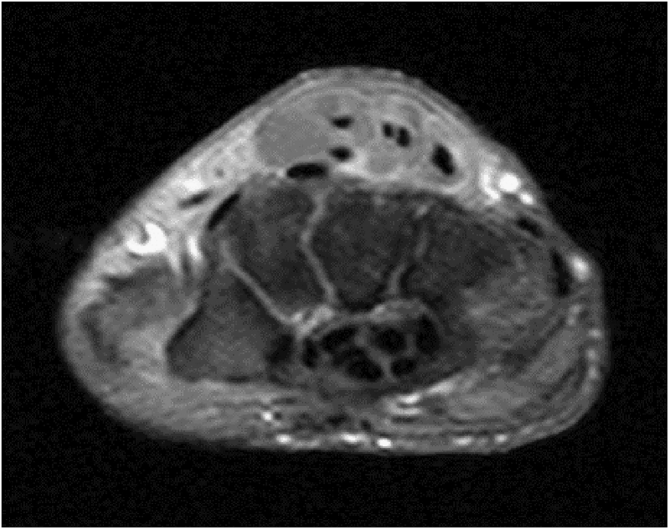
One month later, she presented with a swelling of her right wrist without fever (Fig. 2). An MRI scan showed a typical picture of tenosynovitis (Fig. 3). Rheumatic tests (C Reactive Protein, Rheumatoid factor, Antinuclear Antibodies, Cyclic Citrullinated Peptide) were completely negative and the patient was treated with Nonsteroidal Anti-Inflammatory Drugs.
Fig. 2.
Painful swelling of the right wrist and hand.
Fig. 3.
Wrist MRI SE T1-weighted axial section shows a non-homogeneous solid mass involving extensor digitorum tendons.
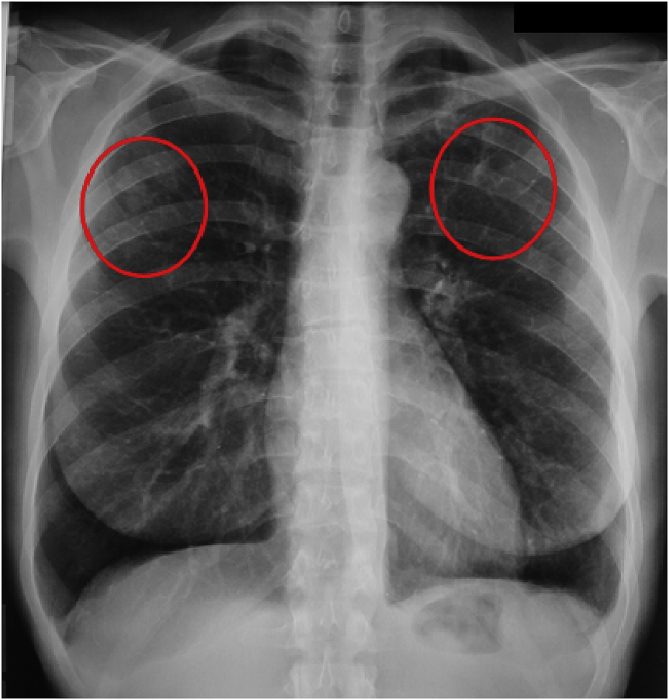
Three months later she presented high fever (39°) and cough without sputum; chest X-ray showed ill defined nodular opacities in the upper lobes and no pleural effusion (Fig. 4).
Fig. 4.
Small nodules in both upper lobes with no sign of left pleural effusion.
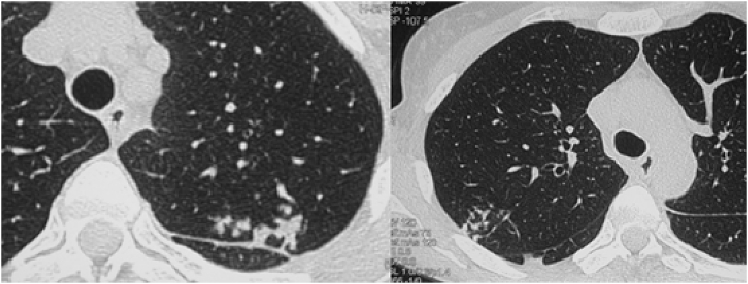
CT scan showed both speculated nodules and branching focal centrilobular opacities consistent with the so called tree-in-bud pattern in the upper lobes (Fig. 5). Laboratory tests, including HIV test, were negative.
Fig. 5.
Irregular nodules in the left apex of the lung and tree-in-bud opacities in the upper lobes.
A diagnostic fibre optic bronchoscopy was performed. There were no secretions in the tracheobronchial tree. A bronchoalveolar lavage (BAL) was performed in the upper left lobe. The BAL was stained with Kinyoun and auramin stain and tuberculosis nucleic acid amplification test (TB-NAAT) were also performed: all these results were negative. Culture on both solid (Lőwenstein Jensen, bioMérieux, Marcy l’Etoile, France) and liquid (Bactec MGIT semi-automated system – Becton Dickinson, Italy) media was positive for M. tuberculosis.
In conclusion, the patient's clinical picture can be summarized as follows: at the beginning left pleural effusion, 2 months later right wrist tenosynovitis and, after another 3 months, pulmonary tuberculosis.
We treated her with rifampicin (600 mg), isoniazid (300 mg), pyrazinamide (500 mg x 2) and ethambutol (500 mg x 3) for 2 months followed by rifampicin and isoniazid for 4 months, resulting in the complete resolution of the pulmonary and wrist involvement.
3. Discussion
The association of tuberculosis (TB) and rheumatological diseases is well known [6], [7]. Mycobacterium tuberculosis can directly infect the musculoskeletal system, as in this case; vice versa, patients with rheumatological disease are prone to develop TB because of their own underlying or drug-induced immunosuppression status.
Tenosynovitis can affect several sites, such as hand, wrist, finger, elbow, ankle, and knee [8]. Trauma, arthritis, infection, and sarcoidosis are all common conditions causing tenosynovitis [9]. Amongst the infections, M. bovis has also been described as a rare aetiology [10]. Most cases published in the literature are isolated episodes [2], [11], [12], [13], [14], [15], [16]. Our case is even more peculiar, being characterized by pleural effusion preceding the lung involvement.
Besides the rare tenosynovitis, our case emphasizes two important aspects: how a superficial diagnostic approach may delay appropriate treatment for tuberculosis and how an incorrect antibiotic therapy can be misleading.
The diagnosis of TB pleural effusion may be challenging since microbiological investigations on pleural fluid rarely yield a diagnosis of pleural TB. Although the diagnostic yield of pleural fluid is highly variable, ranging from 7% to 58% [17], [18], [19], [20], [21], it is mandatory to perform a thoracocentesis. The value of TB-NAAT on extra-pulmonary specimens is controversial [22]. Pleural fluid cytology can be helpful in the diagnosis of pleural TB as the exudate is lymphocyte predominant (≥50%) in the majority of cases [23], [24]. However, lymphocyte predominant pleural effusion can also be seen in other clinical settings such as malignancy, congestive heart failure, chylothorax, lymphoma, yellow nail syndrome, chronic rheumatoid pleurisy, sarcoidosis, and post-coronary artery bypass grafting effusions [25]; therefore, pleural fluid lymphocytosis is only indicative and serves merely to orientate the diagnosis. A lymphocyte-prominent exudative effusion associated with an adenosine deaminase (ADA) level of >40 IU in settings with a high TB prevalence is considered diagnostic for pleural TB [18]. However, in areas with a low TB prevalence such as in our area of Italy, the positive predictive value of the test is 50% and this limits its clinical usefulness [23]. Thus, increased ADA levels should not be equated to M. tuberculosis isolation in pleural fluid or biopsy specimens. False positive results can lead to unnecessary therapy or to a delay in making an alternative diagnosis [26].
Failure to obtain a diagnosis of tuberculous pleurisy results in spontaneous healing (in 35% of cases) or progression to pulmonary or extra-pulmonary tuberculosis within 5 years (in up to 65% of patients) [27]. Concerning the possible tuberculous aetiology of the pleural effusion of our patient, we believe that the subsequent clinical course and the positive response to the quinolone are more than sufficient for us to suspect a TB effusion. A proper diagnosis is therefore essential for a correct treatment. A puncture of the wrist performed at the moment of the tenosynovitis would probably have been diagnostic, avoiding subsequent lung involvement; it did not occur to us to perform one.
The patient was treated with a quinolone by the doctor who saw her before she was referred to us. Our question is: is it correct to treat a not yet microbiologically diagnosed pleural effusion with this antibiotic class? We think that it was a mistake and we agree with those authors that suggest that since the fluoroquinolones are active against M. tuberculosis complex and thus may cause transient improvement in subjects with TB they should be avoided [28], [29].
In conclusion, with this case report, we would like to emphasize the importance of a correct diagnostic approach to tuberculous pleural effusion to prevent subsequent spread of the disease.
We suggest avoiding the use of quinolones in the case of an undiagnosed pleural effusion since they could mask a tuberculous aetiology.
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Hooker M.S., Schaefer R.A., Fishbain J.T. Tuberculous tenosynovitis of the tibialis anterior tendon: a case report. Foot Ankle Int. 2002;23:1131–1134. doi: 10.1177/107110070202301210. [DOI] [PubMed] [Google Scholar]
- 2.Albornoz M.A., Mezgarzedeh M., Neumann C.H. Granulomatous tenosynovitis: a rare musculoskeletal manifestation of tuberculosis. Clin. Rheumatol. 1998:166–169. doi: 10.1007/BF01452268. [DOI] [PubMed] [Google Scholar]
- 3.Aboudola S., Sienko A., Carey R.B. Tuberculous tenosynovitis. Md Hum. Pathol. 2004;35:1044–1046. doi: 10.1016/j.humpath.2004.04.005. [DOI] [PubMed] [Google Scholar]
- 4.Kriegs-Au G., Ganger R., Petje G. The sequelae of late diagnosis in tuberculous flexor tenosynovitis of the hand—a report of 2 cases. Acta Orthop. Scand. 2003;74:221–224. doi: 10.1080/00016470310014003. [DOI] [PubMed] [Google Scholar]
- 5.Kanavel A.B. Tuberculous tenosynovitis of the hand: a report of fourteen cases of tuberculous tenosynovitis. Surg. Gynecol. Obstet. 1923;37:635–647. [Google Scholar]
- 6.Kramer N., Rosenstein E.D. Rheumatologic manifestations of tuberculosis. Bull. Rheum. Dis. 1997;46:5–8. [PubMed] [Google Scholar]
- 7.Franco-Paredes C., Díaz-Borjon A., Senger M.A. The ever-expanding association between rheumatologic diseases and tuberculosis. Am. J. Med. 2006;119:470–477. doi: 10.1016/j.amjmed.2005.10.063. [DOI] [PubMed] [Google Scholar]
- 8.Javadi S., Kan J.H., Orth R.C. Wrist and ankle MRI of patients with juvenile idiopathic arthritis: identification of unsuspected multicompartmental tenosynovitis and arthritis. AJR Am. J. Roentgenol. 2014;202:413–417. doi: 10.2214/AJR.13.10671. [DOI] [PubMed] [Google Scholar]
- 9.Al-Ani Z Z., Oh T.C., Macphie E. Sarcoid tenosynovitis, rare presentation of a common disease. Case report and literature review. J. Radiol. Case Rep. 2015;9:16–23. doi: 10.3941/jrcr.v9i8.2311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Güner M.D., Bektaş U., Akmeşe R., Kamburoğlu H.O. Wrist tenosynovitis due to Mycobacterium bovis infection: case series and review of the literature. Plast. Reconstr. Surg. Glob. Open. 2014;2:e262. doi: 10.1097/GOX.0000000000000238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mrabet D., Ouenniche K., Mizouni H. Tuberculosis tenosynovitis of the extensor tendons of the wrist. BMJ Case Rep. 2011; Aug 31:201. doi: 10.1136/bcr.06.2011.4347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sbai M.A., Benzarti S., Boussen M. Tuberculous flexor tenosynovitis of the hand. Int. J. Mycobacteriol. 2005;4:347–349. doi: 10.1016/j.ijmyco.2015.06.003. [DOI] [PubMed] [Google Scholar]
- 13.Bayram S., Ersen A., Altan M. Tuberculosis tenosynovitis with multiple rice bodies of the flexor tendons in the wrist: a case report. Int. J. Surg. Case Rep. 2016;27:129–132. doi: 10.1016/j.ijscr.2016.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chandrasekharan J., Sambandam S.N., Cheriyakara S. Tuberculous tenosynovitis presenting as finger drop: a case report and a systematic review of the literature. Muscles, Ligaments Tendons J. 2016;6:258–263. doi: 10.11138/mltj/2016.6.2.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Higuchi S., Ishihara S., Kobayashi H. A mass lesion of the wrist: a rare manifestation of tuberculosis. Intern Med. 2008;47(4):313–316. doi: 10.2169/internalmedicine.47.0495. [DOI] [PubMed] [Google Scholar]
- 16.Mrabet D., Ouenniche K., Mizouni H. Tuberculosis tenosynovitis of the extensor tendons of the wrist. BMJ Case Rep. 2011 Aug 31:2011. doi: 10.1136/bcr.06.2011.4347. A.F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Seibert, Haynes J., Jr., Middleton R. Tuberculous pleural effusion: twenty-year experience. Chest. 1991;99:387–390. doi: 10.1378/chest.99.4.883. [DOI] [PubMed] [Google Scholar]
- 18.Diacon A.H., Van de Wal B.W., Wyser C. Diagnostic tools in tuberculous pleurisy: a direct comparative study. Eur. Respir. J. 2003;22:589–591. doi: 10.1183/09031936.03.00017103a. [DOI] [PubMed] [Google Scholar]
- 19.Conde M.B., Loivos A.C., Rezende V.M. Yield of sputum induction in the diagnosis of pleural tuberculosis. Am. J. Respir. Crit. Care Med. 2003;167:723–725. doi: 10.1164/rccm.2111019. [DOI] [PubMed] [Google Scholar]
- 20.Valdes L., San Jose M.E., Pose A. Diagnosing tuberculous pleural effusion using clinical data and pleural fluid analysis. A study of patients less than 40 years-old in an area with a high incidence of tuberculosis. Respir. Med. 2010;104:1211–1217. doi: 10.1016/j.rmed.2010.02.025. [DOI] [PubMed] [Google Scholar]
- 21.Sahn S.A., Huggins J.T., San José M.E. Can tuberculous pleural effusions be diagnosed by pleural fluid analysis alone? Int. J. Tuberc. Lung Dis. 2013;17:787–793. doi: 10.5588/ijtld.12.0892. [DOI] [PubMed] [Google Scholar]
- 22.Trajman A., da Silva Santos Kleiz de Oliveira E.F., Bastos M.L. Accuracy of polymerase chain reaction for the diagnosis of pleural tuberculosis. 2014 Respir. Med. 2014;108:918–923. doi: 10.1016/j.rmed.2014.04.007. [DOI] [PubMed] [Google Scholar]
- 23.Valdes L., Alvarez D., San Jose E. Tuberculous pleurisy: a study of 254 patients. Arch. Intern Med. 1998;158:2017–2021. doi: 10.1001/archinte.158.18.2017. [DOI] [PubMed] [Google Scholar]
- 24.Dalbeth N., Gary Lee Y.C. Lymphocytes in pleural disease. Curr. Opin. Pulm. Med. 2005;11:334–339. doi: 10.1097/01.mcp.0000166490.92659.17. [DOI] [PubMed] [Google Scholar]
- 25.Sahn S.A. The value of pleural fluid analysis. Am. J. Med. Sci. 2008;335:7–15. doi: 10.1097/MAJ.0b013e31815d25e6. [DOI] [PubMed] [Google Scholar]
- 26.Trajman M. Pai, Dheda K. Novel tests for diagnosing tuberculous pleural effusion: what works and what does not? Eur. Respir. J. 2008;31:1098–1106. doi: 10.1183/09031936.00147507. [DOI] [PubMed] [Google Scholar]
- 27.Roper W.H., Waring J.J. Primary serofibrious pleural effusion in military personnel. Am. Rev. Tuberc. Pulm. Dis. 1955;71:616–634. doi: 10.1164/artpd.1955.71.5.616. [DOI] [PubMed] [Google Scholar]
- 28.Migliori G.B., Langendam Miranda W. Protecting the tuberculosis drug pipeline: stating the case for the rational use of fluoroquinolones. Eur. Respir. J. 2012;40:814–822. doi: 10.1183/09031936.00036812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Migliori G.B., Zellweger J.P., Abubakar I. ECDC/ERS task force report. European union standards for tuberculosis care. Eur. Respir. J. 2012;39:807–819. doi: 10.1183/09031936.00203811. [DOI] [PMC free article] [PubMed] [Google Scholar]