Abstract
Purpose
The aim of this study was to systematically evaluate the available literature on surgical treatment for midportion Achilles tendinopathy and to provide an overview of the different surgical techniques.
Methods
A systematic review of the literature available in MEDLINE, EMBASE and the Cochrane database of controlled trials was performed. The primary outcome measure in terms of patient satisfaction and the secondary outcome measures that consisted of complication rate, pain score, functional outcome score and success rate were evaluated. The Downs & Black checklist and the Coleman methodology scale were used to assess the methodological quality of included articles.
Results
Of 1090 reviewed articles, 23 met the inclusion criteria. The included studies reported on the results of 1285 procedures in 1177 patients. The surgical techniques were divided into five categories. Eleven studies evaluated open surgical debridement, seven studies described minimally invasive procedures, three studies evaluated endoscopic procedures, one study evaluated open gastrocnemius lengthening, and one study reported on open autologous tendon transfer. Results regarding patient satisfaction (69–100 %) and complication rate (0–85.7 %) varied widely.
Conclusions
This study demonstrates the large variation in surgical techniques available for treatment of midportion Achilles tendinopathy. None of the included studies compared surgical intervention with nonsurgical or placebo intervention. Minimally invasive and endoscopic procedures yield lower complication rates with similar patient satisfaction in comparison with open procedures. Minimally invasive and endoscopic procedures might therefore prove to be the future of surgical treatment of Achilles midportion tendinopathy.
Level of evidence
IV.
Keywords: Midportion Achilles tendinopathy, Endoscopic surgery, Minimally invasive surgery, Open surgery, Tenotomies
Introduction
Midportion Achilles tendinopathy is a painful condition of the Achilles tendon located 2–7 cm proximal to the insertion on the calcaneus. Symptoms include pain, swelling and impaired performance. It is an over-use injury, often seen in athletes. The incidence varies from 0.2 % in the general population up to 9 % in recreational runners [12, 17].
Initially, treatment of midportion tendinopathy is nonsurgical. Various noninvasive treatment options have been described, including eccentric exercise, the use of orthoses and rest. Additionally, invasive nonsurgical techniques like extracorporeal shockwave therapy and platelet-rich plasma (PRP) injection are commonly used [39]. In approximately 25 % of the patients nonsurgical treatment fails to alleviate symptoms and surgical treatment is indicated [14].
Historically, surgical treatment was performed using an open procedure [13, 26, 32]. With new insights into the aetiology of tendinopathy, new surgical procedures were developed, resulting in a large variety of surgical techniques [19, 34]. Because of the high complication rates in open procedures, less invasive techniques gained popularity [16, 24, 29, 37].
Due to the variety of surgical techniques and the confusing terminology used to describe pathologies of the Achilles tendon, no study to date has provided a clear overview of the literature regarding the best surgical treatment for midportion Achilles tendinopathy. The aim of this study is to systematically evaluate the available literature on surgical treatment for midportion Achilles tendinopathy and to provide an overview of the different surgical techniques in terms of patient satisfaction and complication rate.
Materials and methods
Search strategy
A systematic review of the literature was performed. In collaboration with a clinical librarian, the databases of MEDLINE, EMBASE and the Cochrane database for controlled trials were searched (Fig. 1).
Fig. 1.
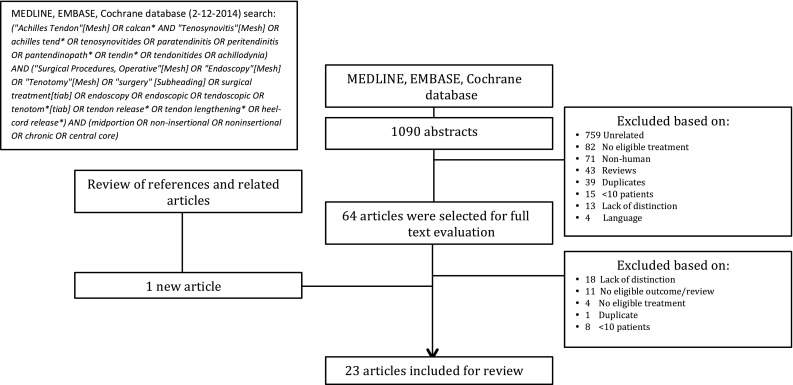
Search strategy
Inclusion criteria
Studies reporting on the results of surgical treatment for midportion Achilles tendinopathy in humans were included. In this study, the definition of midportion Achilles tendinopathy as described by van Dijk et al. [8] is used. Midportion Achilles tendinopathy is defined as symptoms of pain, swelling and impaired performance in combination with a histopathological diagnosis that includes, but is not limited to, the diagnosis of tendinosis 2–7 cm from the calcaneal insertion. Studies were eligible if they assessed the outcome measures of patient satisfaction or complication rate. Reviews and studies reporting on less than ten patients were excluded. Only studies written in English, French or German were considered eligible. Studies lacking clear distinction between midportion and insertional Achilles tendinopathy were excluded. Two authors (TB & RZ) performed title and abstract screening independently. Subsequently, these two authors individually performed full text selection. Disagreement during study selection was settled by discussion.
Data extraction
Data on patient characteristics, surgical technique and outcome were extracted. Patient satisfaction was the primary outcome measure. Secondary outcome measures consisted of complication rate, functional outcome scores, pain scores and success rate. Complications were divided in minor and major (Table 1). Successful treatment was defined as an excellent or good outcome, or when patients were satisfied with the result.
Table 1.
Classification of complications
| Complications | |
|---|---|
| Major | Minor |
| AT rupture | Discomfort |
| Any reoperation | Superficial infections |
| Deep venous thrombosis | Minor wound problems |
| Reflex dystrophy | Scar tenderness/hypertrophy |
| Persisting neuralgia | Mild form of paraesthesia |
| Deep infections/major wound problems | Prolonged hospitalisation |
Methodological quality
Methodological quality of included studies was assessed using the Downs & Black checklist and the Coleman methodology scale [7, 9]. The Downs & Black checklist was designed to evaluate the methodological quality of randomised and nonrandomised studies. It consists of a 27-item checklist with a highest possible score of 33 points. The Coleman methodology scale was designed to evaluate the methodological quality of studies on Achilles tendinopathies. The checklist consists of two parts and has a maximum possible score of 100 points. Two authors (TB & JW) assessed the included studies independently on methodological quality. Correlations between success rate and both the Coleman scale and Downs & Black checklist were calculated.
Data presentation and statistical analysis
Due to the heterogeneity of the data, results were not pooled. Outcome data were presented per study. Ranges of outcome were reported per type of surgical procedure. To calculate the correlations of nonparametric data, the Spearman’s rho correlation coefficient was used. Correlation with a p value <0.05 was considered significant.
Results
After removal of duplicates, the search yielded 1090 articles. Based on title and abstract screening, 1026 articles were excluded (Fig. 1). The remaining 64 articles were eligible for full text evaluation. Forty-two articles were excluded after full text selection. Finally, after screening references of included articles and the related literature, one article was added [6]. A total of 23 studies were included in this study (Table 2; Appendix 1 in Table 5) [1–4, 6, 10, 11, 13, 15, 18, 20–24, 26–31, 33, 36].
Table 2.
Overview of included studies
| Study | N patients (N tendons) | Surgical technique | Coleman | D&B |
|---|---|---|---|---|
| Open debridement | ||||
| Benazzo et al. [4] | A. 20 (20) | A. Open surgery: multiple longitudinal tenotomies and excision degenerations | 54 | 22 |
| B. 32 (32) | B. Open surgery: excision degeneration + soleus fibres transfer | |||
| Johnston et al. [11] | A. 10 (10) | A. Open surgery: excision inflamed paratenon and decompression AT | 29 | 7 |
| B. 7 (7) | B. Open surgery: excision inflamed paratenon, decompression AT + debridement degenerations | |||
| Kvist and Kvist [13] | 182 (201) | Open surgery: removal adhesions between paratenon, crural fascia and skin + excision thickened paratenon | 27 | 14 |
| Lohrer and Nauck [15] | A. 11 (15) | A. Open surgery: release AT + transachillear scarification | 60 | 23 |
| B. 23 (24) | B. Open surgery: release AT + excision intratendinous lesions + transachillear scarification | |||
| Maffulli et al. [18] | 10 (10) | Open surgery: excision paratenon, multiple longitudinal tenotomies and excision of degenerations | 39 | 10 |
| Maffulli et al. [21] | 86 (86) | Open surgery: excision paratenon, multiple longitudinal tenotomies + excision degenerations | 69 | 14 |
| Nelen et al. [26] | A. (93) | A. Open surgery: release AT (not ventrally) + excision inflamed paratenon | 42 | 16 |
| B. (26) | B. Open surgery: debridement tendinosis | |||
| C. (24) | C. Open surgery: debridement tendinosis (reinforcement with turned-down tendon flap) | |||
| Ohberg et al. [27] | 24 (24) | Open surgery: excision hypertrophic paratenon and debridement of degenerations through a longitudinal incision | 52 | 15 |
| Paavola et al. [29] | A. 171 (171) | A. Open surgery: excision adhesions between crural fascia and paratenon | 24 | 9 |
| B. 50 (50) | B. Open surgery: debridement intratendinous lesions | |||
| Paavola et al. [28] | A. 16 (16) | A. Open surgery: excision adhesions between crural fascia and paratenon | 56 | 14 |
| B. 26 (26) | B. Open surgery: excision adhesions between crural fascia and paratenon + debridement intratendinous lesions | |||
| Sarimo and Orava [31] | 24 (24) | Open surgery: fascial adhesiolysis and radiofrequency microtenotomy | 36 | 20 |
| Minimally invasive tendon stripping/tenotomies | ||||
| Alfredson et al. [2] | 10 (10) | Minimally invasive: US–CD-guided release ventral AT | 48 | 17 |
| Alfredson [1]a | A. 15 (18) | A. Minimally invasive: US–CD-guided release ventral AT | 41 | 17 |
| B. 16 (19) | B. Minimally invasive: US–CD-guided release ventral AT by use of a needle | |||
| Alfredson [1]a | 72 (88) | Minimally invasive: US–CD-guided release ventral AT | 30 | 14 |
| Alfredson et al. [3] | 13 (13) | Minimally invasive: US–CD-guided release ventral AT | 46 | 17 |
| Calder et al. [6] | 32 (34) | Minimally invasive: Release AT and excision plantaris tendon | 59 | 21 |
| Maffulli et al. [20] | 39 (39) | Minimally invasive: multiple percutaneous longitudinal tenotomies | 59 | 20 |
| Naidu et al. [24] | 26 (29) | Minimally invasive: circumferential AT release with a tracheal hook + peritendinous infusion of corticosteroids | 40 | 17 |
| Testa et al. [36] | 63 (63) | Minimally invasive: multiple US-guided percutaneous longitudinal tenotomies | 65 | 20 |
| Endoscopic procedures | ||||
| Maquirriain [22] | 24 (27) | Endoscopic: debridement paratenon + two longitudinal tenotomies | 52 | 13 |
| Pearce et al. [30] | 11 (11) | Endoscopic: debridement paratenon + release of plantaris tendon | 60 | 13 |
| Steenstra and van Dijk [33] | 16 (16) | Endoscopic: debridement paratenon + release of plantaris tendon | 26 | 11 |
| Open surgery: gastrocnemius lengthening | ||||
| Duthon et al. [10] | 13 (15) | Open surgery: gastrocnemius lengthening | 65 | 15 |
| Open surgery: autologous tendon transfer | ||||
| Martin et al. [23] | 44 (44) | Open surgery: excision AT + FHL transfer | 54 | 21 |
Outlined are the number of included patients; reported surgical technique; and methodological quality
AT Achilles tendon, US ultrasound, CD colour doppler
aSame study comparing release of ventral AT with knife versus needle
Table 5.
Included studies
| Study | Level of evidence | N patients (N tendons) | Gender (% F) | Mean age (years) | Duration of symptoms (months) | Mean F-U (months) | Diagnosis made by | Diagnosis | Surgical technique |
|---|---|---|---|---|---|---|---|---|---|
| Open debridement | |||||||||
| Benazzo et al. [4] | Level II | A. 20 (20) | A. 15 % | A. 41.6 ± 11.2 | A. 9.14 | A 6;.55.2 ± 14.4 | A. History + Clinical + MRI | A. Midportion Achilles tendinopathy (= intratendinous lesions) | A. Open surgery: multiple longitudinal tenotomies and excision degenerations |
| B. 32 (32) | B. 12.5 % | B. 43.2 ± 12.8 | B. 8.91 | B. 6; 47.2 ± 11.7 | B. History + Clinical + MRI | B. Midportion Achilles tendinopathy (= intratendinous lesions) | B. Open surgery: excision degeneration + soleus fibres transfer | ||
| Johnston et al. [11] | Level IV | A. 10 (10) | A. Tenosynovitis | A. Open surgery: excision inflamed paratenon and decompression AT | |||||
| B. 7 (7) | B. 48 (33–58) | B. Chronic Achilles tendonitis + tenosynovitisa | B. Open surgery: excision inflamed paratenon, decompression AT + debridement degenerations | ||||||
| Kvist and Kvist [13] | Level IV | 182 (201) | 27.5 (12–53) | 7.5 (2–120) | Calcaneal paratenonitis | Open surgery: removal adhesions between paratenon, crural fascia and skin + excision thickened paratenon | |||
| Lohrer and Nauck [15] | Level II | A. 11 (15) | A. 36.4 % | A. 48.4 (± 7.3; 39.0–58.0) | A. 3; 6; 12 | A. Clinical + US-PD + MRIa | A. Isolated midportion Achilles tendinopathy | A. Open surgery: release AT + transachilllear scarification | |
| B. 23 (24) | B. 17.4 % | B. 50.5 (± 9.9; 23–66) | B. 3; 6; 12 | B. Clinical + US-PD + MRIa | B. Midportion Achilles tendinopathy + central core lesions | B. Open surgery: release AT + excision intratendinous lesions + transachillear scarification | |||
| Maffulli et al. [18] | Level IV | 10 (10) | 20 % | 34.8 (21–52) | 87 (27–178) | 35 (27–52) | Clinical + MRIa + USa + CTa | Achilles tendinopathy with central core degeneration, 2–6 cm area | Open surgery: excision paratenon, multiple longitudinal tenotomies and excision of degenerations |
| Maffulli et al. [21] | Level III | 86 (86) | 47.7 % | 25.3 (12–52) | 39.6 (30–60) | Clinical + US + Histological | Tendinopathy of the main body, 2–6 cm area | Open surgery: excision paratenon, multiple longitudinal tenotomies + excision degenerations | |
| Nelen et al. [26] | Level IV | A. (93) | A. Peritendinitis | A. Open surgery: release AT (not ventrally) + excision inflamed paratenon | |||||
| B. (26) | B. Tendinosis | B. Open surgery: debridement tendinosis | |||||||
| C. (24) | C. Extensive tendinosis | C. Open surgery: debridement tendinosis (reinforcement with turned-down tendon flap) | |||||||
| Ohberg et al. [27] | Level IV | 24 (24) | 29.2 % | 43 (26–54) | >6 | 60 (31–82) | History + Clinical + US | Tendinosis, 2–6 cm level | Open surgery: excision hypertrophic paratenon and debridement of degenerations through a longitudinal incision. |
| Paavola et al. [29] | Level IV | A. 171 (171) | A. >3 | A. 0.5; 1; 2.5; 12 (N = 28) | A. History + Clinical + USa | A. Peritendinitis | A. Open surgery: excision adhesions between crural fascia and paratenon | ||
| B. 50 (50) | B. >3 | B. 0.5; 1; 2.5; 12 (N = 28) | B. History + Clinical + USa | B. Tendinosis | B. Open surgery: debridement intratendinous lesions | ||||
| Paavola et al. [28] | Level IV | A. 16 (16) | A. 25 % | A. 37 (±12) | A. 7 | A. History + Clinical + MRIa + USa | A. Tendinopathy: peritendinous adhesions | A. Open surgery: excision adhesions between crural fascia and paratenon | |
| B. 26 (26) | B. 34.6 % | B. 46 (±14) | B. 7 | B. History + Clinical + MRIa + USa | B. Tendinopathy: peritendinous adhesions + localised intratendinous lesion | B. Open surgery: excision adhesions between crural fascia and paratenon + debridement intratendinous lesions | |||
| Sarimo and Orava [31] | Level IV | 24 (24) | 50 % | 54 (39–72) | 14 (6–28) | 30 (18–45) | History + Clinical + US | Chronic midportion Achilles tendinopathy | Open surgery: fascial adhesiolysis and radiofrequency microtenotomy |
| Minimally invasive tendon stripping/tenotomies | |||||||||
| Alfredson et al. [2] | Level I | 10 (10) | 40 % | 45.2 | 23(6–60) | 3; 6 | Clinical + US–CD | Chronic painful midportion Achilles tendinosis | Minimally invasive: US–CD-guided release ventral AT |
| Alfredson [1]b | Level I | A. 15 (18) | A. 33.3 % | A. 46 (31–67) | A. 74 (7–240) | A. Clinical + US–CD | A. Midportion Achilles tendinosis | A. Minimally invasive: US–CD-guided release ventral AT. | |
| B. 16 (19) | B. 37.5 % | B. 47 (31–76) | B. 82 (5–240) | B. Clinical + US–CD | B. Midportion Achilles tendinosis | B. Minimally invasive: US–CD-guided release ventral AT by use of a needle. | |||
| Alfredson [1]b | Level IV | 72 (88) | 36.1 % | >3 | Clinical + US–CD | Midportion Achilles tendinosis | Minimally invasive: US–CD-guided release ventral AT. | ||
| Alfredson et al. [3] | Level IV | 13 (13) | 46.2 % | 53 (34–70) | >6 | 6 | Clinical + US–CD | Midportion Achilles tendinopathy | Minimally invasive: US–CD-guided release ventral AT. |
| Calder et al. [6] | Level IV | 32 (34) | 31.3 % | 27.2 (19–42) | 22.1 (12–48) | Clinical + MRI | Noninsertional Achilles tendinopathy (= paratendinitis + tendinosisa) | Minimally invasive: release AT and excision plantaris tendon | |
| Maffulli et al. [20] | Level IV | 39 (39) | 23.1 % | 45 (34–63) | 13 (6–55) | 204 (180–264) | Clinical + US | Midportion Achilles tendinopathy + paratendinopathya | Minimally invasive: multiple percutaneous longitudinal tenotomies |
| Naidu et al. [24] | Level IV | 26 (29) | 68.8 % | 53 (38–66) | 13 (6–31) | Clinical + radiograph + MRIa + USa | Noninsertional Achilles tendinopathy | Minimally invasive: circumferential AT release with a tracheal hook + peritendinous infusion of corticosteroids | |
| Testa et al. [36] | Level IV | 63 (63) | 51 (±8.2) | History + Clinical + MRIa + US | Chronic Achilles tendinopathy + paratendinopathya | Minimally invasive: multiple US-guided percutaneous longitudinal tenotomies | |||
| Endoscopic procedures | |||||||||
| Maquirriain [22] | Level IV | 24 (27) | 50 % | 45.5 (±8.9) | >6 | 92.4 (60–168) | History + Clinical + MRI | Chronic midportion Achilles tendinopathy | Endoscopic debridement paratenon + two longitudinal tenotomies |
| Pearce et al. [30] | Level IV | 11 (11) | 36.5 (24–55) | 13 (3–36) | 30 (24–39) | Clinical + MRIa + USa | Noninsertional tendinopathy (= paratendinopathy + intratendinous disease) | Endoscopic debridement paratenon + release of plantaris tendon | |
| Steenstra and van Dijk [33] | Level IV | 16 (16) | >24 | 72 (24–84) | Noninsertional tendinopathy + paratendinopathy. | Endoscopic debridement paratenon + release of plantaris tendon | |||
| Open surgery: gastrocnemius recession | |||||||||
| Duthon et al. [10] | Level IV | 13 (15) | 23.1 % | 12; 24 | History + Clinical + MRIa | Noninsertional Achilles tendinopathy (= peritendonitis + tendinosis) | Open surgery: gastrocnemius recession | ||
| Open surgery: autologous tendon transfer | |||||||||
| Martin et al. [23] | Level IV | 44 (44) | 59 % | 58.2 (±10.1) | 40.8 (±22.8) | Clinical + Radiograph + MRI | Chronic degenerative Achilles tendinosis, 2–6 cm area | Open surgery: excision AT + FHL transfer | |
Outlined are level of evidence; patient demographics; duration of follow-up (F-U); reported surgical technique and methodological quality
AT Achilles tendon, US ultrasound, CD color doppler
aOnly in percentage of patients
bSame study comparing release of ventral AT with knife versus needle
Population characteristics
The studies reported on a total of 1177 patients with 1285 affected tendons. 62.7 % of the patients was male. Seven studies did not report on gender distribution [11, 13, 26, 29, 30, 33, 36]. The weighted mean age was 40.2 years. The remaining seven studies did not adequately report on age [1, 10, 21, 26, 29, 33, 36].
Surgical techniques
In this review, the techniques were roughly grouped into five types of procedures. Eleven studies reported open techniques as treatment of midportion Achilles tendinopathy [4, 11, 13, 15, 18, 21, 26–29, 31]. Seven studies evaluated minimally invasive procedures [1–3, 6, 20, 24, 36]. Three studies reported on endoscopic techniques [22, 30, 33], one study evaluated gastrocnemius lengthening by an open procedure [10], and one reported on a technique for open resection of the distal Achilles tendon, followed by interposition of FHL graft [23]. Techniques were classified as minimally invasive based on descriptions in the studies. In six of the included studies reporting minimally invasive techniques, incisions were smaller than 2 cm (Appendix 2 in Table 6).
Table 6.
Surgical techniques
| N of procedures | N of surgeons | Position | Approach | Description | |
|---|---|---|---|---|---|
| Open debridement | |||||
| Benazzo et al. [4] | A. 20 | A. 1 | A. Prone | A. Lateral longitudinal incision | A. Two–three longitudinal tenotomies and excision of degenerated areas (not sutured) |
| B. 32 | B. 2 | B. Prone | B. Lateral longitudinal incision | B. Excision of the degenerations through a longitudinal tenotomy after which a muscle bundle of the soleus muscle was bluntly dissected and distally left attached. The proximal end of the muscle bundle was anchored into the longitudinal incision with absorbable sutures | |
| Johnston et al. [11] | A. 10 | A. Medial longitudinal incision | A. Resection of thickened peritenon after which a one cm portion was resected and the AT was decompressed | ||
| B. 7 | B. Medial longitudinal incision | B. Resection of thickened peritenon after which a one cm portion was resected. If the AT was thickened or swollen, a longitudinal incision was made and degenerations were debrided | |||
| Kvist and Kvist [13] | 201 | Prone | Lateral incision (7 cm) | Fascial incision, after which adhesions between the paratenon and crural fascia and the crural fascia and the skin were removed. Thickened paratenon was excised (not sutured) | |
| Lohrer and Nauck [15] | A. 15 | A. 1 | A. Transverse incision (4 cm) + s.o.s. expanded longitudinally medial or lateral, creating a Z- or L-shape | A. The AT was released, after which transachillear scarification, parallel to the fibres, was performed with a surgical scalpel | |
| B. 24 | B. 1 | B. Transverse incision (4 cm) + s.o.s. expanded longitudinally medial or lateral, creating a Z- or L-shape | B. The AT was released, after which a longitudinal incision was made to excise degenerated lesions. The AT was reconstructed with sutures. With a surgical scalpel transachillear scarification was performed, parallel to the fibres | ||
| Maffulli et al. [18] | 10 | 1 | Prone | Medial longitudinal incision | The paratenon was excised and suspicious areas were explored by three–five longitudinal tenotomies and degenerations were excised (not sutured) |
| Maffulli et al. [21] | 86 | Prone | Medial or lateral curvilinear longitudinal incision (10-12 cm) | The paratenon was excised and suspicious areas were explored by three–five longitudinal tenotomies and degenerations were excised (not sutured) | |
| Nelen et al. [26] | A. 93 | A. Medial longitudinal incision | A. Incision of crural fascia and paratenon, after which the medial, lateral and dorsal aspect of the AT were released (no circular dissection, ventral side AT left untouched). Hypertrophic paratenon was excised | ||
| B. 26 | B. Medial longitudinal incision | B. Debridement tendinosis (sutured side to side) | |||
| C. 24 | C. Medial longitudinal incision | C. Extensive debridement tendinosis, after which the AT was reinforced with a rectangular flap of lateral or medial tendon aponeurosis, turned down on itself and sutured in the defect with resorbable sutures | |||
| Ohberg et al. [27] | 24 | Lateral longitudinal incision | Hypertrophic paratenon was excised, and a longitudinal incision was made to debride degenerations (sutured side to side) | ||
| Paavola et al. [29] | A. 171 | A. 1 | A. Prone | A. Lateral longitudinal incision | A. Fascial incision, after which adhesions between the paratenon and the crural fascia were excised |
| B. 50 | B. 1 | B. Prone | B. Lateral longitudinal incision | B. Fascial incision, after which adhesions between paratenon and crural fascia were removed and a longitudinal incision was made to excise intratendinous lesions (sutured side to side) | |
| Paavola et al. [28] | A. 16 | A. 2 | A. Prone | A. Lateral longitudinal incision | A. Fascial incision, after which adhesions between paratenon and crural fascia were removed |
| B. 26 | B. 2 | B. Prone | B. Lateral longitudinal incision | B. Fascial incision, after which adhesions between paratenon and crural fascia were removed and a longitudinal incision was made to excise intratendinous lesions (sutured side to side) | |
| Sarimo and Orava [31] | 24 | Medial or Lateral longitudinal incision (3–5 cm) | Fascial incision, after which adhesions between paratenon and crural fascia were removed and multiple radiofrequency microtenotomies were performed | ||
| Minimally invasive tendon stripping/tenotomies | |||||
| Alfredson et al. [2] | 10 | Lateral longitudinal incision | US–CD-guided dissection of the AT from the ventral soft tissue by use of a knife followed by haemostasis with diathermia | ||
| Alfredson [1]a | A. 18 | A. Prone | A. Lateral longitudinal incision (1–2 cm) | A. US–CD-guided dissection of the AT from the ventral soft tissue by use of a knife followed by haemostasis with diathermia | |
| B. 19 | B. Prone | B. Medial or lateral needle insertion | B. US–CD-guided release of the AT from the ventral soft tissue by use of a needle | ||
| Alfredson [1]a | 88 | Prone | Lateral longitudinal incision (1–2 cm) | US–CD-guided dissection of the AT from the ventral soft tissue by use of a knife, followed by haemostasis with diathermia | |
| Alfredson et al. [3] | 13 | Medial longitudinal incision (1–2 cm) | US–CD-guided dissection of the AT from the ventral soft tissue by use of a knife followed by haemostasis with diathermia | ||
| Calder et al. [6] | 34 | Medial incision (2–3 cm) | Release of the AT, after which the plantaris tendon was released from the AT and transected distally. The proximal end of the plantaris tendon is sectioned at the musculo-tendinous junction and delivered through a stab incision | ||
| Maffulli et al. [20] | 39 | 1 | Prone | Five stab incisions: 2 medial; 1 central; 2 lateral | Multiple US-guided percutaneous longitudinal tenotomies were created through five stab incisions |
| Naidu et al. [24] | 29 | Prone | Midline longitudinal incision (1–2 cm) | A blunt tracheal hook was passed up and down the AT to perform adhesiolysis. After closure of the paratenon, corticosteroids were infused peritendinously | |
| Testa et al. [36] | 63 | Prone | Stab incision central over degeneration | Adhesiolysis by 0.5 % carbocaine infiltration. Next, six US-guided percutaneous longitudinal tenotomies through one incision, three up- and three downwards, varying 45° were performed | |
| Endoscopic procedures | |||||
| Maquirriain [22] | 27 | 1 | Prone | Two midline portals | Endoscopic debridement of paratenon and release of the crural fascia were performed. Thereafter, two longitudinal tenotomies were performed |
| Pearce et al. [30] | 11 | Prone | Proximal portal medial + distal portal lateral | Endoscopic debridement of paratenon and release of the plantaris tendon were performed | |
| Steenstra and van Dijk [33] | 16 | Prone | Proximal portal medial + distal portal lateral | Endoscopic debridement of paratenon and release of the plantaris tendon were performed | |
| Open surgery: gastrocnemius lengthening | |||||
| Duthon et al. [10] | 15 | 1 | Supine | Medial incision (5 cm) | The gastrocnemius muscle was separated from the soleus muscle by blunt dissection after which the gastrocnemius muscle was cut transversally (not sutured) |
| Open surgery: autologous tendon transfer | |||||
| Martin et al. [23] | 44 | Supine | Medial longitudinal incision (10 cm) | The distal four–six cm of the AT was excised after which the FHL was harvested and interpositioned (secured proximally with a Pulvertaft weave, distally a tunnel is drilled in the calcaneus and the FHL is secured with an interference screw or reflected onto self and sutured) | |
Outlined are number of procedures; number of involved surgeons; positioning; approach and used surgical technique
AT Achilles tendon, US ultrasound, CD color doppler
aSame study comparing release of ventral AT with knife versus needle
Open surgery
Eleven studies described the outcome of an open surgical approach [4, 11, 13, 15, 18, 21, 26–29, 31]. There is a large variation in techniques; however, each technique consisted of the release of the tendon (adhesiolysis, release or excision of the paratenon), debridement of degenerative tissue, longitudinal tenotomies or a combination of these (Table 2; Appendix 2 in Table 6). Four studies compared the results of release of the tendon with or without tenotomies, with a group of patients that additionally underwent debridement of degenerative tissue [11, 15, 28, 29]. One compared the results between a group of patients that underwent debridement without suturing or augmentation with a group in which the tendon was augmented using fibres of the soleus muscle [4]. In another study, three groups were distinguished: no debridement of the tendon was performed in group A. Group B and C consisted of patients with tendinosis and extensive tendinosis. Both groups were treated by excision of degenerations, followed by side-to-side suture for patients in group B or reconstruction with a turndown flap in group C [26].
None of the studies reported on patient satisfaction (Table 3). Complication rates were adequately reported in eight studies and ranged from 0 up to 85.7 % (Table 3) [4, 11, 13, 18, 21, 27, 29, 31]. Success rates varied from 73.1 up to 100 % (Table 4) [13, 15, 26–28, 31].
Table 3.
Patient satisfaction and complication rate
| Study | Postoperative satisfaction | Complications | ||||
|---|---|---|---|---|---|---|
| Satisfied | Unsatisfied | Major | Minor | Total | Reoperations | |
| Open debridement | ||||||
| Benazzo et al. [4] | A. 1/20 (5 %) | A. 2/20 (10 %) | A. 3/20 (15 %) | A. 1/20 (5 %) | ||
| B. 1/32 (3.1 %) | B. 3/32 (9.4 %) | B. 4/32 (12.5 %) | B. 1/32 (3.1 %) | |||
| Johnston et al. [11] | 0/17 (0 %) | 0/17 (0 %) | 0/17 (0 %) | |||
| Kvist and Kvist [13] | 20/201 (10.0 %) | 2/201 (1.0 %) | 22/201 (10.9 %) | 20/201 (10.0 %) | ||
| Lohrer and Nauck [15] | ||||||
| Maffulli et al. [18] | 6/14 (42.9 %) | 6/14 (42.9 %) | 12/14 (85.7 %) | 6/14 (42.9 %) | ||
| Maffulli et al. [21] | 8/86 (9.3 %) | 23/86 (26.7 %) | 31/86 (36.0 %) | 8/86 (9.3 %) | ||
| Nelen et al. [26] | A+B+C. 12/143 (8.4 %) | A+B+C. 2/143 (1.4 %) | A+B+C. 14/143 (9.8 %) | A. 4/93 (4.3 %) | ||
| B. 1/26 (3.8 %) | ||||||
| C. 0/24 (0 %) | ||||||
| Ohberg et al. [27] | 0/24 (0 %) | 2/24 (8.3 %) | 2/24 (8.3 %) | 0/24 (0 %) | ||
| Paavola et al. [29] | A. 9/171 (5.3 %) | A.18/171 (10.5 %) | A. 27/171 (15.8 %) | A. 9/171 (5.3 %) | ||
| B. 0/50 (0 %) | B. 1/50 (2 %) | B. 1/50 (2 %) | B. 0/50 (0 %) | |||
| Paavola et al. [28] | A+B. 2/42 (4.8 %) | A+B. 6/42 (14.3 %) | A+B. 8/42 (19.1 %) | A+B. 2/42 (4.8 %) | ||
| Sarimo and Orava [31] | 1/24 (4.2 %) | 1/24 (4.2 %) | 2/24 (8.3 %) | |||
| Totals | 60/824 (7.3 %) | 66/824 (8.0 %) | 126/824 (15.3 %) | |||
| Minimally invasive tendon stripping/tenotomies | ||||||
| Alfredson et al. [2] | 10/10 (100 %) | 1/10 (10 %) | 0/10 (0 %) | 1/10 (10 %) | ||
| Alfredson [1]a | A. 15/18 (83.3 %)b | A. 3/18 (16.7 %)b | A+B. 3/37 (8.1 %) | A+B. 0/37 (0 %) | A+B. 3/37 (8.1 %) | |
| B. 15/19 (78.9 %)b | B. 4/19 (21.1 %)b | |||||
| Alfredson [1]a | 81/88 (92.0 %)b | 7/88 (8.0 %)b | ||||
| Alfredson et al. [3] | 11/13 (84.6 %) | 2/13 (15.4 %) | ||||
| Calder et al. [6] | 22/32 (69 %)c | 10/32 (31 %)c | 0/34 (0 %) | 1/34 (2.9 %) | 1/34 (2.9 %) | |
| Maffulli et al. [20] | ||||||
| Naidu et al. [24] | 24/26 (92 %)c | 2/26 (7.7 %)c | 1/29 (3.4 %) | 2/29 (6.9 %) | 3/29 (10.3 %) | 1/29 (3.4 %) |
| Testa et al. [36] | 9/75 (12 %) | 14/75 (18.6 %) | 23/75 (30.6 %) | 9/75 (12 %) | ||
| Totals | 14/185 (7.6 %) | 17/185(9.2 %) | 31/185 (16.8 %) | |||
| Endoscopic procedures | ||||||
| Maquirriain [22] | 2/27 (7.4 %) | 0/27 (0 %) | 2/27 (7.4 %) | |||
| Pearce et al. [30] | 8/11 (73 %) | 3/11 (27 %) | 0/11 (0 %) | 0/11 (0 %) | 0/11 (0 %) | 0/11 (0 %) |
| Steenstra and van Dijk [33] | 0/20 (0 %) | 0/20 (0 %) | 0/20 (0 %) | |||
| Totals | 2/58 (3.4 %) | 0/58 (0 %) | 2/58 (3.4 %) | |||
| Open surgery: gastrocnemius lengthening | ||||||
| Duthon et al. [10] | 12/13 (92.3 %)c | 1/13 (7.7 %)c | 0/15 (0 %) | 0/15 (0 %) | 0/15 (0 %) | |
| Open surgery: autologous tendon transfer | ||||||
| Martin et al. [23] | 37/44 (86 %) | 6/44 (13.8 %) | 1/44 (2.3 %) | 4/44 (9.1 %) | 5/44 (11.4 %) | |
aSame study comparing release of ventral AT with knife versus needle
bStudy includes patients who received bilateral surgical treatment; outcome reported on individual tendons
cStudy included patients who received bilateral surgical treatment; outcome reported on patient level
Table 4.
Success rate
| Study | Success rate | |
|---|---|---|
| Successful | Unsuccessful | |
| Open debridement | ||
| Benazzo et al. [4] | ||
| Johnston et al. [11] | ||
| Kvist and Kvist [13]b | 194/201 (96.5 %) | 7/201 (3.5 %) |
| Lohrer and Nauck [15]b | 15/15 (100 %) | |
| 23/24 (95.8 %) | 1 (4.2 %) | |
| Maffulli et al. [18] | ||
| Maffulli et al. [21] | ||
| Nelen et al. [26]b | A. 82/93 (88.2 %) | A. 11/93 (11.8 %) |
| B. 19/26 (73.1 %) | B. 7/26 (26.9 %) | |
| C. 21/24 (87.5 %) | C. 3/24 (12.5 %) | |
| Ohberg et al. [27] | 22/24 (91.7 %) | 2/24 (8.3 %) |
| Paavola et al. [29] | ||
| Paavola et al. [28] | A. 16/16 (100 %) | |
| B. 19/26 (73.1 %) | B. 7/26 (26.9 %) | |
| Sarimo and Orava [31] | 24/24 (100 %) | |
| Minimally invasive tendon stripping/tenotomies | ||
| Alfredson et al. [2] | 10/10 (100 %) | |
| Alfredson [1]a,b | A. 15/18 (83.3 %) | A. 3/18 (16.7 %) |
| B. 15/19 (78.9 %) | B. 4/19 (21.1 %) | |
| Alfredson [1]a,b | 81/88 (92.0 %) | 7/88 (8.0 %) |
| Alfredson et al. [3] | 11/13 (84.6 %) | 2/13 (15.4 %) |
| Calder et al. [6]c | 22/32 (69 %) | 10/32 (31 %) |
| Maffulli et al. [20] | 30/39 (76.9 %) | 9/39 (23.1 %) |
| Naidu et al. [24]c | 24/26 (92 %) | 2/26 (7.7 %) |
| Testa et al. [36] | 47/63 (74.6 %) | 16/63 (25.4 %) |
| Endoscopic procedures | ||
| Maquirriain [22]c | 24/24 (100 %) | |
| Pearce et al. [30] | 8/11 (73 %) | 3/11 (27 %) |
| Steenstra and van Dijk [33] | ||
| Open surgery: gastrocnemius lengthening | ||
| Duthon et al. [10]c | 12/13 (92.3 %) | 1/13 (7.7 %) |
| Open surgery: autologous tendon transfer | ||
| Martin et al. [23] | 37/44 (86 %) | 6/44 (13.8 %) |
aSame study comparing release of ventral AT with knife versus needle
bStudy includes patients who received bilateral surgical treatment; outcome reported on individual tendons
cStudy included patients who received bilateral surgical treatment; outcome reported on patient level
Minimally invasive tendon stripping/tenotomies
Minimally invasive procedures were described in seven included studies [1–3, 6, 20, 24, 36]. Five articles described a technique to perform a release of the Achilles tendon [1–3, 6, 24] with additional excision of the plantaris tendon in one study [6]. The other two minimally invasive techniques described aimed to perform percutaneous longitudinal tenotomies with additional release of adhesions by infiltration performed in one study (Table 2, Appendix 2 in Table 6) [20, 36].
Patient satisfaction was reported in five studies and ranged from 69 up to 100 % (Table 3). [1–3, 6, 24]. Complications rates were adequately reported in four studies, ranging from 2.9 up to 30.6 % (Table 3) [2, 6, 24, 36]. Success rates varied from 69 up to 100 % (Table 4) [1–3, 6, 20, 24, 36].
Endoscopic procedures
Three studies reported on the outcome of endoscopic procedures [22, 30, 33]. In all procedures, debridement of the paratenon was performed, with additional release of the plantaris tendon in two studies [30, 33] and additional longitudinal tenotomies in one study [22] (Table 2, Appendix 2 in Table 6).
Only one study reported on patient satisfaction; in this study 73 % of patients was satisfied (Table 3) [30]. Complications rates varied from 0 to 7.4 % (Table 3) [22, 30, 33]. Success rates varied from 73 up to 100 % (Table 4) [22, 30].
Open surgery: gastrocnemius lengthening
One study evaluated gastrocnemius lengthening through an open procedure (Table 2, Appendix 2 in Table 6) [10]. Using this technique, a satisfaction rate of 92.3 % was achieved in combination with 0 % complications (Table 3). A success rate of 92.3 % was achieved (Table 4).
Open surgery: autologous tendon transfer
One study reported on autologous tendon transfer [23]. The technique consisted of resection of the distal Achilles tendon, followed by interposition of the flexor hallucis longus (FHL) tendon (Table 2, Appendix 2 in Table 6).
The study reported that patient satisfaction was achieved in 86 % of the patients (Table 3). Complications occurred in 11.4 % of the patients (Table 3). A success rate of 86 % was achieved (Table 4).
Methodological quality
The assessment of the methodological quality using the Downs & Black checklist and the Coleman methodological scale resulted in a median score of 12.0 (IQR 10.0–13.25) and 57.5 (IQR 40.0–64.25), respectively (Table 2).
There was no significant correlation between success rate and both Coleman score and Downs & Black score. However, a significant positive correlation was found between year of publication and Coleman score (rho: 0.53, p < 0.01), and year of publication and Downs & Black score (rho 0.66, p < 0.01).
Discussion
The most important finding of the present study is the large variation in surgical techniques available for the treatment of midportion Achilles tendinopathy. Additionally, it demonstrates that minimally invasive and endoscopic procedures have lower complication rates with comparable patient satisfaction in comparison with open procedures. Due to low methodological quality of included studies in combination with large heterogeneity in population, used techniques and reported outcome measures, we refrained from data pooling.
Hitherto, one review evaluating surgical treatment of Achilles tendinopathy was performed [35]. In this study from 2001 a mean success rate of 77.4 % was reported [35]. Additionally, a negative correlation between success rate and methodological quality in studies on the topic of surgical treatment of tendinopathy was established [35]. In contrast to that review, we found no correlation between effectiveness and methodological quality. However, we found a positive correlation between year of publication and Coleman score, in line with a previous review on insertional tendinopathy [38]. This implicates that in current research on Achilles tendinopathy the methodological quality is improving.
Studies on open surgery reported inconsistent results regarding patient satisfaction and the complication rates varied widely. Particularly high complication rates were observed in studies evaluating the outcome of multiple tenotomies via an open procedure [4, 18, 21].
In general, good results regarding patient satisfaction and complication rates were reported in studies on minimally invasive surgery. Most of these studies reported on minimally invasive release of the Achilles tendon or minimally invasive longitudinal tenotomies of the Achilles tendon. One study evaluated the results of excision of the plantaris tendon [6]. In this study promising results were reported. However, more studies are needed to support these findings.
Minimally invasive procedures are assumed to have lower complication rates. Most studies evaluating minimally invasive techniques reported low complication rates (Table 3). However, a particularly high complication rate was observed in the study evaluating multiple percutaneous tenotomies [36].
Excellent results regarding functional outcome and postoperative pain were reported in three small series on endoscopic surgery. There were significant differences in the evaluated endoscopic procedures. Maquirriain et al. [22] reported the results of multiple endoscopic longitudinal tenotomies where in the other studies endoscopic release of the Achilles tendon in combination with release of the plantaris tendon was evaluated [30, 33]. Compared to the study by Pearce et al. a higher complication rate was observed in this study.
One study evaluating the results of gastrocnemius lengthening was included in this review [10]. Although promising results are reported, the study evaluated a mere 13 patients at final follow-up. A recent study reported less promising results regarding self-reported sport function in patients treated for Achilles tendinopathy with gastrocnemius lengthening [25].
One study on FHL transfer was included [23]. Good results were reported; however, a high complication rate was observed. The included retrospective case series reported on 44 patients with a mean age of 58.2 years. However, patients affected by midportion tendinopathy tend to be younger, and a wish for return to high-level sport is often present.
The most important limitation of this review is the limited level of evidence of included articles resulting in a high risk of bias. In addition, the lack of or incomplete reportage of our primary and secondary outcome measures made for an arduous comparison. In addition, the included studies used a large variety of heterogeneous outcome measures to measure functional outcome and pain. Therefore, caution should be taken when interpreting the results presented in this review. Another limitation is the confusing terminology used to describe the various pathological conditions of the Achilles tendon [8].
Despite the low level of evidence of the included study, this systematic review is of clinical significance [5]. This study is the first systematic review to compare surgical techniques for their effectiveness on patient satisfaction and complication rate. The study provides a comprehensive overview and clearly demonstrates the variation per surgical technique in outcome of patient satisfaction and complication rates.
We strongly encourage future studies to be conducted using validated instruments to assess pain and functional outcome. As often advocated, larger populations, prospective studies and long-term follow-up studies are needed to be conclusive on the best surgical treatment option of midportion Achilles tendinopathy.
In addition, no comparative study of surgical treatment and nonsurgical treatment or placebo intervention has been conducted. Therefore, no additional benefit of surgery over nonsurgical treatment, placebo intervention or wait-and-see policy has been established. Future research should therefore strive to compare surgical treatment with nonsurgical or placebo intervention.
Furthermore, as the exact pathophysiology of midportion tendinopathy is still poorly understood, current surgical techniques address a range of hypothetical abnormalities with varying results (Appendix 1 in Table 5). Future research should aim to determine whether the extent of the pathology influences the required surgical approach.
Conclusion
The study provides a comprehensive overview of the current literature and clearly demonstrates the variation in outcome of patient satisfaction and complication rates. None of the included studies compared surgical treatment with nonsurgical treatment or placebo intervention. However, minimally invasive and endoscopic procedures result in lower complication rates compared to open surgical procedures. Minimally invasive and endoscopic procedures might therefore prove to be the future of surgical treatment of Achilles midportion tendinopathy.
Appendix 1
See Table 5.
Appendix 2
See Table 6.
Appendix 3
See Table 7.
Table 7.
Functional outcome and pain score
| Functional outcome measures | Pain scores | Result at follow-up | ||||
|---|---|---|---|---|---|---|
| Study | Preoperative | At follow-up | Preoperative | At follow-up | Successful | Unsuccessful |
| Open debridement | ||||||
| Benazzo et al. [4] | A. AOFAS: 72.0 ± 11.6 | A. AOFAS (6 months): 93.7 ± 5.0a
(55.2 months): 89.8 ± 3.8 |
||||
| A. VISA-A: 53.4 ± 14.7 | A. VISA-A (6 months): 93.3 ± 5.3a
(55.2 months): 88.7 ± 5.4 |
|||||
| A. TEGNER: 6 ± 1.2 | A. TEGNER (55.2 months): 6 ± 0.9 | |||||
| B. AOFAS: 69.0 ± 10.2 | B. AOFAS (6 months): 98.5 ± 3.4a
(47.2 months): 95.1 ± 5.1 |
|||||
| B. VISA-A: 51.9 ± 15.4 | B. VISA-A (6 months): 96.5 ± 5.4a
(47.2 months): 94.4 ± 5.8 |
|||||
| B. TEGNER: 6 ± 1.4 | B. TEGNER (47.2 months): 6 ± 1.1 | |||||
| Johnston et al. [11] | ||||||
| Kvist and Kvist [13]d | 194/201 (96.5 %) | 7/201 (3.5 %) | ||||
| Lohrer and Nauck [15]d | A. VISA-A: 44.2 ± 5.5 (16–66) | A. VISA-A (3 months): 51.4 ± 20.4 (12–86) (6 months): 76.2 ± 18.5 (48–99)a (12 months): 86.3 ± 8.8 (73–97)a |
A. 15/15 (100 %) | |||
| B. VISA-A: 37.0 ± 17.6 (10–79) | B. VISA-A (3 months): 57.0 ± 23.2 (12–97) (6 months): 81.0 ± 15.8 (50–99)a (12 months) 90.3 ± 10.6 (62–100)a |
B. 23/24 (95.8 %) | B. 1/24 (4.2 %) | |||
| Maffulli et al. [18] | ||||||
| Maffulli et al. [21] | ||||||
| Nelen et al. [26]d | A. 82/93 (88.2 %) | A. 11/93 (11.8 %) | ||||
| B. 19/26 (73.1 %) | B. 7/26 (26.9 %) | |||||
| C. 21/24 (87.5 %) | C. 3/24 (12.5 %) | |||||
| Ohberg et al. [27] | 22/24 (91.7 %) | 2/24 (8.3 %) | ||||
| Paavola et al. [29] | ||||||
| Paavola et al. [28] | A. 16/16 (100 %) | |||||
| B. 19/26 (73.1 %) | B. 7/26 (26.9 %) | |||||
| Sarimo and Orava [31] | NPSAO 5.0 (3–7) | NPSAO: 0.7 (0–4)a | 24/24 (100 %) | |||
| VAS rest: 0 mm | ||||||
| VAS daily living: 1.4 mm (0–20 mm) | ||||||
| VAS athletic activity: 6.0 mm (0–40 mm) | ||||||
| Minimally invasive tendon stripping/tenotomies | ||||||
| Alfredson et al. [2] | VAS (3 months): 75 mm | VAS (3 months): 21 mma | 10/10 (100 %) | |||
| Alfredson [1]b,d | A. VAS AT-loading: 69 mm (40–92 mm) | A. VAS AT-loading: 6 mm (0–38 mm)a | A. 15/18 (83.3 %) | A. 3/18 (16.7 %) | ||
| B. VAS AT-loading: 75 mm (40–99 mm) | B. VAS AT-loading: 2 mm (0–15 mm)a | B. 15/19 (78.9 %) | B. 4/19 (21.1 %) | |||
| Alfredson [1]b,d | 81/88 (92.0 %) | 7/88 (8.0 %) | ||||
| Alfredson et al. [3] | VAS AT-loading: 76 mm (55–98 mm) | VAS AT-loading: 7 mm (0–23 mm) | 11/13 (84.6 %) | 2/13 (15.4 %) | ||
| Calder et al. [6]e | FAOS: 333 (321–345) | FAOS: 449 (431–468) | VAS: 58 mm (95 % CI 5.4–6.3) | VAS: 8 mm (95 % CI 0.3–1.3)a | 22/32 (69 %) | 10/32 (31 %) |
| Maffulli et al. [20] | VISA-A: 78.5 (51–94) | 30/39 (76.9 %) | 9/39 (23.1 %) | |||
| Naidu et al. [24]e | Puddu scale: 4.9/6 | Puddu scale: 1.7/6 | VAS: 87 mm | VAS: 24 mma | 24/26 (92 %) | 2/26 (7.7 %) |
| Testa et al. [36] | 47/63 (74.6 %) | 16/63 (25.4 %) | ||||
| Endoscopic procedures | ||||||
| Maquirriain [22]e | VISA-A (N = 15): 37.06 ± 4.99 | VISA-A (N = 15): 97.55 ± 12.11a | VAS 2.2 mm ± 11.5 mm | 24/24 (100 %) | ||
| ATSS-score: 32.66 ± 13.15 | ATSS-score: 97.25 ± 12.31a | |||||
| PGART: 0.25 ± 0.71 | ||||||
| Pearce et al. [30] | AOFAS: 68 (51–82) | AOFAS: 92 (74–100)a | AOS-pain: 28 % | AOS-pain: 8 %a | 8/11 (73 %) | 3/11 (27 %) |
| AOS-disability: 38 % | AOS-disability: 10 %a | |||||
| SF-36: 76 | SF-36: 87 | |||||
| Steenstra and van Dijk [33] | ||||||
| Open surgery: gastrocnemius lengthening | ||||||
| Duthon et al. [10]e | AOFAS: 71 (67–73)c | AOFAS (12 months N = 17d): 100 (90–100)a,c | 12/13 (92.3 %) | 1/13 (7.7 %) | ||
| FFI: 39 (25–45)c | FFI (12 months N = 17d): 12 (10–18)a,c; (24 months N = 17d): 12 (10–19)a,c | |||||
| SF-12 physical: 36 (33–44)c | SF-12 physical (12 months N = 17b): 51 (42–56)a,c; (24 months N = 17d): 51 (46–56)a,c | |||||
| Open surgery: autologous tendon transfer | ||||||
| Martin et al. [23] | AOFAS (N = 19): 91.6 ± 7.7 | VAS: 15 mm (±20 mm) | 37/44 (86 %) | 6/44 (13.8 %) | ||
aStatistically significant (p < 0.05)
bSame study divided into two separate studies
cMedian instead of mean
dStudy includes patients who received bilateral surgical treatment; outcome reported on individual tendons
eStudy included patients who received bilateral surgical treatment; outcome reported on patient level
Appendix 4
See Table 8.
Table 8.
Success rate
| Study | Result at F-U | Success rate | ||||||
|---|---|---|---|---|---|---|---|---|
| Satisfied | Unsatisfied | Excellent | Good | Fair | Poor | Successful | Unsuccessful | |
| Open debridement | ||||||||
| Benazzo et al. [4] | ||||||||
| Johnston et al. [11] | ||||||||
| Kvist and Kvist [13]b | 169/201 (84.1 %) | 25/201 (12.4 %) | 7/201 (3.5 %) | 194/201 (96.5 %) | 7/201 (3.5 %) | |||
| Lohrer and Nauck [15]b | A. 15/15 (100 %) | A. 15/15 (100 %) | ||||||
| B. 23/24 (95.8 %) | B. 1/24 (4.2 %) | B. 23/24 (95.8 %) | B. 1/24 (4.2 %) | |||||
| Maffulli et al. [18] | ||||||||
| Maffulli et al. [21] | ||||||||
| Nelen et al. [26]b | A. 54/93 (58.1 %) | A. 28/93 (30.1 %) | A. 8/93 (8.6 %) | A. 3/93 (3.2 %) | A. 82/93 (88.2 %) | A. 11/93 (11.8 %) | ||
| B. 15/26 (57 %) | B. 4/26 (15.4 %) | B. 4/26 (15.4 %) | B. 3/26 (11.5 %) | B. 19/26 (73.1 %) | B. 7/26 (26.9 %) | |||
| C. 12/24 (50 %) | C. 9/24 (37.5 %) | C. 2/24 (8.3 %) | C. 1/24 (4.2 %) | C. 21/24 (87.5 %) | C. 3/24 (12.5 %) | |||
| Ohberg et al. [27] | 12/24 (50 %) | 10/24 (41.7 %) | 2/24 (8.3 %) | 22/24 (91.7 %) | 2/24 (8.3 %) | |||
| Paavola et al. [29] | ||||||||
| Paavola et al. [28] | A. 5/16 (31.3 %) | A. 11/16 (68.8 %) | A. 16/16 (100 %) | |||||
| B.7/26 (26.9 %) | B.12/26 (46.2 %) | B. 1/26 (3.8 %) | B. 6/26 (23.1 %) | B. 19/26 (73.1 %) | B. 7/26 (26.9 %) | |||
| Sarimo and Orava [31] | 14/24 (58.3 %) | 10/24 (41.7 %) | 24/24 (100 %) | |||||
| Minimally invasive tendon stripping/tenotomies | ||||||||
| Alfredson et al. [2] | 10/10 (100 %) | 10/10 (100 %) | ||||||
| Alfredson [1]a,b | A. 15/18 (83.3 %) | A. 3/18 (16.7 %) | A. 15/18 (83.3 %) | A. 3/18 (16.7 %) | ||||
| B. 15/19 (78.9 %) | B. 4/19 (21.1 %) | B. 15/19 (78.9 %) | B. 4/19 (21.1 %) | |||||
| Alfredson [1]a,b | 81/88 (92.0 %) | 7/88 (8.0 %) | 81/88 (92.0 %) | 7/88 (8.0 %) | ||||
| Alfredson et al. [3] | 11/13 (84.6 %) | 2/13 (15.4 %) | 11/13 (84.6 %) | 2/13 (15.4 %) | ||||
| Calder et al. [6]c | 22/32 (69 %) | 10/32 (31 %) | 22/32 (69 %) | 10/32 (31 %) | ||||
| Maffulli et al. [20] | 30/39 (76.9 %) | 9/39 (23.1 %) | 30/39 (76.9 %) | 9/39 (23.1 %) | ||||
| Naidu et al. [24]c | 24/26 (92 %) | 2/26 (7.7 %) | 24/26 (92 %) | 2/26 (7.7 %) | ||||
| Testa et al. [36] | 35/63 (55.6 %) | 12/63 (19.0 %) | 8/63 (12.7 %) | 8/63 (12.7 %) | 47/63 (74.6 %) | 16/63 (25.4 %) | ||
| Endoscopic procedures | ||||||||
| Maquirriain [22]c | 20/24 (85.1 %) | 4/24 (14.9 %) | 24/24 (100 %) | |||||
| Pearce et al. [30] | 8/11 (73 %) | 3/11 (27 %) | 8/11 (73 %) | 3/11 (27 %) | ||||
| Steenstra and van Dijk [33] | ||||||||
| Open surgery: gastrocnemius lengthening | ||||||||
| Duthon et al. [10]c | 12/13 (92.3 %) | 1/13 (7.7 %) | 12/13 (92.3 %) | 1/13 (7.7 %) | ||||
| Open surgery: autologous tendon transfer | ||||||||
| Martin et al. [23] | 37/44 (86 %) | 6/44 (13.8 %) | 37/44 (86 %) | 6/44 (13.8 %) | ||||
Outlined are patient satisfaction; postoperative result; and success rate
aSame study comparing release of ventral AT with knife versus needle
bStudy includes patients who received bilateral surgical treatment; outcome reported on individual tendons
cStudy included patients who received bilateral surgical treatment; outcome reported on patient level
Compliance with ethical standards
Conflict of interest
None.
References
- 1.Alfredson H. Ultrasound and Doppler-guided mini-surgery to treat midportion Achilles tendinosis: results of a large material and a randomised study comparing two scraping techniques. Br J Sports Med. 2011;45:407–410. doi: 10.1136/bjsm.2010.081216. [DOI] [PubMed] [Google Scholar]
- 2.Alfredson H, Ohberg L, Zeisig E, Lorentzon R. Treatment of midportion Achilles tendinosis: similar clinical results with US and CD-guided surgery outside the tendon and sclerosing polidocanol injections. Knee Surg Sports Traumatol Arthrosc. 2007;15:1504–1509. doi: 10.1007/s00167-007-0415-8. [DOI] [PubMed] [Google Scholar]
- 3.Alfredson H, Spang C, Forsgren S. Unilateral surgical treatment for patients with midportion Achilles tendinopathy may result in bilateral recovery. Br J Sports Med. 2012;48:1421–1424. doi: 10.1136/bjsports-2012-091399. [DOI] [PubMed] [Google Scholar]
- 4.Benazzo F, Zanon G, Klersy C, Marullo M. Open surgical treatment for chronic midportion Achilles tendinopathy: faster recovery with the soleus fibres transfer technique. Knee Surgery Sport Traumatol Arthrosc. 2014 doi: 10.1007/s00167-014-3232-x. [DOI] [PubMed] [Google Scholar]
- 5.Bhandari M, Montori VM, Devereaux PJ, Wilczynski NL, Morgan D, Haynes RB. Doubling the impact: publication of systematic review articles in orthopaedic journals. J Bone Joint Surg Am. 2004;86-A:1012–1016. doi: 10.2106/00004623-200405000-00019. [DOI] [PubMed] [Google Scholar]
- 6.Calder JDF, Freeman R, Pollock N. Plantaris excision in the treatment of non-insertional Achilles tendinopathy in elite athletes. Br J Sports Med. 2014;49:1532–1534. doi: 10.1136/bjsports-2014-093827. [DOI] [PubMed] [Google Scholar]
- 7.Coleman BD, Khan KM, Maffulli N, Cook JL, Wark JD. Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Victorian Institute of Sport Tendon Study Group. Scand J Med Sci Sports. 2000;10:2–11. doi: 10.1034/j.1600-0838.2000.010001002.x. [DOI] [PubMed] [Google Scholar]
- 8.van Dijk CN, van Sterkenburg MN, Wiegerinck JI, Karlsson J, Maffulli N. Terminology for Achilles tendon related disorders. Knee Surgery Sport Traumatol Arthrosc. 2011;19:835–841. doi: 10.1007/s00167-010-1374-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52:377–384. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Duthon VB, Lübbeke A, Duc SR, Stern R, Assal M. Noninsertional Achilles tendinopathy treated with gastrocnemius lengthening. Foot Ankle Int. 2011;32:375–379. doi: 10.3113/FAI.2011.0375. [DOI] [PubMed] [Google Scholar]
- 11.Johnston E, Scranton P, Pfeffer GB. Chronic disorders of the Achilles tendon: results of conservative and surgical treatments. Foot Ankle Int. 1997;18:570–574. doi: 10.1177/107110079701800907. [DOI] [PubMed] [Google Scholar]
- 12.de Jonge S, van den Berg C, de Vos RJ, van der Heide HJL, Weir A, Verhaar JAN, Bierma-Zeinstra SMA, Tol JL. Incidence of midportion Achilles tendinopathy in the general population. Br J Sports Med. 2011;45:1026–1028. doi: 10.1136/bjsports-2011-090342. [DOI] [PubMed] [Google Scholar]
- 13.Kvist H, Kvist M. The operative treatment of chronic calcaneal paratenonitis. J Bone Joint Surg Br. 1980;62:353–357. doi: 10.1302/0301-620X.62B3.7410468. [DOI] [PubMed] [Google Scholar]
- 14.Kvist M. Achilles tendon injuries in athletes. Sports Med. 1994;18:173–201. doi: 10.2165/00007256-199418030-00004. [DOI] [PubMed] [Google Scholar]
- 15.Lohrer H, Nauck T. Results of operative treatment for recalcitrant retrocalcaneal bursitis and midportion Achilles tendinopathy in athletes. Arch Orthop Trauma Surg. 2014;134:1073–1081. doi: 10.1007/s00402-014-2030-8. [DOI] [PubMed] [Google Scholar]
- 16.Longo UG, Ramamurthy C, Denaro V, Maffulli N. Minimally invasive stripping for chronic Achilles tendinopathy. Disabil Rehabil. 2008;30:1709–1713. doi: 10.1080/09638280701786922. [DOI] [PubMed] [Google Scholar]
- 17.Lysholm J, Wiklander J. Injuries in runners. Am J Sports Med. 1987;15:168–171. doi: 10.1177/036354658701500213. [DOI] [PubMed] [Google Scholar]
- 18.Maffulli N, Binfield PM, Moore D, King JB. Surgical decompression of chronic central core lesions of the Achilles tendon. Am J Sports Med. 1999;27:747–752. doi: 10.1177/03635465990270061101. [DOI] [PubMed] [Google Scholar]
- 19.Maffulli N, Longo UG, Loppini M, Denaro V. Current treatment options for tendinopathy. Expert Opin Pharmacother. 2010;11:2177–2186. doi: 10.1517/14656566.2010.495715. [DOI] [PubMed] [Google Scholar]
- 20.Maffulli N, Oliva F, Testa V, Capasso G, Del Buono A. Multiple percutaneous longitudinal tenotomies for chronic Achilles tendinopathy in runners: a long-term study. Am J Sports Med. 2013;41:2151–2157. doi: 10.1177/0363546513494356. [DOI] [PubMed] [Google Scholar]
- 21.Maffulli N, Testa V, Capasso G, Oliva F, Panni AS, Longo UG, King JB. Surgery for chronic Achilles tendinopathy produces worse results in women. Disabil Rehabil. 2008;30:1714–1720. doi: 10.1080/09638280701786765. [DOI] [PubMed] [Google Scholar]
- 22.Maquirriain J. Surgical treatment of chronic achilles tendinopathy: long-term results of the endoscopic technique. J Foot Ankle Surg. 2013;52:451–455. doi: 10.1053/j.jfas.2013.03.031. [DOI] [PubMed] [Google Scholar]
- 23.Martin RL, Manning CM, Carcia CR, Conti SF. An outcome study of chronic Achilles tendinosis after excision of the Achilles tendon and flexor hallucis longus tendon transfer. Foot Ankle Int. 2005;26:691–697. doi: 10.1177/107110070502600905. [DOI] [PubMed] [Google Scholar]
- 24.Naidu V, Abbassian A, Nielsen D, Uppalapati R, Shetty A. Minimally invasive paratenon release for non-insertional Achilles tendinopathy. Foot Ankle Int. 2009;30:680–685. doi: 10.3113/FAI.2009.0680. [DOI] [PubMed] [Google Scholar]
- 25.Nawoczenski DA, Barske H, Tome J, Dawson LK, Zlotnicki JP, Digiovanni BF. Tendinopathy: strength and functional outcomes. J Bone Joint Surg Am. 2015;97:99–105. doi: 10.2106/JBJS.M.01424. [DOI] [PubMed] [Google Scholar]
- 26.Nelen G, Martens M, Burssens A. Surgical treatment of chronic Achilles tendinitis. Am J Sports Med. 1989;17:754–759. doi: 10.1177/036354658901700605. [DOI] [PubMed] [Google Scholar]
- 27.Ohberg L, Lorentzon R, Alfredson H. Good clinical results but persisting side-to-side differences in calf muscle strength after surgical treatment of chronic Achilles tendinosis: a 5-year follow-up. Scand J Med Sci Sports. 2001;11:207–212. doi: 10.1034/j.1600-0838.2001.110403.x. [DOI] [PubMed] [Google Scholar]
- 28.Paavola M, Kannus P, Orava S, Pasanen M, Järvinen M. Surgical treatment for chronic Achilles tendinopathy: a prospective seven month follow up study. Br J Sports Med. 2002;36:178–182. doi: 10.1136/bjsm.36.3.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Paavola M, Orava S, Leppilahti J, Kannus P, Järvinen M. Chronic Achilles tendon overuse injury: complications after surgical treatment. An analysis of 432 consecutive patients. Am J Sports Med. 2000;28:77–82. doi: 10.1177/03635465000280050301. [DOI] [PubMed] [Google Scholar]
- 30.Pearce CJ, Carmichael J, Calder JD. Achilles tendinoscopy and plantaris tendon release and division in the treatment of non-insertional Achilles tendinopathy. Foot Ankle Surg. 2012;18:124–127. doi: 10.1016/j.fas.2011.04.008. [DOI] [PubMed] [Google Scholar]
- 31.Sarimo J, Orava S. Fascial incision and adhesiolysis combined with radiofrequency microtenotomy in treatment of chronic midportion achilles tendinopathy. Scand J Surg. 2011;100:125–128. doi: 10.1177/145749691110000211. [DOI] [PubMed] [Google Scholar]
- 32.Schepsis AA, Leach RE. Surgical management of Achilles tendinitis. Am J Sports Med. 1987;15:308–315. doi: 10.1177/036354658701500403. [DOI] [PubMed] [Google Scholar]
- 33.Steenstra F, van Dijk CN. Achilles tendoscopy. Foot Ankle Clin. 2006;11:429–438. doi: 10.1016/j.fcl.2006.02.001. [DOI] [PubMed] [Google Scholar]
- 34.van Sterkenburg MN, van Dijk CN. Mid-portion Achilles tendinopathy: why painful? An evidence-based philosophy. Knee Surg Sports Traumatol Arthrosc. 2011;19:1367–1375. doi: 10.1007/s00167-011-1535-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tallon C, Coleman BD, Khan KM, Maffulli N. Outcome of surgery for chronic Achilles tendinopathy. A critical review. Am J Sports Med. 2001;29:315–320. doi: 10.1177/03635465010290031101. [DOI] [PubMed] [Google Scholar]
- 36.Testa V, Capasso G, Benazzo F, Maffulli N. Management of Achilles tendinopathy by ultrasound-guided percutaneous tenotomy. Med Sci Sports Exerc. 2002;34:573–580. doi: 10.1097/00005768-200204000-00002. [DOI] [PubMed] [Google Scholar]
- 37.Thermann H, Benetos IS, Panelli C, Gavriilidis I, Feil S Endoscopic treatment of chronic mid-portion Achilles tendinopathy: novel technique with short-term results. Knee Surg Sport Traumatol Arthrosc. 2009;17:1264–1269. doi: 10.1007/s00167-009-0751-y. [DOI] [PubMed] [Google Scholar]
- 38.Wiegerinck JI, Kerkhoffs GM, van Sterkenburg MN, Sierevelt IN, van Dijk CN. Treatment for insertional Achilles tendinopathy: a systematic review. Knee Surg Sport Traumatol Arthrosc. 2013;21:1345–1355. doi: 10.1007/s00167-012-2219-8. [DOI] [PubMed] [Google Scholar]
- 39.Zwiers R, Wiegerinck JI, van Dijk CN. Treatment of midportion Achilles tendinopathy: an evidence-based overview. Knee Surg Sport Traumatol Arthrosc. 2014 doi: 10.1007/s00167-014-3407-5. [DOI] [PubMed] [Google Scholar]


