Abstract
IMPORTANCE
Pediatric traumatic brain injury (TBI) contributes to impairments in behavior and academic performance. However, the long-term effects of early childhood TBI on functioning across settings remain poorly understood.
OBJECTIVE
To examine the long-term functional outcomes of early childhood TBI relative to early childhood orthopedic injuries (OIs). We also examine the moderating role of the social environment as defined by parent report and observational measures of family functioning, parenting practices, and home environment.
DESIGN, SETTING, AND PARTICIPANTS
A prospective, longitudinal, observational cohort study conducted at each child’s home, school, and hospital, including 3 children’s hospitals and 1 general hospital in the Midwest. Patients were enrolled in the initial study between January 2003 and October 2006. Follow-ups were completed between January 2010 and April 2015. Fifty-eight children who sustained a TBI (67%of original enrolled cohort) and 72 children who sustained an OI (61% of the original enrolled cohort) were prospectively followed up from shortly after injury (between the ages of 3 and 7 years at enrollment) to an average of 6.7 years after injury, with assessments occurring at multiple points.
MAIN OUTCOMES AND MEASURES
Long-term functional outcomes in everyday settings, as assessed through the Child and Adolescent Functional Assessment Scale (CAFAS).
RESULTS
Of the 130 children included, the median age for those with OIs was 11.72 years and 11.97, 12.21, and 11.72 years for those with complicated mild, moderate, and severe TBIs, respectively. Children with moderate and severe TBI were rated as having more functional impairments in multiple domains than those with OIs (P < .05). Children with complicated mild TBI had greater impairments in school (odds ratio = 2.93; 95%CI = 1.10–7.82) and with thinking (odds ratio = 15.72; 95%CI = 3.31–74.73) than those with OIs. Functional impairments in children with TBI were more pronounced among children from families with higher levels of permissive (mean CAFAS of 49.71, 35.74, 58.14, and 16.16 for severe TBI, moderate TBI, complicated mild TBI, and OI, respectively, with significant difference between severe TBI and OI [difference = 33.55; P < .001] and complicated mild TBI and OI [difference = 41.98; P < .001]) or authoritarian (mean CAFAS of 56.45, 41.80, 54.90, and 17.12 for severe TBI, moderate TBI, complicated mild TBI, and OI, respectively, with significant difference between severe TBI and OI [difference = 39.33; P < .001], moderate TBI and OI [difference = 24.68; P = .003], and complicated mild TBI and OI [difference = 37.78; P < .001]) parenting or with fewer home resources (mean CAFAS of 69.57, 47.45, 49.00, and 23.81 for severe TBI, moderate TBI, complicated mild TBI, and OI, respectively, with significant difference between severe TBI and OI [difference = 45.77; P < .001], moderate TBI and OI [difference = 23.64; P < .001], and complicated mild TBI and OI [difference = 25.20; P < .001]).
CONCLUSIONS AND RELEVANCE
Even children with relatively mild early TBI experience long-term functional impairments, particularly in the context of less favorable home environments. These findings suggest that improving parenting skills and the quality of the home environment may promote functional recovery following early TBI.
Mounting evidence suggests that early brain injury has more profound and persistent effects than brain injury sustained in later childhood or adolescence.1 Impairments cut across domains of neurocognitive abilities, executive function skills, behavior, and social competence.2 However, to our knowledge, few studies have examined the consequences of early brain injury on everyday functioning, particularly among cohorts that were followed up prospectively since the time of injury. Characterization of everyday functioning following traumatic brain injury (TBI) may help us to understand and predict longterm deficits in educational attainment, employment, relationships, and quality of life.3
A 10-year longitudinal follow-up study,4 a notable exception to the dearth of prospective studies, provides important evidence regarding the effects of early TBI on long-term functioning. The study’s investigative team defined functioning at 10 years in terms of parent-reported adaptive behavior and behavior problems and found that children with severe TBI had poorer adaptive functioning across domains but not significantly higher levels of internalizing or externalizing behavior problems. Although these findings add important information to a scant literature, they were limited by high attrition, a relatively small sample size (N = 59), and reliance on parental report.
Additional previous studies2,5,6 provide support for the influence of the social environment on recovery and for the longer-term social and behavioral outcomes of TBI. Factors such as family functioning,5 parental warmth, negativity, disciplinary practices,6–8 and the stressors and resources in the home2,9 have each been linked to cognitive and behavioral outcomes, with generally stronger associations with behavioral recovery. Several studies have demonstrated stronger effects of the social environment among children with more significant neurological insult,5,10,11 suggesting that children with severe TBI may be more able to benefit from a positive family environment characterized by emotional and educational resources and responsive, nonpunitive parenting.
The goal of this prospective cohort study was to examine the long-term functional outcomes of children who sustained TBI relative to functioning in children who sustained orthopedic injuries (OIs) between 3 and 7 years of age. Unlike previous studies, we used the Child and Adolescent Functional Assessment Scale (CAFAS),12 which is clinical ratings derived from a structured clinical interview with the parent(s), to provide an estimate of functioning in everyday settings, including school, home, and community.
We also examined the moderating role of the social environment as defined by both parent report and observational measures of family functioning, parenting practices, and home environment. We anticipated that impairments in everyday functioning during the middle-school years would be most pronounced among children with TBI whose parents reported using permissive or overly strict disciplinary practices and whose families had poorer functioning and fewer resources.
Methods
Design and Participants
This was a prospective cohort study of environmental influences on long-term functional outcomes (average: 6.7 years after injury) for children who sustained early childhood TBI or OI. Participants who sustained a TBI or OI between ages 3 and 7 years were enrolled from 3 children’s hospitals and 1 general hospital in the Midwest. The institutional review boards of Cincinnati Children’s Hospital Medical Center, Nationwide Children’s Hospital, Rainbow Babies and Children’s Hospital/University Hospitals of Cleveland, and MetroHealth Medical Center approved the study design and methods. Written consent was obtained from all enrolled families. Participants underwent assessments at multiple points across the initial 18 months after injury. Inclusion criteria included hospitalization overnight for traumatic injury (TBI or OI) sustained between the ages of 36 and 83 months, no evidence of child abuse as cause of injury, no history of documented neurological problems or developmental delays before the injury, and English as the primary language in the home. The severity of the TBI was characterized using the Glasgow Coma Scale (GCS), which was available in the medical record of all participants with TBI.13 Severe TBI was defined by a lowest postresuscitation GCS score of 8 or less. The moderate TBI group had a GCS score of 9 to 12. Complicated mild TBI was defined by a GCS score of 13 to 15 with abnormal brain imaging. The OI group included children who sustained a bone fracture (excluding skull fractures) with no alterations in consciousness or other signs or symptoms of head trauma or brain injury.
Given our objective was to examine functional outcomes in middle school when academic and social expectations are increasing, parents were recontacted by both letter and telephone call when the child was in fifth grade and invited to participate in the long-term follow-up study. If contact information was no longer correct, we contacted family members or friends the family listed previously to obtain new contact information. We also attempted to contact families through electronic and physical mailings of the study brochure.
Measures
Everyday Functioning
The CAFAS assessed everyday functioning. The CAFAS uses information from structured interviews with key informants (eg, parents) to generate standardized ratings for functioning across domains and settings. It predicts subsequent service use better than either psychiatric diagnoses or standardized checklists, 14 including the Child Behavior Checklist,15 which is moderately correlated with the CAFAS (r = 0.65). Used widely to assess changes in clinical outcomes for youth receiving mental health services,16 the CAFAS generates ratings for functioning in 8 domains: school, home, community, behavior toward others, moods/emotions, self-harmful behaviors, substance abuse, and thinking. Functioning in each domain is rated on an ordinal scale, ranging from 0 (unimpaired) to 30 (severe impairment) in 10-point increments. A total score is created by summing domain scores (range: 0–240), with scores less than or equal to 50 considered to be “unimpaired” and those greater than 50 as “impaired.” The CAFAS has established validity and excellent interrater reliability, ranging from 0.74 to 0.99.17 For this study, 2 research personnel with advanced degrees in psychology or counseling were certified as CAFAS trainers. Additional raters were trained to achieve an interrater reliability greater than 80%, as recommended by the creator of the CAFAS. 18 Raters were unaware of the severity or nature of each child’s injury. Ten percent of interviews were taped and jointly rated, yielding an overall interrater reliability of 98.7%. The CAFAS was administered only at the last follow-up visit of the study.
Family Environment
Three measures of the social environment were examined as potential moderators of long-term functioning. The Parenting Practices Questionnaire (PPQ)19 is a 62-item rating scale that assesses 3 dimensions of parenting style, consistent with characterizations of authoritarian (parent-centered, demanding, unresponsive, and punishment-heavy), authoritative (high acceptance and expectations, warmth, and autonomy development), and permissive (low expectations of appropriate behaviors, little instruction, and high responsiveness to child’s needs) parenting.20 The scales for each dimension represent composites of subscales derived through factor analysis. For the purposes of the current study, we used total scores for each dimension. The PPQ was developed for children between ages 4 and 12 years and has been used in studies on adolescents with TBI.21 The questionnaire has shown satisfactory reliability and validity in previous research.22 The General Functioning subscale of the McMaster Family Assessment Device (FAD-GF) assesses family functioning.23,24 This 12-item measure possesses satisfactory reliability and validity23,24 and has been shown to predict social and behavioral outcomes following pediatric TBI.3,25–27 Higher scores reflect worse family functioning. The quality of the home environment was assessed using the early adolescent version of the Home Observation for Measures of the Environment (EA HOME).28 The EA HOME was designed for use with children between the ages of 10 and 15 years. It is administered in the child’s home and integrates parent interviews with direct observations of characteristics of the home (eg, space and availability of books) and the quality of the parent-child interactions. The EA HOME has been shown to predict longer-term developmental outcomes28,29 with satisfactory validity and reliability.30 In this study, reliability was assessed by having 2 research assistants complete the EA HOME independently for approximately 5% of the home visits. Interrater agreement exceeded r = 0.92. The total score was used in the current study. Preliminary analyses revealed modest correlations among the family environment variables (r range: 0.17–0.42; all P < .05).
Analyses
Group differences in the CAFAS total score were examined using a linear model adjusted for potential confounders, with Tukey pairwise comparisons between injury groups. Secondary analyses of group differences by rates (odds) of falling in a more impaired category for each of the 8 subscales (rating of 0, 1, 2, or 3, with 3 being the most severely impaired) were conducted using the proportional odds cumulative logit model, which is a special case of logistic regression that allows ordered responses over more than 2 levels.31,32 The primary predictor variables for the logistic regressions were dummy contrasts representing comparisons of each TBI group with the OI group. Covariates included time since injury, age, child’s race/ethnicity, sex, study site, and socioeconomic status z score (Z-SES) as defined by the mean of sample z scores for income based on census tract and parental/guardian education.
Linear regression analysis was used to test the hypothesis that social-environmental characteristics, as assessed by the PPQ, FAD-GF, and EA HOME, moderated the association between injury severity and long-term functional outcomes. Models included injury severity, social-environmental factors and their interactions, time since injury, age, child’s race/ethnicity, sex, and Z-SES as defined by the mean of sample z scores for income based on census tract and parental/guardian education. All analysis was conducted using SAS version 9.3 (SAS Institute).
Results
Sample Description
We successfully reestablished contact with 163 of the 217 participants (75%) eligible for the follow-up assessment. Of these, 17 (10%) declined to participate because they were too busy or the child did not want further assessments. Excluded from the current analyses were 12 children with uncomplicated mild TBI and 4 children whose parents did not complete the CAFAS interview. Seventy-two children with OI and 58 children with TBI completed the follow-up assessment. Participants included 16 of 23 children with severe TBI (69.6%), 14 of 21 children with moderate TBI (66.7%), and 28 of 43 children with complicated mild TBI (65.1%). Participants did not differ significantly (P < .05) from the children who did not complete follow-up with respect to injury type, sex, race/ethnicity, Z-SES, child IQ at baseline, or baseline social-environmental characteristics as measured by the FAD-GF or EA HOME. Participants who did not complete follow-up had higher authoritative PPQ scores (P = .05) but did not differ significantly in authoritarian (P = .18) or permissive scores (P = .31). Within the follow-up sample, none of the TBI groups differed significantly from the OI group in age, time since injury, sex, race/ethnicity, or Z-SES (Table 1). The EA HOME scores were significantly lower for the severe and moderate TBI groups than for the OI group but did not differ significantly between complicated mild TBI and OI groups. Permissive parenting scores were significantly higher for the severe TBI group than the OI group, but the groups did not differ on other social-environmental variables.
Table 1.
Demographics and Baseline Environment Variables by Injury Type
| Characteristic | Median (IQR) | P Valuea | |||
|---|---|---|---|---|---|
| Orthopedic Injuries (n = 72) | Traumatic Brain Injury | ||||
| Complicated Mild (n = 28) | Moderate (n = 14) | Severe (n = 16) | |||
| Age, y | 11.72 (11.23 to 12.28) | 11.97 (10.71 to 12.80) | 12.21 (11.68 to 12.55) | 11.72 (11.03 to 12.80) | .67 |
| Age at injury, y | 5.13 (4.25 to 5.96) | 5.19 (4.30 to 6.11) | 5.82 (4.06 to 6.32) | 5.09 (4.00 to 5.89) | .73 |
| Time since injury, y | 6.58 (6.24 to 7.46) | 6.61 (6.14 to 7.36) | 6.60 (5.82 to 7.86) | 7.04 (6.41 to 7.71) | .71 |
| Female, % | 47 | 36 | 50 | 38 | .69 |
| Race not white, % | 24 | 14 | 43 | 38 | .14 |
| Z-SESb | 0.01 (−0.55 to 0.79) | 0.09 (−0.62 to 0.65) | −0.51 (−1.28 to 1.21) | −0.51 (−0.86 to 0.05) | .16 |
| PPQ | |||||
| Authoritative | 115.0 (106.0 to 123.0) | 113.0 (106.5 to 124.5) | 115.5 (99.5 to 124.0) | 117.0 (99.5 to 121.0) | .90 |
| Authoritarian | 35.5 (31.0 to 42.0) | 35.0 (31.0 to 43.5) | 41.0 (33.0 to 48.0) | 38.5 (32.5 to 43.5) | .43 |
| Permissive | 27.0 (24.0 to 30.5) | 25.5 (23.0 to 31.5) | 30.0 (23.0 to 35.5) | 34.0 (27.0 to 39.0) | .02 |
| EA HOME | 50.5 (45.0 to 55.0) | 49.0 (42.5 to 51.5) | 42.0 (34.0 to 5.0) | 46.0 (43.0 to 49.0) | .02 |
| FAD-GF | 1.67 (1.29 to 1.92) | 1.75 (1.29 to 1.96) | 1.75 (1.50 to 1.92) | 1.96 (1.58 to 2.13) | .15 |
Abbreviations: EA HOME, early adolescent version of Home Observation for Measures of the Environment; IQR, interquartile range; FAD-GF, General Functioning subscale of the McMaster Family Assessment Device; PPQ, Parenting Practices Questionnaire; Z-SES, socioeconomic status z score.
P values are based on Kruskal-Wallis test for continuous outcomes or Fisher exact test of association.
Z-SES was based on parental education and census tract income.
Group Differences on CAFAS
Examination of CAFAS total scores revealed a dose-response association, with higher ratings of functional impairment for children with more severe TBI (P < .001). Scores were significantly higher for all 3 TBI groups (complicated mild, moderate, and severe) compared with the OI group (P < .05 on Tukey pairwise comparisons). Males had significantly higher ratings of impairments compared with females (P = .007).
As depicted in Table 2, significant group differences were also found for the school/work (P = .001), home (P = .04), behavior toward others (P = .04), moods/emotions (P = .002), and thinking (P = .002) subscales. Post hoc analyses indicated that children with severe TBI had significantly higher rates of functional impairments in the domains of school, home, behavior toward others, moods, and thinking compared with those with OI. Similarly, children with moderate TBI had significantly higher rates of functional impairments in school, behavior toward others, moods, and thinking than those with OI. Complicated mild TBI was associated with an increased risk of impairments in school and thinking. Models examining self-harm and substance use failed to converge owing to the low frequency of any impairment in these 2 domains (3 for self-harm and 1 for substance abuse).
Table 2.
Odds Ratio of Functional Impairment: CAFAS Subscales
| Comparison | Odds Ratio (95% CI) | P Value | ||
|---|---|---|---|---|
| Complicated Mild TBI vs OI | Moderate TBI vs OI | Severe TBI vs OI | ||
| School/work | 2.93 (1.10–7.82) | 6.21 (1.73–22.34) | 8.59 (2.56–28.82) | .001 |
| Home | 1.00 (0.40–2.51) | 1.31 (0.39–4.37) | 5.03 (1.61–15.77) | .04 |
| Community | 1.60 (0.11–23.27) | 2.59 (0.21–32.62) | 14.26 (1.64–124.32) | .10 |
| Behavior toward others | 2.93 (0.96–8.90) | 4.02 (1.05–15.37) | 4.87 (1.38–17.25) | .04 |
| Moods/emotions | 2.46 (0.87–6.98) | 10.22 (2.95–35.47) | 4.03 (1.17–13.87) | .002 |
| Self-harmful | … | … | … | … |
| Substance use | … | … | … | … |
| Thinking | 15.72 (3.31–74.73) | 10.00 (1.50–66.67) | 22.39 (3.88–129.19) | .002 |
Abbreviations: CAFAS, Child and Adolescent Functional Assessment Scale; ellipses, models did not converge and no estimates were available; OI, orthopedic injury; TBI, traumatic brain injury.
Social-Environmental Moderators of Functional Impairment
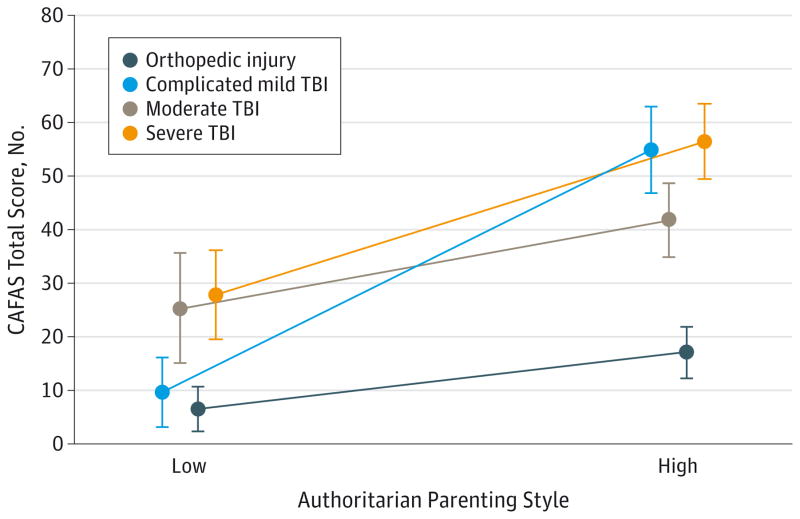
Linear regression analyses examining moderators of global impairment revealed a significant group by authoritarian parenting interaction (P = .03). As depicted in Figure 1, at high levels of authoritarian parenting (1 SD above the mean of the entire cohort), children with any TBI were rated as having greater functional impairments than children with OI; however, at low levels of authoritarian parenting (1 SD below the mean of the entire cohort), only children with severe TBI were rated as having significantly greater functional impairments (difference in mean CAFAS vs OI = 21.35;P = .03). These findings suggest that the effects of complicated mild and moderate TBI on functioning are amplified under conditions of high levels of authoritarian parenting.
Figure 1. Adjusted Mean Levels of Functional Impairment by Group at Low/High Levels of Authoritarian Parenting.
Significant group by authoritarian parenting interaction (F3,113 = 3.14; P = .03). Children with traumatic brain injury (TBI) revealed greater functional impairment ratings than children with orthopedic injury at high authoritarian parenting levels, but only children with severe TBI showed significantly greater functional impairment ratings than those with orthopedic injury at low levels of authoritarian parenting (difference = 21.35; P = .03). Error bars indicate ±1 SE.
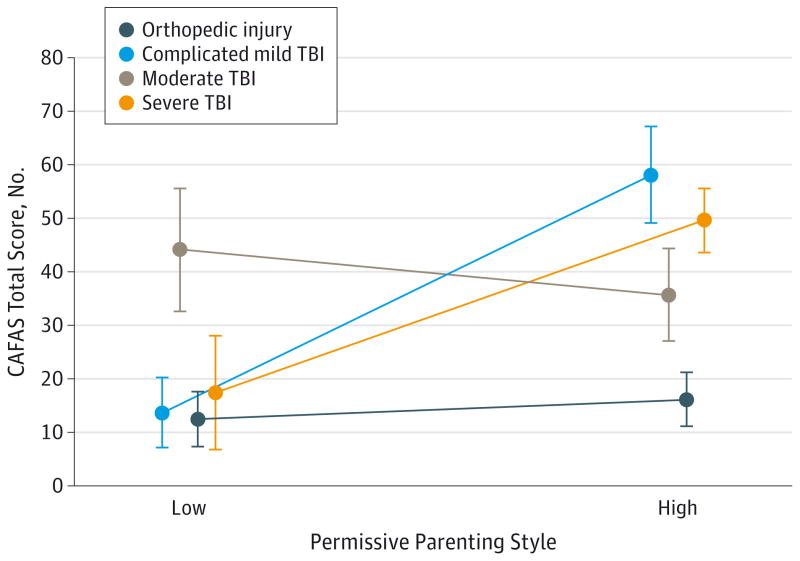
Permissive parenting also moderated the effects of injury severity on functional outcomes (P < .001). As depicted in Figure 2, at low levels of permissive parenting (1 SD below the mean of the entire cohort), children with moderate TBI (P = .007) were rated as having greater functional impairment than children with OI. However, at high levels of permissive parenting (1 SD above the mean of the entire cohort), youths with complicated mild (P < .001) and severe (P < .001) TBI were rated as having greater functional impairment than those with OI.
Figure 2. Adjusted Mean Levels of Functional Impairment by Group at Low/High Levels of Permissive Parenting.
Significant group by permissive parenting interaction (F3,113 = 5.74; P = .001). Children with complicated mild (difference = 33.55; P < .001) and severe (difference = 41.98; P < .001) traumatic brain injury (TBI) revealed greater functional impairment ratings than those with orthopedic injury at high permissive parenting levels, yet children with moderate TBI (difference = 31.64; P = .007) showed greater functional impairment ratings than children with orthopedic injury at low levels of permissive parenting. Error bars indicate ±1 SE.
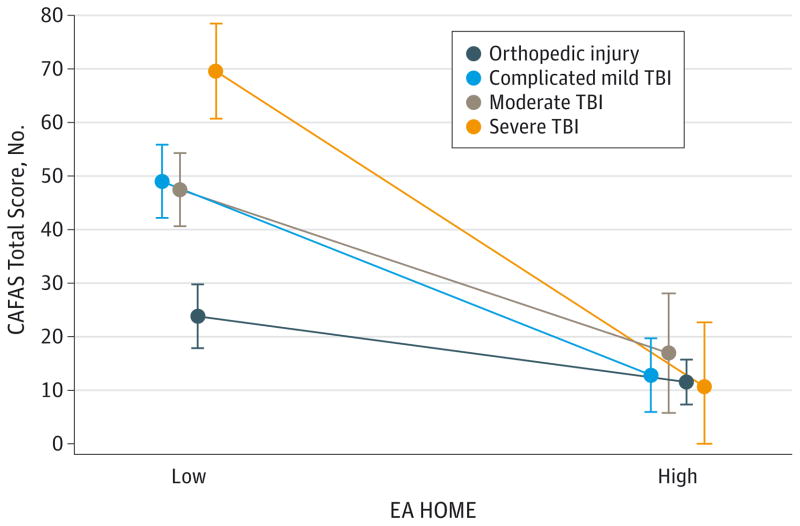
Long-term effects of TBI on functional outcomes were additionally moderated by the EA HOME total (P = .02). As depicted in Figure 3, group contrasts at 1 SD below the mean of the entire cohort (ie, less enriched home environments) revealed significantly poorer functioning following any TBI than following OI. In more enriched home environments (1 SD above the mean of the entire cohort), no significant differences were found in functional impairment between youth with TBI and OI.
Figure 3. Adjusted Mean Levels by Group at Low/High Levels of Facilitative Home Environments.
Significant group by home environment interaction (F3,114 = 3.28; P = .02) revealed significantly poorer long-term functioning outcomes for children with a traumatic brain injury (TBI) than children with an orthopedic injury when the home environment had low enrichment, while high facilitative home environments revealed no significant group differences in functional impairment. EA HOME indicates the early adolescent version of the Home Observation for Measures of the Environment. Error bars indicate ±1 SE.
Discussion
Our findings support the hypothesized association between early childhood TBI and long-term impairments in everyday functioning an average of nearly 7 years after injury. Youths with all severities of TBI were rated as having worse overall functioning than youths with OI. Severe TBI was associated with poorer functioning across domains including school, home, community, behavior toward others, moods/emotions, and thinking. Children with complicated mild, moderate, or severe TBI had higher rates of impairment in school and thinking than those with OI, suggesting that the functional consequences of neurocognitive impairments were persistent and cut across severity levels. Contrary to recent evidence regarding elevated rates of substance use and depression among adolescents with TBI,33,34 rates of impairment in these domains were too low to analyze. However, our cohort comprised emerging adolescents, with an average age of 12 years, who may go on to develop difficulties in these domains later in adolescence.
Parenting practices and quality of the home environment moderated the association between TBI severity and functional outcomes. Consistent with hypotheses and prior research, the adverse effects of TBI on functioning were amplified by either permissive or strict, controlling parenting, as well as by less advantaged home environments. One exception to this pattern of findings was the absence of heightened functional impairments in children with moderate TBI by permissive parenting. Given the small sample size, this contrary finding merits replication with a larger sample.
The current results run counter to earlier findings with this cohort that initial protective effects of the social environment diminished by 18months after injury.2 The renewed relevance of parenting and home environment to long-term functioning following early TBI may be attributable in part to emerging deficits35 in higher-order cognitive skills (ie, executive functions), with increasing demands for self-regulation and organization during early adolescence. Traumatic brain injury– related deficits may become more prominent during this period, particularly in the context of home environments that are not conducive to optimal functioning. Under suboptimal home conditions, even children with less severe TBI (eg, complicated mild TBI) may display functional impairments relative to peers without TBI.
Alternatively, the behavioral and social impairments associated with TBI may contribute to changes in parenting and the home environment over time. Our finding of higher levels of permissive parenting and lower quality home environments in the moderate and severe TBI groups are also consistent with the possibility of reciprocal associations between home environment/parenting and child functioning over time. Although beyond the scope of the current report, further research examining the reciprocal associations of child and family outcomes following pediatric TBI36 is needed to elucidate causality.
The current findings have important implications for family-centered interventions. Given that maladaptive parenting practices (overly punitive or overly permissive) were associated with increased morbidity following complicated mild to severe TBI, interventions to promote more effective parenting may be useful for preventing or ameliorating morbidity. Parenting skills interventions have been successfully trialed with children with TBI37,38 and acquired brain injuries39,40 and have been shown to contribute to improvements in behavior problems and care giving efficacy. Less is known regarding the optimal timing of such interventions, eg, whether a parenting intervention shortly after injury can lead to lasting changes in parenting style or whether parent training needs to be repeated at intervals to prevent emerging impairments.
The limitations of the current study should be noted. Although children who completed this long-term follow-up were comparable in most respects with those who dropped out or were unable to be contacted, they had lower baseline authoritative parenting scores than those who did not complete the follow-up, which may suggest some selection bias. Furthermore, the CAFAS is not commonly used to assess long-term functional outcomes of pediatric TBI, making comparisons across studies difficult. The advantage of the CAFAS relative to more traditional TBI assessments41 is that it focuses on broader functional deficits as they manifest in everyday settings. Additionally, because the CAFAS was administered only at the final assessment, it was not possible to examine changes in functional impairment over time. Structured psychiatric interviews were not conducted and would have yielded further information regarding the effect of early TBI on mental health outcomes in early adolescence. The results should be interpreted with caution because of the small group sizes. The limited number of deficits on some subscales (such as self-harm and substance use) precluded group comparisons and may lead to over fitted models for other subscales. Families that did not speak English at home were excluded, which further limits the generalizability of the study findings.
Conclusions
Findings suggest that children who sustain early TBI are at risk for long-term impairments in everyday functioning, particularly in the context of less optimal home environments and parenting behaviors. Further follow-up is needed to determine whether these functional impairments persist into adulthood and are associated with lower educational and occupation attainments and diminished quality of life.3,42,43
Key Points.
Question
How are long-term functional outcomes different between adolescents with early childhood traumatic brain injury (TBI) and with orthopedic injury, and how do social and home environments affect these outcomes?
Findings
In a prospective longitudinal cohort study, children with early TBI were rated as having higher levels of functional impairments than those with orthopedic injury, with boys having higher levels of impairment than girls. Functional impairments in children with TBI were more pronounced among children from families with higher levels of authoritarian or permissive parenting or with fewer home resources.
Meaning
This follow-up provides important evidence associated with long-term functional impairments in adolescents who sustained early childhood TBI.
Acknowledgments
Funding/Support: This publication was supported by grant R01 HD42729 from the National Institute of Child Health and Human Development and by Trauma Research grants from the State of Ohio Emergency Medical Services. Additional support was provided through grant 8 UL1 TR000077 from the National Center for Advancing Translational Sciences of the National Institutes of Health.
Footnotes
Conflict of Interest Disclosures: None reported.
Role of the Funder/Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Disclaimer: The contents of the article are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health.
Additional Contributions: We acknowledge the paid contributions of Anne Birnbaum, BA, and Nori Minich, BA, at Case University; Holly MacPherson, BSc, Hanna Schultz, MA, and Karen Oberjohn, MA, at Cincinnati Children’s Hospital Medical Center; and Melissa Ginn, BS, and April Hunt, MA, at Nationwide Children’s Hospital. They received compensation from the National Institute of Child Health and Human Development. We would also like to thank the families for their participation over time.
Author Contributions: Dr Wade had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Wade, Yeates, Stancin.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Wade.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Wade, Zhang, Yeates.
Obtained funding: Wade.
Administrative, technical, or material support: Wade, Zhang, Stancin, Taylor.
Study supervision: Wade, Yeates, Stancin, Taylor.
References
- 1.Anderson V, Jacobs R, Spencer-Smith M, et al. Does early age at brain insult predict worse outcome? neuropsychological implications. J Pediatr Psychol. 2010;35(7):716–727. doi: 10.1093/jpepsy/jsp100. [DOI] [PubMed] [Google Scholar]
- 2.Yeates KO, Taylor HG, Walz NC, Stancin T, Wade SL. The family environment as a moderator of psychosocial outcomes following traumatic brain injury in young children. Neuropsychology. 2010;24(3):345–356. doi: 10.1037/a0018387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anderson V, Brown S, Newitt H, Hoile H. Educational, vocational, psychosocial, and quality-of-life outcomes for adult survivors of childhood traumatic brain injury. J Head Trauma Rehabil. 2009;24(5):303–312. doi: 10.1097/HTR.0b013e3181ada830. [DOI] [PubMed] [Google Scholar]
- 4.Catroppa C, Godfrey C, Rosenfeld JV, Hearps SS, Anderson VA. Functional recovery ten years after pediatric traumatic brain injury: outcomes and predictors. J Neurotrauma. 2012;29(16):2539–2547. doi: 10.1089/neu.2012.2403. [DOI] [PubMed] [Google Scholar]
- 5.Kurowski BG, Taylor HG, Yeates KO, Walz NC, Stancin T, Wade SL. Caregiver ratings of long-term executive dysfunction and attention problems after early childhood traumatic brain injury: family functioning is important. PM R. 2011;3(9):836–845. doi: 10.1016/j.pmrj.2011.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wade SL, Cassedy A, Walz NC, Taylor HG, Stancin T, Yeates KO. The relationship of parental warm responsiveness and negativity to emerging behavior problems following traumatic brain injury in young children. Dev Psychol. 2011;47(1):119–133. doi: 10.1037/a0021028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Potter JL, Wade SL, Walz NC, et al. Parenting style is related to executive dysfunction after brain injury in children. Rehabil Psychol. 2011;56(4):351–358. doi: 10.1037/a0025445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Woods DT, Catroppa C, Barnett P, Anderson VA. Parental disciplinary practices following acquired brain injury in children. Dev Neurorehabil. 2011;14(5):274–282. doi: 10.3109/17518423.2011.586371. [DOI] [PubMed] [Google Scholar]
- 9.Wade SL, Stancin T, Taylor HG, Drotar D, Yeates KO, Minich NM. Interpersonal stressors and resources as predictors of parental adaptation following pediatric traumatic injury. J Consult Clin Psychol. 2004;72(5):776–784. doi: 10.1037/0022-006X.72.5.776. [DOI] [PubMed] [Google Scholar]
- 10.Yeates KO, Taylor HG, Drotar D, et al. Preinjury family environment as a determinant of recovery from traumatic brain injuries in school-age children. J Int Neuropsychol Soc. 1997;3(6):617–630. [PubMed] [Google Scholar]
- 11.Taylor HG, Yeates KO, Wade SL, Drotar D, Stancin T, Minich N. A prospective study of short- and long-term outcomes after traumatic brain injury in children: behavior and achievement. Neuropsychology. 2002;16(1):15–27. doi: 10.1037//0894-4105.16.1.15. [DOI] [PubMed] [Google Scholar]
- 12.Hodges K. The Child and Adolescent Functional Assessment Scale Self-Training Manual. Ypsilanti: Eastern Michigan University, Department of Psychology; 1994. [Google Scholar]
- 13.Teasdale G, Jennett B. Assessment of coma and impaired consciousness: a practical scale. Lancet. 1974;2(7872):81–84. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- 14.Hodges K, Wong MM. Use of the Child and Adolescent Functional Assessment Scale to predict service utilization and cost. J Ment Health Adm. 1997;24(3):278–290. doi: 10.1007/BF02832662. [DOI] [PubMed] [Google Scholar]
- 15.Achenbach TM, Rescorla LA. Manual for ASEBA School-Age Forms & Profiles. Burlington: University of Vermont Research Center for Children, Youth, & Families; 2001. [Google Scholar]
- 16.Hodges K, Wong MM, Latessa M. Use of the Child and Adolescent Functional Assessment Scale (CAFAS) as an outcome measure in clinical settings. J Behav Health Serv Res. 1998;25(3):325–336. doi: 10.1007/BF02287471. [DOI] [PubMed] [Google Scholar]
- 17.Hodges K, Wong MM. Psychometric characteristics of a multidimensional measure to assess impairment: the child and adolescent functional assessment scale. J Child Fam Stud. 1996;5(4):445–467. doi: 10.1007/BF02233865. [DOI] [Google Scholar]
- 18.Hodges K. CAFAS: Manual for Training Coordinators, Clinical Administrators, and Data Managers. Ann Arbor, MI: Kay Hodges; 2003. [Google Scholar]
- 19.Robinson CC, Mandleco B, Olsen SF, Hart CH. Authoritative, authoritarian, and permissive parenting practices: development of a new measure. Psychol Rep. 1995;77(3):819–830. doi: 10.2466/pr0.1995.77.3.819. [DOI] [Google Scholar]
- 20.Baumrind D. Current patterns of parental authority. Dev Psychol. 1971;4(1p2):1–103. doi: 10.1037/h0030372. [DOI] [Google Scholar]
- 21.Micklewright JL, King TZ, O’Toole K, Henrich C, Floyd FJ. Parental distress, parenting practices, and child adaptive outcomes following traumatic brain injury. J Int Neuropsychol Soc. 2012;18(2):343–350. doi: 10.1017/S1355617711001792. [DOI] [PubMed] [Google Scholar]
- 22.Robinson CC, Mandleco B, Olsen SF, Hart CH. The Parenting Styles and Dimensions Questionnaire (PSDQ) In: Perlmutter BF, Touliatos J, Holden GW, editors. Handbook of Family Measurement Techniques: Instruments & Index. Vol. 3. Thousand Oaks, CA: Sage; 2001. pp. 319–321. [Google Scholar]
- 23.Byles J, Byrne C, Boyle MH, Offord DR. Ontario Child Health Study: reliability and validity of the general functioning subscale of the McMaster Family Assessment Device. Fam Process. 1988;27(1):97–104. doi: 10.1111/j.1545-5300.1988.00097.x. [DOI] [PubMed] [Google Scholar]
- 24.Miller IW, Epstein NB, Bishop DS, Keitner GI. The McMaster family assessment device: reliability and validity. J Marital Fam Ther. 1985;11(4):345–356. doi: 10.1111/j.1752-0606.1985.tb00028.x. [DOI] [Google Scholar]
- 25.Anderson V, Beauchamp MH, Yeates KO, Crossley L, Hearps SJ, Catroppa C. Social competence at 6 months following childhood traumatic brain injury. J Int Neuropsychol Soc. 2013;19(5):539–550. doi: 10.1017/S1355617712001543. [DOI] [PubMed] [Google Scholar]
- 26.Yeates KO, Swift E, Taylor HG, et al. Short- and long-term social outcomes following pediatric traumatic brain injury. J Int Neuropsychol Soc. 2004;10(3):412–426. doi: 10.1017/S1355617704103093. [DOI] [PubMed] [Google Scholar]
- 27.McCauley SR, Wilde EA, Anderson VA, et al. Pediatric TBI Outcomes Workgroup. Recommendations for the use of common outcome measures in pediatric traumatic brain injury research. J Neurotrauma. 2012;29(4):678–705. doi: 10.1089/neu.2011.1838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bradley RH, Caldwell BM. The HOME Inventory and family demographics. Dev Psychol. 1984;20(2):315–320. doi: 10.1037/0012-1649.20.2.315. [DOI] [Google Scholar]
- 29.Totsika V, Sylva K. The home observation for measurement of the environment revisited. Child Adolesc Ment Health. 2004;9(1):25–35. doi: 10.1046/j.1475-357X.2003.00073.x. [DOI] [PubMed] [Google Scholar]
- 30.Bradley RH, Corwyn RF, Caldwell BM, Whiteside-Mansell L, Wasserman GA, Mink IT. Measuring the home environments of children in early adolescence. J Res Adolesc. 2000;10(3):247–288. doi: 10.1207/SJRA1003_1. [DOI] [Google Scholar]
- 31.Bender R, Grouven U. Ordinal logistic regression in medical research. J R Coll Physicians Lond. 1997;31(5):546–551. [PMC free article] [PubMed] [Google Scholar]
- 32.Hosmer DW, Jr, Lemeshow S, Sturdivant RX. Applied Logistic Regression. Vol. 398. DeKalb, IL: John Wiley & Sons; 2013. [Google Scholar]
- 33.Ilie G, Boak A, Adlaf EM, Asbridge M, Cusimano MD. Prevalence and correlates of traumatic brain injuries among adolescents. JAMA. 2013;309(24):2550–2552. doi: 10.1001/jama.2013.6750. [DOI] [PubMed] [Google Scholar]
- 34.Ilie G, Mann RE, Boak A, et al. Suicidality, bullying and other conduct and mental health correlates of traumatic brain injury in adolescents. PLoS One. 2014;9(4):e94936. doi: 10.1371/journal.pone.0094936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chapman LA, Wade SL, Walz NC, Taylor HG, Stancin T, Yeates KO. Clinically significant behavior problems during the initial 18 months following early childhood traumatic brain injury. Rehabil Psychol. 2010;55(1):48–57. doi: 10.1037/a0018418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Taylor HG, Yeates KO, Wade SL, Drotar D, Stancin T, Burant C. Bidirectional child-family influences on outcomes of traumatic brain injury in children. J Int Neuropsychol Soc. 2001;7(6):755–767. doi: 10.1017/s1355617701766118. [DOI] [PubMed] [Google Scholar]
- 37.Antonini TN, Raj SP, Oberjohn KS, et al. A pilot randomized trial of an online parenting skills program for pediatric traumatic brain injury: improvements in parenting and child behavior. Behav Ther. 2014;45(4):455–468. doi: 10.1016/j.beth.2014.02.003. [DOI] [PubMed] [Google Scholar]
- 38.Brown FL, Whittingham K, Boyd R, Sofronoff K. A systematic review of parenting interventions for traumatic brain injury: child and parent outcomes. J Head Trauma Rehabil. 2013;28(5):349–360. doi: 10.1097/HTR.0b013e318245fed5. [DOI] [PubMed] [Google Scholar]
- 39.Woods DT, Catroppa C, Eren S, Godfrey C, Anderson VA. Helping families tomanage challenging behaviour after paediatric traumatic brain injury (TBI): a model approach and review of the literature. Social Care Neurodisability. 2013;4(3/4):94–104. [Google Scholar]
- 40.Brown FL, Whittingham K, Boyd RN, McKinlay L, Sofronoff K. Improving child and parenting outcomes following paediatric acquired brain injury: a randomised controlled trial of Stepping Stones Triple P plus Acceptance and Commitment Therapy. J Child Psychol Psychiatry. 2014;55(10):1172–1183. doi: 10.1111/jcpp.12227. [DOI] [PubMed] [Google Scholar]
- 41.Babikian T, Asarnow R. Neurocognitive outcomes and recovery after pediatric TBI: meta-analytic review of the literature. Neuropsychology. 2009;23(3):283–296. doi: 10.1037/a0015268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Todis B, Glang A, Bullis M, Ettel D, Hood D. Longitudinal investigation of the post-high school transition experiences of adolescents with traumatic brain injury. J Head Trauma Rehabil. 2011;26(2):138–149. doi: 10.1097/HTR.0b013e3181e5a87a. [DOI] [PubMed] [Google Scholar]
- 43.Anderson V, Brown S, Newitt H, Hoile H. Long-term outcome from childhood traumatic brain injury: intellectual ability, personality, and quality of life. Neuropsychology. 2011;25(2):176–184. doi: 10.1037/a0021217. [DOI] [PubMed] [Google Scholar]