Abstract
Endoscopic ultrasound-guided biliary drainage (EUS-BD) has been increasingly reported as an alternative to percutaneous transhepatic biliary drainage in failed endoscopic retrograde cholangiopancreatography. Moreover, conversion to EUS-BD can be a good alternative when transpapillary biliary drainage is technically possible but complicated by cholangitis because EUS-BD enables one-step internal drainage not traversing the tumor. Herein, we report a case of recurrent cholangitis due to hemobilia and cholecystitis due to tumor involvement to the cystic duct after transpapillary stent placement, which was successfully managed by conversion to EUS-BD and EUS-guided gallbladder drainage in one session.
Keywords: Biliary drainage, endoscopic ultrasound, malignant biliary obstruction
INTRODUCTION
Although transpapillary stenting is the current standard treatment for malignant biliary obstruction (MBO), it can be sometimes complicated by recurrent cholangitis or cholecystitis due to a biliary stent traversing the tumor. Endoscopic ultrasound-guided biliary drainage (EUS-BD) is increasingly reported as an alternative to percutaneous transhepatic biliary drainage (PTBD) in failed endoscopic retrograde cholangiopancreatography (ERCP),[1] but EUS-BD has the potential advantage of internal drainage which does not traverse the tumor. We experienced a case of recurrent cholangitis and cholecystitis after transpapillary stent placement, which was successfully managed by conversion to EUS-BD and EUS-guided gallbladder drainage (EUS-GBD).
CASE REPORT
A 78-year-old female with MBO due to unresectable cholangiocarcinoma was referred to our hospital. Endoscopic retrograde cholangiography (ERC) revealed a friable tumor causing hilar MBO (Type 3a) extending to the orifice of cystic duct (OCD). An uncovered metal stent (Niti-S large cell D-type, Taewoong, Seoul, Korea) was placed [Figure 1], which was complicated by cholangitis due to hemobilia and cholecystitis due to the tumor involvement to OCD.[2] Five sessions of ERC with the left biliary system and gallbladder drainage were performed within 1 month for recurrent cholangitis/cholecystitis, and endoscopic nasobiliary and gallbladder drainage tubes were temporarily inserted [Figure 2] and cholangitis/cholecystitis resolved after the insertion of nasobiliary and gallbladder drainage. Then, we performed conversion to EUS-guided hepaticogastrostomy (EUS-HGS) and EUS-GBD as an alternative to PTBD, utilizing indwelling nasobiliary and naso-gallbladder drainage.
Figure 1.
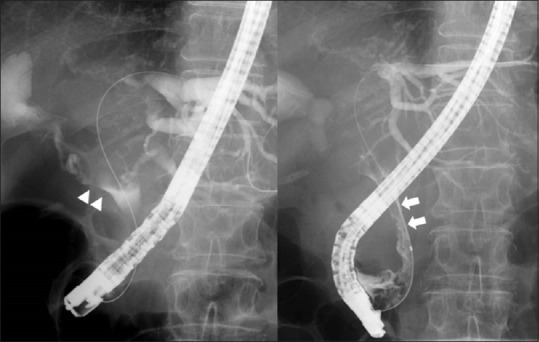
Endoscopic retrograde cholangiography revealed hilar biliary obstruction by a friable tumor with hemobilia. The tumor extended to the orifice of cystic duct (arrowhead) and was easy to bleed (arrow)
Figure 2.
A nasobiliary drainage tube and a naso-gallbladder drainage tube were placed for recurrent cholangitis and cholecystitis
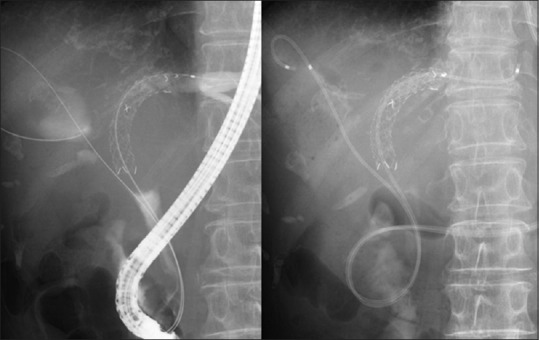
First, EUS-GBD was performed. After contrast injection through a naso-gallbladder tube, gallbladder was punctured with a 19-gauge needle from the duodenal bulb, followed by guidewire insertion. The fistula was dilated with a coaxial electric cautery, and then, two double pigtail stents were placed [Video 1]. Second, EUS-HGS was performed similarly utilizing a nasobiliary tube.[3] Left intrahepatic bile duct was punctured, and a partially covered metal stent was placed from B3 to the stomach[4] after fistula dilation by electric cautery [Figure 3 and Video 2]. After the procedure, cholangitis and cholecystitis were under control, and the patient survived 102 days after the procedure without further biliary events.
Figure 3.

Endoscopoic ultrasound-guided hepaticogastrostomy (a modified Giobor stent, 10 mm × 10 cm; Taewoong) and gallbladder drainage (two Zimmon® biliary stents, 7 Fr × 7 cm, Cook Japan, Tokyo) were performed in a single session
DISCUSSION
EUS-BD has been first reported as an alternative to PTBD in failed ERCP, but its indications have been expanding and it is now evaluated even as primary biliary drainage for MBO in clinical trials. The major reason for failed ERCP is inaccessible ampulla due to gastric outlet obstruction rather than failed cannulation, and EUS-BD demonstrated better outcomes than transpapillary stenting in patients with an indwelling duodenal stent. We believe that MBO refractory to transpapillary stenting can be also an expanded indication for EUS-BD. One of the advantages of EUS-BD over transpapillary stenting and PTBD is its ability of one-step internal drainage not traversing the tumor, and our case clearly illustrated the usefulness of this expanded indication, i.e., recurrent cholangitis due to hemobilia and recurrent cholecystitis due to tumor involvement to OCD.
Conversion to EUS-BD can be technically difficult because of an indwelling biliary stent, but as we previously reported, it can be safely performed utilizing a nasobiliary drainage tube. By placing a temporary nasobiliary tube, we can inflate the biliary system and guide the biliary puncture both on EUS and fluoroscopy by injecting contrast through this tube. In our case, we used both ENBD and ENGBD to facilitate a single session conversion to EUS-BD and EUS-GBD.
A recently developed, lumen-apposing metal stent (LAMS) is preferred for EUS-GBD because of a simple procedure with less risk of bile leak. However, a LAMS is not currently available in Japan, and we selected double pigtail stents rather than tubular-covered metal stents to avoid stent migration.
In summary, MBO refractory to transpapillary stenting can be an expanded indication for EUS-BD even if ERCP is technically possible, and conversion to EUS-BD is feasible using a nasobiliary tube.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understand that her name and initial will not be published and due efforts will be made to conceal her identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Videos Available on: www.eusjournal.com
REFERENCES
- 1.Khashab MA, Levy MJ, Itoi T, et al. EUS-guided biliary drainage. Gastrointest Endosc. 2015;82:993–1001. doi: 10.1016/j.gie.2015.06.043. [DOI] [PubMed] [Google Scholar]
- 2.Isayama H, Kawabe T, Nakai Y, et al. Cholecystitis after metallic stent placement in patients with malignant distal biliary obstruction. Clin Gastroenterol Hepatol. 2006;4:1148–53. doi: 10.1016/j.cgh.2006.06.004. [DOI] [PubMed] [Google Scholar]
- 3.Nakai Y, Isayama H, Yamamoto N, et al. Conversion to EUS-guided biliary drainage by temporary nasobiliary drainage placement in patients with prior biliary stenting? Endosc Ultrasound. doi: 10.4103/2303-9027.199763. DOI:10.4103/2303-9027.199763. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nakai Y, Isayama H, Yamamoto N, et al. Safety and effectiveness of a long, partially covered metal stent for endoscopic ultrasound-guided hepaticogastrostomy in patients with malignant biliary obstruction. Endoscopy. 2016;48:1125–8. doi: 10.1055/s-0042-116595. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


