Abstract
MicroRNAs (miRNAs or miRs) and the target genes before and after warm acupuncture at the genetic level were assessed, and the cytokines and neurotransmitters related to insomnia were studied. Male Sprague-Dawley rats were used to create PCPA insomnia rat models and randomly divided into the normal, model, warm acupuncture, and drug groups. The Dinghui Acupoint, Heyi Acupoint, and Xin Acupoint were inserted in the Mongolian medicine warm acupuncture group. The differential expression profile of microRNA in the brain tissue of the insomnia rats was determined before and after Mongolian medicine warm acupuncture for establishment of miR-101a mimics and inhibitor. qPCR was used to detect the expression level of miR-101a. Western blotting was used to detect the expression level of PAX8. The rats receiving Mongolian medicine warm acupuncture had 141 miRNAs with differential expression compared with the normal rats. The expression level of miR-101a in the cells of the hippocampus of the insomnia rats transfected with miR-101a mimics increased significantly at 72 h (P<0.05). The activity of the neuronal cells transfected with miR-101a inhibitor increased significantly at 72 h (P<0.05). The western blotting result indicated that the expression of the PAX8 protein in the neuronal cells of the insomnia model rats was inhibited and downregulated significantly at 72 h after addition of miR-101a mimics compared with that in the scramble added group (P<0.01). The levels of the interleukins IL-1, IL-2, and IL-6 and the tumor necrosis factor-α in the hypothalamus, hippocampus, and prefrontal cortex decreased significantly compared with those in the blank control group (P<0.05). The levels of noradrenaline, dopamine, and glutamic decreased significantly following warm acupuncture or western medicine treatment (P<0.05). In conclusion, this study demonstrates that the upregulation of miR-101a in the rats treated with warm acupuncture is directly associated with PAX8 regulation.
Keywords: warm acupuncture, insomnia, miR-101a, Mongolian medicine
Introduction
Insomnia is a subjective experience characterized by a difficulty in falling asleep and/or staying asleep, which results in the failure of sleep quality or quantity to meet an individual's normal physiological needs and affects their social functions. It is the most common sleep disorder with very high rates of morbidity (1). According to an investigation by the World Health Organization, ~1/3 of the world's population suffers from sleep disorders (2). The percentage of people with various types of sleep disorders in China is significantly higher (35%) than the rest of the world (27%). Thus, effective prevention and treatment of insomnia is a main focus of research in the world (3).
In clinical treatment, hypnotics are primarily used in modern medicine. This drug treatment may be accompanied by many side effects. It is not an ideal therapeutic regimen due to its poor long-term efficacy and addiction, and tolerance, in the case of long-term administration (4). Mongolian medicine has a unique mechanism and good efficacy in treatment of insomnia. In Mongolian medicine, it is believed that the imbalance among Heyi, Xila, and Badagan, predominance of Heyi in the heart and white meridian, and Heyi blood intermingling arising from dysfunctions are the basic etiology and pathogenesis. Such negative emotions as tension, worry, fear, depression and anxiety; and social environment, diet, daily life and movement conditions are external factors. In the Mongolian medicine, the treatment of insomnia mainly focuses on relieving Heyi and regulating Heyi, Xila, and Badagan (5–7). The warm needling therapy is one of most common methods for the treatment of insomnia in Mongolian medicine as it functions in warming and smoothing meridians, regulating qi and blood, regulating voxels, enhancing immunity, and preventing and treating diseases. It is widely accepted way of treatment by the patients due to such characteristics as high efficiency, safety, no side effects, simplicity and no drug dependence (8). Thus, the warm needling therapy has considerable advantages in the treatment of insomnia, such as significant efficacy, safety, simplicity, and economy.
Our study first investigates the role of the Mongolian medical warm acupuncture in hypnotizing the PCPA-induced insomnia models. We also discuss the levels of related microRNAs (miRNAs or miRs) and target genes before and after warm acupuncture. Finally, we observed the insomnia-related cytokines and neurotransmitter content, probed into the biological foundation of Mongolian medical warm acupuncture in treating insomnia in combination with the clinical tests, and preliminarily explain the multi-dimension complex mechanism of the Mongolian medical warm acupuncture.
Materials and methods
Rat modeling and grouping
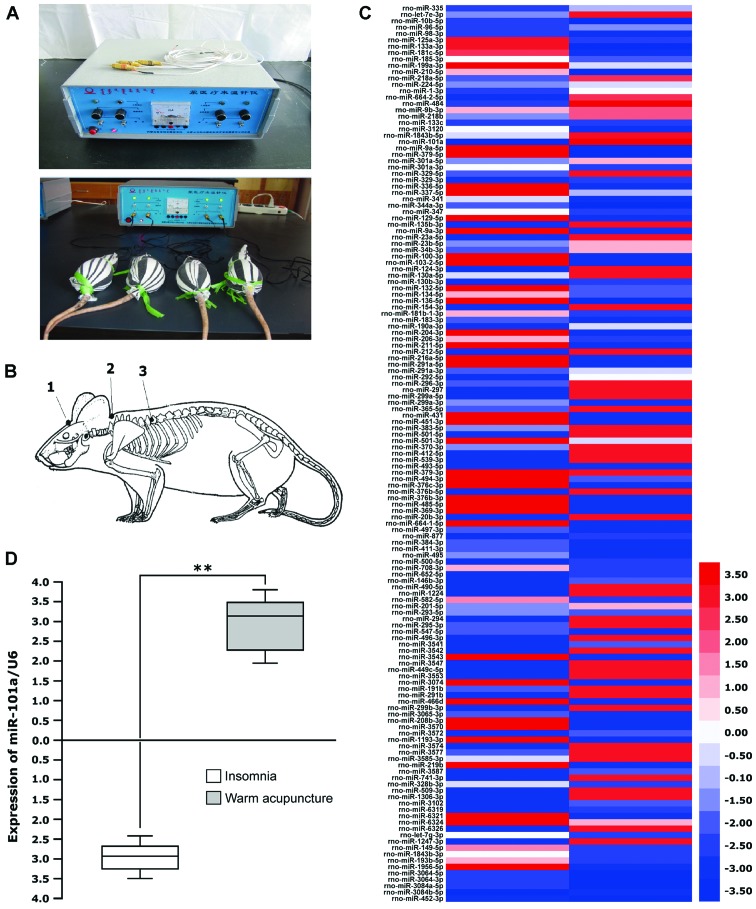
Experimental apparatus of the Mongolian medicine Model MY-I electric heating needle warmers (patent no. ZL 2011 2 0058078.0) (Fig. 1A) and sterile Mongolian medicine silver needles were produced by Inner Mongolia Medical University (Hohhot, China). Experimental animals and modeling A of a total of 60 clean Sprague-Dawley rats weighing 160–180 g (provided by the Laboratory Animal Center of Inner Mongolia University) were raised adaptively for 7 days and then intraperitoneally injected with PCPA (Lanbote, Beijing, China) at a dose of 300 mg/kg between 8:30-9:00 a.m. each day for 2 consecutive days at the 8th day for establishing models of insomnia rats. PCPA was dissolved with normal saline (pH 7.0–8.0) and made into a suspension as per l ml/100 g.
Figure 1.
Digital expression profile of miR-101a. (A) Mongolian medicine electric heating needle warmers and rat acupuncture bag. (B) Selection of acupuncture points, 1 is the Dinghui Acupoint, 2 is the Heyi Acupoint, 3 is the Xin Acupoint. (C and D) A high throughput analysis is conducted for the expression of miRNA in the brain tissue of the insomnia rats receiving Mongolian medical warm acupuncture and the brain tissue of the insomnia rats receiving no treatment with the digital miRNAs expression profile method. The miRNAs with expression changed significantly are identified in the liver cancer. Red represents upregulation and blue represents downregulation. The insomnia rats receiving warm acupuncture and the insomnia rats receiving no warm acupuncture were subjected to determination by qPCR. The median is −2.9 times in the treatment group and the median is 3.2 times in the non-treatment group (**P<0.01).
The evaluation of the PCPA insomnia rats were as follows: significantly frequent activities, abnormal sensitivity to such stimulus as sound and light, strengthened excitability, enhanced aggressiveness, greyish white excrement, circadian rhythm disorders and frequent daytime activities, occurred to the rats at 28–30 h after the second intraperitoneal injection of PCPA, which indicated that the models were successfully established (9). This study was approved by the Animal Ethics Committee of Inner Mongolia Medical University.
The Sprague-Dawley rats were divided into 4 groups randomly, the normal, model, warm acupuncture and medication groups of 15 rats each. In the normal group, the rats were adaptively raised for 7 days and intraperitoneally injected with normal saline (0.l ml/kg) for 2 consecutive days from the 8th day. The rats were also fed twice at a fixed time for 1 h each day without any other stimuli. In the model group, the rats were adaptively raised for 7 days and intraperitoneally injected with PCPA (300 mg/kg) in the morning of each day for 2 consecutive days from the 8th day in order to establish insomnia rat models without any other stimuli. In the warm acupuncture group, the rats were adaptively raised for 7 days and intraperitoneally injected with normal saline (0.l ml/kg) between 8:30-9:00 a.m. each day for 2 consecutive days from the 8th day. The Dinghui Acupoint, Heyi Acupoint, and Xin Acupoint of each rat was stimulated with warm acupuncture for 15 min each time (Mongolian Model MY-I electric heating needle warmers) at ~40°C (be careful not to burn the needling site) once each day for 7 consecutive days starting from the 10th day. In the medication group, the rats in the model group were adaptively raised for 7 days and intraperitoneally injected with diazepam (batch no. 20150126; North China PharmaceuticaL Co., Ltd., Shijiazhuang, China) once a day at a dose of 0.92 mg/kg/day for 7 consecutive days.
Criteria for acupoint selection and acupoints
The criteria for the normal warm acupuncture group and model + warm acupuncture group are as follows: The effective acupoints were selected on the basis of the classic theory of Mongolian medicine and clinical treatment (Fig. 1B). Acupoints: i) Dinghui Acupoint refers to the intersection between the line drawn above the middle of the two eyebrows and the line drawn above the middle of the superior margins of the two lobes, i.e., Baihui Acupoint in traditional Chinese medicine. The acupoint was stimulated to alleviate ‘Heyi hoarseness’, daftness, visual deterioration, dizziness and headache. ii) Heyi Acupoint is located at the center of the superior fovea of first thoracic vertebrae and stimulated to treat such Heyi diseases as daftness, palpitation, agitation, stammer, staying awake at night, pale coated tongue and neck rigidity. iii) Xin Acupoint is located at the center of the inferior fovea of seventh thoracic vertebrae and stimulated to treat palpitation, atrial fibrillation, daftness, ‘Badagan and Heyi’ heart diseases, insomnia, delirium, anorexia and delirium (10).
Sampling method
The rats in the normal, model, and warm acupuncture groups were decollated. The prefrontal cortex, hypothalamus, and hippocampus of each rat were removed quickly on ice, weighed, and preserved at −70°C.
Determination of the differential expression profile of microRNA in the brain tissue of the insomnia rats before and after Mongolian medical warm acupuncture
Analysis of the microRNA expression profile
The brain tissue of the insomnia rat model and the rats receiving warm acupuncture was collected. The total RNA was extracted using the TRIzol reagent. The miRNAs chip was used to analyze the expression profiles of miRNAs in the cells of both groups.
The principle of the miRNAs chip technology are as follows: The miRNAs in the specimens to be tested are collected and hybridized with the complementary probes on specific chips. The miRNAs 3′ terminal end in the specimens to be tested are usually marked with fluorescence groups. The fluorescence intensity could be scanned after hybridization and non-specific elution. The miRNAs with significant differential expression can be screened following substantial data processing. The significance of changes in miRNA expression was determined by screening for possible target miRNAs. The differential expression of miRNAs was detected using the stem-loop real-time quantitative RT-PCR method using the special miRNAs quantitative detection kit (Guangzhou RiboBio Co., Ltd., Guangzhou, China).
Prediction and verification of the biological information of the target gene in the differentially expressed miRNAs
The prediction of biological information of target genes of miRNAs was done using the online budget software. It primarily uses the following three types of software: TargetScan, PicTar, and miRanda. The eukaryotic expression carrier was established for the differential miRNAs. Bioinformatics was used to predict and verify whether the target molecules of miRNAs include PAX8. The miRNAs closely associated with target molecules that served as the research subject.
miR-101a mimics and inhibitor
miR-101a inhibitor was the reverse complementary sequence of the miR-101a mature individuals and performed 2′-O-methyl modification for all basic groups. The negative control (scramble) of the miRNA inhibitor was a sequence that does not match with any known human miRNA sequence. All of them were synthesized by the Guangzhou RiboBio Co., Ltd. The miR-101a sequence mimics were (5′-TCCCCCGGGCCAGAGGTTGTAACGTTGTCTAT-3′); miR-101a inhibitor sequence (5′-GAAACCCAGCAGACAAAGCTTTGTTGCCTAACGAAC-3′); and internal reference U6snRNA (5′-CACCACGTTTATACGCCGGTG-3′).
Real-time fluorescent quantitative PCR detection of the expression levels of miR-101a in the brain tissue of rats in the warm acupuncture treatment group
Reverse transcription of miRNAs
Small molecular RNA (1 µg) was diluted to 10 µl. A total of 2 µl of the RT primer working solution and 4.5 µl of DEPC water were added. The mixture was denatured for 5 min at 72°C and quickly cooled on ice. After the addition of the following reverse transcription components (the above mixture; 5 µl of 5X buffer, 2.5 µl 10 mM dNTP, 0.5 µl RNase inhibitor and 1.0 µl ReverTra Ace). The solution was reacted for 1 h at 42°C and for 5 min at 95°C, cooled on ice, and then preserved.
SYBR ExTaq Mix quantitative PCR amplification was performed for the expression of miR-101a in brain tissue of the warm acupuncture rats, insomnia model rats, and normal control rats. U6 was amplified for the internal reference control. The reaction system was as follows: 12.5 µl of SYBR ExTaq Mix II (Guangzhou RiboBio Co., Ltd.), 1 µl of upstream primer, 1 µl of downstream primer, 2 µl of cDNA template, and 8.5 µl of dH2O. The reaction conditions were as follows: 95°C for 10 sec, 95°C for 5 sec; 58°C for 30 sec, microplate reading at 72°C for 30 sec, microplate reading for 30 cycles at 72°C for 10 min, 55°C for 5 min, the solubility curve 55–95°C, and 0.3°C/microplate reading for 1 sec. U6 served as the internal reference gene. The relative expression of the target gene was calculated using formula 2−ΔΔCq (11).
Detection of the expression levels of PAX8 with western blotting
The brain tissue of rats in the blank control, insomnia model, and warm acupuncture groups were collected, respectively. The histocytes were lysed and the cytoplasm and nuclear protein supernatant were extracted for a SDS-PAGE gel. The wet transfer method was used after it was electrophoresed for 2 h at a constant voltage of 120 V. It was electrically transferred onto the PVDF membrane, immersed in TBST blocking buffer containing 5% skim milk for 1 h at room temperature, and rinsed with TBST. The primary antibody was added (Beyotime Biotech, Nanjing, China) and vibrated overnight at 4°C. It was then rinsed several times with TBST solution. After addition of the rabbit anti-human related polyclonal antibody (Beyotime Biotech), it was vibrated for 1 h and rinsed 3 times. The PAX8 level was detected after ECL development.
Culture of neurocytes of adult rats
After the rats were euthanized, the hippocampus was separated under the microscope to remove the meninges and blood vessels. They were rinsed 3 times with the D-Hank's solution (Beyotime Biotech), cut into milky fluid-type pieces and digested in the CD-Hank'S-dispase-DNase-papin (DDDP) (Beyotime Biotech) at 37°C. The DMEM/F12 containing 10% fetal bovine serum (FBS) was added to terminate the digestion. The solution was centrifuged for 5 min at 600 × g; the supernatant was discarded. Cells were re-suspended with DMEM/F12 containing 10% FBS and inoculated into a culture flask containing poty-omithine (10 µg/m1) and laminin (5 µg/m1). The solution was replaced by serum-free DMEM/F12 cell culture medium at 24 h. In addition, 1% N2, 2% B27, and 20 ng/ml EGF and bFGF (mesenchymal stem cell medium, SCM) were added. When the cells grew to 80–90% confluency, they were digested with Acctuase (Beyotime Biotech) for passaging and inoculated into a new culture flask in the ratio of 1:3. HPCs were digested into a single-cell suspension and inoculated in the culture plate or culture dish containing poly-omithine (50 µg/m1) and laminin (10 µg/m1). In order to improve cell survival, the media was changed to differential medium (DMEM/F12, 1 ng/ml bFGF, 1% FBS, 100 nmol/l retinoic acid (Beyotime Biotech) at 24 h after cell adherence; the solution was changed every 2 days. The cells were differentiated for 14 days and then turned into neuronal cells (12).
Dual-luciferase reporter gene experiments
Results indicated that miR-101a might have a targeted-regulating relationship with the PAX8 gene after the bioinformatic prediction of the miRNA target gene using the on-line budgeting software TargetScan, PicTar, and miRanda. The luciferase reporter gene plasmid containing PAX8 3′UTR (Applied Biosystems, Foster City, CA, USA) was established. The eukaryotic expression plasmid of the miR-101a gene and the luciferase reporter gene plasmid containing 3′UTR was used to co-transfect the HEK293 cells. A luciferase dual reporter gene experiment was conducted to identify the target relationship between miR-101a and PAX8. The luciferase reporter vector pMIR-Report™ was purchased from the Applied Biosystems.
Luciferase activity experiment
The 3 groups of neuronal cells were inoculated into a 24-well microplate with 5×104 cells/well and transfected with calcium phosphate at 24 h. All types of required DNA were transfected. The receptor expression vector and the scramble, miR-101a mimics/inhibitor expression plasmids containing the luciferase reporter gene were transfected into the cells. The media was discarded. Cells were washed once with PBS and 120 µl of lysis buffer was added to each well. It was centrifuged for 5 min at 9,500 × g. The supernatant was collected. A total of 20 µl of cell lysis buffer was well mixed with 10 µl of luciferase detection reagent. Spectrafluo plus was used to detect the fluorescence signal and the ratio between the fluorescence value and the corresponding OD value of the B-gal galactosidase was the relative activity of the calibrated luciferase.
Detection of related cytokines, neurotransmitters, and receptors
The enzyme-linked immunosorbent assay (ELISA) (BioSino Bio-Technology and Science Inc., Beijing, China) was used to detect the levels of the interleukins of IL-1, IL-2, and IL-6 and the tumor necrosis factor-α (TNF-α) at the above sites. Detection of monoamine neurotransmitters in the brain tissue was conducted using the high performance liquid chromatography-electrochemical detection method to determine the levels of noradrenaline (NE), dopamine (DA), 5-hydroxytryptamine (5-HT), glutamic (Glu) acid, and γ-aminobutyric acid (GABA). The high performance post-column derivatization-electrochemical detector method was used to determine the level of acetylcholine (Ach) (BioSino Bio-Technology and Science Inc.).
Statistical analysis
SAM and TIGR Multiple Array Viewer software package (TMeV version 4.0) (J. Craig Venter Institute, La Jolla, CA, USA) were used to conduct an unsupervised cluster analysis for the miRNAs chip expression profile. The fluorescent real-time quantitative PCR detection used the Sequence Detection system (SDS) 2.3 software for data analysis. The expression level of miRNAs were expressed with the ΔCq value (Cq miRNA-Cq U6). The biological experimental data were expressed with mean ± standard deviation. The intergroup difference between the groups was subject to Student's t-test. The comparison of intergroup enumeration data used the Chi-square test or the Fisher's exact probability method. P<0.05 was considered to indicate a statistically significant difference. The difference was considered remarkably statistically significant when P<0.01. The statistical analysis was conducting using the SPSS 18.0 software (SPSS, Inc., Chicago, IL, USA).
Results
Differences in expression of miR-101a in the brain tissue before and after treating the rats for insomnia with Mongolian medical warm acupuncture
Based on analysis of the chip data, it was found that differences were present in the expression of 141 miRNAs after the Mongolian medical warm acupuncture compared to the normal rats (Fig. 1C). Changes in miR-101a were the most significant and increased 98 times compared to that of the model group. Then, we conducted a fluorescent real-time quantitative PCR study on the levels of miR-101a in 15 insomnia rats receiving warm acupuncture. It was found that the median increased to 3.2 times from the −2.9 times in the model group (P<0.001; Fig. 1D).
Expression of miR-101a in the hippocampus before and after treating the insomnia rats with Mongolian medical warm acupuncture
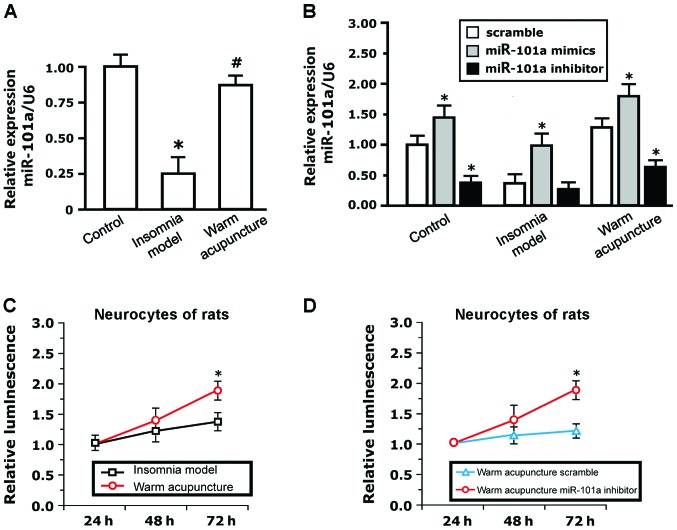
To study the biological functions of miR-101a, fluorescent real-time quantitative PCR was used to detect the expression of miR-101a in the hippocampus before and after treatment of the insomnia rats with Mongolian medical warm acupuncture. The results indicated that the expression levels of miR-101a in the brain tissue of rats in the insomnia model group decreased significantly compared to that in the brain histiocytes of normal rats (P<0.05). The expression levels of miR-101a increased significantly and approximated the normal value following warm acupuncture (P<0.05; Fig. 2A). The expression of miR-101a in the blank neurocytes transfected with miR-101a mimics increased significantly at 72 h (P<0.05) compared to that in the negative control group. The expression of miR-101a in the blank neurocytes transfected with miR-101a inhibitor decreased significantly at 72 h (P<0.05; Fig. 2B). The expression of miR-101a in cells transfected with miR-101a mimics at 72 h in the insomnia model group increased significantly (P<0.05) compared to that in the negative control group. The expression of miR-101a in cells transfected with miR-101a inhibitor at 72 h in the insomnia model group had no significant changes (Fig. 2B). The expression of miR-101a in cells transfected with miR-101a mimics increased significantly at 72 h (P<0.05) following Mongolian medical warm acupuncture compared to that in the negative control group. The expression levels of miR-101a in cells transfected with miR-101a inhibitor decreased significantly (P<0.05; Fig. 2B).
Figure 2.
Experimental verification of regulation of neurocytes of rats with exogenous miR-101a molecules. (A) The expression levels of miR-101a in the neurocytes cultured in vitro in the blank control, insomnia model, and warm acupuncture groups are detected with the fluorescent real-time quantitative PCR technique. The expression level decreases significantly in the insomnia model group (*P<0.01) and increases significantly in the warm acupuncture group (#P<0.01); (B) the neurocytes of the rats in the three groups cultured in vitro are transfected with miR-101a inhibitor and mimics. They exhibit positive and negative dependence expression except for the insomnia model mimics group; (C) the neurocytes of the rats in the warm acupuncture group cultured in vitro show strong viability at 24 h and significant viability at 48 h compared with those in the insomnia model group (*P<0.05); (D) the neurocytes of the rats in the warm acupuncture group cultured in vitro are transfected with the blank plasmid and the miR-101a inhibitor. The inhibitor inhibits the viability of the cells at 24 h and significantly inhibits the viability of the neurocytes at 48 h compared with the control group (*P<0.05).
There were no differences in the luciferase activity of neuronal cells cultured in vitro between the model group and the Mongolian medical warm acupuncture group within the initial 24 h. The cell activity in the Mongolian medical warm acupuncture group increased compared to that in the model group at 48 h. The cell activity in the Mongolian medical warm acupuncture group increased significantly compared to that in the model group at 72 h (P<0.05; Fig. 2C). In order to further verify the effects of miR-101a on the activity of the neurocytes, the neuronal cells of the rats receiving Mongolian medical warm acupuncture were transfected with miR-101a inhibitor and scramble control. As seen in Fig. 2D, the activity of the cells transfected with miR-101a inhibitor was higher at 48 h compared to the activity of the cells transfected with scramble. The activity of cells transfected with miR-101a inhibitor increased significantly at 72 h (P<0.05).
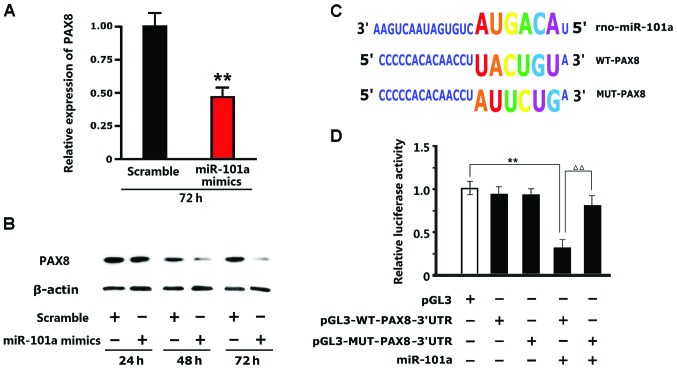
miR-101a inhibits the expression of the PAX8 protein
The results of western blotting indicated that the expression of the PAX8 protein in the neuronal cells of the insomnia model rats cultured in vitro with miR-101a mimics added was inhibited and downregulated significantly (P<0.01) compared to the expression of the PAX8 protein in the neuronal cells of the insomnia model rats cultured in vitro with scramble control (Fig. 3A and B). The results of luciferase in the 293T cells indicated that pGL3M-MUT-PAX8-3′UTR and pGL3M-WT-PAX8-3′UTR in the negative control group had no significant changes compared with pGL3M in the blank plasmid group. After addition of miR-101a mimics, no significant changes occurred to the activity in the MUT group while the fluorescence intensity in the WT group decreased significantly. This indicated that miR-101a can bind to the specific sequence in the WT-PAX8-3′UTR promoter and change the specific sequence of the promoter whereas miR-101a does not function (Fig. 3C and D).
Figure 3.
miR-101a inhibiting the expression of the (A and B) PAX8 protein. Western blotting results of the neurocytes of the rats in the warm acupuncture group cultured in vitro indicate that the PAX8 protein is significantly downregulated at 72 h after addition of miR-101a mimics (**P<0.01); (C) WT-PAX8 and MUT-PAX8 plasmid design; (D) the luciferase report results of the 293T cells indicate that there are no significant changes in pGL3M-MUT-PAX8-3′UTR and pGL3M-WT-PAX8-3′UTR in the negative control group compared with blank control group pGL3M. After addition of miR-101a mimics, there are no significant changes in the activity in the MUT group while the fluorescence intensity in the WT group decreased significantly (**P<0.01; ΔΔP<0.01).
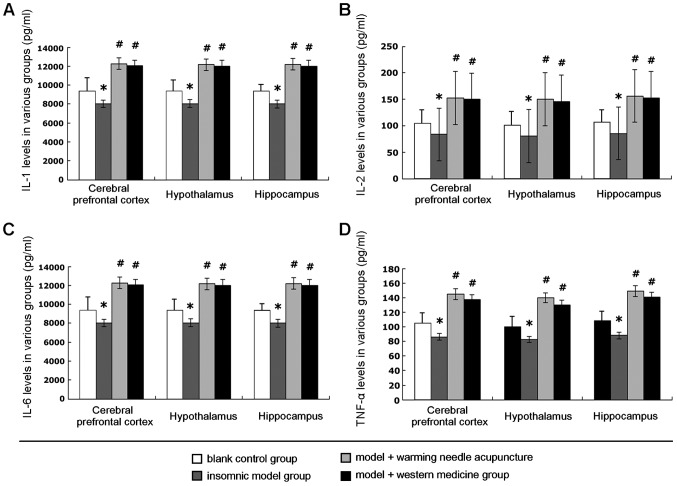
Detection of the levels of IL-1, IL-2, IL-6, and TNF-α
The results of detection of levels of interleukin IL-1, IL-2, and IL-6, and TNF-α are shown in Fig. 4. The levels of interleukins IL-1, IL-2, and IL-6 and TNF-α in the hypothalamus, hippocampus, and prefrontal cortex tissue of the insomnia rats decreased significantly compared with those in the blank control group; differences were significant (P<0.05). After treatment with warm acupuncture or western medicine, the levels of the interleukins IL-1, IL-2, IL-6, and TNF-α at various sites increased significantly compared to those in the model group; there were statistical differences (P<0.05). Results indicate that warm acupuncture had significant efficacy in treatment of insomnia rats. Its basic efficacy was equivalent to that of the drug treatment.
Figure 4.
Levels of (A) interleukin (IL)-1, (B) IL-2, (C) IL-6, and (D) tumor necrosis factor (TNF)-α in the hypothalamus, hippocampus, and prefrontal cortex tissue of the rats. There is a significant difference between the insomnia model and the blank control groups, *P<0.05; #there is a significant difference between the warm acupuncture group and the insomnia model group, *P<0.05.
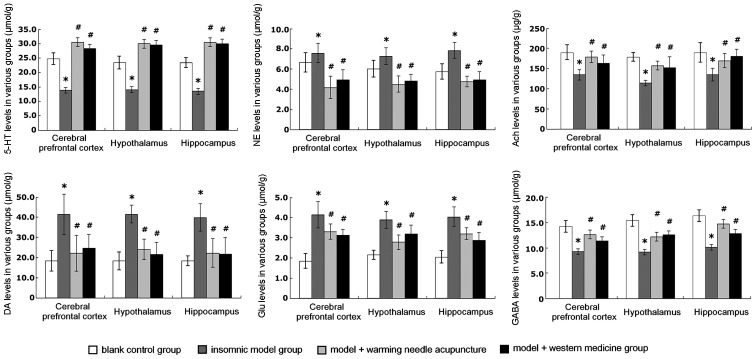
Detection of the levels of 5-HT, NE, Ach, DA, Glu, and GABA
The results of the levels in the hypothalamus, hippocampus, and prefrontal cortex tissue of the rats are shown in Fig. 5. The detection results indicated that the levels of NE, DA, and Glu of the rats in the insomnia model group were significantly higher than those in the blank control group (P<0.05). After warm acupuncture or treatment with western medicine, the levels of NE, DA, and Glu decreased significantly compared to those in the insomnia model group; differences were statistically significant (P<0.05). The difference in efficacy between warm acupuncture treatment and western medicine treatment was not significant, indicating that the treatment outcomes were not different. The levels of 5-HT, GABA, and Ach of the rats in the insomnia model group were significantly lower than those in the blank control group; there was a statistically significant difference (P<0.05). The levels of 5-HT, GABA, and Ach of the insomnia rats increased significantly after warm acupuncture or western drug treatment compared to those in the insomnia model group. There was a statistically significant difference (P<0.05). No significant difference was observed between the warm acupuncture and western drug treatment, demonstrating that the treatment outcome of Mongolian medical warm acupuncture was similar to the outcome of western drug treatment.
Figure 5.
Levels of 5-hydroxytryptamine (5-HT), noradrenaline (NE), acetylcholine (Ach), dopamine (DA), glutamic (Glu), and γ-aminobutyric acid (GABA in the hypothalamus, hippocampus, and prefrontal cortex of the rats. There is a significant difference between the insomnia model group and blank control group, *P<0.05; #there is a significant difference between the warm acupuncture group, drug treatment group, and the insomniamodel group, *P<0.05.
Discussion
In the Mongolian medical warm acupuncture therapy, patients are subject to the insertion of special silver needles into fixed acupoints and warming moxibustion for the prevention and treatment of diseases and recovery of patients. The acupuncture effect, hyperthermia effect, and specific stimulation of acupoints are combined to produce some biological effects for treatment of diseases (13). A great deal of clinical research indicates that Mongolian medical warm acupuncture is simple, efficient, and safe in the treatment of insomnia (14).
Mongolian medicine can improve sleep and treat insomnia by alleviating Heyi, circulating Heyi blood, and balancing Heyi, Xila, and Badagan (15). In the Mongolian medicine, it is believed that the warm needling therapy can dredge the meridians, regulate qi and blood, voxel, and strengthen the immunity. Modern research demonstrates that acupuncture plays a role in regulating neurohumor, strengthening and activating the anti-disease ability, and improving the immunity of the organism. It is a good choice for insomnia patients. There are many clinical reports on the treatment of insomnia with Mongolian medical warm acupuncture (16). The Mongolian medical warm acupuncture therapy is used in all of these clinical reports. The Dinghui Acupoint, Heyi Acupoint, and Qianding Acupoint are largely selected for the treatment of insomnia with acupuncture and satisfactory efficacy is achieved. It is thus clear that Mongolian medical warm acupuncture is very efficacious in treating insomnia (17).
There is no uniform criteria for the quantitative and qualitative assessment of the acupuncture treatment indexes in traditional Mongolian medicine. The investigation of the indexes of several neurotransmitters does not completely represent the physiological indexes of the whole organism and conform to the holistic concept in the Mongolian medicine theory. As the acupuncture mechanism is very complex, it is difficult to analyze and master the mechanism from a physiological point-of-view. However, the changes in miRNA levels in an organism can be determined in a standard and objective manner. Thus, studying Mongolian medical warm acupuncture with miRNA levels as the medium can embody the macroscopic and integral characteristics and conform to the microcosmic and targeted characteristics of the modern molecular biological techniques (18).
The expression levels of miR-101a in the Mongolian medical warm acupuncture treatment group is increased compared to the insomnia rat model group. Transfection of miR-101a inhibitor can successfully decrease the expression of endogenous miR-101a in cells. It can be inferred that the target gene of miR-101a may be the paired box gene 8, PAX8 (19) through anylsis by the TargetScan, PicTar and miRanda software. In 2014, researchers investigated >47,000 Europeans and ~5,000 African-Americans. Researchers compared their genetic information and the time for falling asleep at night and results have shown that the sleep mode is influenced by the genetic difference. A certain gene region may influence the sleep mode by regulating the thyroid hormone levels. This DNA region is close to the PAX8 gene, which is associated with the development and functions of the thyroid gland (20). Patients with hypothyroidism are prone to drowsiness and patients with thyroid hyperfunction may suffer from insomnia. We discovered that the principle of Mongolian medical warm acupuncture in improving insomnia is directly associated with the role of miR-101a in the regulation of the PAX8 gene.
In modern medicine, research on insomnia has shown that the sleep-wake up cycle is a physiological process involving coordination and integration of multiple systems and centers with a complex regulatory mechanism. It is primarily associated with such structures as sleep activated cells of the preoptic region of the reticular system of the brain stem, histaminergic neurons in the papilla nodule region and cerebral cortex. The neurotransmitters closely associated with the wakeup-sleep cycle such as GABA, Ach, 5-HT, DA, NE, histamine and orexin; IL-1 and TNFs have sleep regulation roles, and non-peptide substances aid in regulating sleep (21–23). Furthermore, we also demonstrated that treating insomnia with Mongolian medical warm acupuncture is also associated with the above neurotransmitters.
Mongolian medical warm acupuncture integrates acupuncture effect, hyperthermia, and acupoint specific stimulation and achieves organism regulation and disease treatment via the complex multi-system, multi-channel, and multi-path mechanism relevant to blood circulation, nervous system and immune function (24). Our study demonstrates that the upregulation of expression of miR-101a is directly associated with PAX8 regulation in treating rats with warm acupuncture. Our study verifies multiple neurotransmitter regulation networks which provide biological research demonstration for modern treatment with Mongolian medical warm acupuncture and scientific support for the modernization development of the traditional national medicine.
Acknowledgements
This study was funded by the following projects: National Natural Science Foundation of China (no. 81560801); Science and Technology Innovation Fund of Provincial Department of Finance, Inner Mongolia Autonomous Region; Collaborative Innovation Project of Mogolian Medicine, Inner Mongolia Autonomous Region; Technology Reserve Project of Provincial Department of Science and Technology, Inner Mongolia Autonomous Region. Inner Mongolia Autonomous Region Mongolian Medicine Cooperative Innovation Project. Inner Mongolia Autonomous Region ‘Prairie excellence’ Project.
References
- 1.Vgontzas AN, Fernandez-Mendoza J, Liao D, Bixler EO. Insomnia with objective short sleep duration: The most biologically severe phenotype of the disorder. Sleep Med Rev. 2013;17:241–254. doi: 10.1016/j.smrv.2012.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.e Silva JA Costa, Chase M, Sartorius N, Roth T. Special report from a symposium held by the World Health Organization and the World Federation of Sleep Research Societies: an overview of insomnias and related disorders - recognition, epidemiology, and rational management. Sleep. 1996;19:412–416. doi: 10.1093/sleep/19.5.412. [DOI] [PubMed] [Google Scholar]
- 3.Wang YM, Chen HG, Song M, Xu SJ, Yu LL, Wang L, Wang R, Shi L, He J, Huang YQ, et al. Prevalence of insomnia and its risk factors in older individuals: A community-based study in four cities of Hebei Province, China. Sleep Med. 2016;19:116–122. doi: 10.1016/j.sleep.2015.10.018. [DOI] [PubMed] [Google Scholar]
- 4.Han KH, Kim SY, Chung SY. Effect of acupuncture on patients with insomnia: Study protocol for a randomized controlled trial. Trials. 2014;15:403. doi: 10.1186/1745-6215-15-403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen YS, Lu J, Su-Chao LM, Wu QZ, Tu Y, Bo A. Effects of electro-warmed needle of inner-Mongolian medicine on serum TNF-alpha, ACTH and corticosterone contents in fatigue rats. Zhen Ci Yan Jiu. 2008;33:258–261. (In Chinese) [PubMed] [Google Scholar]
- 6.Lu J, Chen YS, A GL, Tu Y. Effects of electric mildly-warmed needle of inner mongolian medicine on liver MDA and GSH content, GSH-Px and SOD activity in fatigue rats. Zhen Ci Yan Jiu. 2007;32:167–169. (In Chinese) [PubMed] [Google Scholar]
- 7.Kim TH, Jung SY. Mongolian traditional-style blood-letting therapy. J Altern Complement Med. 2013;19:921–924. doi: 10.1089/acm.2012.0752. [DOI] [PubMed] [Google Scholar]
- 8.Bao HS. Research of Zhanbra Dorje's contribution on the development of Mongolian medicine. Zhonghua Yi Shi Za Zhi. 2010;40:29–32. (In Chinese) [PubMed] [Google Scholar]
- 9.Murray NM, Buchanan GF, Richerson GB. Insomnia Caused by Serotonin Depletion is Due to Hypothermia. Sleep. 2015;38:1985–1993. doi: 10.5665/sleep.5256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Si LG, Wang YH, Wuyun G, Bao LD, Bo A. The effect of Mongolian medical acupuncture on cytokines and neurotransmitters in the brain tissue of insomniac rats. Eur J Integr Med. 2015;7:492–498. doi: 10.1016/j.eujim.2015.05.008. [DOI] [Google Scholar]
- 11.Sun X, Luo S, He Y, Shao Y, Liu C, Chen Q, Cui S, Liu H. Screening of the miRNAs related to breast cancer and identification of its target genes. Eur J Gynaecol Oncol. 2014;35:696–700. [PubMed] [Google Scholar]
- 12.Zhu X, Zhao H, Lin Z, Zhang G. Functional studies of miR-130a on the inhibitory pathways of apoptosis in patients with chronic myeloid leukemia. Cancer Gene Ther. 2015;22:573–580. doi: 10.1038/cgt.2015.50. [DOI] [PubMed] [Google Scholar]
- 13.Marrelli M, Paduano F, Tatullo M. Human periapical cyst-mesenchymal stem cells differentiate into neuronal cells. J Dent Res. 2015;94:843–852. doi: 10.1177/0022034515570316. [DOI] [PubMed] [Google Scholar]
- 14.Yu E, Amri H. China's Other Medical Systems: Recognizing Uyghur, Tibetan, and Mongolian Traditional Medicines. Glob Adv Health Med. 2016;5:79–86. doi: 10.7453/gahmj.2015.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Safavi-Abbasi S, Brasiliense LB, Workman RK, Talley MC, Feiz-Erfan I, Theodore N, Spetzler RF, Preul MC. The fate of medical knowledge and the neurosciences during the time of Genghis Khan and the Mongolian Empire. Neurosurg Focus. 2007;23:E13. doi: 10.3171/FOC-07/07/E13. [DOI] [PubMed] [Google Scholar]
- 16.Bo A, Si L, Wang Y, Xiu L, Wu R, Li Y, Mu R, Ga L, Miao M, Shuang F, et al. Clinical trial research on Mongolian medical warm acupuncture in treating insomnia. Evid Based Complement Alternat Med. 2016;2016:6190285. doi: 10.1155/2016/6190285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yundeng Exploration of Mongolian translation of The Four medical tantras (rGyud-bzhi) Zhonghua Yi Shi Za Zhi. 1989;1989:185–188. (In Chinese) [PubMed] [Google Scholar]
- 18.Erihenbatu The Mongolian medical schools and its exponents. Zhonghua Yi Shi Za Zhi. 1988;18:108–112. (In Chinese) [PubMed] [Google Scholar]
- 19.Burenbatu BM, Borjigin M, Eerdunduleng, Huo W, Gong C, Zhang G Hasengaowa, Longmei, Li M, Zhang X, et al. Profiling of miRNA expression in immune thrombocytopenia patients before and after Qishunbaolier (QSBLE) treatment. Biomed Pharmacother. 2015;75:196–204. doi: 10.1016/j.biopha.2015.07.022. [DOI] [PubMed] [Google Scholar]
- 20.Riesco-Eizaguirre G, Wert-Lamas L, Perales-Patón J, Sastre-Perona A, Fernández LP, Santisteban P. The miR-146b-3p/PAX8/NIS regulatory circuit modulates the differentiation phenotype and function of thyroid cells during carcinogenesis. Cancer Res. 2015;75:4119–4130. doi: 10.1158/0008-5472.CAN-14-3547. [DOI] [PubMed] [Google Scholar]
- 21.Gottlieb DJ, Hek K, Chen TH, Watson NF, Eiriksdottir G, Byrne EM, Cornelis M, Warby SC, Bandinelli S, Cherkas L, et al. Novel loci associated with usual sleep duration: The CHARGE Consortium Genome-Wide Association Study. Mol Psychiatry. 2015;20:1232–1239. doi: 10.1038/mp.2014.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Srichomkwun P, Admoni O, Refetoff S, de Vries L. A Novel Mutation (S54C) of the PAX8 Gene in a Family with Congenital Hypothyroidism and a High Proportion of Affected Individuals. Horm Res Paediatr. 2016;86:137–142. doi: 10.1159/000445891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Arrigoni E, Saper CB. What optogenetic stimulation is telling us (and failing to tell us) about fast neurotransmitters and neuromodulators in brain circuits for wake-sleep regulation. Curr Opin Neurobiol. 2014;29:165–171. doi: 10.1016/j.conb.2014.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Paulson KL, Shay BL. Sympathetic nervous system responses to acupuncture and non-penetrating sham acupuncture in experimental forearm pain: A single-blind randomised descriptive study. Acupunct Med. 2013;31:178–184. doi: 10.1136/acupmed-2012-010223. [DOI] [PubMed] [Google Scholar]