Abstract
Objective
Examine changes in prevalence of obesity and target health behaviors (fruit, vegetable, and beverage consumption; physical activity; screen time; sleep duration) among students from communities that participated in the Massachusetts Childhood Obesity Research Demonstration Project (MA-CORD) compared to controls.
Methods
MA-CORD was implemented in two low-income communities. School-level prevalence of obesity among students in grades 1, 4 and 7 was calculated for the intervention communities and nine matched control communities pre- and post-intervention. Fourth and 7th grade students’ self-reported health behaviors were measured in intervention communities at baseline and post-intervention.
Results
Among 7th graders (the student group with greatest intervention exposure), we observed a statistically significant decrease in prevalence of obesity from baseline to post-intervention in Community 2 (−2.68 percent, p=0.049) and a similar but non-significant decrease in Community 1 (−2.24 percent, p=0.099). Fourth and 7th grade students in both communities were more likely to meet behavioral targets post-intervention for sugar-sweetened beverages (both communities: p<0.0001) and water (Community 1: p<0.01; Community 2: p=0.04), and in Community 2 for screen time (p<0.01).
Conclusions
This multisector intervention was associated with a modest reduction in obesity prevalence among 7th graders in one community compared to controls, along with improvements in behavioral targets.
Keywords: Childhood obesity, intervention, public health
Introduction
Childhood obesity persists as a pressing public health issue. While evidence suggests recent progress among 2- to 5-year-olds1, overall prevalence of childhood obesity is historically high and may still be increasing for older adolescents.2 Moreover, racial/ethnic and socioeconomic disparities appear to be increasing.3,4,5 In recent years, there has been a movement towards multilevel, multisector approaches for the prevention and control of obesity, with the Institute of Medicine stating that engagement across levels and settings is critical for reducing disparities in obesity risk.6 While the evidence base for such interventions is growing7–11, there is still a need for empirical evidence for multisector approaches in diverse communities in the United States.
The Childhood Obesity Research Demonstration (CORD) project is a multilevel, multisector community intervention that integrated clinical and public health evidence-based approaches to promote healthy lifestyle behaviors and reduce rates of obesity among underserved children 2–12 years of age.12 Massachusetts was one of three demonstration grantees, in addition to California and Texas, under the CORD framework.12 The design and evaluation of the Massachusetts CORD project (MA-CORD) has been previously described. 13,14 In short, MA-CORD was implemented in two low-income communities in Massachusetts (2012–2014) and targeted six community sectors or settings: schools, health centers, afterschool, community, early care and education, and Special Supplemental Nutrition Program for Women, Infants, and Children (WIC). Collectively, the intervention activities were designed to reduce the prevalence of childhood obesity and promote key behavioral targets: replacement of nutrient-poor foods with fruits and vegetables, decreased consumption of sugar-sweetened beverages (SSB), increased physical activity (PA), decreased screen time, and increased sleep duration.
In this study, we examine changes in the prevalence of obesity among elementary and middle school students in the two intervention communities compared with nine matched control communities. We also describe changes in students’ self-reported diet, PA, sleep, and media behaviors from pre intervention to post intervention for the two intervention communities. These findings add important empirical evidence to the body of literature concerning multilevel, multisector community-based interventions and may inform the design of future obesity prevention efforts.
Methods
Intervention Setting
The MA-CORD intervention was implemented in two diverse, low-income Massachusetts communities from 2012-2014; both communities received the intervention. These communities were selected using a competitive application process, and selection criteria included income and capacity for obesity prevention.13 For comparison with these 2 intervention communities, 9 control communities were selected based on criteria described in the Selection of Control Communities section below.
Characteristics of the intervention and control communities and students are summarized in Table 1. The communities were predominantly non-Hispanic white (both 68%) with large Hispanic populations (Community 1: 22%, Community 2: 17%) and had per capita incomes that were substantially lower (Community 1: $22,620, Community 2: $21,056) than the state overall ($35,500 in 2012).15 Approximately two-thirds of the student body in both intervention communities were defined as low-income (Community 1: 66.5%, Community 2: 67.7%). Across both intervention communities, each with a single school district, there were 28 schools eligible to participate in MA-CORD (Community 1: 3 elementary schools, 2 middle schools and 1 combined elementary/middle school; Community 2: 19 elementary schools and 3 middle schools).
Table 1.
Baseline Characteristics of Communities and Schools Participating in the MA-CORD Intervention, Massachusetts, USA
| Community Demographics | Community 1 | Community 2 | Control Communities (N=9)3 |
|---|---|---|---|
| Total Population (n)1 | 40,318 | 95,072 | 84,372 |
| Per capita income ($)2 | 22,620 | 21,056 | 27,742 |
| Persons below poverty level (%)2 | 20.6 | 23.5 | 16.4 |
| School Characteristics6 | Community 1 | Community 2 | Control Communities (N = 9) |
|
| |||
| Race/Ethnicity4 (% of students) | |||
| Black/African American, non-Hispanic | 6.6 | 11.7 | 8.5 |
| Hispanic/Latino | 41.4 | 28.2 | 30.1 |
| White, non-Hispanic | 42.4 | 51.0 | 50.7 |
| % Low-income4,5 | 66.5 | 67.7 | 59.8 |
| Average % obesity, grades 1,4,7 (SD)6 | 25.5 (2.9) | 21.0 (1.7) | 21.6 (2.7) |
State and County QuickFacts, Census 2010: U.S. Census Bureau; [August 12, 2016]. Available from: http://quickfacts.census.gov/qfd/states/25/2545000.html.
State and County QuickFacts, American Community Survey 2010–2014: U.S. Census Bureau; [August 12, 2016]. Available from: http://quickfacts.census.gov/qfd/states/25/2545000.html.
Control community demographics are average values across all 9 communities
School/District Profiles, Enrollment Data: Massachusetts Department of Elementary and Secondary Education; [December 1, 2015]. Available from: http://profiles.doe.mass.edu/.
Low-income defined as being eligible for either free/reduced price lunch, transitional aid to families or the Supplemental Nutrition Assistance Program based on family household income
Student demographic characteristics reported are all averages across the period 2009–2012
Study procedures were approved by the human subjects committees of the Massachusetts Department of Public Health, Harvard T.H. Chan School of Public Health, Massachusetts General Hospital, and Harvard Pilgrim Health Care Institute in June 2012.
Description of the MA-CORD Intervention Components
MA-CORD intervention components have been described in detail elsewhere. 13,16 The intervention components in sectors most likely to affect the school-aged population are summarized briefly below and in Figure 1, and the timing of intervention components and measures is depicted in Figure 2.
Figure 1.
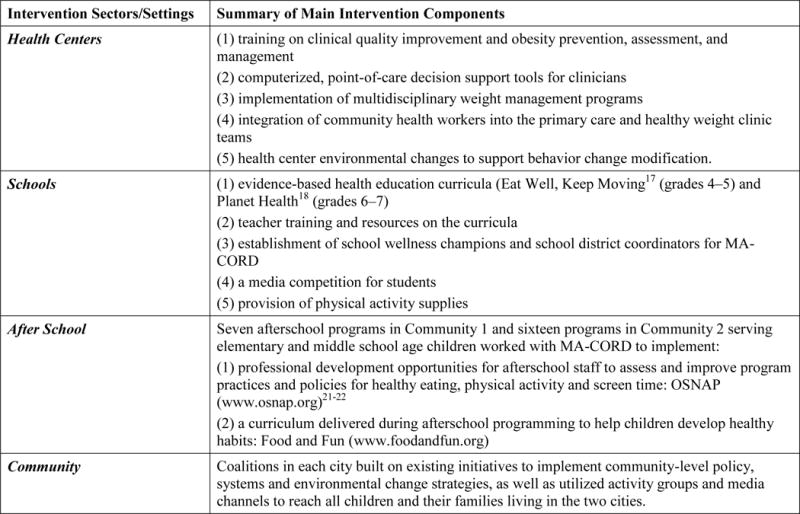
Intervention components in sectors most likely to affect the school-aged population.
Figure 2.
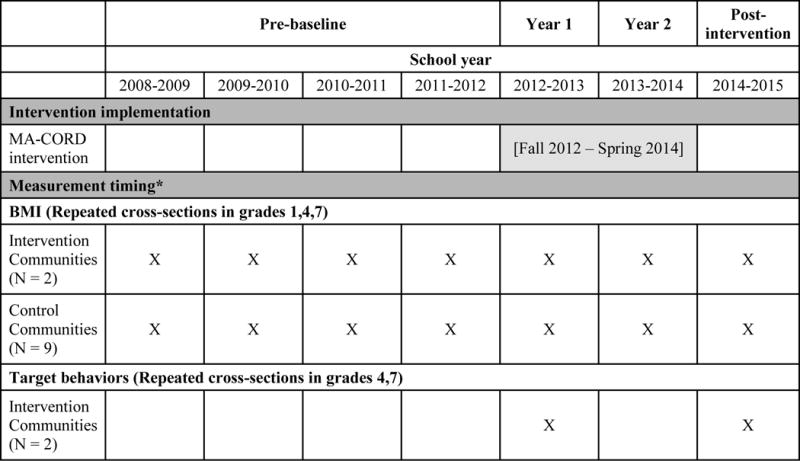
Timing of MA-CORD Implementation and Measurements.
*This study utilized two designs: a quasi-experimental design with pre/post data for the intervention communities and the matched control communities (for obesity prevalence) and a quasi-experimental design with pre/post data for only the intervention communities (for behavioral outcomes).
Intervention components in each city’s public elementary and middle schools included evidence-based health education curricula (Eat Well, Keep Moving17 in grades 4–5 and Planet Health18 in grades 6–7), as well as teacher training and resources on the curricula. The program established a school district coordinator for each community and at least one school wellness champion in each school to receive training and help ensure that MA-CORD activities were carried out. PA supplies were also provided to schools in Community 2, and a student media competition was held to increase awareness of MA-CORD and promote the target behaviors.19
MA-CORD intervention activities in other sectors most likely to affect the school-aged population include those implemented in health centers, afterschool programs, and the broader community. In short, each city’s federally qualified community health centers implemented training, computerized point-of-care decision support tools20, and multidisciplinary weight management programs, in addition to integrating community health workers into clinic teams and making environmental changes to support the intervention. Seven afterschool programs in Community 1 and sixteen programs in Community 2 worked with MA-CORD to implement professional development opportunities for staff related to healthy eating, PA and screen time (OSNAP), and also implemented the Food and Fun curriculum (available at www.OSNAP.org) to help children develop healthy habits.21,22 Finally, coalitions in each city built upon existing initiatives to implement community-level policy, systems and environmental change strategies, and utilized media channels to reach all children and their families living in the two communities.
Evaluation Design
This study utilized two designs: a quasi-experimental design with pre/post data for the intervention communities and the matched control communities (for obesity prevalence) and a quasi-experimental design with pre/post data for only the intervention communities (for behavioral outcomes). As described below, our approach for the obesity prevalence analysis made use of an extended (4 year) pre-baseline period and then three data collection points after the intervention began: early in each of the subsequent three school years.
Data Collection Procedures
Massachusetts public schools are required to measure heights and weights of all children in grades 1, 4, 7, and 10 on an annual basis and document prevalence of overweight and obesity by gender and grade.23 As a result, obesity prevalence data in these grades were available for the 2 intervention and 9 control communities for an extended pre-baseline period (four school years preceding the intervention), the intervention period (i.e. the 2012–2013 and 2013–2014 school years), and post-intervention.
For schools receiving the MA-CORD intervention, this procedure was modified during the 2012–2013 (baseline) and 2014–2015 (post-intervention) school years to also include a written, self-reported student survey that measured demographic characteristics (age, gender, and race/ethnicity) and the five target behaviors. All 4th and 7th graders from the intervention communities were invited to complete this survey at the time of height/weight measurement (N = 2456 students at baseline, N = 2506 at follow-up). There is evidence for moderate validity for these self-reported outcome measures in students as young as 4th grade. 14, 26 First-grade students did not complete the survey over concerns about their ability to report information accurately. The school nurse documented first-grade students’ demographic information using school records.
Thus, in the intervention communities, student height and weight were measured each year for all students in grades 1, 4, and 7, and student self-reported health behaviors were measured at baseline and post-intervention for students in grades 4 and 7. In the control communities, student obesity prevalence data were measured each year for students in grades 1, 4, and 7; student health behaviors were not assessed due to logistical constraints. Due to the data collection schedule and the fact that the curricula were implemented during the two years of intervention with students in grades 4–7 only, at the time of final follow-up students in grade 7 had the longest exposure to the intervention and were the only grade (of those measured) to have received any classroom based lessons.
To operationalize students’ potential exposure to MA-CORD intervention activities across the sectors, we collected information on the number of students eligible to receive the MA-CORD intervention, the percent of eligible teachers who attended trainings (in the school sector), the number of children ages 6–12 years attending each community’s health center in relation to school enrollment, and program enrollment in the afterschool sector in relation to school enrollment, in order to estimate reach of the intervention.
Selection of Control Communities
Among Massachusetts communities that collected height and weight data, sixty-six communities had complete school obesity data for grades 1, 4, and 7 during the four pre-intervention years and two intervention years (i.e. all school years ending in 2009–2014). These communities were considered eligible for selection as matched control communities. Nine control communities were selected using Euclidean distance matching, based on racial/ethnic composition (% black, % white, % Hispanic) and percent low-income in each school district. Average rates of each characteristic across the pre-intervention period (school years ending in 2009–2011) were used. The sum of linear differences across matching variables was calculated for each eligible control community in relation to each of the two intervention communities, and eligible control communities were ranked from smallest to largest distance. All distance calculations were conducted using SAS PROC DISTANCE, with matching variables standardized to a mean of 0 and standard deviation of 1. There was complete overlap in the top 9 matches for each intervention community, so those 9 districts were selected to serve as controls for both intervention districts. The inclusion of additional matching variables (percent female, obesity prevalence, and overweight prevalence), in addition to racial/ethnic composition and low-income percentage, had no appreciable impact on the ranks of control communities. Validating this matching approach, a regression model predicting average rates of obesity among the 66 eligible control communities and 2 intervention communities across the pre-intervention period, school racial/ethnic composition and low-income percentage explained 72% of the variation in obesity rates (R2=0.72).
Primary Outcome Measures
Outcome measures have been described in detail previously24; brief descriptions are as follows:
Prevalence of obesity
Children’s weight and height were measured by school nurses and were used to calculate child body mass index (BMI) (kg/m2) and age and sex-specific BMI percentiles (Li 2015). A standard definition of childhood obesity (≥ 95th BMI percentile for age and sex) was used.25
Dietary behaviors
Children were asked about fruit, vegetable, SSB (i.e., non-diet sodas and fruit-flavored drinks), 100% juice, and water consumption on the previous day, with a 4-point response scale (e.g., 0 = did not eat any vegetables, 1 = ate vegetables 1 time yesterday, 2 = ate vegetables 2 times yesterday, and 3 = ate vegetables 3 or more times yesterday).26,27
PA
Children were asked about the number of days in the past week that they participated in at least 30 minutes of moderate-to-vigorous PA (i.e. “physical activity that made your heart beat fast or made you breathe hard”).26,27
Screen time
Children’s screen time was assessed using two questions on time spent watching television/digital video discs (TV/DVDs) and time spent playing video games and computer games for a typical weekday and weekend day in the past week. This information was used to calculate average daily screen time.17,28
Sleep duration
Children recalled the times they went to bed and woke up the next morning on a usual weekday, which were used to calculate total sleep time.24
Dichotomous outcome targets were defined in accordance with MA-CORD behavioral guidelines and national recommendations as follows: 0 occasions drinking SSBs on the previous day, 1 or 0 occasions of 100% juice, 1 or more occasions of water, 5 or more occasions of fruits and vegetables, less than 2 hours of daily screen time, 10 or more hours of sleep on a usual day, and at least 30 minutes of PA every day.
Statistical Analyses
Our primary analysis examined change in the prevalence of obesity in the intervention communities compared to change in the matched controls. Repeated population cross-sections of obesity prevalence were available for all children in grades 1, 4, and 7 in the two intervention communities and the nine control communities at each of seven time points (4 years pre-baseline and three data collection points after the intervention began).
We used SAS PROC MIXED to examine change in the prevalence of obesity in each intervention community relative to the control communities. We used linear mixed models with a random intercepts model, assuming compound symmetry, and using the repeated function to account for the nesting of repeated annual grade-specific obesity rates within communities. Our model included terms for the year of observation, changes in slope following the intervention in the two intervention communities, indicators for each intervention community, indicators for grade, and measures of race/ethnicity (% non-Hispanic African American, % Hispanic/Latino, and % non-Hispanic White students) and % low-income at the school level. This last variable was defined as the % of enrollment who met any of the following: the student is eligible for free or reduced price lunch; or, the student receives Transitional Aid to Families benefits; or, the student is eligible for Supplemental Nutrition Assistance Program benefits. This variable was not available for 2014–2015, so we carried forward the previous year’s value. Additionally, we stratified models examining change in obesity prevalence by grade level. As previously noted, we expected to see the largest effects among 7th graders because they had the longest exposure to the main component of the school intervention (i.e., the health curricula), and they were the only students of those measured to have received any classroom-based intervention at the time of final follow-up.
To assess change in the behavioral targets, the prevalence of target behaviors at baseline and post-intervention follow up was examined. Eligible subjects for behavioral outcomes analyses had complete data on gender, age, race/ethnicity, school, dietary outcomes, sleep, screen time, and PA. After excluding students with implausible values for sleep (i.e. <3 hours or >18 hours) and implausible values for screen time (i.e. > 3 SD above the mean), our analytic sample consisted of 1918 students at baseline and 1783 students at follow-up. This comparison was limited to the intervention communities since survey data were not available from a control community.
Using individual-level data from repeated cross-sections, we used log binomial regression (with generalized estimating equations to account for clustering by school) to estimate the risk ratio of meeting behavioral targets post-intervention compared to baseline. Models were stratified by community and adjusted for any differences in student gender, grade, and race/ethnicity between pre- and post-intervention periods. To test for potential heterogeneity of associations by grade, grade-stratified models were examined as well. All analyses were conducted using SAS (version 9.3; SAS Institute, Cary, NC, USA).
Results
Based on the number of students eligible to receive the MA-CORD intervention and the percent of eligible teachers who attended trainings, we estimate that 100% of eligible students in Community 1 and approximately 70% of eligible students in Community 2 were reached by the school-sector classroom lessons. In contrast, based on afterschool program enrollment and public school enrollment (grades K-8), we estimate that 11% of students in Community 1 and 7% of students in Community 2 were potentially reached by the intervention in the afterschool setting, and based on community health center attendance and public school enrollment approximately 8% of students in Community 1 and 14% of students in Community 2 were reached by the intervention in the clinical setting.
Change in Obesity Prevalence
Results from the model examining change in prevalence of obesity are presented in Table 2. Overall, we did not observe a significant decrease in the percent of students with obesity from baseline to post-intervention in either community in comparison with controls (Community 1: −0.77% change per year, 95% CI = −2.06, 0.52, p = 0.240; Community 2: −0.17% change per year, 95% CI = −1.45, 1.11, p = 0.795). However, a statistically significant decrease in the percent of students with obesity from baseline to post-intervention was observed for grade 7 in Community 2 (−2.68% change per year, 95% CI = −5.34, −0.01, p = 0.049) and a marginally significant decrease was observed for grade 7 in Community 1 (−2.24% change per year, 95% CI = −4.92, 0.43, p = 0.099) compared to the control communities. Results did not change when models were additionally adjusted for gender, and no significant effect was observed for grades 1 and 4. Additionally, in a secondary analysis examining the effect of the intervention in both communities combined, compared to the control communities, we also observed a statistically significant decrease for grade 7 (−2.46% change per year, 95% CI = −4.43, −0.49, p = 0.015) but not for grades 1 and 4.
Table 2.
Change in percent of students per year with obesity pre- to post-intervention, overall and stratified by grade
| Coefficient Estimate | 95% | CI | P-value | |
|---|---|---|---|---|
| Overall | ||||
|
| ||||
| Intervention effect, Community 1 vs. control communities | −0.77 | −2.06 | 0.52 | 0.240 |
| Intervention effect, Community 2 vs. control communities | −0.17 | −1.45 | 1.11 | 0.795 |
|
| ||||
| Grade 1 and 4 | ||||
|
| ||||
| Intervention effect, Community 1 vs. control communities | −0.08 | −1.34 | 1.17 | 0.895 |
| Intervention effect, Community 2 vs. control communities | 1.07 | −0.18 | 2.31 | 0.092 |
|
| ||||
| Grade 7 | ||||
|
| ||||
| Intervention effect, Community 1 vs. control communities | −2.24 | −4.92 | 0.43 | 0.099 |
| Intervention effect, Community 2 vs. control communities | −2.68 | −5.34 | −0.01 | 0.049 |
Models included terms for the year of observation, for changes in slope following the intervention in the two intervention communities, indicators for each intervention community, indicators for grade, and measures of race/ethnicity (% non-Hispanic African American, % Hispanic/Latino, and % non-Hispanic White students) and % low-income at the school level.
Bold text indicates statistical significance.
Change in the Behavioral Targets
Results from models examining change in behavioral outcomes are presented in Table 3. Statistically significant improvements were observed in both communities with respect to consumption of SSBs (Community 1: RR = 1.29, 95% CI = 1.14, 1.46; Community 2: RR = 1.21, 95% CI = 1.11, 1.32) and water (Community 1: RR = 1.07, 95% CI = 1.03, 1.11; Community 2: RR = 1.04, 95% 1.00, 1.07; although the crude result showed a decline in water consumption for Community 2, after adjusting for pre- to post-differences in gender and grade, water consumption increased). A statistically significant improvement was observed in Community 2 in screen time (RR = 1.24, 95% CI = 1.09, 1.41). There were no significant differences observed in either community for fruits and vegetables, 100% juice, sleep, or PA. There were no meaningful differences by grade in grade-stratified models.
Table 3.
Behavioral Outcomes by MA-CORD Community
| Behavioral Target | Percent (n) | Adjusted Model* | ||||
|---|---|---|---|---|---|---|
| Baseline (n=1918) |
Year 2 (n=1783) |
RR | 95% | CI | p-value | |
| SSB intake (soda and fruit punch), 0 times yesterday | ||||||
|
| ||||||
| Community 1 | 13.88(145) | 17.42 (182) | 1.29 | 1.14 | 1.46 | <0.0001 |
| Community 2 | 15.47 (41l) | 17.28 (459) | 1.21 | 1.11 | 1.32 | <0.0001 |
|
| ||||||
| 100% Juice intake, ≤ 1 time yesterday | ||||||
|
| ||||||
| Community 1 | 34.93 (365) | 35.31 (369) | 1.05 | 0.99 | 1.11 | 0.08 |
| Community 2 | 38.59 (1025) | 34.34 (912) | 0.96 | 0.90 | 1.02 | 0.15 |
|
| ||||||
| Water, ≥ 1 time yesterday | ||||||
|
| ||||||
| Community 1 | 42.87 (448) | 44.11 (461) | 1.07 | 1.03 | 1.11 | <0.01 |
| Community 2 | 43.00 (1142) | 40.93 (1087) | 1.04 | 1.00 | 1.07 | 0.04 |
|
| ||||||
| Fruit and vegetable, ≥ 5 times yesterday | ||||||
|
| ||||||
| Community 1 | 5.74 (60) | 6.99 (73) | 1.23 | 0.99 | 1.54 | 0.06 |
| Community 2 | 3.80 (101) | 3.84 (102) | 1.10 | 0.83 | 1.45 | 0.50 |
|
| ||||||
| Screen time, < 2 hours daily | ||||||
|
| ||||||
| Community 1 | 15.69 (164) | 15.50 (162) | 1.01 | 0.84 | 1.20 | 0.96 |
| Community 2 | 15.06 (400) | 16.91 (449) | 1.24 | 1.09 | 1.41 | <0.01 |
|
| ||||||
| Sleep, ≥ 10 hours on a usual day | ||||||
|
| ||||||
| Community 1 | 20.10 (210) | 20.29 (212) | 0.99 | 0.86 | 1.14 | 0.90 |
| Community 2 | 19.73 (524) | 18.00 (478) | 1.02 | 0.95 | 1.09 | 0.64 |
|
| ||||||
| Physical Activity, ≥ 30+ min every day | ||||||
|
| ||||||
| Community 1 | 7.95 (76) | 8.68 (83) | 1.02 | 0.80 | 1.30 | 0.87 |
| Community 2 | 6.96 (167) | 4.88 (117) | 0.77 | 0.57 | 1.03 | 0.08 |
Adjusted for grade (in non-stratified models), race, gender and clustering based on school; modeling the probability that the outcome = 1 (desired outcome as stated)
Bold text indicates statistical significance.
Discussion
We observed a decline in obesity prevalence among 7th grade students in one of the two intervention communities compared to the control communities. Although the relative change in obesity prevalence in the other intervention community was not significant, the effect size was similar for both intervention communities (Community 1: −2.24% change per year, p = 0.099; Community 2: −2.68% change per year, p = 0.049). This effect was limited to 7th grade students, which is consistent with how the school-sector intervention was implemented.16 We sought to reduce the prevalence of obesity across all of the target ages; however, the most substantial intervention components in the school sector targeted only some grades (grades 4–7), and evaluation data from repeated cross-sections were only available from grades 1, 4 and 7—the grades in which student height and weight is measured in Massachusetts. Thus, among the students with post-intervention data, only those in grade 7 had received the classroom-based lessons while in grade 5 (during year 1 of the intervention) and grade 6 (during year 2 of the intervention). Intervention exposure for the other grades with measurement data (1 and 4) was limited to intervention components in afterschool programs and community health centers that had smaller reach, as well as some of the broader community efforts of MA-CORD. Given the brief duration of intervention, the significant effect in Community 2 and the marginal effect for Community 1 is a notable change. Future work should include a clear measure of exposure across various sectors.
With an approximately 2–3% reduction in obesity prevalence per year, these findings are comparable to results from some other community-based interventions7,8,10 and curricula18 that have demonstrated modest, statistically significant improvements in student relative weight status. In addition, there were observable improvements in both communities with respect to SSB and water consumption as well as improvements in screen time in Community 2, but there were no observable effects with respect to fruits and vegetables, juice, sleep or PA.
Overall there were six suggested lessons from the Eat Well, Keep Moving17 curriculum (in both 4th and 5th grade) and five from Planet Health18 (in both 6th and 7th grade) related to four of the five target behaviors. Because none of these lessons addressed sleep, the lack of effect on sleep duration is perhaps unsurprising. However, there was a focus on screen time reduction, and we observed a significant improvement in screen time in Community 2. There was also a focus on healthier beverages, and we observed significant improvements in both SSB and water consumption. Details regarding lessons learned from community stakeholders,29 and additional details of implementation in the school sector16, have been previously reported. Though results reported herein are specific to students living in two low-income communities in MA, summary results from other CORD demonstration sites and cross-site evaluation results are forthcoming.
This study has several strengths, notably the large and racially/ethnically diverse sample, in addition to the use of matched controls for the primary obesity prevalence analysis. The largest limitation is the possibility that temporal trends could differ among communities for reasons other than the intervention. Though there were overall reductions in childhood obesity in Massachusetts during the study period, the use of control communities addresses the potential concern that secular trends explained intervention changes in obesity prevalence. This comparison was not possible for the behavioral targets because the student behavioral surveys were only collected in the two intervention communities.
Conclusion
Improvements in the prevalence of obesity (among 7th graders in one community compared to controls), and in selected behavioral targets were modest, but should be considered in the context of the substantial challenges of implementing a large scale, multi-sectoral intervention in two financially constrained communities over a fairly short period of time. Future work should continue to consider factors associated with successful implementation of such community-based initiatives, as well as the long-term sustained impacts of such efforts.
Study Importance Questions.
1. What is already known about this subject?
Obesity prevalence is at a historically high level and may still be increasing for older adolescents; racial/ethnic and socioeconomic disparities may be increasing.
In recent years, there has been a movement towards multilevel, multisector approaches for the prevention and control of obesity.
The evidence base for such interventions is growing, but there is still a need for empirical evidence for multisector approaches in diverse communities in the U.S.
2. What does your study add?
This study provides empirical evidence for implementation of multisector approaches in two low-income, diverse communities in Massachusetts.
This multisector intervention was associated with a significant reduction in obesity prevalence among 7th graders in one community compared to controls, along with improvements in behavioral targets.
Acknowledgments
The authors wish to thank the families, institutions, faculty, research staff, students and MA-CORD study group for participating in the MA-CORD study.
Funding: This study was supported by the Centers for Disease Control and Prevention (CDC), National Center for Chronic Disease Prevention and Health Promotion (Award # U18DP003370). This work is solely the responsibility of the authors and does not represent official views of the CDC. R Franckle’s work was supported by a predoctoral training grant (T32 DK 007703) and a postdoctoral fellowship (T32 HL 098048) from the National Institutes of Health (NIH). J. Falbe’s work was additionally supported by a postdoctoral fellowship from the American Heart Association (grant 14POST20140055). R. Blaine’s work was funded under an NIH Doctoral Training Grant in Cancer Epidemiology (T32 CA 0900). E. Taveras is supported by grant K24 DK10589 from the National Institute of Diabetes and Digestive and Kidney Diseases.
Footnotes
Disclosure: The authors declare no conflict of interest.
Clinical trial registration number: NCT02110615
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of Childhood and Adult Obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Lawman HG, et al. Trends in Obesity Prevalence Among Children and Adolescents in the United States, 1988–1994 Through 2013–2014. JAMA. 2016;315(21):2292–2298. doi: 10.1001/jama.2016.6361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Falbe J, Cotterman C, Linchey J, Madsen KA. Ethnic Disparities in Trends in High BMI Among California Adolescents, 2003–2012. Am J Prev Med. 2016;51(2):e45–e55. doi: 10.1016/j.amepre.2016.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Madsen KA, Weedn AE, Crawford PB. Disparities in Peaks, Plateaus, and Declines in Prevalence of High BMI Among Adolescents. Pediatrics. 2010;126(3):434–442. doi: 10.1542/peds.2009-3411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Olds T, Maher C, Zumin S, et al. Evidence that the prevalence of childhood overweight is plateauing: data from nine countries. Int J Pediatr Obes. 2011;6(5–6):342–360. doi: 10.3109/17477166.2011.605895. [DOI] [PubMed] [Google Scholar]
- 6.Accelerating Progress in Obesity Prevention: Solving the Weight of the Nation. 2015 Sep;:1–479. [PubMed] [Google Scholar]
- 7.Sanigorski AM, Bell AC, Kremer PJ, Cuttler R, Swinburn BA. Reducing unhealthy weight gain in children through community capacity-building: results of a quasi-experimental intervention program, Be Active Eat Well. Int J Obes. 2008;32(7):1060–1067. doi: 10.1038/ijo.2008.79. [DOI] [PubMed] [Google Scholar]
- 8.Economos CD, Hyatt RR, Must A, et al. Shape Up Somerville two-year results: A community-based environmental change intervention sustains weight reduction in children. Preventive Medicine. 2013;57(4):322–327. doi: 10.1016/j.ypmed.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 9.de Silva-Sanigorski AM, Bell AC, Kremer P, et al. Reducing obesity in early childhood: results from Romp & Chomp, an Australian community-wide intervention program. Am J Clin Nutr. 2010;91(4):831–840. doi: 10.3945/ajcn.2009.28826. [DOI] [PubMed] [Google Scholar]
- 10.Pettman T, Magarey A, Mastersson N, Wilson A, Dollman J. Improving weight status in childhood: results from the eat well be active community programs. Int J Public Health. 2013;59(1):43–50. doi: 10.1007/s00038-013-0455-4. [DOI] [PubMed] [Google Scholar]
- 11.Kremer P, Waqa G, Vanualailai N, et al. Reducing unhealthy weight gain in Fijian adolescents: results of the Healthy Youth Healthy Communities study. Obesity Reviews. 2011;12:29–40. doi: 10.1111/j.1467-789X.2011.00912.x. [DOI] [PubMed] [Google Scholar]
- 12.Dooyema CA, Belay B, Foltz JL, Williams N, Blanck HM. The Childhood Obesity Research Demonstration Project: A Comprehensive Community Approach To Reduce Childhood Obesity. Childhood Obesity. 2013;9(5):454–459. doi: 10.1089/chi.2013.0060. [DOI] [PubMed] [Google Scholar]
- 13.Taveras EM, Blaine R, Davison K, et al. Design of the Massachusetts Childhood Obesity Research Demonstration (MA-CORD) Study. Childhood Obesity. 2015;11(1):1–12. doi: 10.1089/chi.2014.0031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Davison K, Falbe J, Taveras EM, et al. Evaluation overview for the Massachusetts Childhood Obesity Research Demonstration (CORD) project. Childhood Obesity. 2014 Sep;:1–39. doi: 10.1089/chi.2014.0059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.United States Census Bureau. State & County QuickFacts. http://quickfacts.census.gov/qfd/states/25000.html Accessed September 17, 2014.
- 16.Blaine RE, Franckle RL, Ganter C, et al. Using School Staff Members to Implement a Childhood Obesity Prevention Intervention in Low-Income School Districts: the Massachusetts Childhood Obesity Research Demonstration (MA-CORD Project), 2012–2014. Prev Chron Dis. 2017;14:160381. doi: 10.5888/pcd14.160381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gortmaker SL, Cheung LW, Cheung LWY, et al. Impact of a School-Based Interdisciplinary Intervention on Diet and Physical Activity Among Urban Primary School Children: Eat Well and Keep Moving. Arch Pediatr Adolesc Med. 1999;153:975–983. doi: 10.1001/archpedi.153.9.975. [DOI] [PubMed] [Google Scholar]
- 18.Gortmaker SL, Peterson K, Wiecha J, et al. Reducing Obesity via a School-Based Interdisciplinary Intervention Among Youth: Planet Health. Arch Pediatr Adolesc Med. 1999;153:409–418. doi: 10.1001/archpedi.153.4.409. [DOI] [PubMed] [Google Scholar]
- 19.Criss S, Cheung L, Giles C, et al. Media Competition Implementation for the Massachusetts Childhood Obesity Research Demonstration Study (MA-CORD): Adoption and Reach. IJERPH. 2016;13(4):403–411. doi: 10.3390/ijerph13040403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Taveras EM, Marshall R, Horan CM, et al. Rationale and design of the STAR randomized controlled trial to accelerate adoption of childhood obesity comparative effectiveness research. Contemporary Clinical Trials. 2013;34(1):101–108. doi: 10.1016/j.cct.2012.10.005. [DOI] [PubMed] [Google Scholar]
- 21.Giles CM, Kenney EL, Gortmaker SL, et al. Increasing Water Availability During Afterschool Snack. Am J Prev Med. 2012;43(S2):S136–S142. doi: 10.1016/j.amepre.2012.05.013. [DOI] [PubMed] [Google Scholar]
- 22.Cradock AL, Barrett JL, Giles CM, et al. Promoting Physical Activity With the Out of School Nutrition and Physical Activity (OSNAP) Initiative. JAMA Pediatr. 2016;170(2):155–158. doi: 10.1001/jamapediatrics.2015.3406. [DOI] [PubMed] [Google Scholar]
- 23.Massachusetts Department of Public Health. BMI Screening Guidelines for Schools. 2014:1–27. http://www.mass.gov/eohhs/docs/dph/com-health/school/bmi-screening-guidelines-for-schools.pdf.
- 24.Davison KK, Falbe J, Taveras EM, et al. Evaluation Overview for the Massachusetts Childhood Obesity Research Demonstration (MA-CORD) Project. Childhood Obesity. 2015;11(1):23–36. doi: 10.1089/chi.2014.0059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention. Defining Childhood Obesity. https://www.cdc.gov/obesity/childhood/defining.html Published November 16, 2016. Accessed November 16, 2016.
- 26.Thiagarajah K, Fly AD, Hoelscher DM, et al. Validating the Food Behavior Questions from the Elementary School SPAN Questionnaire. J Nutr Educ and Behav. 2008;40(5):305–310. doi: 10.1016/j.jneb.2007.07.004. [DOI] [PubMed] [Google Scholar]
- 27.Hoelscher DM, Day RS, Kelder SH, Ward JL. Reproducibility and validity of the secondary level School-Based Nutrition Monitoring student questionnaire. J Am Diet Assoc. 2003;103(2):186–194. doi: 10.1053/jada.2003.50031. [DOI] [PubMed] [Google Scholar]
- 28.Schmitz KH, Harnack L, Fulton JE, et al. Reliability and Validity of a Brief Questionnaire to Assess Television Viewing and Computer Use by Middle School Children. J Sch Health. 2004;74(9):370–377. doi: 10.1111/j.1746-1561.2004.tb06632.x. [DOI] [PubMed] [Google Scholar]
- 29.Ganter C, Aftosmes-Tobio A, Chuang E, et al. Lessons Learned by Community Stakeholders in the Massachusetts Childhood Obesity Research Demonstration (MA-CORD) Project, 2013–2014. Prev Chron Dis. 2017;14:160273. doi: 10.5888/pcd14.160273. [DOI] [PMC free article] [PubMed] [Google Scholar]


