Abstract
Objective:
To describe the feasibility of a neuromuscular exercise (NEMEX) program in patients with mild to moderate knee osteoarthritis (KOA).
Background:
Neuromuscular exercise has been increasingly used in patients with osteoarthritis to achieve sensorimotor control and improved daily function.
Treatment:
A study of the first 23 physically active patients (11 men, 12 women; age range = 48–70 years) who had mild to moderate KOA and were undergoing an 8-week, twice-weekly program, consisting of 11 exercises with 3 to 4 levels of difficulty, as part of an ongoing randomized controlled trial. The level of difficulty was noted for each exercise and session. We recorded exertion, pain, adverse events, and adherence. For the 18 patients who participated in 6 or more sessions, a progression of at least 1 level of difficulty (out of 3–4) was observed in half or more of the exercises. However, few patients progressed to jumping activities. Exertion ranged from light to very heavy. Four patients reported a clinically relevant increase in short-term pain after 1 to 2 of the 16 scheduled sessions. No adverse musculoskeletal events were reported. Notably, 3 patients dropped out due to increased (n = 2) or persisting (n = 1) knee pain. However, their pain ratings did not show worsening symptoms.
Uniqueness:
This NEMEX-KOA program was designed for physically active middle-aged patients with mild to moderate KOA; therefore, it involved exercises and difficulty levels that were more challenging than a previously described NEMEX program for patients eligible for total joint replacement.
Conclusions:
In patients with baseline mild to severe pain with activity, the NEMEX-KOA program was feasible. Progression was achieved with few incidents of clinically relevant increases in pain and no adverse events. However, jumping activities were not feasible. These findings hold promise for investigating the efficacy of the NEMEX-KOA program in individuals with mild to moderate KOA.
Key Words: physiotherapy, training, pain management
Key Points
In patients with mild to moderate knee osteoarthritis, the neuromuscular exercise program was feasible for progression, exertion, pain, adverse events, and adherence but not for jumping activities.
Most patients progressed to more complex neuromuscular exercises. Those who attended more sessions generally progressed to higher levels of difficulty.
Temporary increases in exercise-related pain were limited, and no adverse musculoskeletal events occurred.
Researchers should investigate the efficacy of this program on knee-joint loads, pain, and functional performance in patients with mild to moderate knee osteoarthritis.
Exercise effectively reduces knee pain and improves function in patients with knee osteoarthritis (KOA).1 The mechanisms by which exercise reduces pain are poorly understood, and a variety of exercise interventions, ranging from aerobic exercise to isolated resistance training, have been used.2 Unlike conventional strength training, neuromuscular exercise (NEMEX) is aimed at improving sensorimotor control and attaining functional joint stabilization by addressing the quality of movement in all 3 movement planes.3 Researchers1,4,5 have found that NEMEX feasibly and effectively relieves pain, improves function, alters knee biomechanics, and improves the muscle-activation patterns of the surrounding knee musculature in patients with severe KOA and degenerative meniscal tears. Furthermore, NEMEX has been shown to improve articular cartilage quality in middle-aged patients who have had meniscectomies and are at high risk of KOA.6 These results indicate that NEMEX may have important implications for KOA treatment and benefit patients at risk for or with early-stage KOA. However, a detailed NEMEX treatment strategy for patients with mild to moderate KOA has not been described except in the protocol paper of our study.7
The primary aims of the NEMEX program, to improve sensorimotor control and functional joint stabilization (ie, quality of movement), differ from those of traditional osteoarthritis programs, which have a main goal of improving cardiovascular output (ie, walking programs) or enhancing muscle strength (ie, strength training with machines).3,8 The NEMEX-KOA program that we describe was designed for physically active, middle-aged patients with mild to moderate KOA; therefore, it involves exercises and difficulty levels that are more challenging than in the previously described NEMEX program for total joint replacement.4
In this study, we provide novel information on the progression of individual exercises, pain response, and perceived exertion. This information can help clinicians and researchers better understand patient responses, such as length of eventual pain flare and exertion from exercise, and the various mechanisms for progressing NEMEX. Thus, the purpose of this case series was to describe the feasibility of a progressive NEMEX therapy program aimed at improving postural control and functional performance in physically active, middle-aged patients with mild to moderate KOA. Feasibility was defined as progressions in the level of exercise difficulty, perceptions of exertion and pain from exercise, and adherence to exercise. To evaluate feasibility, we investigated the patients' responses to the program for (1) progression over time in each exercise, (2) exertion after individual sessions, (3) changes in pain before and after individual sessions, (4) adverse events, and (5) adherence to training.
CASE DESCRIPTION
The subsequent reporting follows the recommendations of the CAse REport (CARE) guidelines.9 In this case series, we report on the first 23 patients (11 men, 12 women) who were randomized to exercise therapy in an ongoing randomized controlled trial (ClinicalTrials.gov Identifier: NCT01638962). To ensure continued blinding of study personnel, analysis of the primary outcome in the randomized controlled trial was conducted by a statistician who was masked to group allocation and was not directly involved in the study. All participants had mild to moderate KOA and were randomized to a supervised exercise program lasting 8 weeks, with 2 sessions weekly. They were recruited via general practitioners and the communities of Odense and Middelfart, Denmark. The inclusion criteria were, in summary, age from 40 to 70 years; persistent knee pain in accordance with the American College of Rheumatology criteria10; Knee injury and Osteoarthritis Outcomes Score (KOOS; http://www.koos.nu) pain subscale score of less than 8011; radiographic severity grade of 0 to 3 on the Kellgren and Lawrence scoring system12; body mass index (BMI) of less than 32. Exclusion criteria were leg surgery or trauma within the last 6 months or any contraindication to exercise, nonsteroidal anti-inflammatory drugs, or radiographs. The full list of inclusion and exclusion criteria is available from the published study protocol.7 All participants provided written informed consent, and the study was approved by the regional Committee for Medical Research Ethics (project-ID: S-20110153) and the Danish Data Protection Agency (journal-ID: 2011-41-7045).
Initial Visit
At the initial visit, participants were screened for eligibility during a clinical examination (ie, KOA, BMI, and pain level) by the project manager (B.C.). Given the primary outcome of total knee-joint load for the randomized controlled trial, eligible patients were subsequently examined by radiographs to exclude those with greater lateral than medial joint space narrowing or a medial KOA Kellgren and Lawrence grade 4 (ie, large osteophyte, marked narrowing of the joint space, severe sclerosis, and definite deformity of the bone ends).12
Outcome Measures
Participant Characteristics
We recorded age, sex, and BMI at the initial visit. The University of California at Los Angeles (UCLA) Activity Score13 and the KOOS were collected at a baseline examination that took place separately from the initial visit. The UCLA Activity Score assesses self-reported current activity level on a scale ranging from 1 (wholly inactive, dependent on others, and cannot leave residence) to 10 (regularly participates in impact sports).13 The KOOS is a questionnaire that assesses self-reported outcomes for 5 subscales (pain, symptoms, activities of daily living, function in sport and recreation, and knee-related quality of life), with scores for each subscale ranging from 0 (extreme symptoms) to 100 (no symptoms).
The outcome measures were progression in the level of difficulty of the individual NEMEXs for each exercise and session, exertion after each exercise session, pain from exercise sessions and resting pain over the duration of the study, adverse events, and adherence to training. We defined good feasibility as progression in the level of difficulty for most exercises, increased perceived exertion with an increased level of exercise difficulty, no more than moderate pain after the absolute majority of exercise sessions, no serious adverse events, and at least moderate adherence to training (ie, having attended at least 6 of the 16 possible exercise sessions).
Registration of Progression of Individual Exercises
At each exercise session, the supervising physiotherapist recorded in an exercise diary the level of difficulty at which all specific exercises were performed. Exercises were categorized into 4 levels of difficulty (2 exercises included only 3 levels each). The difficulty increased with each level, and examples of how an increase was induced included changing to a softer, more challenging surface during a weight-bearing exercise or increasing load, or both. Whereas each level was associated with increased complexity, the increase in complexity might not be linear (ie, the increase from level 1 to level 2 was not necessarily similar to the increase from level 2 to level 3).
Registration of Exertion and Pain in Relation to the Individual Exercise Sessions
For each exercise session, the supervising physiotherapist instructed the patient to rate his or her exertion on the Borg14,15 category ratio (CR-10) scale (0 = nothing at all to 10 = extremely stong [almost maximal]).
Pain from exercise was defined by the change in pain from before to after each exercise session. The supervising physiotherapist instructed the patient to orally rate his or her pain while looking at a numeric range scale (NRS; 0 = no pain, 10 = pain as bad as it could be). The scale was split into 3 sections. Pain up to 2 was considered safe and colored green; between 2 and 5, acceptable and colored yellow; and greater than 5, avoid and colored red.4,16 Finally, resting pain over the duration of the study was calculated as the change in resting pain from before the first to before the last exercise session.
Registration of Adverse Events and Adherence
Adverse events were recorded using a nonleading questionnaire at separate test sessions at baseline and postintervention. Adverse events were coded according to the Medical Dictionary for Regulatory Activities,17 as currently required by all regulatory authorities, including the US Food and Drug Administration and the European Agency for the Evaluation of Medicinal Products.18 In this report, we restricted adverse events to the musculoskeletal system because they are the most likely to result from exercise. An adverse event was defined as a change in the following symptoms: cramps, joint pain, back pain, swollen joints, or sciatic pain.
Adherence to the NEMEX-KOA for each patient was reported as the number of sessions attended during the intervention period, including the first and last sessions, out of a maximum of 16 sessions. Patients who exercised for less than 6 weeks (out of 8 weeks) were retrospectively asked about reasons for low attendance.
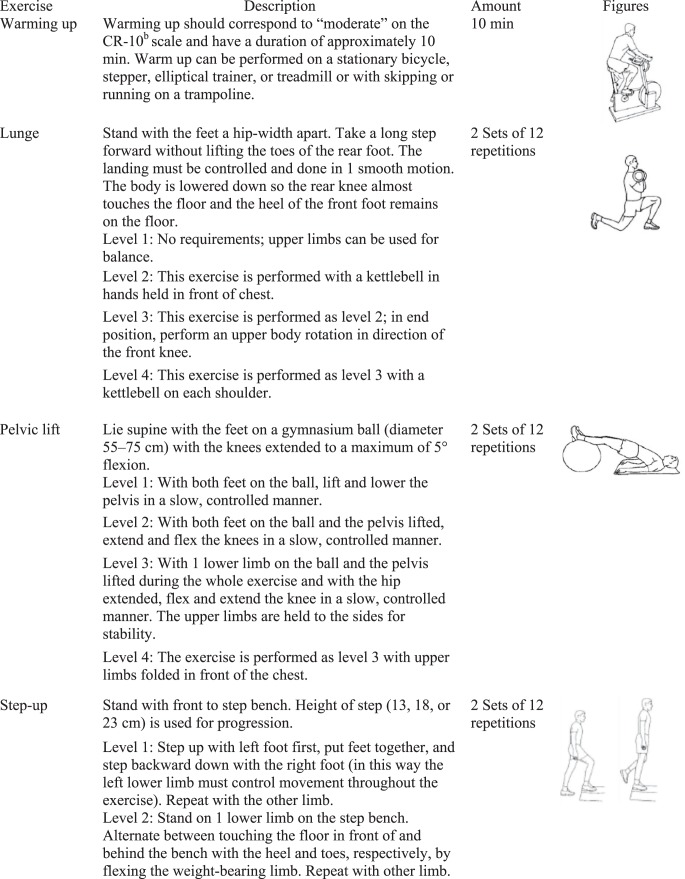
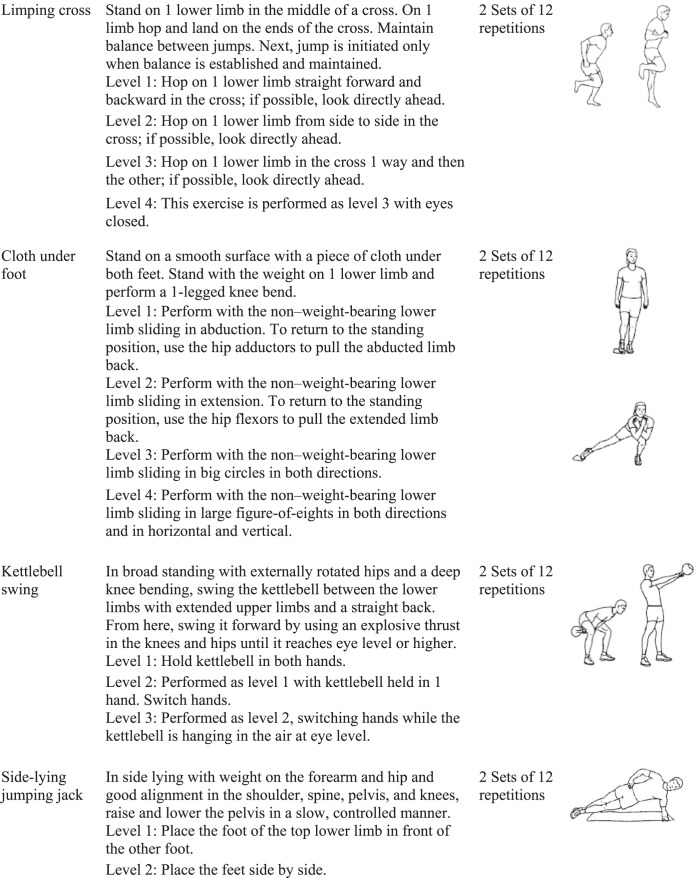
The Neuromuscular Exercise Program
We applied the principles of neuromuscular training described by Clausen et al7 (Appendix). In brief, each exercise session consisted of warming up, NEMEXs, and cooling down.
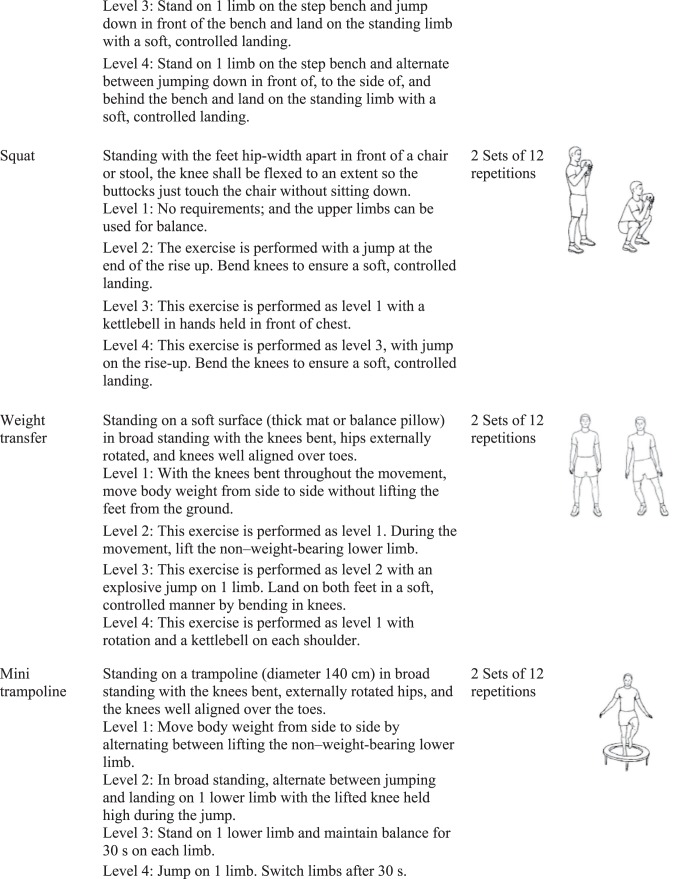
Warming up involved ergometer cycling, treadmill walking, or stepping exercise for 10 minutes at a “rather strenuous” level.15 Neuromuscular exercises comprised 11 exercises with the following key elements: functional performance, postural control, lower extremity muscle strength, balance, and functional stability of the trunk and knee. Definitions are provided in Table 1.3 The exercises were mainly performed in a closed kinetic chain. Higher levels for some exercises included jumping; for the limping-cross and mini-trampoline exercises, all levels required jumping. Levels requiring jumping focused on a controlled takeoff and landing and not on jump height specifically. Each exercise was performed in 2 sets of 12 repetitions, with rest time corresponding to the duration of 1 set. The exercises were performed bilaterally but focused on the affected lower extremity. To allow for progression, 4 levels of difficulty were available for each exercise except for the kettlebell swing and cable/elastic-band exercises, which had 3 levels each. Patients progressed when the supervising physiotherapist deemed that an exercise was performed with good sensorimotor control and good quality (by visual inspection) and patients perceived that they could perform the movement with minimal exertion and with control of the movement. Cooling down included gait retraining (eg, walking in various ways, including backward with an emphasis on alignment) and stretching exercises for the lower extremity muscles (10 minutes).4,5
Table 1. .
Constructs Related to Exercise and Muscle Function
| Constructs |
Definition3 |
| Strength gain | An increase in the amount of external force that a muscle can exert by increasing neural output or muscle mass |
| Postural control | The ability to perform voluntary movements without losing one's posture; includes postural stability and orientation, proprioception, muscle-activation patterns, coordination, and functional performance |
| Functional performance | The ability to perform a complex movement that challenges balance, coordination, postural control, and strength without losing quality of movement (eg, lower limb alignment during weight bearing). Correct functional alignment means that the knee is lined up over the second toe without tending to fall inward (medially) during knee flexion. |
| Closed kinetic chain exercise | Weight-bearing exercise with a distally situated axis of motion and movement occurring in several joints; the distal segment is usually fixed to a supporting surface (eg, squat) |
| Open kinetic chain exercise | Non–weight-bearing exercise with a proximally situated axis of motion and movement occurring at a single joint; the distal segment is free to move (eg, cable/elastic-band exercise) |
As described in the study protocol,7 patients were offered two 60-minute supervised training sessions each week. Based on earlier studies,4,19 the intervention period was set to 8 weeks, with 2 weekly sessions (maximum = 16 sessions). The training involved groups of up to 6 patients at a time and was conducted at 1 of 2 clinics under the supervision of 1 of 2 experienced physiotherapists specializing in the training of musculoskeletal disorders. All 4 supervising physiotherapists (2 per clinic) received education in the exercise program before the study started, were supervised by a colleague, and had regular meetings with the first author (B.C.) to ensure compliance with the study protocol and the exercise program. Each patient was monitored individually to ensure that the exercises were performed at a level consistent with his or her current level of neuromuscular function.
RESULTS
Patients
Participants consisted of 23 patients (11 men, 12 women; age range = 48–70 years; BMI range = 22.6–31.9 kg/m2; Table 2). The KOOS pain scores ranged from 39 to 83, corresponding to mild to moderate or severe knee pain within the week before the study, and KOOS function in sport and recreation scores ranged from 10 to 85, corresponding to mild to extreme difficulty. The UCLA Physical Activity scores ranged from 4 to 10, with 21 of 23 participants regularly engaged in active events (ie, from light activities to sports). The KOOS subscale and UCLA Physical Activity scores are provided in Table 2.
Table 2. .
Descriptive Information and Outcomes for All Patients
| Descriptive Information |
Patient Identification |
||||||||||||||||||||||
| 1 |
2 |
3 |
4 |
5 |
6 |
7 |
8 |
9 |
10 |
11 |
12 |
13 |
14 |
15 |
16 |
17 |
18 |
19 |
20 |
21 |
22 |
23 |
|
| Sex | F | F | F | F | F | M | F | F | M | M | M | M | M | F | F | F | M | M | M | F | F | M | M |
| Age, y | 48 | 69 | 52 | 56 | 70 | 53 | 65 | 54 | 59 | 66 | 65 | 66 | 68 | 69 | 54 | 57 | 52 | 46 | 50 | 60 | 56 | 65 | 67 |
| Body mass index, kg/m2 | 25.1 | 25.7 | 22.9 | 31.6 | 27.3 | 26.7 | 24.4 | 24.9 | 24.1 | 22.6 | 30.4 | 30.1 | 24.4 | 25.0 | 26.1 | 26.7 | 25.7 | 27.8 | 25.3 | 28.9 | 30.9 | 31.9 | 26.3 |
| Index kneea | L | R | L | L | R | L | L | L | R | R | R | L | L | R | R | R | R | L | R | L | L | R | L |
| No. of sessions attendedb | 2 | 2 | 2 | 3 | 5 | 6 | 6 | 7 | 7 | 7 | 8 | 11 | 11 | 12 | 12 | 12 | 12 | 13 | 13 | 13 | 14 | 14 | 16 |
| Attendancedc | 3 | 4 | 3 | 10 | 12 | 49 | 31 | 52 | 24 | 49 | 42 | 56 | 52 | 56 | 45 | 49 | 45 | 53 | 53 | 52 | 56 | 52 | 56 |
| University of California at Los Angeles Physical Activity scored | 10 | 7 | 4 | 8 | 8 | 9 | 7 | 8 | 7 | 7 | 7 | 10 | 8 | 7 | 9 | 7 | 9 | 9 | 9 | 10 | 5 | 8 | 8 |
| Knee Injury and Osteoarthritis Outcome Scoree | |||||||||||||||||||||||
| Pain | 64 | 61 | 47 | 64 | 50 | NA | 58 | 67 | 72 | 78 | 56 | 69 | 67 | 42 | 78 | 39 | 83 | 72 | 61 | 75 | 69 | 61 | 64 |
| Symptoms | 64 | 82 | 54 | 71 | 71 | 93 | 71 | 68 | 75 | 89 | 54 | 82 | 75 | 71 | 86 | 79 | 79 | 68 | 71 | 75 | 54 | 71 | NA |
| Activities of daily living | 74 | 78 | 62 | 72 | 32 | NA | 75 | 69 | 84 | 97 | 59 | 75 | 71 | 47 | 88 | 68 | 94 | 79 | 62 | 93 | 56 | 71 | 76 |
| Function in sport and recreation | 10 | 65 | 15 | 20 | 25 | 80 | 50 | 45 | 20 | 70 | 10 | 75 | 15 | 15 | 55 | 55 | 70 | 35 | 50 | 85 | 15 | 45 | 30 |
| Knee-related quality of life | 44 | 63 | 38 | 44 | 38 | 50 | 50 | 25 | 44 | 75 | 44 | 75 | 31 | 13 | 75 | 63 | 69 | 69 | 44 | 44 | 31 | 44 | 50 |
| Outcomes, numeric range scalef | |||||||||||||||||||||||
| Pain level before first exercise session | 7 | 1 | 3 | 4 | 8 | 1 | 2 | 1 | 2 | 1 | 0 | 3 | 1 | 0 | 6 | 5 | 2 | 2 | 2 | 4 | 2 | 0 | 4 |
| Pain level after exerciseg | 1–3 | 3–5 | 3–4 | 3–4 | 0–6 | 0–1 | 0–3 | 0–5 | 1–4 | 0–5 | 0–4 | 0–3 | 0–2 | 0–6 | 0–4 | 0–5 | 0–4 | 0–4 | 1–4 | 3–6 | 1–2 | 0–1 | 0–1 |
| No. of sessions with pain after exercise >5 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 3 | 0 | 0 | 0 |
Abbreviations: F, female; L, left; M, male; NA, not available; R, right.
Defined as the most painful knee or dominant lower extremity.
Number of exercise sessions attended during the intervention period (maximum = 16 sessions).
Number of days of attendance during the intervention period from the first to the last session (maximum = 56 days [8 weeks]).
The 10-point scale included anchors of 1 (wholly inactive, dependent on others, and cannot leave residence) and 10 (regularly participates in impact sports).
A score of 0 indicated extreme symptoms, and a score of 100 indicated no symptoms.
The 10-point scale included anchors of 0 (no pain) and 10 (pain as bad as it could be).
Range for all exercise sessions.
Progression of Exercises
The 18 patients who participated in 6 or more sessions progressed to the more complex levels of difficulty in half or more of the NEMEXs, and overall, patients who performed more exercise sessions progressed to higher levels of difficulty. The progression for each exercise is described in this subsection.
Neuromuscular Exercises Focused on Strength Gain (Lunge, Squat, Step-Up, and Kettlebell Swing).
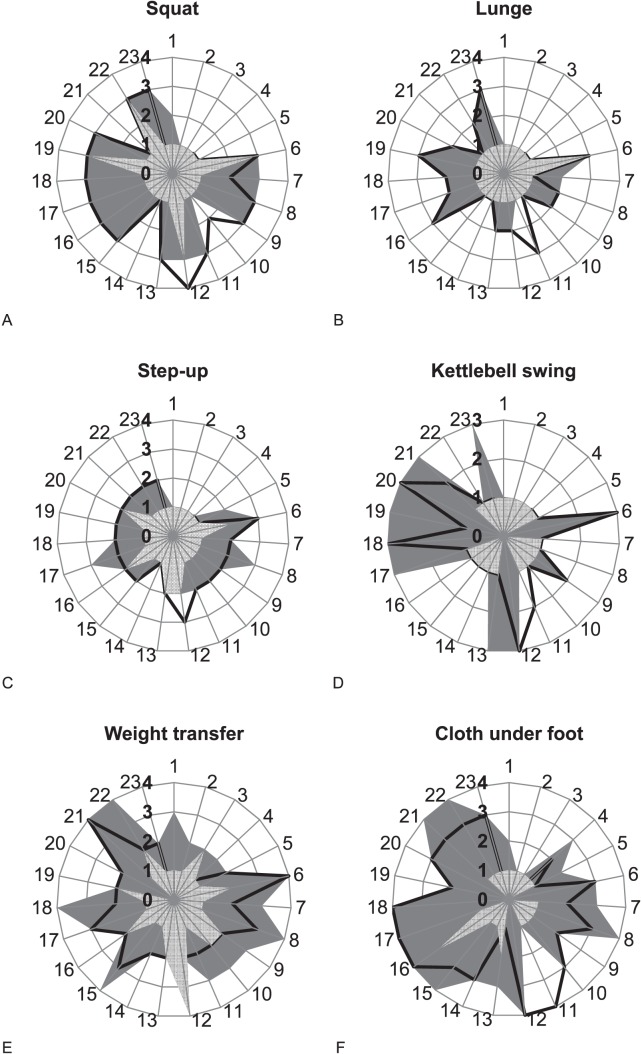
Patients who participated in 6 or more exercise sessions progressed to a moderate level of difficulty; most commonly, the final level was reached after participating in half of the total number of sessions (Figure 1A through D). For the kettlebell-swing exercise, 9 patients progressed to the highest level of difficulty.
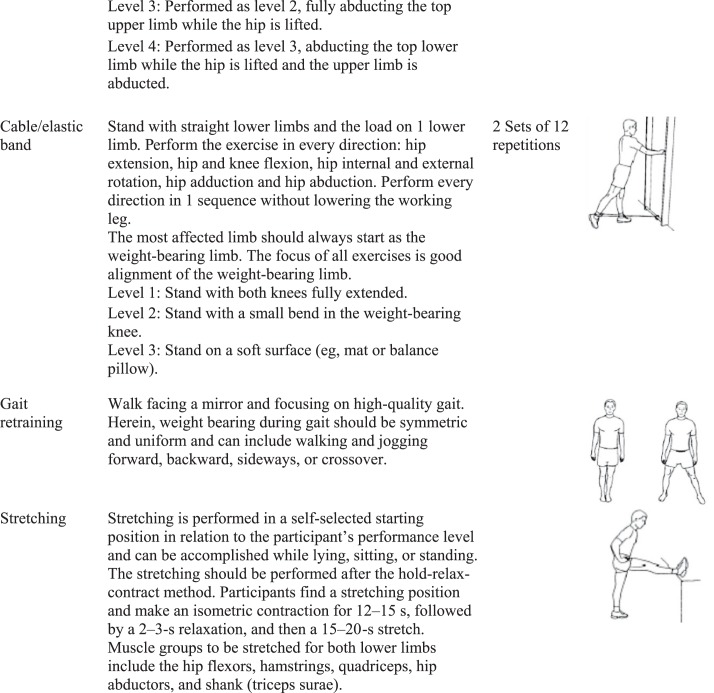
Figure 1. .
Level of difficulty at which each exercise was performed at the first, halfway, and last exercise sessions. Neuromuscular exercises focused on strength gain: (A) squat, (B) lunge, (C) step-up, and (D) kettlebell swing; functional performance: (E) weight transfer, (F) cloth under foot, (G) mini trampoline, (H) cable and elastics band; postural stability: (I) pelvic lift and (J) side-lying jumping jacks; and some levels containing jumps: (G) mini trampoline, (K) limping cross, (A) squat, levels 2 and 4, (C) step-up, levels 3–4, and (E) weight transfer, level 3.
Neuromuscular Exercises Focused on Functional Performance (Weight Transfer, Mini-Trampoline, Cloth Under Foot, and Cable/Elastic-Band Exercise).
All patients who participated in 6 or more sessions and 1 patient who participated in 3 sessions progressed to moderate to high levels of difficulty (ie, levels 2–4). Progression occurred gradually over 8 weeks (Figure 1E through H).
Figure 1. (Continued from previous page.).
The numbers (0–3/4) from the center to the circumference corresponds to the level of difficulty, with 1 being the lowest. The numbers (1–23) around the circumference refer to the 23 individual patients. The light gray area indicates the level of difficulty for the patients at the first session. The black line indicates the level of difficulty for the patients at the halfway (median) session of the attended sessions. The dark gray area indicates the level of difficulty for the patients at the last session. Patients with identifications 1–5 attended 2–5 exercise sessions and those with identifications 6–23 attended 6–16 sessions.
Neuromuscular Exercises Focused on Postural Stability (Side-Lying Jumping Jacks and Pelvic Lift).
Only 6 of 23 patients progressed beyond the second level of difficulty for these exercises (Figure 1I and J).
Neuromuscular Exercises With Some Levels Including Jumps (All Levels of Limping Cross and Mini-Trampoline, Squat Levels 2 and 4, Step-Up Levels 3 and 4, and Weight Transfer Level 3).
Fewer than half of the patients (n = 11) progressed and achieved exercise levels involving jumps on a firm surface (eg, wooden floor; Figure 1A, C, and K), although they were able to perform jumps on a soft surface (eg, trampoline or soft exercise mat; Figure 1E and G).
Exertion
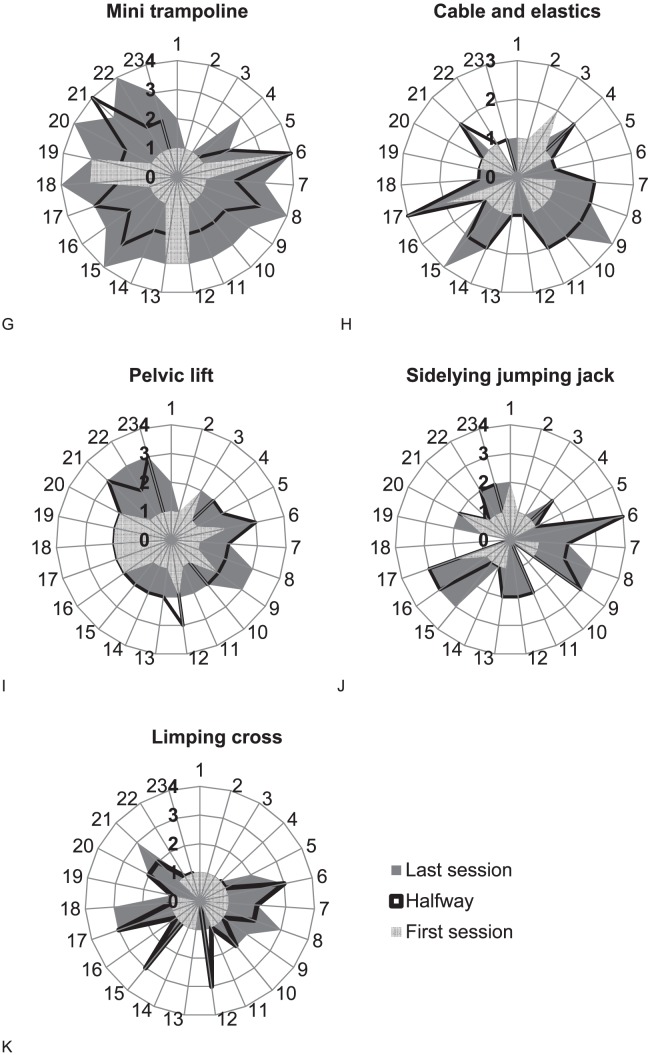
Perceived exertion of the exercise program for each patient ranged from weak (light) to very strong (2 to 8 on CR-10; Figure 2). Our expectation that patients would report increased exertion after the level of difficulty increased was only partially met; 11 patients reported that the last exercise session was more strenuous than the first session. Nine of the 18 participants who attended 6 or more sessions reported that the last session was more strenuous than the first.
Figure 2. .
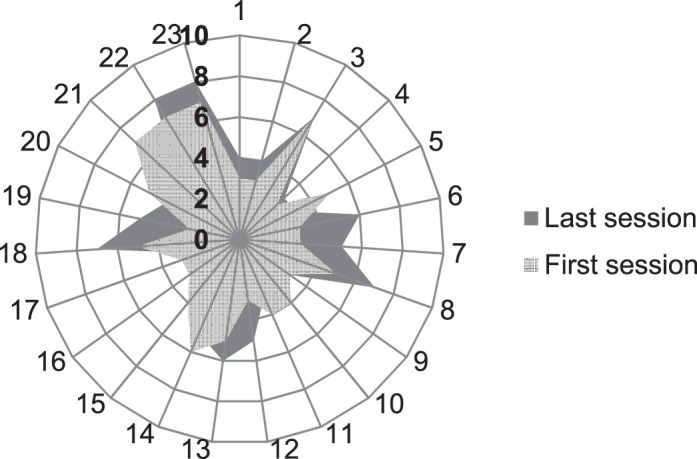
Perceived exertion after the first and last exercise sessions. The numbers (0–10) from the center to the circumference indicate exertion levels, with 0 representing nothing at all and 10 representing extremely strong (almost max). The numbers (1–23) around the circumference refer to the 23 individual patients. The light gray area indicates the perceived exertion level for the patients at the first session. The dark gray area indicates the exertion level for the patients at the last session. Patients with identifications 1–5 attended 2–5 exercise sessions and those with identifications 6–23 attended 6–16 sessions.
Pain
Pain From Exercise.
Overall, we found few reports of a clinically relevant increase in pain from exercise and few reports of severe pain after exercise. Four patients reported a short-term clinically relevant increase in pain from exercise (defined as >2 NRS) after participating in 1 to 2 of 16 scheduled sessions.16 The increased pain was temporary, and the patients continued the exercise program. After exercise, 3 patients reported a pain level greater than 5 NRS after 1, 2, and 3 sessions, respectively (Table 2).
Resting Pain.
The resting pain before the first exercise session ranged from 0 to 8, with 4 patients reporting a pain level equal to or greater than 5 NRS; 3 of these patients reported decreased pain from exercise, and 1 reported no change in pain from exercise (Table 2). Resting pain levels before the last exercise session similarly ranged from 0 to 8, with 2 patients reporting a pain level equal to or greater than 5 NRS; both patients reported decreased pain from exercise (data not shown).
Adverse Events
No patient reported any treatment-specific adverse musculoskeletal events on the questionnaire.
Adherence
For the 8-week exercise program, attendance ranged from 2 to 16 sessions. The 23 patients attended a total of 208 exercise sessions out of 368 possible sessions over 3 to 56 days (Table 2). Seven patients attended for less than 6 weeks and gave the following reasons: increased knee pain (n = 2; patients 3 and 5); knee pain that was due to the original pain and disability and not necessarily aggravated by the exercise (n = 1; patient 4); and other reasons, such as work, transportation, and a cardiovascular procedure (n = 4; patients 1, 2, 7, and 9). Two of 3 patients who reported a high level of pain (>5 NRS) before the first session attended only 2 and 5 sessions, respectively, whereas 13 of 14 patients who reported a low level of pain (≤2 NRS) before the first session attended at least 6 sessions (Table 2).
DISCUSSION
In this case series, we provide a detailed description of a progressive NEMEX program specifically designed for physically active patients with mild to moderate KOA. The program is feasible because the majority of patients progressed to more complex levels of difficulty for most of the NEMEXs with few reports of short-term increased pain from exercise or temporary high levels of postexercise pain, no adverse musculoskeletal events, and moderate adherence to the exercise program. Notably, 3 patients with high levels of pain at baseline did not complete the 8-week program.
Neuromuscular Exercise and Other Types of Exercise
Exercise types that have been evaluated for efficacy as treatments for KOA include resistance, aerobic, and performance (proprioceptive, sensorimotor, balance, neuromuscular) exercises. These types of exercise differ in aims and content.2 Whereas aerobic exercise is used to increase cardiac output and resistance training is used to increase the load a muscle can generate, performance exercise focuses on the knee joint and is used to improve postural control, dynamic joint stability, and functional performance of the lower extremity. In their meta-analysis, Juhl et al2 observed similar effect sizes for pain with resistance, aerobic, and performance exercises in patients with KOA. In addition to reducing pain and symptoms, effective treatment approaches for KOA that can slow disease progression are needed.20 Although we did not investigate this in our study, NEMEXs, which target the efficiency of lower limb movement and muscle-activation patterns, might effectively slow disease progression. In their randomized study, Roos and Dahlberg6 found that 4 months of NEMEX were associated with increased proteoglycan content of the cartilage matrix immediately after an exercise intervention. Increased proteoglycan content translates into greater cartilage stiffness and a greater ability to withstand load. In a long-term follow-up of the same sample, Owman et al21 found that a shorter relaxation time for delayed gadolinium-enhanced magnetic resonance imaging of cartilage at baseline was associated with a higher grade of joint-space narrowing 11 years later, suggesting that lower proteoglycan content is an early marker of future osteoarthritis.
Method of Monitoring Progression
We presented each patient's progression in NEMEX exercises as the level of difficulty at which he or she exercised at the first, halfway or median point, and last exercise session.
Progression from the first to the last exercise session illustrates advancement through the complete intervention (up to 8 weeks). The halfway session shows the rate at which patients progressed and indicates whether an exercise had enough levels of difficulty or was associated with floor or ceiling effects. The reliability of the threshold for exercise progression is unknown. To improve the between-therapists agreement on threshold for progression, the 2 supervising physiotherapists from each clinic participated in familiarization sessions and discussions led by the project manager (B.C.).
Progression in Exercises
As expected, patients progressed differently through the individual exercises of the NEMEX-KOA program. Patients who attended 6 or more exercise sessions progressed to more complex levels of difficulty in most exercises (as seen in Figure 1: patients 1–5 performed exercises at lower levels of difficulty [ie, unfilled circles] compared with patients 6–23 [ie, increased fill of the circles]). Whereas methodologic differences exist, the literature2,22 supports our findings, suggesting that greater exercise attendance is positively related to physical function.
For NEMEXs focusing on strength gain, patients progressed quickly to the levels of sufficient technique; however, they were less able to progress to the more advanced levels that challenge functional performance. Similar to resistance training,23 a familiarization period with low loads seems to be needed for NEMEX-KOA until sufficient technique is learned. In the kettlebell-swing exercise, 9 patients progressed to the highest level of difficulty, indicating a ceiling effect for them. However, we observed a lack of progression to higher levels for most patients, which could be explained by upper extremity stress introduced in the kettlebell swing and lunge. In addition, the higher levels of difficulty for the squat, step-up, and limping cross included jumping, which clearly was a hindrance to progression. In an in vitro study, Nia et al24 showed that cartilage in early-stage osteoarthritis is most sensitive to high loading rates (comparable with jumping activities). Consequently, exercises involving jumping should be performed only with great caution and under supervision.
For NEMEXs focused on functional performance, patients progressed throughout the duration of the exercise program, and most patients reached the most difficult levels. To reduce the risk of ceiling effects with long-term use, we recommend additional levels of high difficulty for progression in exercises with a focus on functional performance. An example is increasing the difficulty of the cloth-under-foot exercise (Figure 1H) by placing the weight-bearing foot on a balance pillow. For the exercises in which only a few patients progressed to the highest level of difficulty, we suggest adding intermediate levels that may promote progress. Examples include adding a level to the side-lying jumping-jack exercise (Figure 1J) to require that the position be maintained for 30 seconds in 3 sets and changing the surface used for the limping-cross exercise (Figure 1K) to a soft exercise mat with fingertip support on a railing or wall during jumping.
Exertion
We observed large variations in perceived exertion levels, and only half of the patients reported increased exertion with increased exercise difficulty. These findings are comparable with those reported for aerobic25 and resistance training26,27 in patients with KOA. We demonstrated no relationship between change in perceived exertion and exercise progression, pain from exercise, resting pain, and number of attended sessions, indicating that progression in the program and attendance did not depend on perceived exertion.
Pain
Three patients reported pain levels greater than 5 NRS after 1 or more exercise sessions, which is comparable with the results from 2 studies of NEMEX.4,28 Ageberg et al4 reported that 32% of patients with KOA noted a pain level greater than 5 NRS after 1 or more exercise sessions before total joint replacement. Stensrud et al28 observed that 5% of patients with degenerative meniscal tears reported pain greater than 5 NRS after 1 or more exercise sessions. In terms of increased pain after an individual session, NEMEX-KOA was as safe as NEMEX for total joint replacement. For comparison, in studies of aerobic and resistance training, increased knee pain was reported by 8% to 18% of patients with KOA who performed aerobic25 or resistance26,29 training, respectively. In these studies, increased knee pain was measured with various methods, ranging from logbooks to documentation by instructors and reports of dropouts. Whereas a direct comparison with our study is difficult due to methodologic differences, NEMEX-KOA seems to be as safe as any other exercise intervention for patients with mild to moderate KOA.
Adverse Events
No treatment-specific adverse musculoskeletal events other than occasional pain flares were reported on the nonleading adverse-event questionnaire or in the exercise diary. Immediate adverse musculoskeletal events were recorded through a self-reported, nonleading questionnaire. In accordance with previous studies, serious adverse events were rare in patients with KOA when exercising. Serious adverse events have been reported in 2% to 4% of patients and were limited to fractures due to falling or dropping equipment.30,31
Adherence
Overall, we observed moderate attendance at the exercise program with large individual variations (2 to 16 sessions). We considered attendance of ≥6 sessions as acceptable, as long as low attendance was not due to treatment-related adverse events or increased pain. Three patients stated that they stopped exercise due to increased or persistent knee pain when performing the NEMEX-KOA. However, these oral statements were reflected only in the pain (>5 NRS after 2 exercise sessions) that 1 of these 3 patients (patient 5) reported. None of them described adverse events, including joint pain, on the self-reported adverse-events questionnaire. Similar dropout rates due to increased knee pain have been noted in other studies5,26 testing NEMEXs for patients with severe KOA. Furthermore, comparable dropout rates (2%–12%) have been observed with resistance training in patients with moderate KOA.26,29 Readers should consider that reported variations in dropout rates from countries around the world may be associated with cultural differences related to pain tolerance for both patients and physiotherapists and with other factors, such as differences in health care systems and recruitment strategies.
Limitations
Our study had limitations. Given the design, it was neither our aim nor possible to evaluate or compare the effects of the NEMEX therapy program with a control group. Instead, we described the NEMEX-KOA in detail and demonstrated its feasibility for progression, exertion, pain, adverse events, and adherence in patients with mild to moderate KOA.
CONCLUSIONS
We described a NEMEX program for mild to moderate KOA and demonstrated that it is feasible for progression, exertion, pain, adverse events, and adherence. Most patients progressed to more complex NEMEXs. Jumping activities, however, were generally not feasible. Patients who attended more exercise sessions were typically able to progress to higher levels of difficulty. We observed limited incidences of temporary increases in exercise-related pain and no reports of adverse musculoskeletal events. This case series holds promise for investigating the efficacy of the NEMEX-KOA program on knee-joint loads, pain, and functional performance in individuals with mild to moderate KOA.
ACKNOWLEDGMENTS
This trial was funded by the Region of Southern Denmark Research Fund; The Danish Rheumatism Association Fund, Gentofte; the Association of Danish Physiotherapists Fund, Copenhagen; the Ryholt Grant, Gentofte; the Family Hede Nielsen Fund, Horsens; and the Odense University Hospital Free Research Funds. These organizations provided funding only and had no other role in the study. Dr Clausen was funded, in part, by a PhD scholarship from the University of Southern Denmark, Odense. We thank ExorLive AS for providing the illustrations for the exercise program in the Appendix.
Appendix. NEMEX-KOA Training Programa
Copyright © by ExorLive AS (www.exorlive.com). Used with permission.
a Participants performed 2 sessions per week. Progression was made when the supervising physiotherapist deemed that an exercise was performed with good sensorimotor control and good performance quality (by visual inspection) and the participant perceived that he or she could perform the movement with minimal exertion and control of the movement.
b The CD-10 scale ranging from 0 (nothing at all) to 10 (extremely strong [almost max]).
REFERENCES
- 1. Thorstensson CA, Henriksson M, von Porat A, Sjödahl C, Roos EM. . The effect of eight weeks of exercise on knee adduction moment in early knee osteoarthritis: a pilot study. Osteoarthritis Cartilage. 2007; 15 10: 1163– 1170. [DOI] [PubMed] [Google Scholar]
- 2. Juhl C, Christensen R, Roos EM, Zhang W, Lund H. . Impact of exercise type and dose on pain and disability in knee osteoarthritis: a systematic review and meta-regression analysis of randomized controlled trials: impact of exercise type and dose in knee osteoarthritis. Arthritis Rheumatol. 2014; 66 3: 622– 636. [DOI] [PubMed] [Google Scholar]
- 3. Ageberg E, Roos EM. . Neuromuscular exercise as treatment of degenerative knee disease. Exerc Sport Sci Rev. 2015; 43 1: 14– 22. [DOI] [PubMed] [Google Scholar]
- 4. Ageberg E, Link A, Roos EM. . Feasibility of neuromuscular training in patients with severe hip or knee OA: the individualized goal-based NEMEX-TJR training program. BMC Musculoskelet Disord. 2010; 11: 126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Villadsen A, Overgaard S, Holsgaard-Larsen A, Christensen R, Roos EM. . Postoperative effects of neuromuscular exercise prior to hip or knee arthroplasty: a randomised controlled trial. Ann Rheum Dis. 2014; 73 6: 1130– 1137. [DOI] [PubMed] [Google Scholar]
- 6. Roos EM, Dahlberg L. . Positive effects of moderate exercise on glycosaminoglycan content in knee cartilage: a four-month, randomized, controlled trial in patients at risk of osteoarthritis. Arthritis Rheum. 2005; 52 11: 3507– 3514. [DOI] [PubMed] [Google Scholar]
- 7. Clausen B, Holsgaard-Larsen A, Søndergaard J, Christensen R, Andriacchi TP, Roos EM. . The effect on knee-joint load of instruction in analgesic use compared with neuromuscular exercise in patients with knee osteoarthritis: study protocol for a randomized, single-blind, controlled trial (the EXERPHARMA trial). Trials. 2014; 15: 444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bennell KL, Hinman RS. . A review of the clinical evidence for exercise in osteoarthritis of the hip and knee. J Sci Med Sport. 2011; 14 1: 4– 9. [DOI] [PubMed] [Google Scholar]
- 9. Gagnier JJ, Kienle G, Altman DG, et al. . The CARE guidelines: consensus-based clinical case reporting guideline development. BMJ Case Rep. 2013; 2013:bcr2013201554. [DOI] [PMC free article] [PubMed]
- 10. Altman R, Asch E, Bloch D, et al. . Development of criteria for the classification and reporting of osteoarthritis: classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthritis Rheum. 1986; 29 8: 1039– 1049. [DOI] [PubMed] [Google Scholar]
- 11. Roos EM, Toksvig-Larsen S. . Knee injury and Osteoarthritis Outcome Score (KOOS): validation and comparison to the WOMAC in total knee replacement. Health Qual Life Outcomes. 2003; 1: 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Altman RD, Gold GE. . Atlas of individual radiographic features in osteoarthritis, revised. Osteoarthritis Cartilage. 2007; 15 suppl A: A1– A56. [DOI] [PubMed] [Google Scholar]
- 13. Terwee CB, Bouwmeester W, van Elsland SL, de Vet HCW, Dekker J. . Instruments to assess physical activity in patients with osteoarthritis of the hip or knee: a systematic review of measurement properties. Osteoarthritis Cartilage. 2011; 19 6: 620– 633. [DOI] [PubMed] [Google Scholar]
- 14. Borg G. . Psychophysical scaling with applications in physical work and the perception of exertion. Scand J Work Environ Health. 1990; 16 suppl 1: 55– 58. [DOI] [PubMed] [Google Scholar]
- 15. Borg G, Ljunggren G, Ceci R. . The increase of perceived exertion, aches and pain in the legs, heart rate and blood lactate during exercise on a bicycle ergometer. Eur J Appl Physiol Occup Physiol. 1985; 54 4: 343– 349. [DOI] [PubMed] [Google Scholar]
- 16. Thomeé R. . A comprehensive treatment approach for patellofemoral pain syndrome in young women. Phys Ther. 1997; 77 12: 1690– 1703. [DOI] [PubMed] [Google Scholar]
- 17. Medical Dictionary for Regulatory Activities. MedDRA MSSO Web site. http://www.meddra.org/. Accessed December 2011.
- 18. Riecke BF, Christensen R, Christensen P, et al. . Comparing two low-energy diets for the treatment of knee osteoarthritis symptoms in obese patients: a pragmatic randomized clinical trial. Osteoarthritis Cartilage. 2010; 18 6: 746– 754. [DOI] [PubMed] [Google Scholar]
- 19. Fransen M, McConnell S, Harmer AR, Van der Esch M, Simic M, Bennell KL. . Exercise for osteoarthritis of the knee. Cochrane Database Syst Rev. 2015; 1:CD004376. [DOI] [PMC free article] [PubMed]
- 20. Hunter DJ. . Lower extremity osteoarthritis management needs a paradigm shift. Br J Sports Med. 2011; 45 4: 283– 288. [DOI] [PubMed] [Google Scholar]
- 21. Owman H, Ericsson YB, Englund M, et al. . Association between delayed gadolinium-enhanced MRI of cartilage (dGEMRIC) and joint space narrowing and osteophytes: a cohort study in patients with partial meniscectomy with 11 years of follow-up. Osteoarthritis Cartilage. 2014; 22 10: 1537– 1541. [DOI] [PubMed] [Google Scholar]
- 22. van Gool CH, Penninx BW, Kempen GI, et al. . Effects of exercise adherence on physical function among overweight older adults with knee osteoarthritis. Arthritis Rheum. 2005; 53 1: 24– 32. [DOI] [PubMed] [Google Scholar]
- 23. Peterson MD, Gordon PM. . Resistance exercise for the aging adult: clinical implications and prescription guidelines. Am J Med. 2011; 124 3: 194– 198. [DOI] [PubMed] [Google Scholar]
- 24. Nia HT, Bozchalooi IS, Li Y, et al. . High-bandwidth AFM-based rheology reveals that cartilage is most sensitive to high loading rates at early stages of impairment. Biophys J. 2013; 104 7: 1529– 1537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wang TJ, Lee SC, Liang SY, Tung HH, Wu SFV, Lin YP. . Comparing the efficacy of aquatic exercises and land-based exercises for patients with knee osteoarthritis: efficacy of aquatic vs. land exercises for knee OA. J Clin Nurs. 2011; 20 17–18: 2609– 2622. [DOI] [PubMed] [Google Scholar]
- 26. Bennell KL, Kyriakides M, Metcalf B, et al. . Neuromuscular versus quadriceps strengthening exercise in patients with medial knee osteoarthritis and varus malalignment: a randomized controlled trial: neuromuscular exercise and knee adduction moment. Arthritis Rheumatol. 2014; 66 4: 950– 959. [DOI] [PubMed] [Google Scholar]
- 27. McKnight PE, Kasle S, Going S, et al. . A comparison of strength training, self-management, and the combination for early osteoarthritis of the knee. Arthritis Care Res (Hoboken). 2010; 62 1: 45– 53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Stensrud S, Risberg MA, Roos EM. . Effect of exercise therapy compared with arthroscopic surgery on knee muscle strength and functional performance in middle-aged patients with degenerative meniscus tears: a 3-mo follow-up of a randomized controlled trial. Am J Phys Med Rehabil. 2015; 94 6: 460– 473. [DOI] [PubMed] [Google Scholar]
- 29. Huang MH, Lin YS, Yang RC, Lee CL. . A comparison of various therapeutic exercises on the functional status of patients with knee osteoarthritis. Semin Arthritis Rheum. 2003; 32 6: 398– 406. [DOI] [PubMed] [Google Scholar]
- 30. Kovar PA, Allegrante JP, MacKenzie CR, Peterson MG, Gutin B, Charlson ME. . Supervised fitness walking in patients with osteoarthritis of the knee: a randomized, controlled trial. Ann Intern Med. 1992; 116 7: 529– 534. [DOI] [PubMed] [Google Scholar]
- 31. Ettinger WH Jr Burns R, Messier SP, et al. . A randomized trial comparing aerobic exercise and resistance exercise with a health education program in older adults with knee osteoarthritis: The Fitness Arthritis and Seniors Trial (FAST). JAMA. 1997; 277 1: 25– 31. [PubMed] [Google Scholar]