Abstract
Reference:
Claes S, Hermie L, Verdonk R, Bellemans J, Verdonk P. Is osteoarthritis an inevitable consequence of anterior cruciate ligament reconstruction? A meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2013;21(9):1967–1976.
Clinical Question:
What is the prevalence of radiographic knee osteoarthritis (OA) at a mean follow-up equal to or greater than 10 years after autologous anterior cruciate ligament (ACL) reconstruction, with or without meniscectomy?
Data Sources:
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting guidelines were used to conduct this meta-analysis. Studies were identified by searching PubMed, MEDLINE, EMBASE, and Cochrane Library dating from their earliest file until October 2010. Key terms applied for searching were anterior cruciate ligament or ACL, autologous, follow-up, long-term, outcome, reconstruction, results, treatment, and (osteo)arthritis or osteoarthrosis. The reference lists of included studies were also manually checked to ensure that relevant articles were not omitted.
Study Selection:
The authors limited their search to English- and French-language journals. Included studies provided radiographic outcomes after autologous ACL reconstruction and had a mean follow-up of ≥10 years. Excluded studies evaluated ACL reconstruction with major concomitant surgical procedures (eg, meniscal allograft transplantation, high tibial osteotomy). In addition, data from 2 studies completed by the same research team with identical patient populations were limited to the article with the longest follow-up. Finally, manuscripts with inaccurate or incomplete data were excluded.
Data Extraction:
The following key characteristics of each study were extracted: type of study (prospective or retrospective); ACL surgical procedure (eg, open or arthroscopic bone-patellar tendon-bone graft); time frame of surgery; mean follow-up (in years) post–ACL reconstruction; total number of participants with radiographs; total number of participants with radiographic OA at follow-up; and number of participants with meniscectomy before, during, or after ACL reconstruction. Although the OA diagnosis was based on radiographic criteria, the included studies used 4 OA classifications and grading scales: Ahlbäck, Fairbanks, Kellgren and Lawrence, and International Knee Documentation Committee. Regardless of classification or grading scale, OA was defined as the presence of joint-space narrowing: Ahlbäck grades 1 through 5, modified Fairbanks grades 2 and 3, Kellgren and Lawrence ≥2, and International Knee Documentation Committee grades C and D. Tibiofemoral and patellofemoral OA data were collapsed due to the lack of reporting specificity among the studies. Participants were categorized into a meniscectomy or nonmeniscectomy group if this information was reported. Partial or total meniscectomies before, during, or after ACL reconstruction were collapsed regardless of location (medial or lateral compartment), and those patients who underwent a meniscal repair were grouped into the nonmeniscectomy group. Data were analyzed using odds ratios, the Cochran χ2 test, and a random-effects meta-regression analysis. The DerSimonian and Laird approach was used to assess study heterogeneity. P values below .05 were considered statistically significant.
Main Results:
The initial computerized database search resulted in 211 possible studies. However, after the authors applied the inclusionary and exclusionary criteria, only 16 studies were relevant. A total of 1554 participants were available at the follow-up period. Mean follow-up ranged from 10 to 24.5 years; 11 of the 16 articles had a mean follow-up between 10 and 12 years. Heterogeneity was large (I2 = 96%), which indicated that the included studies generated a wide range of knee OA prevalence (2%–79%). Almost 28% (95% confidence interval [CI] = 16.3%, 43.5%) of participants had radiographic knee OA. A total of 1264 participants were involved in studies that evaluated meniscectomies (n = 11). Among the 614 participants with either partial or total meniscectomies, 50.4% had radiographic knee OA (95% CI = 27.4%, 73.1%). In contrast, only 16.4% (95% CI = 7.0%, 33.9%) of those without a meniscectomy had radiographic knee OA.
Conclusions:
The findings of Claes et al reflected a radiographic knee OA prevalence at a minimum average of 10 years' postautologous ACL reconstruction that was lower than commonly perceived (up to 79%). In addition, meniscectomy was an important risk factor (3.54-fold increase) for developing OA after ACL reconstruction.
Key Words: osteoarthrosis, prevalence, outcomes
COMMENTARY
Anterior cruciate ligament (ACL) injury is common among high school, collegiate, and recreational athletes. When treating the injury, clinicians need to consider a multitude of factors, particularly if other structures, such as the meniscus or articular cartilage, are damaged. Although clinicians and patients often focus on selecting treatments that facilitate a fast return to participation without exposing the joint to further injury after ACL reconstruction, they should also consider the long-term risk for developing osteoarthritis (OA) and associated functional disability, reduced quality of life, and economic burdens (eg, loss of wages, health care costs).1 In this recent meta-analysis, Claes et al2 reported that the prevalence of radiographic knee OA after ACL reconstruction was approximately 28% when knee OA was classified by radiographic evidence of joint-space narrowing. They also found that patients who underwent meniscectomy might be 3.54 times more likely to have radiographic knee OA after ACL reconstruction than those without meniscectomy. As athletic trainers, we need to focus not only on primary prevention of knee injuries (which is a key risk factor for the onset of OA) but also on the secondary prevention of the long-term sequelae of OA. The goals of secondary prevention could include reducing the risk of further injury to the damaged joint.
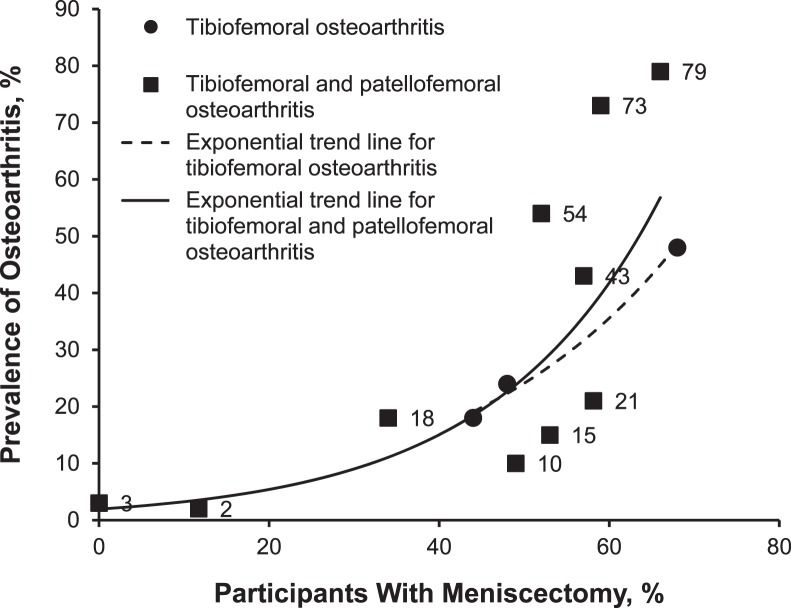
Authors of research studies that assess radiographic knee OA after ACL injury have reported conflicting prevalence rates over the last several years, making it difficult to identify modifiable risk factors for OA after an ACL injury that could be therapeutic targets. The meta-analysis by Claes et al consisted of 16 studies in which the prevalence rates in the individual studies ranged from 2% to 79%. This wide range is attributed to meniscectomy status: 16.4% and 50.4% prevalence for those without or with a meniscectomy, respectively. Furthermore, we conducted a secondary analysis of the Claes et al data and found that as the prevalence of meniscectomy increased, so too did the prevalence of radiographic knee OA (Figure). In the studies with the highest OA prevalence rates (79%, 73%, and 54%), more than 50% of participants had undergone meniscectomy, whereas in the studies with less than 20% OA prevalence rates, meniscectomy rates were very low (2%, 3%, and 10%). The relationship between meniscectomy and OA is not surprising due to the altered joint mechanics (eg, increased local contact pressure) and joint biochemistry (eg, increased inflammation) associated with meniscectomy.
Figure.
Prevalence of radiographic knee osteoarthritis in patients who underwent anterior cruciate ligament reconstruction and concomitant meniscectomy. Data are from the meta-analysis of Claes et al.2
Although Claes et al focused only on knees after autologous ACL reconstruction, another systematic review3 demonstrated that individuals treated with an ACL reconstruction or conservative treatment had similar prevalences of knee OA (32.6%–51.2% with reconstruction, 24.5%–42.3% with conservative care). Furthermore, Frobell et al4 recently conducted a randomized clinical trial and reported that 26% of participants had radiographic knee OA within 5 years of injury, regardless of treatment strategy (ie, early ACL reconstruction, optional-delayed ACL reconstruction, or no ACL reconstruction with rehabilitation only). Therefore, standard treatment strategies are not ameliorating the risk of knee OA, despite attempts to restore joint strength, function, and stability. Ostensibly, we lack sufficient data to assess the risk for knee OA after contemporary treatment interventions and protocols (eg, different ACL grafts, surgical techniques, rehabilitation protocols, return-to-play criteria).
Sensitivity analysis of the effect of meniscal injury on knee OA post–ACL reconstruction is warranted but was limited in the current study. It is yet to be determined how meniscal injury management, such as meniscal repair or minimal resection, preserves joint integrity (thereby minimizing the loss of meniscal function) and function. Because data regarding meniscal repairs were included in the nonmeniscectomy category, we do not know the role of this intervention in the development of radiographic knee OA. Given the current clinical trend to either preserve the meniscus by repair or remove as little tissue as possible, we need more information regarding outcomes. Unfortunately, Claes et al were unable to determine whether the meniscectomies were partial or total, because many of the studies lacked these key details. These questions emphasize the need for standardization when reporting meniscal status, which ultimately can be translated to evidence-based patient care.
Claes et al did not account for age, although it is an important risk factor for developing knee OA. The mean age of patients in 11 of the 16 studies was 38.9 years at an average follow-up of 10 to 12 years. In the United States, individuals between 35 and 45 years of age are reported5 to have a prevalence of symptomatic knee OA of 1.74% to 5.53%. Although radiographic OA is associated with a more liberal definition (strictly defined by radiographs and not accounting for symptoms individuals may be experiencing) than symptomatic OA, these estimated numbers are still not even a quarter of the prevalence that Claes et al reported (28%). Despite the fact that individuals without a meniscectomy have a lower prevalence of OA, we need to acknowledge that 16.4% is still a high prevalence for OA among a relatively young population. As health care professionals, we must recognize that almost one-third of our patients with ACL reconstructions may have early-onset radiographic OA at approximately 10 years after surgery and may be at risk for pain, disability, and other burdens (eg, lost wages, increased health care costs, reduced quality of life). Many of these patients may live with pain and disability for more than half their lives.
This meta-analysis had several additional limitations. Claes et al included only studies of patients who underwent autologous ACL reconstruction; their findings are not applicable to the patients who undergo reconstruction with allografts or synthetic grafts or opt for nonsurgical conservative care. The generalizability of this study to other graft types (eg, hamstrings autografts) is also limited because the authors of most of the studies reviewed by Claes et al primarily used bone-patellar tendon-bone grafts. Similarly, the rapid evolution of ACL surgical procedures and clinical rehabilitation also challenges the generalizability of these findings. Unfortunately, because Claes et al had a minimum follow-up time of 10 years, these data may not be clinically relevant to today's athletes who are receiving cutting-edge ACL reconstruction techniques or meniscal treatments. Furthermore, our understanding of whether current treatment strategies (eg, surgery, rehabilitation, return-to-play criteria) modify the risk for OA will be delayed until more sensitive imaging techniques (eg, magnetic resonance imaging) are adopted in clinical trials of ACL injury treatments. In the meantime, it is important to develop effective strategies to ameliorate the symptoms of those who may be living with this debilitating disease for more than half their lives. Last, Claes et al did not report any sex-specific results. Knowing whether differences exist between males and females would allow clinicians to better understand OA pathology and improve care for their patients. Accounting for sex differences would also allow us to identify trends and risk factors.
Despite these limitations, certain steps and solutions are clear. We should strive to standardize the reporting of key risk factors (eg, meniscal status), criteria by which OA is defined, and use of sensitivity analyses or quality rating of studies (or both). If reporting details are standardized, researchers and clinicians can more readily compile and analyze data to determine which factors modify the risk for knee OA. However, not only does the way in which research is reported need to be altered, but we must also address changes in current treatment and prevention interventions.
CONCLUSIONS
The Claes et al meta-analysis provides a framework and direction for conducting future evidence-based OA research. Although they reported a lower rate of knee OA after ACL reconstruction than is commonly perceived, it is important to realize that this population was at greater risk than the general population. Equally important is that many patients who undergo ACL reconstruction, particularly with a meniscectomy, will spend more than half their lives with knee OA and its debilitating effects. Accordingly, athletic trainers as health care professionals have a responsibility to address the management of ACL injury and long-term disease prevention in addition to facilitating return to play. Education is key for providing information regarding further risk, lifestyle changes, and maintaining an active lifestyle and healthy weight; implementing appropriate rehabilitation programs would also markedly benefit these individuals. Osteoarthritis is not an inevitable consequence of ACL reconstruction.
REFERENCES
- 1. Katz JN, Losina E. OARSI. Primer. Chapter 2: burden of OA-health services and economics . Osteoarthritis Research Society International Web site. http://primer.oarsi.org/content/chapter-2-burden-oa-health-services-and-economics. Accessed August 10, 2015. [DOI] [PMC free article] [PubMed]
- 2. Claes S, Hermie L, Verdonk R, Bellemans J, Verdonk P. . Is osteoarthritis an inevitable consequence of anterior cruciate ligament reconstruction? A meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2013; 21 9: 1967– 1976. [DOI] [PubMed] [Google Scholar]
- 3. Harris K, Driban JB, Sitler MR, Cattano NM, Hootman JM. . Five-year clinical outcomes of a randomized trial of anterior cruciate ligament treatment strategies: an evidence-based practice paper. J Athl Train. 2015; 50 1: 110– 112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Frobell RB, Roos HP, Roos EM, Roemer FW, Ranstam J, Lohmander LS. . Treatment for acute anterior cruciate ligament tear: five year outcome of randomised trial. BMJ. 2013; 346:f232. [DOI] [PMC free article] [PubMed]
- 5. Losina E, Weinstein AM, Reichmann WM, et al. Lifetime risk and age at diagnosis of symptomatic knee osteoarthritis in the US. Arthritis Care Res (Hoboken). 2013; 65 5: 703– 711. [DOI] [PMC free article] [PubMed] [Google Scholar]