Significance
This study adds to the state of the art by analyzing the impact of International Monetary Fund (IMF) programs on children’s health, mediated by their parents’ education. It is the first to combine macrodata and microdata to address this issue systematically across five dimensions of child health: water, malnutrition, shelter, sanitation, and health care access. The sample represents about 2.8 billion (about 50%) of the world’s population in year 2000. Using multilevel models, we find that, although IMF programs do not correlate directly with child health indicators, they reduce the protective effect of parental education on child health, especially in rural areas, and have a mixed impact across the five dimensions of urban child health.
Keywords: International Monetary Fund, education, child health, development, structural adjustment
Abstract
Parental education is located at the center of global efforts to improve child health. In a developing-country context, the International Monetary Fund (IMF) plays a crucial role in determining how governments allocate scarce resources to education and public health interventions. Under reforms mandated by IMF structural adjustment programs, it may become harder for parents to reap the benefits of their education due to wage contraction, welfare retrenchment, and generalized social insecurity. This study assesses how the protective effect of education changes under IMF programs, and thus how parents’ ability to guard their children’s health is affected by structural adjustment. We combine cross-sectional stratified data (countries, 67; children, 1,941,734) from the Demographic and Health Surveys and the Multiple Indicator Cluster Surveys. The sample represents ∼2.8 billion (about 50%) of the world’s population in year 2000. Based on multilevel models, our findings reveal that programs reduce the protective effect of parental education on child health, especially in rural areas. For instance, in the absence of IMF programs, living in an household with educated parents reduces the odds of child malnourishment by 38% [odds ratio (OR), 0.62; 95% CI, 0.66–0.58]; in the presence of programs, this drops to 21% (OR, 0.79; 95% CI, 0.86–0.74). In other words, the presence of IMF conditionality decreases the protective effect of parents’ education on child malnourishment by no less than 17%. We observe similar adverse effects in sanitation, shelter, and health care access (including immunization), but a beneficial effect in countering water deprivation.
Parental education is a key determinant of child health. Across developing countries, children born to mothers with no education are three times more likely to die at a young age than those born to mothers with secondary education (1). At the same time, the allocation of scarce resources to essential social and public health institutions in low- and middle-income countries frequently unfolds under the policy parameters set by powerful international financial institutions (2), like the International Monetary Fund (IMF).
The IMF monitors the global economy and provides support to governments in economic turmoil, notably via its lending programs. In exchange for low-cost financing, governments must agree to implement a set of reforms, known as “conditionalities.” The IMF relies on conditionalities to foster macroeconomic stability through “correct[ing] maladjustments in [government] balance of payments without resorting to measures destructive of national or international prosperity” (3).
The success of IMF programs and the degree of collateral damage they produce for public health is an ongoing controversy (2, 4–6). Already in the 1980s, the years of recession and omnipresent IMF programs especially in Africa and Latin America, the United Nations Children’s Fund (UNICEF) cautioned against endangering vulnerable households and child health (7). Following the recent global recession, further UNICEF reports revealed that policy makers remained focused on short-term economic considerations, while rolling back critical education and health interventions (8). The IMF responded to such critiques by emphasizing its commitment to strengthening public health. Its Poverty Reduction Strategy (9) has—purportedly—been tailored to the needs of low-income countries (10). However, although past research has studied the impact of IMF programs on child health (11–13), no study—to our knowledge—has conducted a systematic global analysis using microdata.
This study assesses the connections between IMF programs and parents’ ability to protect their children’s health. Educational attainment is a reliable indicator of parents’ earning and socioeconomic class (14), and thus, households’ ability to withstand economic change (15–18). As a tool to promote development, governments provide free or low-cost education. Parents benefit as their human capital increases, giving them more capabilities to nurture their children. Conditional cash transfer programs keep children in schools and away from child labor, which increase their cognitive capacities and improve their health (19). However, access to and the value of education can be affected by economic reform policies (20, 21). In the pursuit of macroeconomic stability, IMF programs include austerity measures that are associated with significant rollbacks of these social policies (22). For instance, governments are forced to spend less on teachers and contracting teachers’ wages. Tuition costs are passed on to the households, reducing parents’ access to quality education. Their human capital decreases, their employability, and earnings (7), ultimately affecting the health of their children. Consequently, we hypothesize a link between such IMF-mandated austerity measures and the protective effect of parental education on child health.
Data and Methods
Data.
This study combines country, household, and child-level data; SI Appendix, Table S1 reports sources. The microdata comes from the Demographic and Health Survey (DHS) and UNICEF’s Multiple Indicator Cluster Survey (MICS). Building on a two-stage cluster sampling procedure, the aim of these nationally representative surveys is to measure living conditions (23). In the first stage, the DHS and MICS statisticians construct a sampling frame defining the stratification of the population by key demographics, using the latest census. This frame numbers country regions into primary sampling units (clusters), which are then further sampled with a probability proportional to their population size. In the second stage, all households are listed in each cluster, of which about 20–30 are randomly selected for an on-location face-to-face interview. The sample sizes normally vary between 4,000 and 30,000 households depending on population size, with a typical response rate exceeding 90% (24). With these standardized procedures, DHS and MICS surveys enable global analyses.
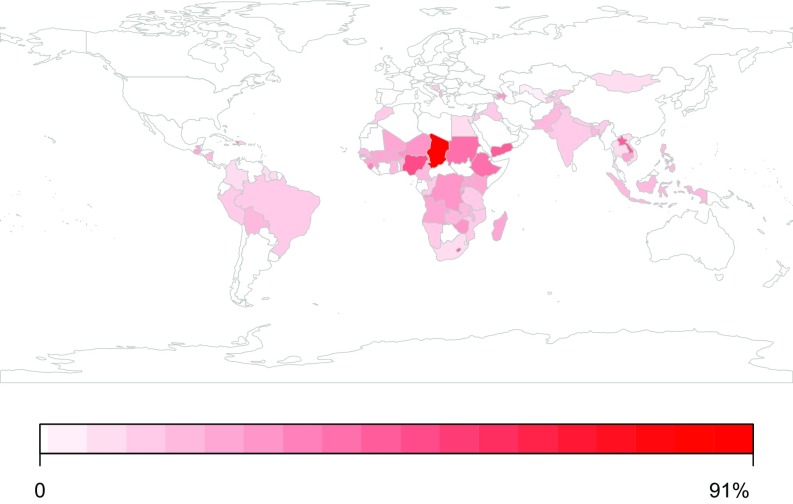
Our pooled sample represents about 2.8 billion (∼50%) of the world’s population by year 2000. Fig. 1 captures this sample’s geographical distribution of child health deprivation. Our dataset includes 67 low- and middle-income countries sampled once, with different timing, determined by the DHS and MICS. The surveys were conducted around the year 2000 with a range of about ±5 y, just before the substantial global efforts put in place by various agencies to immunize children: notably, before the Millennium Development Goals were taking effect and just before the Bill and Melinda Gates Foundation became involved. SI Appendix, Table S2 outlines sample years and sizes.
Fig. 1.
World map of severe child health deprivation. Data sample and average severe child health deprivation (in percentage). Authors’ calculations are based on the microdata. White color indicates excluded country.
We measure child health across five dimensions: children’s access to nonhazardous sanitation, improved water sources, and vital health care (including immunization), safe housing, and whether they are sufficiently nourished. We derive these definitions from Gordon et al.’s (25) pioneering study of child poverty in the developing world. Table 1 outlines how these five dimensions are operationalized. A core strength of these measures is that they indicate actual access to resources, instead of consumption opportunities as is done in monetary approaches. The term “deprivation” is understood as a latent continuum that ranges from no to mild, moderate, severe, and extreme deprivation (26). Severe and extreme deprivations describe circumstances that exert highly deleterious effects on children’s health, eventually resulting in mortality (25). Table 1 outlines these five thresholds; when a child’s health circumstances reaches over these cut-points, then that child is deprived in that dimension (covering both extreme and severe), with a resulting dichotomous outcome variable.
Table 1.
Individual-level indicator—dependent variables—five dimensions of overall child health
| Deprivation | Definition | Cases | Percent deprived, % |
| Water | Children who only have access to surface water (e.g., rivers) for drinking or who lived in households where the nearest source of water was more than 15 min away. Children <18 y old. | 1,941,734 | 24 |
| Malnutrition | Children whose heights and weights for their age were more than −3 SDs below the median of the international reference, that is, severe anthropometric failure. Children <5 y old. | 815,264 | 7 |
| Shelter | Children in dwellings with more than five people per room and/or with no flooring material. Children <18 y old. | 1,926,435 | 51 |
| Sanitation | Children who had no access to a toilet of any kind in the vicinity of their dwelling, that is, no private or communal toilets or latrines. Children <18 y old. | 1,940,599 | 28 |
| Health (immunization and health access) | Children who had not been immunized against diseases or young children who had a recent illness involving diarrhea and had not received any medical advice or treatment [polio, measles, DPT (against diphtheria, pertussis, and tetanus), tuberculosis (Bacillus Calmette-Guérin) recommended by the WHO]. Children <5 y old. | 944,895 | 13 |
We use the head of household’s educational attainment from the DHS and MICS as a measure of parental education. The head is the person leading the household’s family affairs and is commonly the oldest man (27). We focus on the head of household’s rather than the mother’s education, as the head, with his or her elevated status in the family, is likely to affect both the child’s and mother’s behavior (28). Educational attainment, regardless of whether it is the head’s or the mother’s, correlates highly with poverty; less educated respondents consistently have lower socioeconomic status than their educated counterparts. We include a household geographical indicator to capture urban vs. rural disparities. Our design controls for the number of adults and children living in the household; the more adults dwelling in the households, the more likely children are properly cared for (29). The analysis also controls for the age and gender of the child. SI Appendix, Table S3 shows the frequency of children by their age, head’s educational attainment, and household location.
Finally, we draw on country-level data. The presence or absence of IMF programs in a particular country and year is measured as a dummy variable (30). This measure indicates that the government and the IMF have agreed to implement a program to adjust the fiscal imbalances in the target country, in exchange for a loan (2). The starting year defines when the program was approved, if the agreement was signed in the first half of the year; otherwise, the starting period is the following year. These programs are tailored to each country, but will contain on average 40 conditions of which about 15 tend to be structural (31). Structural adjustment is the most intrusive type of condition, often reducing social spending considerably, containing privatization or liquidations of state-owned enterprises in various public sectors (5): energy, agriculture, water and sewage systems, healthcare, and education. Other types of conditions include tax increases and trade liberalization. With the use of a dummy variable, we assume that programs have similar effects on child health. Even though an imperfect indicator, this approach follows conventions in the field (2, 32), including work by the IMF itself (30). Unraveling the heterogeneous effect of conditionalities is an important future research task.
The analysis also included additional country-level variables, defined in SI Appendix, Table S1, that could confound the effect on child health; SI Appendix, Table S4 shows descriptive statistics, whereas SI Appendix, Table S5 outlines correlations.
Statistical Methods.
The analysis has two core equations. First, we estimate a Heckman selection model to predict a country’s likelihood to participate in an IMF program, as program participation is not random. Poorer countries, being more vulnerable to economic turmoil, are more likely to solicit IMF support (2). Relying on a version of the specification used by the IMF’s Independent Evaluation Office (33), we use the following: IMF program participation in the previous year, gross domestic product (GDP) growth, democracy, current account balance, GDP per capita, the total number of countries on IMF programs, and United Nations voting affinity with Group of Seven countries. The latter two variables fulfill the exclusion restriction: a variable that is significant in explaining the country’s participation decision in an IMF program, but is not correlated with the dependent variable of the outcome equation. After estimation, we calculate the inverse Mills ratio to be included in the outcome equation to control for the unobserved factors, potentially affecting selection into programs (34). A complete outline of the motivation behind the Heckman model is given in SI Appendix, SI Text.
Second, we estimate the IMF effect on child health with multilevel equations to account for the hierarchical nature of our data (35): children are nested in households, households in neighborhoods, neighborhoods in broader geographical regions, and last, all these levels are nested in countries. Because of some sparse observations within households and by neighborhood, the estimation does not converge when we include these levels. We settled on a parsimonious two-level model: children nested in countries. This model is likely to give some upward-biased standard errors for the household variables but does not otherwise affect the estimates:
Our base model is a random intercept logit model with child i nested in country k. The random term captures each country’s deviation from the conditional mean (the intercept); it is assumed to be normally distributed with variance . The outcome variable measures whether a child is severely health deprived or not, in five dimensions (the index d). The key explanatory variable, , indicates whether an IMF agreement was in place in the preceding year. controls for selection bias, as described above: a positive effect implies that unobserved factors, which make IMF program participation more likely, increase the probability of severe deprivation. A number of country controls, , as well as household and child controls are included, : log GDP per capita, received foreign aid, health spending, civil war, population dependency ratio (share of the population aged under 15 and over 65), democracy, and year of interview. All country-level covariates are lagged 2 y. The superscript indicates the level of analysis (a designates the child level, and b designates the country level).
Time is present in two ways in our research design: first, in terms of the sampling date of when the DHS and MICS surveyed children’s living conditions (which varies between countries); and second, as lags of the country-level covariates (as described above, we use an identical lag structure across countries). Each child (and country) is only sampled once, thus rendering the design of our study cross-sectional. IMF programs’ effect on children will likely take some time to materialize and to fade out; using the presence of a program in the previous year has been proposed as an appropriate way of capturing this lagged impact (12, 13). We lag the pretreatment conditions by 2 y and thus avoid posttreatment bias, which will give us the total treatment effect (36).
Although our design does not use quasiexperimental design methods, such as difference-in-differences, which would require preprogram and postprogram measurements of child health, it nevertheless captures differences in child health by parental educational attainment between countries under treatment and countries serving as controls. We do this by including a set of interaction terms to our base model to capture these moderation effects (37). We stratify the analysis further by evaluating this effect by household location, as the literature has found large heterogeneity when looking at disparities between urban and rural households in low- and middle-income countries (29).
The lack of pretreatment and posttreatment measurement of child health implies that we cannot study shifts in deprivation prevalence and trajectories of child health as a function of IMF programs. Ideally, a panel study of children followed over time, before and after the presence of an IMF program, and in countries with and without a program, would enable a full-fledged causal analysis. Although we do not claim causality, our approach nonetheless sheds important light on the complex associations between IMF programs, parental education, and child health.
Results
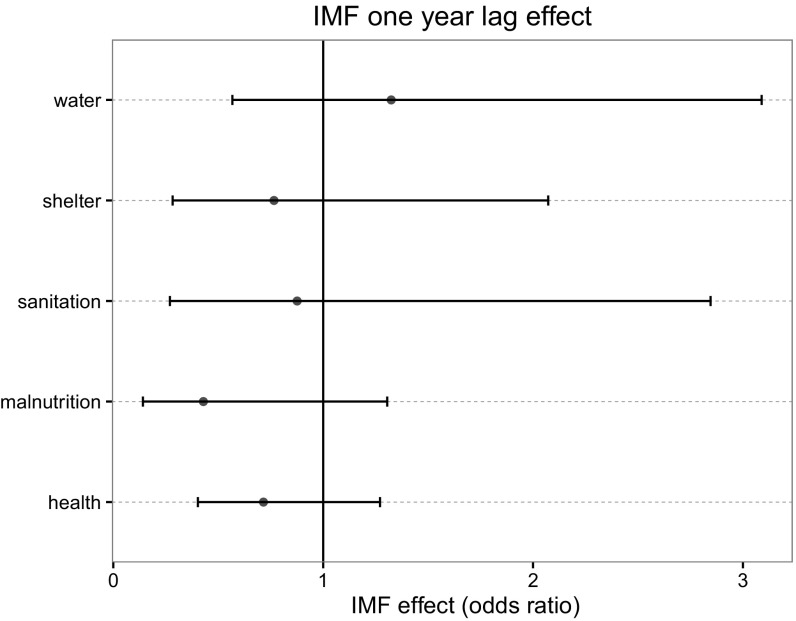
Fig. 2 visualizes the estimated impact of IMF programs on the five dimensions of child health—the complete regressions results are presented in SI Appendix, Table S6. Programs have no direct statistically significant effect. The confidence intervals are large, as this is a country-level measure with weaker statistical power compared with the child-level measures. As expected, as the head of household’s level of education increases, the odds of severe child health deprivation decrease. For instance, living in a household where at least one of the parents has primary education corresponds to a 16% drop in the odds of severe malnourishment compared with one with no parental education; the difference is even starker, at 42%, for parents with secondary education. This beneficial effect of parental education is consistent and significant across all five child health dimensions.
Fig. 2.
Marginal effect of IMF program on five dimensions of child health. Above OR 1, the effect is adverse; below 1, the effect is beneficial (the lower OR, the less likely the child is deprived). The models cannot detect any significant effect. Error bars are 95% CIs.
Our models reveal a highly pronounced gap between rural and urban populations: a shift from urban to rural areas increases the odds of water and sanitation deprivation prevalence by a factor of 5. For malnourishment and health deprivation, the same shift is associated with a 50% increase. Although these disparities are well known in the development literature (29, 38), less is known about how they change in the presence of IMF programs.
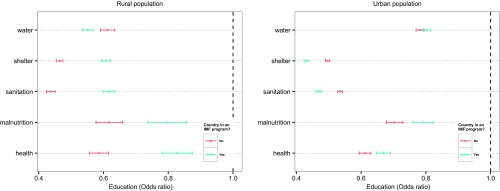
In the next step, we estimate the moderation effect of IMF programs on education and household location. Fig. 3 visualizes how the marginal effects of education change according to the presence or absence of programs, stratified by rural vs. urban context; SI Appendix, Table S8 shows these exact interactive effects. SI Appendix, Table S7 reports the full estimated model, which include a three-way interaction between programs, head of household’s education, and household’s location (urban vs. rural). We reduced the three education categories (no education, primary, and secondary plus) to two (no education vs. education), facilitating interpretation. We report the unreduced models in SI Appendix, Table S15. Except for location interacted with education for health deprivation, all interaction terms are statistically significant.
Fig. 3.
The protective effect of education in the urban vs. rural population. The panel shows the effect of the head of household’s education on their children’s health outcomes (educated vs. noneducated), moderated by country participation in IMF programs. The figure captures the partial marginal effect on the OR scale with 95% CIs. Above OR 1, the effect is adverse; below 1, the effect is beneficial. When a country participates in a program, the beneficial effect of parental education against malnutrition and health deprivation tends to weaken in both the urban and rural population; the beneficial effect of parental education increases in shelter and sanitation deprivations in urban population.
For rural populations, the protective effect of parental education decreases significantly when countries participate in IMF programs. Children face higher odds of suffering from deprivation in four out of the five dimensions. In the absence of a program, children living in an educated household have a reduced odds of being malnourished by 38% [odds ratio (OR), 0.62; 95% CI, 0.66–0.58], compared with children of uneducated households; under adjustment, this beneficial effect drops to 21% (OR, 0.79; 95% CI, 0.86–0.74). In other words, the presence of IMF conditionality erodes the protective effect of education against child malnourishment by no less than 17% in rural contexts. This effect is comparable across the other deprivations. In shelter deprivation, the presence of IMF yields an erosion of 15%; in sanitation, the decrease is 18%; and in health (healthcare including immunization), the loss is 24%. Water deprivation is an exception: living in an educated household improves children’s odds of avoiding water deprivation by 39% (OR, 0.61; 95% CI, 0.63–0.59) to 45% (OR, 0.55; 95% CI, 0.57–0.53).
In contrast, children in urban areas see no change in the odds of water deprivation, but they experience a beneficial change in the odds of being shelter and sanitation deprived. The shift from no to some parental education corresponds to a change from a 50% (OR, 0.5; 95% CI, 0.50–0.49) to 57% (OR, 0.43; 95% CI, 0.44–0.42) decrease in the odds of suffering from shelter deprivation, an improvement of 7%. In sanitation deprivation, the improvement is also 7%. Conversely, urban children experience a deterioration in the odds of being malnourished and health deprived (healthcare including immunization): 9% and 6%, respectively.
SI Appendix, SI Text discusses and SI Appendix, Tables S10–S14 present our tests of the robustness of the selection equation, with alternative specifications; SI Appendix, Figs. S1 and S2 show how these specification affect the outcome model. Overall, these tests show that the results produced in the outcome stage hold even with a less robust selection equation (less predictive probit model). SI Appendix, SI Text presents further sensitivity analysis, focusing on the specification of the multilevel models (outcome stage)—keeping the selection equation constant. First, in the interaction analysis above, we reduced the education three-level categories to a binary one (educated vs. noneducated) for clarity of presentation purposes. We present the result for the three-level interaction in SI Appendix, Table S15 and Figs. S3 and S4. Although there are some nuances in the moderation effect, the inference we draw are consistent. Second, instead of 1-y lagged effect, we estimated the main effect of IMF programs using three versions of historical burden: sum of programs (SI Appendix, Table S16 and Fig. S5), count of structural conditions (SI Appendix, Table S17 and Fig. S6), and count of quantitative conditions (SI Appendix, Table S18 and Fig. S7). The results confirm the absence of significant direct relationships with all five dimensions of child health. SI Appendix, SI Text also outlines checks of key multilevel model assumptions, normality of residuals (SI Appendix, Figs. S8–S12) and homoscedasticity (SI Appendix, Figs. S13–S17). These tests show a fair conformity to these assumptions. The inferences drawn from this study hold even by controlling for potential outliers (e.g., Sudan and Malawi). Fourth, sample (DHS and MICS) weighted estimations are presented in SI Appendix, Table S9, showing high consistency with the unweighted estimations used in the main results. Last, we face no serious multicollinearity between our key country variables, as shown by the correlation matrix in SI Appendix, Table S5.
Discussion
This study has shown that IMF programs erode the protective effect of parental education on child health, especially in rural areas. We also find some mixed results in urban areas. Children of educated parents still have better health than their peers with uneducated parents. However, this gap shrinks under programs. We offer some potential explanations of these observations by highlighting the broader relationship between IMF programs and the societal effects of austerity (5, 7, 13, 32, 38–40). Our study raises four main questions.
First, and most importantly, why does the protective effect of parental education erode under IMF programs? Our results indicate that austerity undermines the benefits and value of educational capital. We propose a series of interlinked ways in which this can happen. A first (direct) mechanism involves the impacts of reduced fiscal space under austerity, which undermines a government's capacity to provide tuition-free or low-cost quality education. On the one hand, fewer parents will gain access to education. On the other, even those who may get an education, will be affected by IMF-mandated government wage bill ceilings, which can limit the numbers of teachers in public schools, leading to staff shortages, reduced teaching quality, and further devaluation of education (21, 41). This depreciation of educational resources is then likely to reduce the beneficial effect of parental education on child health, weakening the capabilities of households and communities (20).
Another (indirect) mechanism is intertwined with the first: under austerity, governments spend less not only on education but also on the protection of labor. Reductions in public spending on social policies, mandated by the IMF, can yield social insecurity and wage repression, resulting in a downward mobility for the middle classes. In the context of rapidly changing socioeconomic environments during periods of structural adjustment programs, degrading employment prospects wrought by economic deregulation curb the otherwise important marginal utility of basic educational resources in the making of parents' ability to protect their children (4, 13, 42). As a result, the gap between parents who have an education and those who lack gets reduced.
Over and above these mechanisms, parents lacking an education in the first place—who tend also to be the poorest segment of the population—are already economically excluded from the labor market, and therefore, these changes seems to affect them less.
Second, why is the protective effect of education weaker in rural compared with urban areas, under IMF programs? It is plausible that, under economic turmoil, governments will channel scarce resources toward cities rather than villages, as these are major sites for corporate profit, and thus can generate further tax revenue (4). This, in turn, implies that educated rural families have a harder time mobilizing resources for the benefits of their children.
Third, why do the benefits of education increase in rural areas in relation to water deprivation? Among its manifold privatization conditionalities, water privatization has been imposed by the IMF in developing countries (43). Against the backdrop of previous research, our findings suggest that the more educated—who tend to also have higher socioeconomic status—stand out as the principal beneficiaries of this measure. As people will have to pay the full cost for water access, the poor will tend to choose less costly, albeit less safe, water sources (4). The availability of water is more widespread in the urban areas, which can explain why no significant change is observed in our models.
Fourth, why do the benefits of education decrease in relation to malnutrition and health care access, not only in rural but also in urban areas? A potential mechanism lies in the IMF’s Poverty Reduction Strategy, which might be equalizing the risk exposure across different educational, socioeconomic, and spatial landscapes (44). However, the Poverty Reduction Strategy commenced post-1999, meaning only some of the surveys in our sample would pick up this potential effect. Another possible explanation pertains to the seeming inefficiency of health systems, as evidenced by the insignificant effect of health spending in our models. The absence of any effect is consistent across different measures for health spending; of eight different, it is only significant in one case (SI Appendix, Tables S19 and S20). Realistically, increased health spending should have some beneficial effect on children’s health. However, under IMF programs, government subsidies for immunization, healthcare, and food are often the first to be dismantled (13, 45). This may indicate that health-related resources are inefficiently allocated by governments implementing adjustment programs. Further research can probe the concrete mechanisms through which conditionalities affect health system efficiency.
Before evaluating the policy relevance of this study, it is important to note its main limitations. First, this study focuses on program participation as an aggregate package of conditions. Disentangling the effect of the various types of conditions on child health is an important task for future research (31). Second, the research design permits mainly a discussion of correlation but not causation. For lack of a proper time dimension for the outcome variable, our study cannot establish the nature and direction of causality. Although we used a lagged treatment variable for IMF programs and the country-level covariates, we cannot control for endogenous child health trends (initial values before program implementation). Third, we used Gordon et al. and UNICEF’s definitions (thresholds) for severe child health deprivations (25). Evaluating how the results change across different thresholds is an important task for future studies. Fourth, we focused on the educational attainment of the head of household, who tends to be the husband or the oldest male of the family (27). Although this is an encompassing proxy of the household’s socioeconomic status (28), there might be further differential effects in relation to the gender of the child and paternal structures. Our results show, for example, that, except for access to health services including vaccination where we find no significant difference between boys and girls, for the other outcomes boys tend to have higher odds of being deprived. The difference is small for water, shelter, and sanitation (1% higher odds), and larger in nutritional deprivation (6%). This differential might be explicated by further disentangling family gender compositions.
Although we used data sampled over a decade ago, there are substantive reasons to believe that the effects of IMF programs are still comparable today. Even though the IMF has sought to change its public image and purports to have transformed its lending practices (9), its programs still aim toward the same goals: to balance government spending via steep reductions in social spending, privatization of public services, and declines in the provision of public goods as educational resources (8, 31, 46).
In sum, our study suggests that IMF programs are working at cross-purposes vis-à-vis child health. IMF interventions seek to foster economic stability, which yields beneficial effects for the population. However, at the same time, these IMF-mandated adjustment measures diminish the protective effect of parental education on child health. Government officials need to ensure that policy recommendations or demands made by the IMF do not entail inadvertent deleterious effects, whether directly or via erosion of parental resources. One way of achieving this is to expand the recently launched cocooperation among the IMF, the World Bank, and UNICEF (47, 48), geared toward closer monitoring of the sociospatially multidirectional impacts of adjustment on children. This effort would give policy makers the opportunity to identify both beneficial and adverse effects over time, and thus to orient adjustment policies toward fostering economic stability without endangering population health.
Supplementary Material
Footnotes
The authors declare no conflict of interest.
This article is a PNAS Direct Submission. A.S. is a guest editor invited by the Editorial Board.
See Commentary on page 6421.
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.1073/pnas.1617353114/-/DCSupplemental.
References
- 1.UNICEF . The State of the World’s Children 2015. United Nations Children’s Fund; New York: 2014. [Google Scholar]
- 2.Vreeland JR. The International Monetary Fund: Politics of Conditional Lending. Routledge, Taylor and Francis Group; New York: 2007. [Google Scholar]
- 3.IMF 2016 Introduction to the IMF. Available at www.imf.org/external/index.htm. Accessed August 30, 2016.
- 4.Babb S. The social consequences of structural adjustment: Recent evidence and current debates. Annu Rev Sociol. 2005;31:199–222. [Google Scholar]
- 5.Kentikelenis AE. Structural adjustment and health: A conceptual framework and evidence on pathways. Soc Sci Med. February 23, 2017 doi: 10.1016/j.socscimed.2017.02.021. [DOI] [PubMed] [Google Scholar]
- 6.Summers LH, Pritchett LH. The structural-adjustment debate. Am Econ Rev. 1993;83:383–389. [Google Scholar]
- 7.Cornia GA, Jolly R, Stewart F. Adjustment with a Human Face. Vol 1: Protecting the Vulnerable and Promoting Growth. Clarendon; Oxford: 1987. [Google Scholar]
- 8.Ortiz I, Cummins M. A Recovery for All: Rethinking Socio-Economic Policies for Children and Poor Households. UNICEF; New York: 2012. [Google Scholar]
- 9.IMF 2016 Factsheet–Poverty Reduction Strategy in IMF-Supported Programs. Available at www.imf.org/external/index.htm. Accessed August 8, 2016.
- 10.IMF 2005 Strengthening the IMF’s Support for Low-Income Countries. Available at https://www.imf.org/external/np/exr/ib/2005/092105.htm. Accessed August 8, 2016.
- 11.Curtis E. Child health and the international monetary fund: The Nicaraguan experience. Lancet. 1998;352:1622–1624. doi: 10.1016/S0140-6736(98)03248-6. [DOI] [PubMed] [Google Scholar]
- 12.Pandolfelli LE, Shandra J, Tyagi J. The International Monetary Fund, structural adjustment, and women’s health: A cross-national analysis of maternal mortality in sub-Saharan Africa: Structural adjustment maternal mortality. Sociol Q. 2014;55:119–142. [Google Scholar]
- 13.Shandra CL, Shandra JM, London B. The International Monetary Fund, structural adjustment, and infant mortality: A cross-national analysis of sub-Saharan Africa. J Poverty. 2012;16:194–219. [Google Scholar]
- 14.Gakidou E, Cowling K, Lozano R, Murray CJ. Increased educational attainment and its effect on child mortality in 175 countries between 1970 and 2009: A systematic analysis. Lancet. 2010;376:959–974. doi: 10.1016/S0140-6736(10)61257-3. [DOI] [PubMed] [Google Scholar]
- 15.Daoud A, Halleröd B, Guha-Sapir D. What is the association between absolute child poverty, poor governance, and natural disasters? A global comparison of some of the realities of climate change. PLoS One. 2016;11:e0153296. doi: 10.1371/journal.pone.0153296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nandy S, Daoud A, Gordon D. Examining the changing profile of undernutrition in the context of food price rises and greater inequality. Soc Sci Med. 2016;149:153–163. doi: 10.1016/j.socscimed.2015.11.036. [DOI] [PubMed] [Google Scholar]
- 17.Garfinkel I, McLanahan S, Wimer C. Children of the Great Recession. Russell Sage Foundation; New York: 2016. [Google Scholar]
- 18.Daoud A, Puaca G. An organic view of students’ want formation: Pragmatic rationality, habitus and reflexivity. Br J Sociol Educ. 2011;32:603–622. [Google Scholar]
- 19.Cornia GA, Danziger SH, editors. Child Poverty and Deprivation in Industrialized Countries, 1945–1995. Clarendon; Oxford: 1997. [Google Scholar]
- 20.Nielsen HD. From Schooling Access to Learning Outcomes: An Unfinished Agenda: An Evaluation of World Bank Support to Primary Education. World Bank Independent Evaluation Group; Washington, DC: 2006. [Google Scholar]
- 21.Rowden R. Impacts of IMF Policies on National Education Budgets and Teachers. Education International Research Institute; Brussels: 2011. [Google Scholar]
- 22.Alexander NC. Paying for education: How the World Bank and the International Monetary Fund influence education in developing countries. Peabody J Educ. 2001;76:285–338. [Google Scholar]
- 23.International ICF. Demographic and Health Survey Sampling and Household Listing Manual. MEASURE DHS; Calverton, MD: 2012. [Google Scholar]
- 24.Corsi DJ, Neuman M, Finlay JE, Subramanian SV. Demographic and health surveys: A profile. Int J Epidemiol. 2012;41:1602–1613. doi: 10.1093/ije/dys184. [DOI] [PubMed] [Google Scholar]
- 25.Gordon D, Nandy S, Pantazis C, Pemberton S, Townsend P. Child Poverty in the Developing World. Polity Press; Bristol, UK: 2003. [Google Scholar]
- 26.Townsend P. Deprivation. J Soc Policy. 1987;16:125–146. [Google Scholar]
- 27.Randall S, Coast E, Leone T. Cultural constructions of the concept of household in sample surveys. Popul Stud (Camb) 2011;65:217–229. doi: 10.1080/00324728.2011.576768. [DOI] [PubMed] [Google Scholar]
- 28.Subramanian SV, Corsi DJ. Moving beyond a maternal perspective to child survival. Indian Pediatr. 2016;53:867–869. doi: 10.1007/s13312-016-0949-2. [DOI] [PubMed] [Google Scholar]
- 29.Halleröd B, Rothstein B, Daoud A, Nandy S. Bad governance and poor children: A comparative analysis of government efficiency and severe child deprivation in 68 low-and middle-income countries. World Dev. 2013;48:19–31. [Google Scholar]
- 30.Clements B, Gupta S, Nozaki M. What happens to social spending in IMF-supported programmes? Appl Econ. 2013;45:4022–4033. [Google Scholar]
- 31.Kentikelenis AE, Stubbs TH, King LP. IMF conditionality and development policy space, 1985–2014. Rev Int Polit Econ. 2016;23:543–582. [Google Scholar]
- 32.Kentikelenis AE, Stubbs TH, King LP. Structural adjustment and public spending on health: Evidence from IMF programs in low-income countries. Soc Sci Med. 2015;126:169–176. doi: 10.1016/j.socscimed.2014.12.027. [DOI] [PubMed] [Google Scholar]
- 33.IEO . Fiscal Adjustment in IMF-Supported Programs. IMF Independent Evaluation Office; Washington, DC: 2003. [Google Scholar]
- 34.Heckman JJ. Sample selection bias as a specification error. Econometrica. 1979;47:153–161. [Google Scholar]
- 35.Goldstein H. Multilevel Statistical Models. 4th Ed Wiley; Chichester, UK: 2011. [Google Scholar]
- 36.Angrist JD, Pischke J-S. Mostly Harmless Econometrics: An Empiricist’s Companion. Princeton Univ Press; Princeton: 2008. [Google Scholar]
- 37.Hosmer DW, Lemeshow S. Applied Logistic Regression. 2nd Ed Wiley-Interscience; New York: 2000. [Google Scholar]
- 38.Daoud A. Quality of governance, corruption, and absolute child poverty in India. J South Asian Dev. 2015;10:1–20. [Google Scholar]
- 39.Harper C, Jones N. Impacts of economic crises on child well-being. Dev Policy Rev. 2011;29:511–526. [Google Scholar]
- 40.Stubbs T, Kentikelenis A, Stuckler D, McKee M, King L. The impact of IMF conditionality on government health expenditure: A cross-national analysis of 16 West African nations. Soc Sci Med. 2017;174:220–227. doi: 10.1016/j.socscimed.2016.12.016. [DOI] [PubMed] [Google Scholar]
- 41.Marphatia AA. The adverse effects of International Monetary Fund programs on the health and education workforce. Int J Health Serv. 2010;40:165–178. doi: 10.2190/HS.40.1.j. [DOI] [PubMed] [Google Scholar]
- 42.Buchmann C. The debt crisis, structural adjustment and women’s education. Int J Comp Sociol. 1996;37:5–30. [Google Scholar]
- 43.Kochhar MK, et al. Is the Glass Half Empty Or Half Full?: Issues in Managing Water Challenges and Policy Instruments. International Monetary Fund; Washington, DC: 2015. [Google Scholar]
- 44.IMF 2013 Factsheet—The Multilateral Debt Relief Initiative—IMF. Available at www.imf.org/external/index.htm. Accessed August 30, 2016.
- 45.Daoud A. (Quasi)scarcity and global hunger: A sociological critique of the scarcity postulate with an effort to synthesis. J Crit Realism. 2007;6:199–225. [Google Scholar]
- 46.Babb SL, Kentikelenis AE. International financial institutions as agents of neoliberalism. In: Cahill D, Cooper M, Konings M, editors. The SAGE Handbook of Neoliberalism. SAGE Publications; Thousand Oaks: 2017. in press. [Google Scholar]
- 47.UNICEF 2015 UNICEF experts available during World Bank Group/IMF Spring Meetings, 17–19 April 2015 (UNICEF, New York). Available at https://www.unicef.org/. Accessed August 12, 2016.
- 48.Newhouse DL, Suarez-Becerra P, Evans M. 2016 New estimates of extreme poverty for children. Policy Research Working Paper No. 7845 (The World Bank, Washington, DC). Available at documents.worldbank.org/curated/en/402511475417572525/New-estimates-of-extreme-poverty-for-children.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.