Significance
People with Parkinson’s disease, the second most common neurodegenerative disorder, have a lower risk and decreased incidence of cancer with the one exception being melanoma. The fact that, compared with other malignancies, melanoma occurs more frequently in patients with Parkinson’s disease and vice versa and that there is an association between a history of melanoma and an increased prevalence of prodromal markers of Parkinson’s disease prompted us to explore the possibility of an inverse biological link between these two diseases. The findings of our study suggest that α-synuclein, one of the key regulators in Parkinson’s disease, although toxic to dopaminergic neurons, is protective for advanced melanoma cells.
Keywords: melanoma, Parkinson's disease, α-synuclein, oligomer modulator treatment, autophagy
Abstract
Recent epidemiological and clinical studies have reported a significantly increased risk for melanoma in people with Parkinson’s disease. Because no evidence could be obtained that genetic factors are the reason for the association between these two diseases, we hypothesized that of the three major Parkinson’s disease-related proteins—α-synuclein, LRRK2, and Parkin—α-synuclein might be a major link. Our data, presented here, demonstrate that α-synuclein promotes the survival of primary and metastatic melanoma cells, which is the exact opposite of the effect that α-synuclein has on dopaminergic neurons, where its accumulation causes neuronal dysfunction and death. Because this detrimental effect of α-synuclein on neurons can be rescued by the small molecule anle138b, we explored its effect on melanoma cells. We found that treatment with anle138b leads to massive melanoma cell death due to a major dysregulation of autophagy, suggesting that α-synuclein is highly beneficial to advanced melanoma because it ensures that autophagy is maintained at a homeostatic level that promotes and ensures the cell’s survival.
In 1972, an article published in the journal Archives of Pathology (1) reported that a patient with Parkinson’s disease (PD), who had been treated with levodopa, developed multiple primary melanomas. For almost 40 y thereafter, little if any attention was paid to a possible link between PD and melanoma. This changed in 2010 when the data of a 31-center North American study were published (2), which showed that the prevalence of melanoma, but not other types of skin cancer, is more than twofold higher in patients with PD than in the general population. Subsequent data from epidemiological as well as clinicopathological studies, conducted in Australia, Asia, and Scandinavia, have not only confirmed this finding, but also found in some cases a six- to eightfold increased risk of melanoma in patients with PD (3–6). Furthermore, a recent study (7) revealed an association between a history of melanoma and increased prevalence of prodromal markers of PD. Using the Utah Cancer Registry as a resource, it was reported (8) that not only PD patients but also their relatives have a significantly elevated risk for melanoma and, conversely, that relatives of patients with melanoma have an increased risk for PD. Given this finding, the authors postulated that there is a genetic association between PD and melanoma. However, two subsequent studies (9, 10) showed that the PD susceptibility loci and PD-specific single nucleotide polymorphisms, identified in genome-wide association studies, neither play a role in melanoma development nor contribute to the association between PD and melanoma. Likewise, a family-based matched cohort study, conducted in Sweden, ruled out familial genetic factors as the reason for the association between PD and melanoma (11).
The causes of PD are not clearly established. However, dysfunctions of the major PD-related genes/proteins—SNCA/α-synuclein, PARK8/LRRK2, and PARK2/Parkin—contribute to the loss of cells in different parts of the brain and foremost in the substantia nigra. The general assumption in the case of α-synuclein is that toxic gain-of-function/overactivity leads to the misfiring and subsequent death of neurons and, in the case of the other two genes/proteins, that the mechanisms of cell death are linked to severely reduced mitochondrial activity and/or proteosomal and lysosomal malfunctions.
α-Synuclein is an intrinsically disordered protein the physiological function of which is still not known. However, when it aggregates, it forms toxic oligomers and eventually fibrils, which form Lewy bodies that are a hallmark of PD. The formation of these toxic oligomers rather than the fibril formation is likely the reason for neuronal dysfunction and, eventually, neuronal death. The small molecule anle138b, which removes toxic α-synuclein oligomers, rescues neurons from the adverse effects of α-synuclein aggregation (12).
We hypothesized that there is an inverse molecular link between PD and melanoma and that proteins that are “detrimental players” in PD are “beneficial players” in melanoma because their functions confer significant survival benefits to primary and metastatic melanoma. In the present study, we provide experimental evidence, in vitro and in vivo, that α-synuclein functions as a pertinent rheostat for melanoma cell autophagy—a major survival mechanism for primary and metastatic melanoma—and that interfering with this role of α-synuclein has detrimental consequences for advanced melanoma.
Results
Status of α-Synuclein/SNCA, LRRK2/PARK8, and Parkin/PARK2 Expression in Normal Skin, Nevi, and Early and Advanced Melanoma.
It has been reported that α-synuclein is expressed in melanoma (13) and that overexpressing it enhances the proliferation of B16 murine melanoma (14). However, scientific data regarding status and level of expression of the three major PD-related genes/proteins—α-synuclein/SNCA, LRRK2/PARK8, and parkin/PARK2—alongside one another in nevi and in early and advanced melanoma were not available. Therefore, to determine which of these three genes/proteins that are strongly linked to PD are expressed in the different stages of melanoma development and to what extent, we probed the same tissues of a nevus > melanoma progression tissue microarray (TMA) (15) with antibody to the respective protein encoded by the genes SNCA, PARK8, or PARK2.
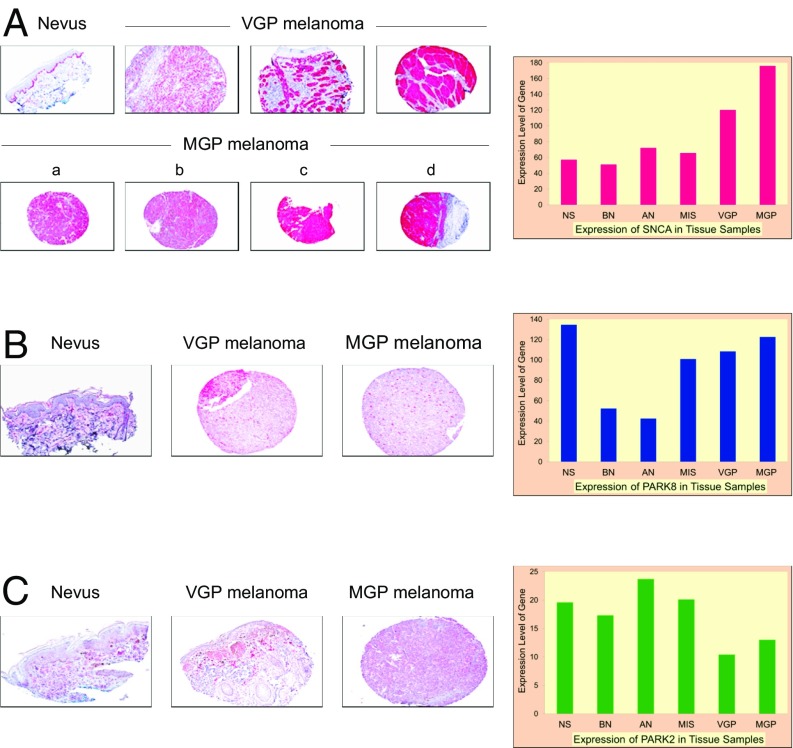
Depicted in Fig. 1A are examples of α-synuclein expression in TMA cores representing a nevus, three primary melanomas in vertical growth phase (VGP) melanoma, and four melanomas in metastatic growth phase (MGP) melanoma obtained from different organ sides. The results of this analysis revealed that α-synuclein was expressed primarily, if not exclusively, in melanoma cells in both VGP and MGP melanoma tissue cores and in nevus tissue cores, it was expressed primarily in melanocytes residing along the epidermal–dermal junction, a finding that is in agreement with previously reported data (13). Because our analysis demonstrated the strongest expression of α-synuclein in TMA cores representing advanced melanoma, we queried the Gene Expression Omnibus (GEO) Dataset GSE4587 from a whole-genome expression profiling study that we had previously conducted (16) for the level of expression of the SNCA gene in tissues ranging from normal skin > MGP melanoma. Our data, obtained upon profiling of nonmicrodissected tissue samples representing normal skin (NS), benign nevi (BN), atypical nevi (AN), melanoma in situ (MIS), and VGP and MGP melanomas, suggest that SNCA is expressed at elevated levels in VGP and MGP melanomas compared with MIS and AN (Fig. 1A, bar graph).
Fig. 1.
Expression of α-synuclein/SNCA, LRRK2/PARK8, and Parkin/PARK2 in normal skin and nevus and melanoma tissues. (A) Images of select normal skin, nevus, and VGP and MGP melanoma TMA cores (a: s.c. metastasis; b: GI metastasis; c: brain metastasis; d: melanoma-infiltrated lymph node) probed with an anti–α-synuclein antibody and counterstained with hematoxylin. Bar graph: Expression of the SNCA gene, determined via previously conducted whole-genome expression profiling in NS, BN, AN, MIS, VGP melanoma, and MGP melanoma. (B) Select images of a nevus, a VGP melanoma, and an MGP melanoma (s.c. metastasis) probed with an antibody to LRRK2 and counterstained with hematoxylin. Bar graph: Expression of the PARK8 (LRRK2) gene, determined via previously conducted whole-genome expression profiling in NS, BN, AN, MIS, VGP melanoma, and MGP melanoma. (C) Select images of a nevus, a VGP melanoma, and an MGP melanoma (s.c. metastasis) probed with an anti-Parkin antibody and counterstained with hematoxylin. Bar graph: Expression of the PARK2 gene, determined via previously conducted whole-genome expression profiling in NS, BN, AN, MIS, VGP melanoma, and MGP melanoma. (A–C, 10× magnification.)
Probing the TMAs with an antibody to LRRK2 (Fig. 1B) showed that, unlike α-synuclein, LRKK2 was not expressed in every melanoma cell in the VGP and MGP melanoma TMA cores and that only a few melanocytes in the nevus TMA cores showed expression of LRRK2 (Fig. 1B). Furthermore, whereas the PARK8 (LRRK2) expression profile (Fig. 1B, bar graph) suggests that expression of the PARK8 (LRRK2) gene is higher in MIS and in VGP and MGP melanomas compared with BN and AN, its level of expression is highest in NS. Regarding Parkin (Fig. 1C), our TMA analysis showed that it is expressed in some melanoma cells, but unlike in the case of α-synuclein, not all of the melanoma TMA cores revealed expression of Parkin, and melanocytes in the nevus tissue cores showed relatively weak expression. Furthermore, our whole-genome expression profiling data (Fig. 1C, bar graph) suggest that expression of the PARK2 gene is lower in VGP and MGP melanomas compared with NS, BN, AN, and MIS.
Level of Expression, Subcellular Localization, and State of α-Synuclein Protein in VGP and MGP Melanoma Cells.
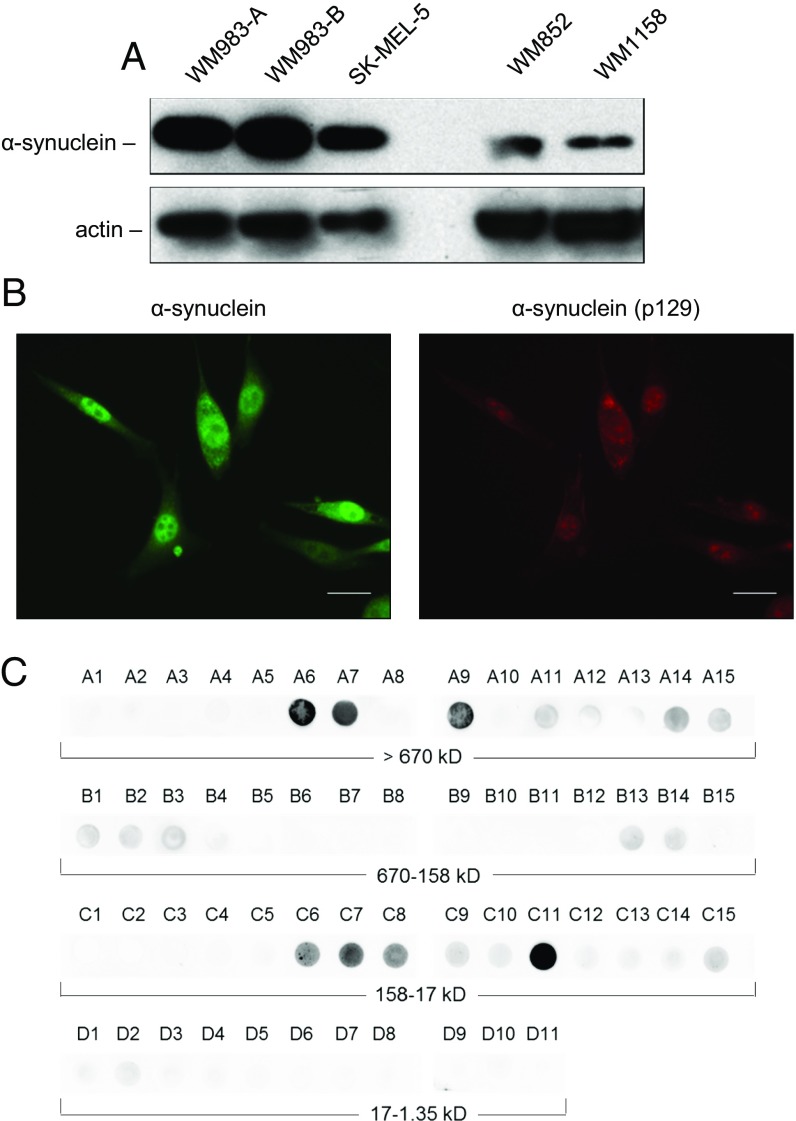
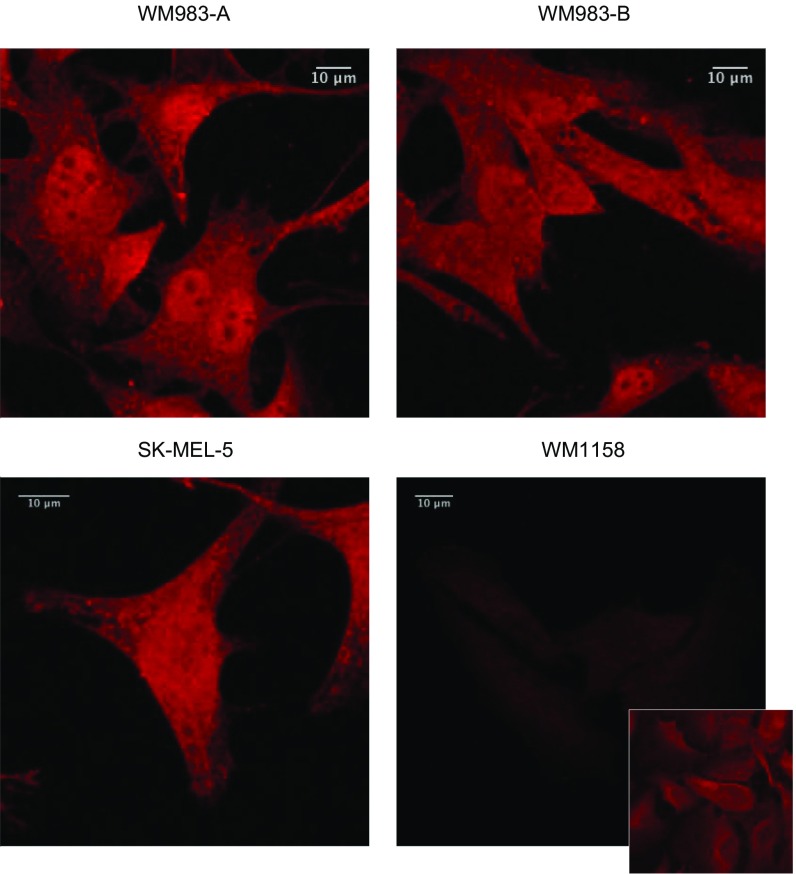
To determine the level of expression and subcellular localization of α-synuclein protein in cell lines derived from tumors representing advanced melanoma, we performed immunoblot analyses of the VGP melanoma cell line WM983-A, the three MGP melanoma cell lines WM983-B, SK-MEL-5, WM852, and the WM1158 melanoma cell line that was established from a superficial spreading melanoma in the radial growth phase (RGP)/VGP. As shown in Fig. 2A, the cell lines WM983-A and WM983-B, which were derived from a VGP and an MGP melanoma of the same patient, and the MGP melanoma cell line SK-MEL-5 express high levels of α-synuclein. In comparison, the WM852 (MGP) and the WM1158 (RGP/VGP) melanoma cell lines contain lower levels of α-synuclein protein (Fig. 2A). To determine the subcellular localization of α-synuclein in these cell lines, we performed immunofluorescence studies with two different antibodies to α-synuclein. Both antibodies detected α-synuclein throughout the nucleus and cytoplasm of the melanoma cell lines WM983-B (Fig. 2B and Fig. S1), WM983-A, and SK-MEL-5 (Fig. S1), and at a low level in WM1158 (Fig. S1).
Fig. 2.
Expression and presence of monomeric as well as oligomeric species of α-synuclein protein in melanoma cells. (A) Immunoblot analysis of α-synuclein expression in the VGP melanoma cell line WM983-A; in the MGP melanoma cell lines WM983-B, SK-MEL-5, and WM852; and in the RGP/VGP melanoma cell line WM1158. Ten micrograms each of whole-cell lysate, prepared from WM983-A, WM983-B, or SK-MEL-5 cells, was loaded per lane. To visualize clearly expression of α-synuclein protein in the low-level α-synuclein–expressing melanoma cell lines WM852 and WM1158, 20 µg each of whole-cell lysate was loaded per lane. Probing with an anti-actin antibody served as loading control. (B) Immunofluorescence analysis of α-synuclein expression in WM983-B melanoma cells probed with antibody to α-synuclein (pseudocolored green) or phosphorylated α-synuclein (pSer129) (pseudocolored red). (Scale bars, 30 μm.) (C) Presence of monomeric as well as α-synuclein oligomeric species in WM983-B melanoma cells detected by SEC–filter trap assay. Collected fractions (A1 > A15, B1 > B15, C1 > C15, D1 > D11) were applied to nitrocellulose membrane and probed with an anti–α-synuclein antibody.
Fig. S1.
Immunofluorescence analysis of expression of α-synuclein protein in melanoma cell lines WM983-A, WM983-B, SK-MEL-5, and WM1158. The background-subtracted and mean-filtered fluorescence images, captured at 63× magnification, of the anti–α-synuclein antibody-probed melanoma cells (pseudocolored red) are maximum intensity projections of 12–16 sections taken at the same laser power and gain settings. The Inset in the image of WM1158 melanoma cells was captured at a 3× higher laser power to make the cellular fluorescence visible.
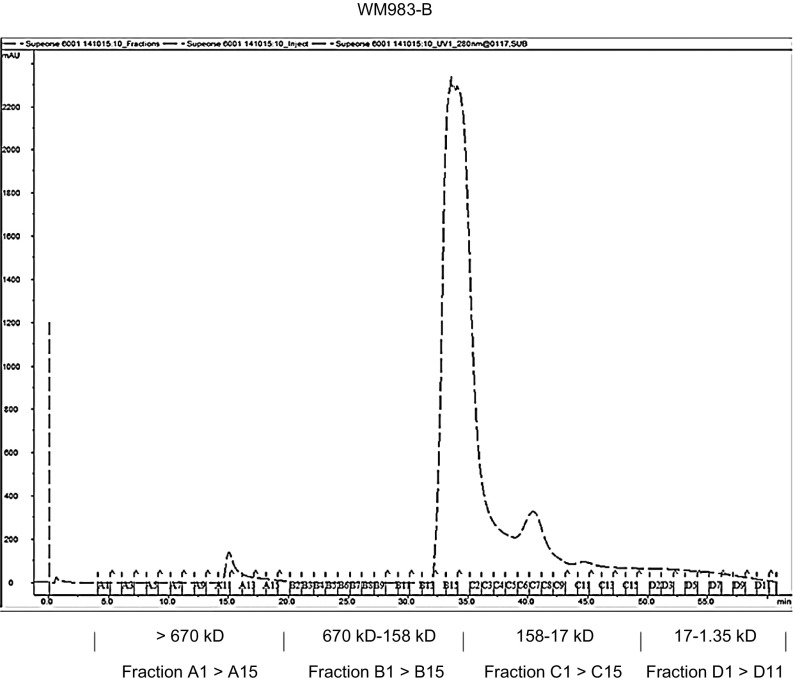
Previously, it was reported that, following phosphorylation at Ser129, α-synuclein is translocated to the cell surface (17) from where, as shown in the case of SK-MEL-5 cells (18), it is released and spreads, possibly by way of melanoma exosomes, to other cells where it is endocytosed. Performing immunofluorescence analysis, we obtained evidence that α-synuclein is phosphorylated at Ser129 in WM983-B melanoma cells (Fig. 2B). In addition, WM983-B melanoma whole-cell lysate, separated by size exclusion chromatography (SEC) (Fig. S2), followed by filter trap–dot blot analysis of the collected fractions with an anti–α-synuclein antibody, showed monomeric α-synuclein as well as its distribution in fractions of higher-molecular-weight species between 17–158 kDa and >670 kDa (Fig. 2C), indicating that in these cells α-synuclein is oligomerized and also likely interacting with other proteins.
Fig. S2.
SEC elution profile of WM983-B melanoma whole-cell lysate. Chromatogram of WM983-B melanoma whole-cell lysate separated by SEC. A total of 56 fractions were collected. Molecular weight sizes for the fractions were assessed using a gel filtration standard (bovine thyroglobulin: 670 kDa; bovine y-globulin: 158 kDa; chicken albumin: 44 kDa; horse myoglobin-17: kDa; vitamin B12: 1.35 kDa).
Treatment of Melanoma Cells Expressing High Levels of α-Synuclein with Oligomer Modulators Affecting α-Synuclein Causes Overt Changes in Melanoma Cell Morphology and Inhibits Melanoma Cell Proliferation.
To gain insights into the possible function(s) of the α-synuclein protein in advanced melanoma, we treated the melanoma cell lines WM983-A, WM983-B, SK-MEL-5, WM852, and WM1158 with a panel of diphenyl–pyrazole (DPP) compounds. The DPP scaffold, identified from the small-molecule DIVERSet libraries (Chem-Bridge) by way of inhibition of prion protein aggregation followed by medicinal chemistry optimization of DPP compounds, led to the identification of anle138b and anle138c (12). Neither of these two compounds binds to α-synuclein monomers (19), but they both reduce the formation of toxic oligomers and therefore also, indirectly, fibrils. Furthermore, in the A30P α-synuclein transgenic mouse model, anle138b removed toxic oligomers and fibrils forming from these oligomers and improved locomotion performance; and in a spreading model of PD, anle138b reduced the spreading and improved locomotion performance (12).
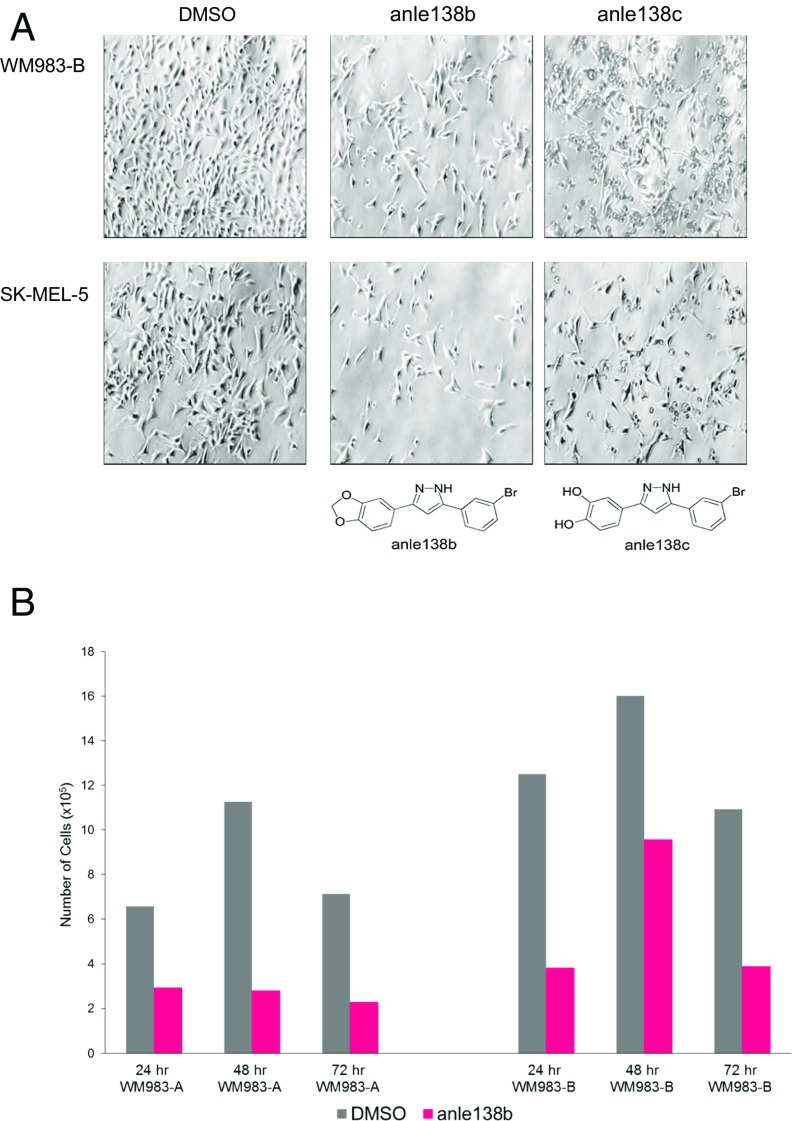
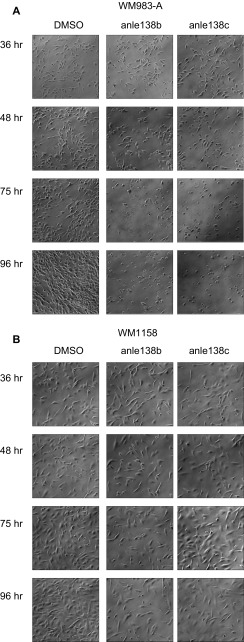
From an initial screen of 16 compounds from the DPP library, we found that anle138b and anle138c significantly affected the high-level α-synuclein–expressing cell lines WM983-A, WM983-B, and SK-MEL-5. To assess the possible impact of anle138b as well as anle138c on the different melanoma cell lines, we treated them with increasing doses of either compound, dissolved in dimethyl sulfoxide (DMSO), and added to serum-free culture medium. The two melanoma cell lines WM983-B and SK-MEL-5, expressing high levels of α-synuclein, demonstrated, time- and dose-dependently, major morphological changes manifested first by the formation of cell clusters, followed by increasing detachment from the surface of the tissue culture dish. Fig. 3A shows representative images of WM983-B and SK-MEL-5 melanoma cells treated for 48 h with a single dose of 10 µM of either anle138b or anle138c. We also observed that treatment with anle138b caused a more rapid morphological change than anle138c. To determine whether the effect of the two anle compounds was related to the amount of α-synuclein produced by the cells, we compared the proliferation of the (VGP) WM983-A high-level (Fig. S3A) and the (RGP/VGP) WM1158 low-level α-synuclein–producing melanoma cells over a period of 96 h with replenishment of each anle compound at 48 h (Fig. S3B). The morphological changes in the WM983-A and WM1158 cells lines did not occur as rapidly as in the case of the MGP melanoma cell lines WM983-B and SK-MEL-5. However, residual WM983-A cells, which remained attached to the tissue culture dish at 96 h, were not able to proliferate again after removal of the anle138b-containing culture medium, followed by rinsing three times with fresh medium and subsequent incubation in serum-free medium. In contrast, the WM1158 cells did not show a significantly altered morphology from the treatment with anle138b or anle138c, showed reduced proliferation only after 48 h, and were able to recover proliferation normally following removal of anle138b at 96 h and addition of fresh culture medium containing serum.
Fig. 3.
Treatment of melanoma cells with the α-synuclein oligomer modulators anle138b or anle138c changes the morphology of the cells and inhibits their proliferation. (A) Phase-contrast images, captured at 10× magnification, showing the morphology of WM983-B and SK-MEL-5 melanoma cells that for 48 h had received DMSO only or were treated for 48 h with a single dose (10 µM) of anle138b or anle138c. (B) Proliferation of WM983-A and WM983-B melanoma cells that had received DMSO only or were treated with 10 µM of anle138b for 24, 48, or 72 h with replenishment of 10 µM of the compound at 48 h. Shown for each time point and cell line is the mean of triplicate samples analyzed (n = 1).
Fig. S3.
Morphology of WM983-A (VGP) and WM1158 (RGP/VGP) melanoma cells treated with anle138b or anle138c. Phase-contrast images, captured at 10× magnification, showing the morphology of WM983-A (A) and WM1158 (B) melanoma cells that had received DMSO only or had been treated with a single dose (10 µM) of anle138b or anle138c for 36, 48, 75, or 96 h with replenishment of an equivalent dose of each compound or DMSO only at 48 h.
Because the morphological changes in the high-level α-synuclein–expressing melanoma cells occurred more rapidly following addition of anle138b than of anle138c, we performed the subsequent studies, presented below, primarily with anle138b, which has no antioxidative effects and does not impair the expression or degradation of α-synuclein (12), and, unlike anle138c, has excellent oral bioavailability and penetration of the blood–brain barrier (12).
To compare how rapidly anle138b affected the proliferation of melanoma cells, expressing α-synuclein at a high level, we treated the melanoma cell lines WM983-A (VGP) and WM983-B (MGP) for 24, 48, or 72 h with 10 μM of anle138b with replenishment of the compound (10 μM) at 48 h. As shown in Fig. 3B, in as little as 24 h, a single dose of 10 μM of anle138b inhibited the proliferation of both cell lines to a significant extent.
Anle138b Treatment of Melanoma Cells Damages Their Plasma Membrane, Disrupts Their Mitochondrial Membrane Potential, and Dysregulates Autophagy.
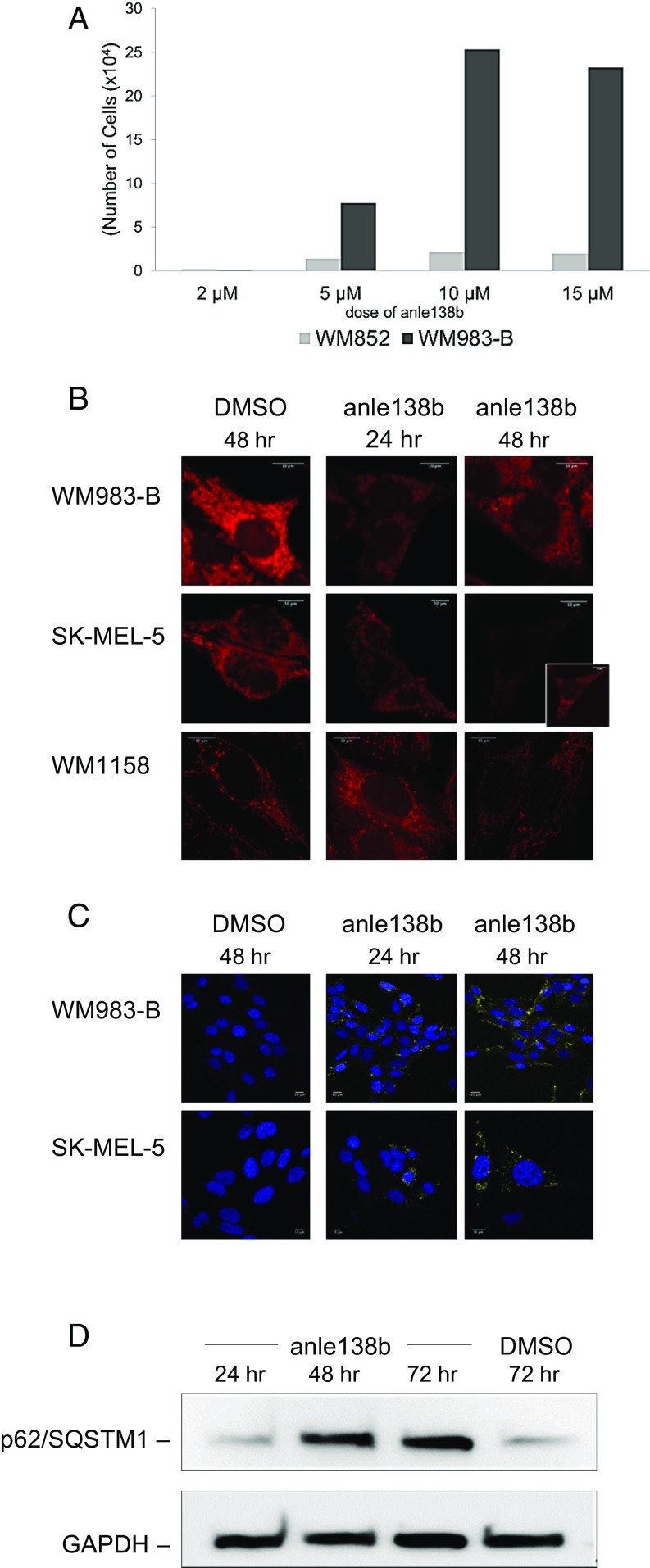
To determine the effect of increasing doses of anle138b on melanoma cell viability and whether it is cytotoxic to the cells and thus compromises their plasma membrane integrity, we performed a lactate dehydrogenase (LDH) cytotoxicity assay of culture supernatants collected from WM983-B and WM852 melanoma cells that were treated for 96 h with increasing doses of anle138b with replenishment of an equivalent dose of the compound at 48 h. As shown in Fig. 4A, the high-level α-synuclein–expressing WM983-B cells showed strong killing that reached a maximum at a 10 μM dose of anle138b, possibly due to its low solubility above this dose in serum-free medium. In comparison, the number of cells killed in response to anle138b treatment was significantly lower in the case of the low-level α-synuclein–expressing WM852 cells (Fig. 4A).
Fig. 4.
Treatment of melanoma cells with the α-synuclein oligomer modulator anle138b leads to melanoma cell killing due to plasma membrane damage, mitochondrial dysfunction, and dysregulation of melanoma cell autophagy. (A) LDH release-based quantitation of anle138b treatment-induced cell killing of WM852 and WM983-B melanoma cells that were treated with 2, 5, 10, or 15 µM of the oligomer modulator for 96 h with replenishment of each equivalent dose at 48 h. Shown for each dose and cell line is the mean of four replicates analyzed (n = 1). (B) Maximum intensity projections of confocal image stacks of MitoTracker dye-stained WM983-B, SK-MEL-5, and WM1158 melanoma cells (pseudocolored red) that for 48 h had received DMSO only or were treated for 24 h or 48 h with a single 10-μM dose of anle138b. Inset in the image of SK-MEL-5 melanoma cells, treated for 48 h with anle138b, was captured at 5× higher laser power to make the fluorescence visible. (C) Confocal immunofluorescence image analysis of LC3 expression in WM983-B and SK-MEL-5 melanoma cells that for 48 h had received DMSO only or were treated with a single dose (10 μM) of anle138b for 24 h or 48 h. The anti-LC3B antibody-probed melanoma cells (pseudocolored yellow) were counterstained with fluorescent DRAQ5 (pseudocolored blue). (D) Immunoblot analysis of p62/SQSTM1 expression in WM983-B melanoma cells that were treated with anle138b (7.5 μM) for 24, 48, or 72 h with replenishment of an equivalent dose at 48 h. WM983-B melanoma cells that for 72 h, with replenishment at 48 h, had received DMSO only, served as the control. The immunoblot was probed with an anti-GAPDH antibody for loading control. (B and C, 63× magnification.)
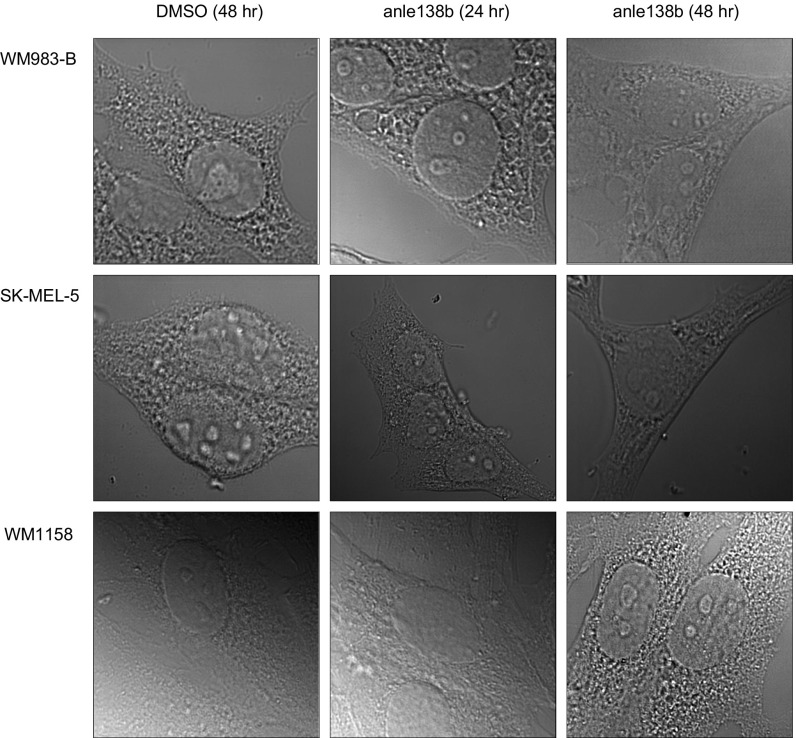
Although following addition of anle138b, the morphological changes in the WM983-A, WM983-B, and SK-MEL-5 melanoma cell lines occurred quite rapidly, they were not indicative of the cells undergoing apoptosis. This observation was supported by the fact that neither the anle138b- nor the anle138c-treated cells exhibited abnormal condensation and fragmentation of chromatin, nor were they positive for cleaved caspase 3. However, as shown in Fig. 4B, the mitochondrial membrane potential of WM983-B and SK-MEL-5 melanoma cells was significantly reduced as early as 24 h following addition of a single 10-μM dose of anle138b, whereas the low-level α-synuclein–expressing WM1158 cells started to show some reduction in mitochondrial membrane potential only after 48 h of anle138b treatment. Differential interference contrast (DIC) images of the morphology of the anle138b-treated WM983-B, SK-MEL-5, and WM1158 melanoma cells from the same panels appear in Fig. 4B are shown in Fig. S4.
Fig. S4.
DIC images of the MitoTracker dye-stained WM983-B, SK-MEL-5, and WM1158 melanoma cells treated with anle138b (10× magnification). DIC images showing the morphology of the MitoTracker dye-stained WM983-B, SK-MEL-5, and WM1158 melanoma cells that for 48 h had received DMSO only or were treated for 24 h or 48 h with a single dose (10 μM) of anle138b.
We observed a clear effect of the anle compounds on the autophagy pathway of the melanoma cells. WM983-B cells, treated with anle138b, demonstrated prominent punctate up-regulation of the autophagosome marker, the microtubule-associated protein 1 light chain 3B (LC3), in about 60% of the cells still attached at 24 h and in 95% of the cells remaining on the cell culture dish at 48 h, whereas WM983-B cells that had received DMSO only showed less than 1% cells with LC3 puncta at 96 h (Fig. 4C). Following addition of anle138c, the effect was seen later with levels of 8% at 24 h and 78% after 96 h. Similar levels of punctate LC3 loci were also observed for the SK-MEL-5 melanoma cells upon treatment with anle138b (Fig. 4C) and even higher levels were observed with anle138c.
To determine how soon following the addition of anle138b to high-level α-synuclein–expressing melanoma cells autophagy was dysregulated, and whether a dose below 10 μM of anle138b would suffice, we treated WM983-B melanoma cells with 7.5 μM of anle138b for 24, 48, or 72 h with replenishment of an equivalent dose of the compound at 48 h. Probing WM983-B melanoma whole-cell lysates with an antibody to the protein, p62/SQSTM1, which is required for the aggregation of ubiquitinylated proteins and their clearance via autophagy, showed that anle138b treatment for 24 h did not lead to an increase in p62/SQSTM1 expression (Fig. 4D). However, after 48 h and 72 h of anle138b treatment (Fig. 4D), the level of expression of this autophagy cargo adaptor protein was notably elevated compared with WM983-B cells that had received DMSO only (Fig. 4D).
Anle138b Administered Systemically to Nude Mice Bearing High-Level α-Synuclein–Expressing Human Melanoma Xenografts Reaches the Tumors and Affects Their Morphology and Autophagy.
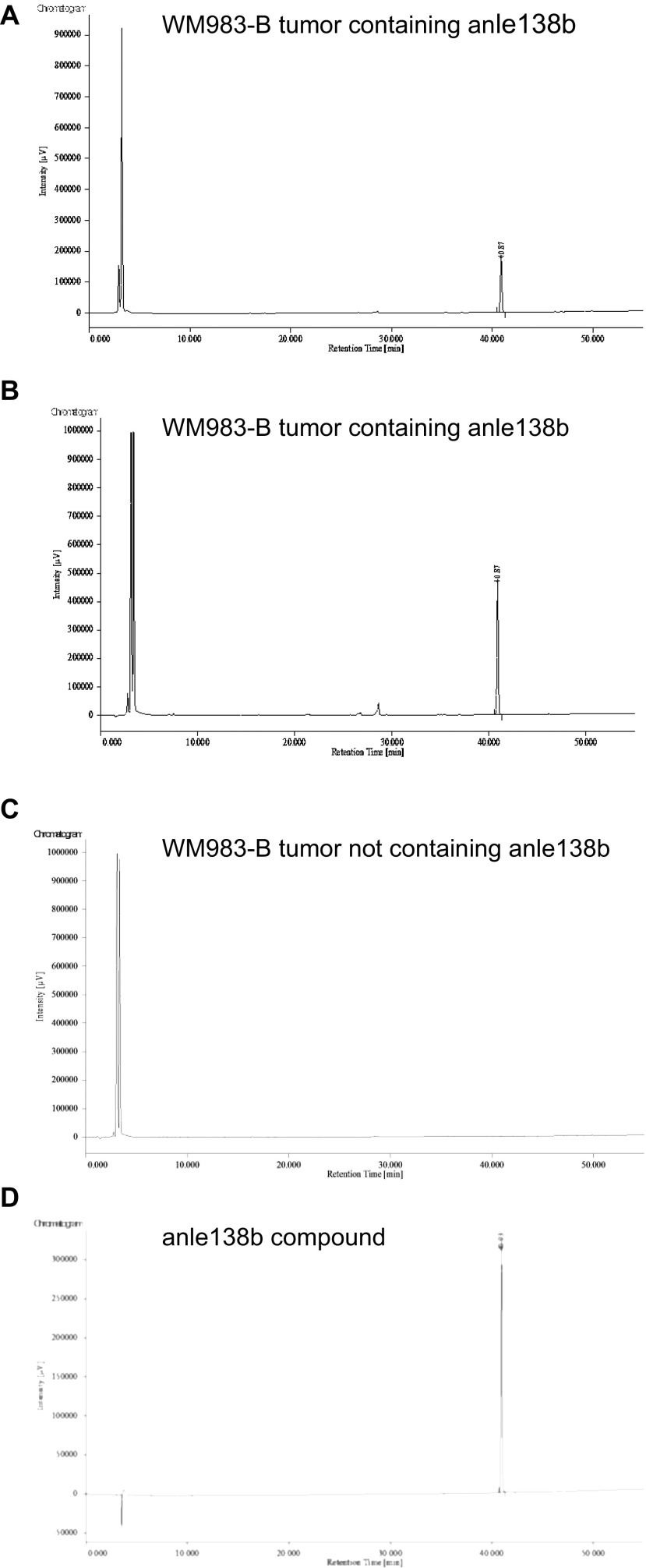
To determine whether the DPP compound, anle138b, when administered systemically to human MGP melanoma cells grown as s.c. tumors in nude mice, would reach the tumors, we performed the following study. A nude mouse, bearing high-level α-synuclein–expressing (MGP) WM983-B human melanoma xenografts on its lower right and lower left dorsal side, received food pellets mixed with anle138b for 7 d. A second nude mouse, also bearing WM983-B tumors on its lower right and lower left dorsal side, received the same type of food pellets not containing anle138b for 7 d. After the mice were killed, we performed the following analyses on the postmortem resected and thereafter cryopreserved tumors.
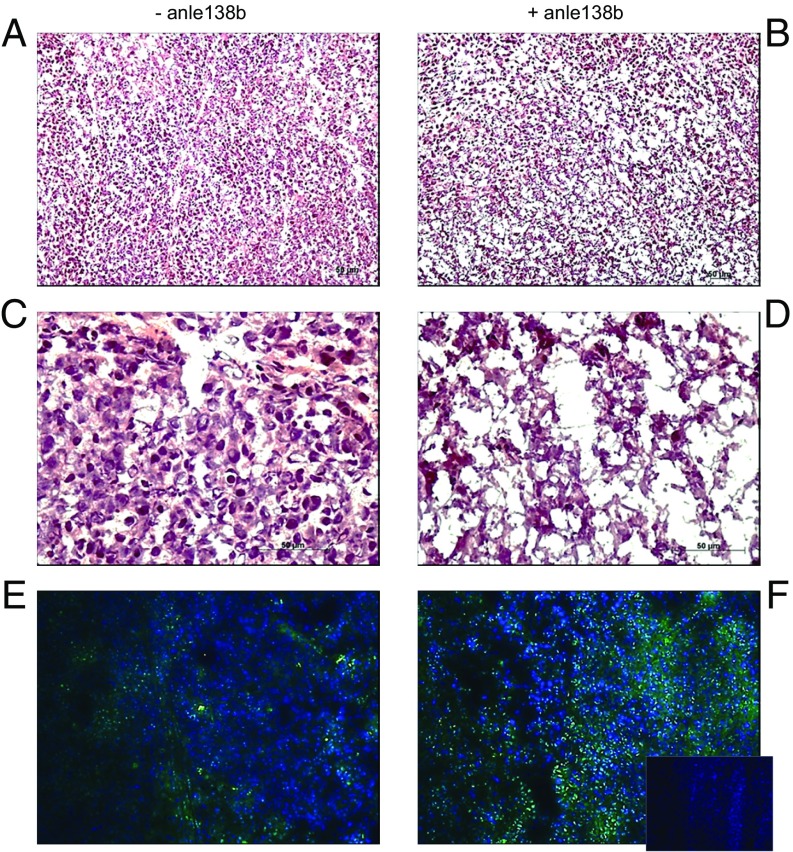
First, the results of our pharmacokinetic (PK) analysis of the resected tumors showed that anle138b was present at a level of 125 μM in the tumor (weight of tumor: 57 mg) resected from the right dorsal side (Fig. S5A) and at a level of 110 μM in the tumor (weight of tumor: 218 mg) resected from the left dorsal side (Fig. S5B) of the WM983-B human melanoma xenograft-bearing animal that had received food pellets mixed with anle138b. In contrast, anle138b was not detected in a tumor resected from the WM983-B human melanoma xenograft-bearing mouse that had received food pellets without anle138b (Fig. S5C). Second, hematoxylin and eosin (H&E) staining of tissue sections, prepared from one of the WM983-B human melanoma xenografts that had been resected from the animal that had received the food pellets mixed with anle138b (Fig. 5 B and D), showed that the morphology of these tumor cells, arranged in a scattered pattern with focally pronounced disturbances in the tissue’s architecture, differed from the morphology of the tumor cells in a WM983-B control tumor that did not contain anle138b (Fig. 5 A and C). Third, probed with anti-LC3 antibody, tissue sections from a WM983-B human melanoma xenograft, resected from the animal that had received anle138b-containing food pellets, showed more LC3-positive cells (Fig. 5F) compared with anti-LC3 antibody-probed tissue sections prepared from one of the WM983-B human melanoma xenograft control tumors that did not contain anle138b (Fig. 5E).
Fig. S5.
Analytical HPLC of high-level α-synuclein–expressing WM983-B human melanoma xenografts resected from a nude mouse that had received food pellets mixed with anle138b and from a nude mouse that had received food pellets not containing anle138b. (A and B) Chromatograms showing the presence of anle138b in the two tumors resected from the animal that received food pellets mixed with anle138b. (C) Chromatogram of one the tumors resected from the animal that had received food pellets not containing anle138b. (D) Chromatogram of the anle138b DPP compound (reference sample).
Fig. 5.
Systemic administration of anle138b to high-level α-synuclein–expressing human melanoma xenografts affects the xenografts’ morphology and autophagy. (A–D) H&E-stained tissue sections, prepared from one of the WM983-B human melanoma xenografts that had received food pellets not containing anle138b (A and C) and from one of the WM983-B human melanoma xenografts that had been resected from the animal that had received food pellets mixed with anle138b (B and D). The photographs shown in A and B were taken at 100× magnification, and in C and D at 40× magnification. (E and F) LC3 immunohistochemical staining of a tissue section (F, Inset, 100× magnification), prepared from one of the WM983-B human melanoma xenografts that had been resected from the animal that had received food pellets not containing anle138b (E) and from one of the WM983-B human melanoma xenografts that had been resected from the animal that had received food pellets mixed with anle138b (F). The anti-LC3B antibody-probed WM983-B human melanoma xenograft tissue sections (pseudocolored green) were counterstained with fluorescent DAPI (pseudocolored blue). The Inset in F shows a tissue section from the anle138b-containing WM983-B tumor, probed with Alexa-488 secondary antibody only and counterstained with fluorescent DAPI (pseudocolored blue).
Discussion
Little if any information is yet available regarding the underlying mechanisms that are the reason for the epidemiological link between PD, which affects an estimated 7–10 million people worldwide, and advanced melanoma, the most aggressive type of skin cancer that accounts for 75% of all skin-cancer–related deaths. Because it had been ruled out that genetic factors link these two diseases, we explored the possibility that the association could be α-synuclein, LRRK2, or Parkin, which are the key regulators of PD.
We provide tissue-based evidence that, unlike LRRK2 and Parkin, it is α-synuclein that is expressed almost exclusively in melanoma cells. Interestingly, the GEO profiles of the NCI-60 cancer cell line panel also show that, compared with cell lines derived from cancer tissue from nine different origin types (breast, central nervous system, colon, leukemia, melanoma, non-small cell lung, ovarian, prostate, and renal), malignant melanoma cell lines overall have the highest level of SNCA expression [National Center for Biotechnology Information (NCBI) GEO Dataset Browser GDS 4296(ACCN)snca]. Likewise, information available in the Human Protein Atlas (www.proteinatlas.org) shows strong expression of α-synuclein in advanced melanoma compared with other malignancies, including other types of skin cancer.
Mutations in the SNCA gene are rare whereas mutations in the PARK8 gene, which encodes the 2,527-aa multidomain LRRK2 protein, are the most common cause of autosomal dominant PD. The data of our nevus > advanced melanoma TMA analysis showed that LRRK2 is expressed at various levels in some but not in all nevocytes and melanoma cells. Furthermore, in some of the VGP and MGP melanoma TMA cores, we also detected LRRK2 expression in cells interspersing the tumor cells. Mutations in the PARK2 gene, which encodes the E3-ubiquitin ligase Parkin, are the most frequent genetic cause of autosomal recessive juvenile PD. As in the case of α-synuclein, our TMA analysis showed that Parkin is expressed in melanoma cells. However, compared with α-synuclein, the level of Parkin expression in the VGP and MGP melanoma TMA cores was significantly lower, and not all of the melanoma TMA cores showed expression of Parkin, which supports the suggestion that in melanoma PARK2 is a tumor suppressor (20). Two other genes, which have been linked to PD, are DJ-1 and ATP13A2. We did not determine the status of expression of DJ-1 in tissues ranging from nevi > advanced melanoma, but a histopathological study has shown that, in cutaneous melanoma, cytoplasmic expression of DJ-1 is decreased (21), whereas in the serum of patients with metastatic uveal melanoma it is elevated (22, 23). To date, it is not known whether ATP13A2 plays a role in melanoma, but in light of its putative interplay with α-synuclein (24), it is noteworthy that the ATP13A2-specific dataset from our previously conducted whole-genome expression profiling study indicates that, as in the case of SNCA, the ATP13A2 gene is up-regulated with progression from nevi > melanoma.
Gaining important insights into pivotal prosurvival mechanisms and pathways for advanced melanoma constitutes one of the essential tasks to finding effective therapies for patients with this disease. The important finding presented here is that treatment of high-level α-synuclein–expressing VGP and MGP melanoma cells with the α-synuclein and prion protein oligomer modulator anle138b or anle138c leads to rapid melanoma cell death due to plasma membrane damage, a severe reduction in mitochondrial membrane potential, and a major dysregulation of autophagy. Furthermore, with a view toward potential future clinical applications for advanced melanoma, in the setting of a preclinical human melanoma xenograft study we provide evidence that systemically administered anle138b not only reaches the tumor, but also is present at high levels in the tumor cells and that it affects their morphology and autophagy.
Our finding that treatment of high-level α-synuclein–expressing melanoma cells with anle138b leads to dysregulation of melanoma cell autophagy vis-à-vis the finding that, in a mouse model of tauopathies, anle138b treatment did not change the level of the autophagy markers LC3 and p62/SQSTM1 (25) suggests that the biological consequence(s) of treatment with anle138b is cell-type–specific. This specificity may be linked to the deleterious effects that α-synuclein has on neurons in a synucleinopathy such as PD, whereas in an aggressive malignancy such as advanced melanoma, high-level expression of α-synuclein not only is beneficial to cell survival, but also possibly promotes, likely by way of spreading via melanoma exosomes (18), the formation and growth of melanoma brain metastases to which this disease is particularly prone.
By now, it is well established that in normal cells autophagy has a protective role whereas in cancer it has a dual role—as a suppressor in the early stages of cancer development and as a facilitator/promoter in the advanced stages (26–29). Thus far, little is known about to what extent autophagy plays a role in nevus > melanoma progression and in melanoma in its early versus advanced stages. However, it has been reported that RGP, VGP, and in particular MGP melanomas express significantly lower levels of LC3 than nevi (30) and that median p62/SQSTM1 expression levels are lower in American Joint Committee on Cancer (AJCC) stage III/IV than in AJCC stage I/II melanomas (31). This is in concordance with our finding that the two MGP melanoma cell lines, WM983-B and SK-MEL-5, that had received DMSO only, showed an LC3-positive phagosome signal in less than 1% of the cells and that the level of p62/SQSTM1 expression in the DMSO-treated WM983-B cells was low. On the other hand, recent and increasing evidence, obtained primarily in the context of melanoma–BRAF inhibitor resistance studies, suggests that autophagy is a pertinent survival mechanism for advanced melanoma (32–36).
In summary, our findings presented here provide evidence that α-synuclein, which in PD exerts severe toxic functions, promotes and thereby is highly beneficial to the survival of melanoma in its advanced stages. In addition, our data suggest that dysregulating autophagy in VGP and MGP melanoma cells by way of interfering with the aggregation of α-synuclein might be a powerful approach to a triple combination therapy encompassing an anle138b-like compound, a small-molecule inhibitor targeting a key regulator of advanced melanoma, and deployment of a potent immunostimulatory antibody.
Materials and Methods
A more complete description is available in SI Materials and Methods.
Melanoma Cell Lines, TMAs, and GEO Datasets.
The human melanoma cell lines WM983-A, WM983-B, WM852, and WM1158 were propagated in vitro as described (37). The human melanoma cell line SK-MEL-5 (CLS Cell Lines Service) was propagated in Eagle’s Minimum Essential Medium supplemented with nonessential amino acids, sodium pyruvate, and 10% FBS.
Following antigen retrieval and prior staining of test TMAs to determine the optimal dilution (signal-to-noise performance) for each antibody, tissue cores of a nevus > melanoma progression TMA (15) were probed by standard immunohistochemistry with antibody to α-synuclein (MJFR1), LRRK2 (MJFF2), or Parkin (Abcam), followed by scanning of the TMA slides with an Aperio ScanScope (Leica Microsystems) to generate digital images of the antibody-probed tissue cores. For information regarding the GEO datasets, see SI Materials and Methods.
SEC–Filter Trap Assay.
WM983-B melanoma cells were lysed in PBS containing 0.5% Triton X-100 and protease inhibitors. The protein lysate (2.2 mg/0.5 mL) was filtered through a 0.45-μm centrifuge tube filter before loading onto a Superose 6 10/300GL column (GE Healthcare Bio-Sciences) connected to an ÄKTApurifier 10 (GE Healthcare Life Sciences). The collected fractions were placed for 10 min in a 95 °C water bath, and thereafter the entire volume of every collected fraction was loaded onto nitrocellulose membranes by way of a dot-blot vacuum system. After blocking in Tris-buffered saline-Tween 20 containing 5% nonfat dry milk, the membranes were probed with a mouse monoclonal anti–α-synuclein (Syn-1) antibody (BD Biosciences), followed by incubation with a corresponding HRP-conjugated secondary antibody and chemiluminescent substrate (EMD Millipore). The SEC–filter trap assay was repeated twice.
Melanoma Xenograft Study.
Four-week-old female nude mice (CAnN.Cg-Foxn1nu/Crl) (Charles River Laboratories) were injected subcutaneously on their lower right and lower left dorsal side with WM983-B (MGP) human melanoma cells (1 × 107 cells per side). When the tumors had reached a size of 2.3–3.0 mm in any direction, the normal food pellet diet of one of the animals was replaced with food pellets mixed with anle138b (2 g of anle138b/kg of food pellets) (ssniff Spezialdiäten GmbH), and the normal food pellet diet of the other animal was replaced with food pellets (ssniff Spezialdiäten GmbH) not containing anle138b. Both tumor-bearing animals were killed 7 d after having received the food pellets with or without anle138b, and the resected tumors were immediately frozen in liquid nitrogen. These studies were carried out under approved Niedersächsisches Landesamt für Verbraucherschutz und Lebensmittelsicherheit (LAVES) protocol (33.19–42502-04–14/1724). Analyses of the tumors were performed as described in SI Materials and Methods.
SI Materials and Methods
Melanoma Cell Lines, TMAs, GEO Datasets.
From the datasets of our whole-genome expression profiling study (16) that we had previously deposited in the NCBI GEO database (dataset GSE4587), we sourced the expression level of SNCA from the mean of the values listed for NS (n = 2), AN (n = 2), MIS (n = 2), VGP melanoma (n = 2), MGP melanoma (n = 5) under profile GDS1989/236081, PARK8 (LRRK2) under profile GDS1989/229584, and PARK2 under profile GDS1989/207058.
Immunoblot Analysis.
For the analysis of α-synuclein protein expression, whole-cell lysates were separated on 12% SDS/PAGE, transferred onto PVDF membrane, cross-linked by a 30-min treatment at room temperature with 0.4% paraformaldehyde (PFA) in PBS, blocked with 5% powdered milk, probed with antibody against α-synuclein (MJFR1) (Abcam), followed by incubation with an HPR-conjugated secondary antibody and SuperSignal West Pico chemiluminescent substrate (Thermo Fisher Scientific). Protein loading was determined by secondary probing with an anti-actin (ab1801) antibody (Abcam).
For the analysis of p62/SQSTM1 protein expression, WM983-B melanoma whole-cell lysates were separated on 12% SDS/PAGE, transferred onto nitrocellulose membrane, blocked with 3% BSA, probed with an anti-p62/SQSTM1 antibody (Cell Signaling Technology), followed by incubation with a corresponding HPR-conjugated secondary antibody and chemiluminescent substrate (EMD Millipore). Protein loading was determined by secondary probing with an anti-GAPDH antibody (Thermo Fisher Scientific).
Anle138b and Anle138c Inhibitor Treatment and Melanoma Cell Proliferation Analysis.
Ten- or 30-mM stock solutions of anle138b or anle138c were made in DMSO. Because anle138b and anle138c bind strongly to FBS, melanoma cells, plated for 24 h in tissue-culture medium containing 10% FBS, were rinsed three times with serum-free medium before addition of anle138b, anle138c, or an equivalent volume of DMSO only in serum-free medium. Forty-eight hours later, the cell culture medium was removed, followed by addition of an equivalent dose of anle138b or anle138c or DMSO only in serum-free culture medium. Because the (RGP/VGP) WM1158 melanoma cells do not proliferate well in serum-free culture medium, 20 ng/mL of recombinant human basic fibroblast growth factor was added to the serum-free culture medium during treatment of these cells with anle138b or anle138c. Proliferation of melanoma cells that had received DMSO only or were treated with anle138b was determined by counting the cells with a hemocytometer.
LDH Cytotoxicity Analysis.
Replicates of WM983-B as well as WM852 melanoma cells were plated at 3 × 105 cells per well in 35-mm tissue culture plates. Twenty-four hours later, the cells were rinsed three times with serum-free medium, followed by addition of increasing doses of anle138b or DMSO only. Forty-eight hours later, the cell culture medium was removed, followed by addition of equivalent doses of anle138b or DMSO only in serum-free medium. Culture medium, collected 48 h later, was centrifuged to pellet and remove cellular debris. Using a PHERAstar FS microplate reader (BMG LABTECH) and spectrophotometric absorbance measurement, the release of LDH enzyme activity into the tissue culture medium was determined with an LDH cytotoxicity assay kit (Roche Diagnostics). Serum-free culture medium supernatants from the WM983-B and WM852 melanoma cells that had received DMSO only served as background controls and their values were subtracted. Cells from the DMSO controls were trypsinized, counted, and lysed according to the manufacturer’s instructions. The number of melanoma cells killed was obtained by normalizing LDH release, recorded for each dose of anle138b, to the LDH released upon lysis of a known number of melanoma cells (calibration curve). Standard curves for both cell lines were superimposable.
Cytology and Immunofluorescence.
Cell morphology.
Phase-contrast or DIC images of the melanoma cells that had been treated for various times with anle138b or anle138c or had received DMSO only were captured with a 10× N.A. 0.6 objective on a Zeiss Axiovert 100 microscope with a Hamamatsu Orca charge-coupled device camera. At least four images, at random areas per culture dish, were recorded for each time point.
Mitochondrial membrane potential.
Melanoma cell lines WM983-B, SK-MEL-5, and WM1158 were treated with anle138b or received DMSO only for 24 h or 48 h. Before fixation with 3.7% PFA, the cells were incubated with 200 nM MitoTracker Red CMXRos (Thermo Fisher Scientific) for 30 min at 37 °C. Confocal image stacks were captured with a 63× N.A. 1.2 Apochromat water immersion lens on a Zeiss LSM 510 Meta confocal microscope in fluorescence and transmission modes.
α-Synuclein staining.
WM983-B melanoma cells, fixed with 4% PFA and blocked for 30 min at 37 °C with 5 mg/mL of BSA in 0.05% Triton-X 100/PBS, were probed with a rabbit polyclonal anti–α-synuclein (C-20) antibody (Santa Cruz Biotechnology) or a mouse monoclonal antiphosphorylated α-synuclein (pSyn#64) antibody (Wako Chemicals) and imaged with a 40×/0.60 objective on a Leica DMI6000B inverted microscope. Immunofluorescence comparison of α-synuclein protein expression in the melanoma cell lines WM983-A, WM983-B, SK-MEL-5, and WM1158 was made by fixation of proliferating cells in 3.7% PFA for 20 min and permeabilization and staining with a mouse monoclonal anti–α-synuclein (Syn211) antibody (EMD-Millipore), followed by a goat anti-mouse Alexa-546 secondary antibody. Confocal image stacks were acquired with a 63× N.A. 1.4 oil immersion objective on a Zeiss LSM 510 Meta confocal microscope at the same gain and laser powers.
Autophagy.
WM983-B and SK-MEL-5 cells that for 24 h or 48 h were treated with anle138b or had received DMSO only were fixed for 20 min with 3.7% PFA, permeabilized, and probed with an anti-LC3B (clone 2G6) antibody (nanoTools Antikörpertechnik), followed by a donkey anti-mouse Alexa-488 secondary antibody and Draq5 DNA counterstain. Confocal image stacks were obtained with a 63× N.A. 1.2 objective on a Zeiss LSM 510 Meta confocal microscope.
Melanoma Xenograft Study.
Cryopreserved WM983-B human melanoma xenograft tissues were brought to 4 °C before their transfer into Precellys CKMix 2-mL tissue homogenizing tubes and homogenization in 0.5–1.00 mL acetonitrile using a Precellys Evolution Super homogenizer (Bertin Instruments). Homogenization (6,800 × g, eight cycles for 30 s with a 30-s pause between cycles) was repeated four times. Thereafter, the homogenate was ultrasonicated for 2 min at 25 °C and centrifuged for 2 min. A 100-μL aliquot of the supernatant was injected into an HPLC system. Analytical HPLC was performed using a Waters HPLC system with a Waters 996 Photodiode Array Detector. All separations involved a mobile phase of 0.1% trifluoroacetic acid (TFA) (vol/vol) in water (solvent A) and 0.1% TFA in acetonitrile (solvent B). HPLC was performed using reversed-phase (RP) column Eurospher RP 18, 100 Å, 5 μm, 250 × 4.6 mm at flow rates of 1 mL/min with a gradient of solvent B from 0 to 100% in 50 min. The effluent was monitored for UV absorption at 260 nm. Samples were quantitated using peak area ratio of compounds to external standard.
Tissue sections, prepared from the WM983-B human melanoma xenografts, were fixed with methanol, treated with blocking solution (goat serum: 0.25% Triton X-100), and probed with an anti-LC3 (NB100-2220) antibody (Bio-Techne), followed by addition of a goat anti-rabbit Alexa-488 secondary antibody, counterstaining with fluorescent DAPI, and fluorescent mounting medium (Dako). Images of the anti-LC3 antibody-probed and counterstained tissue sections were obtained with a 10× N.A. 0.45 objective on a Zeiss AXIO Imager M1 epifluorescence and brightfield microscope. H&E staining was performed according to standard protocols.
Acknowledgments
We thank Dr. Thomas M. Jovin for his suggestion to test the anle compounds on the melanoma cell lines; Dr. Sigrid Broekaert for assistance with the histopathological analysis; and Anette Bennemann and Dr. Verena Lorenz for technical assistance with the immunohistochemistry and imaging of the human melanoma xenograft tissue sections. This work was supported by funds from the Deutsche Forschungsgemeinschaft; Cluster of Excellence, Center for Nanoscale Microscopy and Molecular Physiology of the Brain (T.F.O.); and the Max Planck Society (C.G. and D.J.A.-J.).
Footnotes
Conflict of interest statement: C.G. and A.G. are cofounders and shareholders and A.L. is a part-time employee of MODAG GmbH.
This article is a PNAS Direct Submission.
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.1073/pnas.1700200114/-/DCSupplemental.
References
- 1.Skibba JL, Pinckley J, Gilbert EF, Johnson RO. Multiple primary melanoma following administration of levodopa. Arch Pathol. 1972;93:556–561. [PubMed] [Google Scholar]
- 2.Bertoni JM, et al. North American Parkinson’s and Melanoma Survey Investigators Increased melanoma risk in Parkinson disease: A prospective clinicopathological study. Arch Neurol. 2010;67:347–352. doi: 10.1001/archneurol.2010.1. [DOI] [PubMed] [Google Scholar]
- 3.Ferreira JJ, et al. Skin cancer and Parkinson’s disease. Mov Disord. 2010;25:139–148. doi: 10.1002/mds.22855. [DOI] [PubMed] [Google Scholar]
- 4.Paisán-Ruiz C, Houlden H. Common pathogenic pathways in melanoma and Parkinson disease. Neurology. 2010;75:1653–1655. doi: 10.1212/WNL.0b013e3181fb4466. [DOI] [PubMed] [Google Scholar]
- 5.Bajaj A, Driver JA, Schernhammer ES. Parkinson’s disease and cancer risk: A systematic review and meta-analysis. Cancer Causes Control. 2010;21:697–707. doi: 10.1007/s10552-009-9497-6. [DOI] [PubMed] [Google Scholar]
- 6.Olsen JH, Jørgensen TL, Rugbjerg K, Friis S. Parkinson disease and malignant melanoma in first-degree relatives of patients with early-onset melanoma. Epidemiology. 2011;22:109–112. doi: 10.1097/EDE.0b013e3181fe21a8. [DOI] [PubMed] [Google Scholar]
- 7.Walter U, et al. Frequency and profile of Parkinson’s disease prodromi in patients with malignant melanoma. J Neurol Neurosurg Psychiatry. 2016;87:302–310. doi: 10.1136/jnnp-2014-310239. [DOI] [PubMed] [Google Scholar]
- 8.Kareus SA, Figueroa KP, Cannon-Albright LA, Pulst SM. Shared predispositions of parkinsonism and cancer: A population-based pedigree-linked study. Arch Neurol. 2012;69:1572–1577. doi: 10.1001/archneurol.2012.2261. [DOI] [PubMed] [Google Scholar]
- 9.Meng S, et al. No association between Parkinson disease alleles and the risk of melanoma. Cancer Epidemiol Biomarkers Prev. 2012;21:243–245. doi: 10.1158/1055-9965.EPI-11-0905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dong J, et al. Susceptibility loci for pigmentation and melanoma in relation to Parkinson’s disease. Neurobiol Aging. 2014;35:1512.e5–1512.e10. doi: 10.1016/j.neurobiolaging.2013.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wirdefeldt K, et al. Parkinson’s disease and cancer: A register-based family study. Am J Epidemiol. 2014;179:85–94. doi: 10.1093/aje/kwt232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wagner J, et al. Anle138b: A novel oligomer modulator for disease-modifying therapy of neurodegenerative diseases such as prion and Parkinson’s disease. Acta Neuropathol. 2013;125:795–813. doi: 10.1007/s00401-013-1114-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Matsuo Y, Kamitani T. Parkinson’s disease-related protein, alpha-synuclein, in malignant melanoma. PLoS One. 2010;5:e10481. doi: 10.1371/journal.pone.0010481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Israeli E, et al. α-Synuclein expression selectively affects tumorigenesis in mice modeling Parkinson’s disease. PLoS One. 2011;6:e19622. doi: 10.1371/journal.pone.0019622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Watson-Hurst K, Becker D. The role of N-cadherin, MCAM and beta3 integrin in melanoma progression, proliferation, migration and invasion. Cancer Biol Ther. 2006;5:1375–1382. doi: 10.4161/cbt.5.10.3241. [DOI] [PubMed] [Google Scholar]
- 16.Smith AP, Hoek K, Becker D. Whole-genome expression profiling of the melanoma progression pathway reveals marked molecular differences between nevi/melanoma in situ and advanced-stage melanomas. Cancer Biol Ther. 2005;4:1018–1029. doi: 10.4161/cbt.4.9.2165. [DOI] [PubMed] [Google Scholar]
- 17.Lee BR, Matsuo Y, Cashikar AG, Kamitani T. Role of Ser129 phosphorylation of α-synuclein in melanoma cells. J Cell Sci. 2013;126:696–704. doi: 10.1242/jcs.122093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hansen C, et al. α-Synuclein propagates from mouse brain to grafted dopaminergic neurons and seeds aggregation in cultured human cells. J Clin Invest. 2011;121:715–725. doi: 10.1172/JCI43366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Deeg AA, et al. Anle138b and related compounds are aggregation specific fluorescence markers and reveal high affinity binding to α-synuclein aggregates. Biochim Biophys Acta. 2015;1850:1884–1890. doi: 10.1016/j.bbagen.2015.05.021. [DOI] [PubMed] [Google Scholar]
- 20.Hu HH, et al. PARKIN inactivation links Parkinson’s disease to melanoma. J Natl Cancer Inst. 2015;108:djv340. doi: 10.1093/jnci/djv340. [DOI] [PubMed] [Google Scholar]
- 21.Hintsala HR, Soini Y, Haapasaari KM, Karihtala P. Dysregulation of redox-state-regulating enzymes in melanocytic skin tumours and the surrounding microenvironment. Histopathology. 2015;67:348–357. doi: 10.1111/his.12659. [DOI] [PubMed] [Google Scholar]
- 22.Chen LL, et al. DJ-1: A promising marker in metastatic uveal melanoma. J Cancer Res Clin Oncol. 2015;141:315–321. doi: 10.1007/s00432-014-1804-2. [DOI] [PubMed] [Google Scholar]
- 23.Pardo M, et al. The characterization of the invasion phenotype of uveal melanoma tumour cells shows the presence of MUC18 and HMG-1 metastasis markers and leads to the identification of DJ-1 as a potential serum biomarker. Int J Cancer. 2006;119:1014–1022. doi: 10.1002/ijc.21942. [DOI] [PubMed] [Google Scholar]
- 24.Lopes da Fonseca T, Outeiro TF. ATP13A2 and alpha-synuclein: A metal taste in autophagy. Exp Neurobiol. 2014;23:314–323. doi: 10.5607/en.2014.23.4.314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wagner J, et al. Reducing tau aggregates with anle138b delays disease progression in a mouse model of tauopathies. Acta Neuropathol. 2015;130:619–631. doi: 10.1007/s00401-015-1483-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Galluzzi L, et al. Autophagy in malignant transformation and cancer progression. EMBO J. 2015;34:856–880. doi: 10.15252/embj.201490784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.White E. The role for autophagy in cancer. J Clin Invest. 2015;125:42–46. doi: 10.1172/JCI73941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.White E. Deconvoluting the context-dependent role for autophagy in cancer. Nat Rev Cancer. 2012;12:401–410. doi: 10.1038/nrc3262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kroemer G, Levine B. Autophagic cell death: The story of a misnomer. Nat Rev Mol Cell Biol. 2008;9:1004–1010. doi: 10.1038/nrm2527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Miracco C, et al. Beclin 1 and LC3 autophagic gene expression in cutaneous melanocytic lesions. Hum Pathol. 2010;41:503–512. doi: 10.1016/j.humpath.2009.09.004. [DOI] [PubMed] [Google Scholar]
- 31.Ellis RA, et al. Prognostic impact of p62 expression in cutaneous malignant melanoma. J Invest Dermatol. 2014;134:1476–1478. doi: 10.1038/jid.2013.497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Xie X, Koh JY, Price S, White E, Mehnert JM. Atg7 overcomes senescence and promotes growth of BrafV600E-driven melanoma. Cancer Discov. 2015;5:410–423. doi: 10.1158/2159-8290.CD-14-1473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Goodall ML, et al. Development of potent autophagy inhibitors that sensitize oncogenic BRAF V600E mutant melanoma tumor cells to vemurafenib. Autophagy. 2014;10:1120–1136. doi: 10.4161/auto.28594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ma XH, et al. Targeting ER stress-induced autophagy overcomes BRAF inhibitor resistance in melanoma. J Clin Invest. 2014;124:1406–1417. doi: 10.1172/JCI70454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Maes H, Agostinis P. Autophagy and mitophagy interplay in melanoma progression. Mitochondrion. 2014;19 Pt A:58–68. doi: 10.1016/j.mito.2014.07.003. [DOI] [PubMed] [Google Scholar]
- 36.Maddodi N, et al. Induction of autophagy and inhibition of melanoma growth in vitro and in vivo by hyperactivation of oncogenic BRAF. J Invest Dermatol. 2010;130:1657–1667. doi: 10.1038/jid.2010.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Becker D, Meier CB, Herlyn M. Proliferation of human malignant melanomas is inhibited by antisense oligodeoxynucleotides targeted against basic fibroblast growth factor. EMBO J. 1989;8:3685–3691. doi: 10.1002/j.1460-2075.1989.tb08543.x. [DOI] [PMC free article] [PubMed] [Google Scholar]