Education is considered an important social determinant of health (1, 2). Higher levels of educational attainment appear to be health-enhancing for those who have them (3), and provide intergenerational health benefits for their children (4) as well as their parents (5). Increased knowledge and skills leading to higher wages, as well as psychosocial advantages, such as social standing and control beliefs, are posited as mechanisms that link higher education and improved health (1, 2). In the context of low- and middle-income countries (LMICs), parental education (maternal in particular) is often held as a solution to improve children’s health (6). Meanwhile, a substantial number of governments in LMICs face considerable economic challenges, such as low macroeconomic growth, price instability, balance of payments crises, and high inflation, leading to their adoption of the International Monetary Fund’s (IMF) structural conditionality programs (hereafter, IMF-programs) (7). In exchange for the IMF’s low-cost lending and technical assistance, recipient governments must agree to implement a number of conditionalities, such as increased debt management, privatization of state-owned enterprises, trade liberalization, labor reforms, and anticorruption measures (8). It has been argued that IMF-programs not only directly impact health outcomes adversely, but also indirectly, by altering the influences of social determinants of health (8).
In PNAS, Daoud et al. (9) provide a cross-sectional assessment of whether the protective relationship between the educational attainment of the household head (hereafter, education) and child severe malnutrition, lack of access to health services, sanitation, shelter, and water are attenuated in countries that have been exposed to IMF-programs compared with countries not exposed to IMF-programs during the period 1992–2007. Daoud et al. (9) collectively refer to these outcomes as child health, even though the outcomes are a combination of child health (e.g., malnutrition) and household (e.g., access to water) outcomes, with the latter potentially being an independent input into the former (10). Daoud et al. report that the strength of the association between education and child/household outcomes is attenuated in countries with IMF-programs compared with countries without IMF-programs. This pattern, however, was not consistent across the five outcomes. For example, large attenuation was observed for access to health services and sanitation and, contrary to the hypothesis put forward by Daoud et al. (9), a stronger association was present for access to water. Inconsistency in the attenuation of education effects was also observed across urban and rural populations.
Daoud et al. (9) posit explanations to the expected as well as counter-expected findings, which, although plausible, remain to be tested. Importantly, the lack of a main effect of IMF-programs across the five outcomes warns us against overinterpreting the moderating (interaction) influence of IMF-programs on the observed effects of education. Even if there were to be moderator influences of IMF-programs, the extent to which the observed pattern for education is a reflection of moderating influences on other socioeconomic factors, such as household wealth, is unclear. The observational study design comparing education effects in countries with IMF-programs vs. countries without IMF-programs also prevents causal interpretation of the reported findings. Even though Daoud et al. recognize this critical limitation, they still claim that “IMF programs erode the protective effect of parental education” (9). Regardless, Daoud et al. should be commended for exploring a question of considerable policy relevance.
In this commentary, we discuss two issues that are central for policy deliberations on improving health in LMICs: (i) embracing the substantive country-heterogeneity in the relationship between education and health, and (ii) explicitly understanding and testing specific mechanisms through which education influences health.
Embracing Country-Specificity in Analysis and Inference
The nature and scope of exposure to an IMF-program is a function of a country’s unique circumstances (8). The circumstances vary with regard to the specific parameters of an IMF-program (e.g., stand-by arrangements vis-à-vis extended fund facility programs, the amount of financial support, the conditionality, and length of exposure to IMF-programs) as well as the socioeconomic and political context of the country (11). Thus, comparing countries with and without IMF-programs poses a fundamental identification challenge (8, 11). We provide an empirical illustration of the importance of country-specificity in the relationship between education and the five outcomes. Unlike Daoud et al. (9), however, we restricted this empirical exploration to selected countries for which we could observe a time period without an IMF-program (absence of at least 3 y) and a time period with an IMF-program in the Demographic and Health Surveys. Comparing the same country but separated by an unexposed and exposed time period is an improvement over the cross-sectional design adopted by Daoud et al. (9).
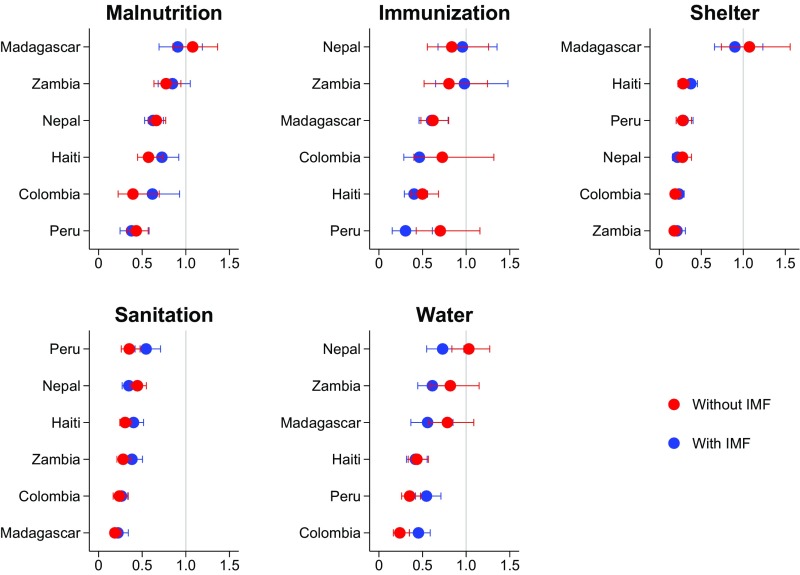
Our empirical analysis provides two salient observations. First, comparing the odds ratios (ORs) associated with being educated for the same country but separated by a without– and with–IMF-program period for the five outcomes, we find no consistent evidence for a moderating role of the IMF-program period on the effects of education (Fig. 1). In Colombia, for example, we find strong protective effects of education in both the without– and with–IMF-program periods. Conversely, in Madagascar, no statistically significant education effects were observed for two of five outcomes in both without– and with–IMF-program periods. Meanwhile, in Nepal, education effects were stronger (four of five outcomes) in the time period with an IMF-program. Second, there is marked country heterogeneity in the education effects under the IMF-program period. For severe malnutrition, the OR associated with being educated varied from 0.38 in Peru to 0.91 in Madagascar during the IMF-period, with similar ranges observed for the other outcomes.
Fig. 1.
ORs and 95% CIs with being educated for five outcomes under two time periods (without and with IMF-programs) in selected countries. ORs and 95% CIs are based on coefficients on education (no education vs. some education) in country-specific logistic regression models separately for five child/household outcomes. The five outcomes were: (i) severe malnutrition (severely stunted, underweight or wasted), (ii) immunization (never immunized vs. at least once), (iii) living in a dwelling without flooring material, (iv) access to surface water only, and (v) no access to a toilet of any kind. The sample included children younger than 5-y-old with complete data on the child’s sex and age as well as household head education. All models controlled for child age and sex, and SEs were clustered at the primary sampling unit level. Data for the analysis were from the Demographic and Health Surveys for Colombia (2000, 2005), Haiti (1994/1995, 2000), Madagascar (1997, 2003/2004), Nepal (2001, 2006), Peru (1991/1992, 2004/2006), and Zambia (1996, 2001/2002). IMF-program exposure by country and year was obtained from www.imf.org/external/pubs/ft/sdn/2011/data/sdn1115.xls. Additional data/analysis-related details can be requested from the authors, as space and formatting restrictions did not allow us to describe all of the details here.
Collectively, the above two findings suggest that a causal conclusion about the moderating effects of IMF-programs is problematic. Even if there were to be such effects, ignoring the country-specificity is likely to produce inferences that either could be misleading (at worst) or not useful (at best) for policy deliberation.
Education and Health: Time to Understand and Test the Mechanisms
That education is causally related to child outcomes is implicit in the study by Daoud et al. (9) and others (6). Existing observational studies, however, are likely to be confounded by unobserved factors, such as genetic (12) or other unobserved behavioral and familial factors, that affect both parental education and child health. The presence of such confounding in observational studies was recently demonstrated in a large cross-comparative study showing the similarity in the effect size of paternal and maternal education on child malnutrition (4). In addition, in the absence of randomized trials, quasi-experimental studies may provide a promising approach to identifying causal effects of parental schooling. In Zimbabwe, for example, a “natural experiment” exploiting a large supply-side education reform found no causal effect of parental schooling on child malnutrition, including severe malnutrition (13). These recent studies suggest that the association (including the stated magnitude) between parental education and child outcomes may not be causal and exaggerated.
One needs to question whether parental education is a specific exposure or whether it is simply a marker (proxy) for the household’s socioeconomic status. Because emerging evidence suggests that it may be the latter, understanding and testing the specific pathways (1) through which education impacts health might be more useful and productive (14). Disentangling and intervening on the context-specific pathways of education is likely to provide an opportunity to impact child health, particularly because uneducated adult parents are unlikely to return to school and gain a specific level of formal educational attainment. Providing health literacy to mothers, for example, has been shown to be independently related to child immunization, suggesting that there are potentially mitigating pathways for parents who are not formally educated (15). Furthermore, there may be “threshold” levels of formal education to detect and intervene on specific pathways (16). The impact on economic outcomes induced by basic education, for example, may be too small to make a significant difference in child health, as opposed to the new skills learned in upper secondary school or higher (such as future-oriented thinking) with strong economic returns in the labor market. In short, greater specificity to defining education and the mediating components that are likely to be moderated, across subgroups and contexts, would be arguably more informative and useful to improve child health in low-resource settings than exclusively relying on educational attainment.
Summary
Daoud et al. intentionally restricted their study largely to a period before the Millennium Development Goals were well under way, and before the substantial global infusion of resources to addressing child health in LMICs (9). Changes have also occurred to the lending mechanisms of multilateral financial institutions, such as the IMF and World Bank (17). Notwithstanding the identification challenges and issues highlighted in this commentary, these changes also raise the question of the validity of inferences drawn from pre- or early 2000s for current policy discussion and action. Global efforts to reduce the burden of avoidable disease and deprivation in LMICs could still be undermined, even in the presence of more health-sensitive and propoor policies by multilateral financial institutions. Although attempting to quantify the impact of adverse policy contexts on social factors of health is useful to trigger policy deliberations, even well-intentioned studies will suffer from serious shortcomings, such as those related to study design, inadequate evidence of pathways, and heterogeneous findings, underscoring the limits of empirical evidence to forge consensus and action. Under such circumstances, a “freedom” or “value-based” perspective to assessing the rationale for certain policies or interventions might be equally important (18), especially within the context of social determinants of health that often have considerable intrinsic eminence.
Footnotes
The authors declare no conflict of interest.
See companion article on page 6492.
References
- 1.Braveman P, Gottlieb L. The social determinants of health: It’s time to consider the causes of the causes. Public Health Rep. 2014;129:19–31. doi: 10.1177/00333549141291S206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Montez JK, Friedman EM. Educational attainment and adult health: Under what conditions is the association causal? Soc Sci Med. 2015;127:1–7. doi: 10.1016/j.socscimed.2014.12.029. [DOI] [PubMed] [Google Scholar]
- 3.Subramanian SV, Huijts T, Avendano M. Self-reported health assessments in the 2002 World Health Survey: How do they correlate with education? Bull World Health Organ. 2010;88:131–138. doi: 10.2471/BLT.09.067058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vollmer S, Bommer C, Krishna A, Harttgen K, Subramanian SV. The association of parental education with childhood undernutrition in low- and middle-income countries: Comparing the role of paternal and maternal education. Int J Epidemiol. 2016;46:312–323. doi: 10.1093/ije/dyw133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.De Neve J-W, Kawachi I. Spillovers between siblings and from offspring to parents are understudied: A review and future directions for research. Soc Sci Med. 2017;183:56–61. doi: 10.1016/j.socscimed.2017.04.010. [DOI] [PubMed] [Google Scholar]
- 6.Gakidou E, Cowling K, Lozano R, Murray CJL. Increased educational attainment and its effect on child mortality in 175 countries between 1970 and 2009: A systematic analysis. Lancet. 2010;376:959–974. doi: 10.1016/S0140-6736(10)61257-3. [DOI] [PubMed] [Google Scholar]
- 7.International Monetary Fund 2016 Factsheet IMF conditionality. Available at https://www.imf.org/external/np/exr/facts/conditio.htm. Accessed May 25, 2017.
- 8.Kentikelenis AE, Stubbs TH, King LP. IMF conditionality and development policy space, 1985–2014. Rev Int Polit Econ. 2016;23:543–582. [Google Scholar]
- 9.Daoud A, et al. Impact of International Monetary Fund programs on child health. Proc Natl Acad Sci USA. 2017;114:6492–6497. doi: 10.1073/pnas.1617353114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Corsi DJ, Mejía-Guevara I, Subramanian SV. Risk factors for chronic undernutrition among children in India: Estimating relative importance, population attributable risk and fractions. Soc Sci Med. 2016;157:165–185. doi: 10.1016/j.socscimed.2015.11.014. [DOI] [PubMed] [Google Scholar]
- 11.Summers LH, Pritchett LH. The structural-adjustment debate. Am Econ Rev. 1993;83:383–389. [Google Scholar]
- 12.Marioni RE, et al. Social Science Genetic Association Consortium Genetic variants linked to education predict longevity. Proc Natl Acad Sci USA. 2016;113:13366–13371. doi: 10.1073/pnas.1605334113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.De Neve JW, Subramanian SV. Causal effect of parental schooling on early childhood undernutrition—Quasi-experimental evidence from Zimbabwe. Am J Epidemiol. 2017 doi: 10.1093/aje/kwx195. [DOI] [PubMed] [Google Scholar]
- 14.Deaton A, Cartwright N. 2016 Understanding and misunderstanding randomized controlled trials. NBER Working Paper No. 22595 (National Bureau of Economic Research, Cambridge, MA). Available at www.nber.org/papers/w22595. Accessed May 25, 2017.
- 15.Johri M, et al. Association between maternal health literacy and child vaccination in India: A cross-sectional study. J Epidemiol Community Health. 2015;69:849–857. doi: 10.1136/jech-2014-205436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Heckman JJ. The economics, technology, and neuroscience of human capability formation. Proc Natl Acad Sci USA. 2007;104:13250–13255. doi: 10.1073/pnas.0701362104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ruger JP. The changing role of the World Bank in global health. Am J Public Health. 2005;95:60–70. doi: 10.2105/AJPH.2004.042002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sen A. Development as Freedom. Oxford Univ Press; Oxford: 2001. p. xvi. [Google Scholar]