Abstract
The purpose of this study was to investigate the relationship between the statuses of hospitalized children with diagnosis of respiratory tract disease with cigarette use in the parents. This descriptive study was conducted in a Gowerment Hospital in the Sakarya city center in Turkey between June 2007 and June 2008. The inclusion criterion was willingness of families with children hospitalized due to diagnosis of respiratory disease to particípate in the study. Data were collected from 345 parents using the questionnaire prepared by researchers. In our study parental smoking was observed in 42.3% of fathers, 7.8% mothers and for 20.9% both parents were smoking. It was found that the hospitalization rates were more than two times higher in children diagnosed with pneumonia and bronchitis and three times higher in children hospitalized for asthma whose parents smoke at home compared to those whose parents are non-smokers. Health care professionals who take care of children need to discuss the harmful effects of smoking and the importance of reducing childhood exposure to secondhand smoke; parents should be educated and encouraged not to smoke.
Keywords: parent, smoking, respiratory tract diseases, child, hospitalized
INTRODUCTION
Environmental Tobacco Smoke (ETS) exposure or passive cigarette smoking is a major public health problem [1]. Asthma and other respiratory diseases are a major health issue in childhood. Asthma is the most common chronic illness in children and adolescents [2]. Exposure to passive smoking in children is especially associated with increased upper and lowers respiratory infection and increased asthmatic symptoms. Results of epidemiologic studies provide strong evidence that exposure of children to environmental tobacco smoke is associated with increased rates of lower respiratory illness and asthma [3, 4, 5]. It is assumed that the asthma is the leading cause of the visits to physicians and hospitalization in young children and adolescents and is increasing in many countries [3]. Respiratory diseases account for approximately one third of the hospitalizations of children and adolescents less than 15 years of age in the United States and asthma is one of the leading causes of hospitalization for children [4]. A wide variety of factors have been identified as risks for respiratory disease. Environmental Tobacco Smoke is prominent one among these factors [5]. ETS is one of the most important and widespread toxic exposures to be found in the indoor environment of children. Exposure to ETS during early life is associated with many adverse health effects, such as childhood chronic respiratory symptoms and infections [6, 7]. Children are the most vulnerable group for ETS exposure because their bronchial tubes are smaller and their immune systems are less developed, making them more likely to develop respiratory and aural consequences if exposed to cigarette smoke. They also breathe faster and take in more harmful chemicals per kg of body weight than adults [7]. It is estimated that ETS is responsible for lower respiratory tract infections in 300 000 children each year. Among children younger than 18 years, it is estimated that 22 percent are exposed to passive smoke in their homes [8]. Globally, including Turkey, the percentage of children exposed to environmental tobacco smoke is noticeably high [1]. In Turkey, smoking rates increased by 89% from 1984 to 2000 [9]. Different Passive smoking rates (58.0%, 59.9% and 53.4%) were reported for children in Turkey [10, 11, 12]. Exposure of children to environmental tobacco smoke increases the risk of lower respiratory illness, especially during the first 2 years of life [13]. Wheezing and doctor-diagnosed asthma are more closely related to passive/environment tobacco smoke in the preschool than in school-children 5-16 years of age, but such findings should not detract from the statement that the single most important measure to improve the health of children would be the exclusion of tobacco smoke from their environments [14].
Tobacco smoke is one of the most important preventable environmental risk faktors to which children are exposed. The objective of the study was to investigate the relationship between the status of hospitalized children with diagnosis of respiratory tract disease with cigarette use in the parents.
MATERIALS AND METHODS
This descriptive study was conducted in a Gowerment Hospital in the Sakarya city center in Turkey between June 2007 and June 2008. Study started after receiving approval from related local authorities. The inclusion criteria was; willingness to participate of families who have children hospitalized due to diagnosis of respiratory disease in the date of study. Survey data were collected during 1 year on Monday and Friday in each week. Questionnaires were administered to families (n=345) whose children were hospotalized. Survey data were collected with a questionnaire prepared by researchers containing the characteristics of family and the child. Medical diagnosis of the patient was obtained from patient files. All parents in the sample received an anonymous self-administered questionnaire that containing an explanation about the purpose of the study, advising that they were under no obligation to complete the questionnaire, explaining that the information obtained would remain confidential. Filling of questionnaire has taken max.10 minutes.
Statistical analysis
The data were analysed using a statistical packet programme (SPSS 16). Data are presented as mean ± standard deviation (SD). Chi-Sguare Test was used for statistical analysis. Differences were considered significant at p< 0.05. Other data were descriptively presented as percentages.
RESULTS
The mean age of children was 21.47±22.96 months (min 1 month-max 96 month). Mean age of the mothers was 28.65±5.99 and father age was 32.27±6.09 years.
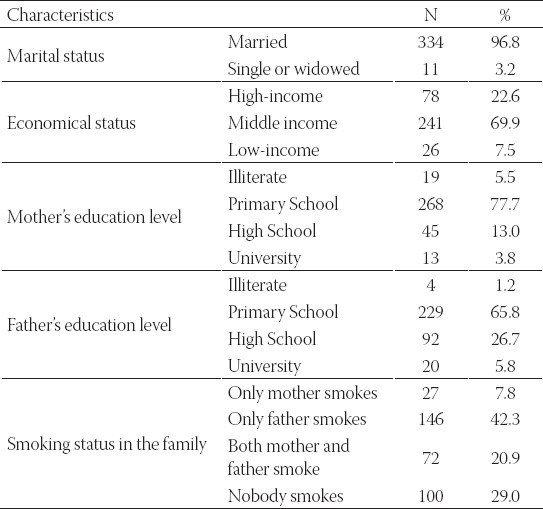
Smoking rates at home were found significantly higher in the family in which father’s educational status was low (χ2= 4.46, p=0.039). The smoking rate of parents in the families who defined themselves in bad economic situation and the status of children exposed to cigarette smoke at home was determined high and the differences were statistically significant (respectively;χ2=8.42, p=0.004, χ2=14.900, p=0.000)(Table 1).
TABLE 1.
Baseline characteristics of the study population
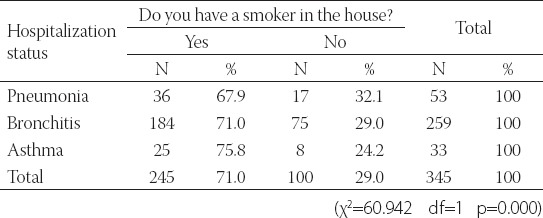
It was found that the rates of hospitalization with a diagnosis of pneumonia and bronchitis in children of parents who smoke at home more than two times higher than non-smoke, three times higher in those who are hospitalized with a diagnosis of asthma (Table 2).
TABLE 2.
Comparison of parents smoking status at home and the causes for children hospitalization
DISCUSSION
In our study, at least one parent was a smoker in more than 71% of the families. A survey in Greece revealed smoking prevalence among adults with preschool children to be 44% (52% of fathers and 36% of mothers) [15]. Other studies found that the proportion of children aged 6-12 years living with a currentsmoker in the household was around 50%: 46% in Germany, 48% in Switzerland and 58% in Italy and the Netherlands [16]. In our study parental smoking were 42.3% for father, 7.8% for mother and 20.9% both parents. In Farideh’s study [17] it was found that at least one parent in 231 (35.7%) families was a smoker. A recent global survey has estimated the prevalence of smoking in men to be 40% as compared to 12% in women [18]. The World Health Organization (WHO) conducted the Global Youth Tobacco Survey between 1999 and 2005 and found that approximately 44% of youths were exposed to tobacco smoke at home and that 47% had at least 1 parent who smoked [19]. In our study, the families who defined themselves as in bad economic situation and the family that father’s educational status was low the rates of exposure to cigarette smoke of their children at home was determined high. Reports suggest that smoking remains concentrated among the poor and less well educated, precisely the families who can least afford the financial burden [17, 20, 21]. A study from Tehran identified poverty as one of the most common reasons for cigarette smoking in parent [17]. Exposure is particularly high in low-income. Twenty-five percent of children live with at least one smoker, and parental smoking accounts for 90% of children’s exposure in the home [22]. Farideh and Mojgan [17] shows the prevalence of smokers in families with different socio-economic status (SES), highlighting the fact that in families with high socioeconomic status, the percentage of smokers was significantly lower than in the families with middle and lower SES (p=0.025 in both instances). Passive smoking has a harmful effect on the respiratory health of children. In our study, the rates of hospitalization with a diagnosis of pneumonia and bronchitis in children of parents who smoke at home was determined more than two times higher than non-smoke Rantakallio [23] showed that, among children younger than 1 year, those with mothers who smoked cigarettes were almost four times as likely to be hospitalized as were the infants of nonsmoking mothers, and the number of hospitalizations increased with the number of cigarettes the mother smoked per day. During the first 5 years of life, pneumonia and bronchitis were about twice as likely and acute nasopharyngitis and sinusitis in the upper respiratory tract were about 1.5 times as likely in children whose mothers smoke. In our study, the rates of hospitalization with a diagnosis of asthma in children of parents who smoke at home more than three times higher than non-smoke. In Gilmour’s study it is stated that since the 1980s, numerous large studies have identified significant relations between parental smoking and development of asthma in children [24]. Tanaka et al. [25] had stated in a study which conducted in Japan in children who exposured to tabacco smoke increased prevalence of wheeze and asthma. They account for leading causes of visits to physicians and hospitalization with asthma being one of the main and increasing causes of hospitalization in young children and adolescents in many countries [3]. The results of studies in various countries are comparable with our results.
CONCLUSION
In this study, smoking rate was found to be higher in the parents whose children are hospitalized with a diagnosis of pneumonia, bronchitis and astma. Parents must be educated about harmfull effects of tobacco smoke exposure on their children.
DECLARATION OF INTEREST
We declare no financial support from government or other parties for this study.
REFERENCES
- 1.Cinar ND, Dede C. Effects of environmental tobacco smoke on the respiratory health of children. Pak. J. Med. Sci. 2010;26:223–228. [Google Scholar]
- 2.Niksić D, Saracević E, Cemerlić-Kulić A, Kurspahić-Mujcić A, Bajraktarević S, Niksić H. Evaluation of efficiency practical issues in the management of childhood asthma. Bosn J Basic Med Sci. 2005;5(4):40–5. doi: 10.17305/bjbms.2005.3229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jedrychowski W, Perera FP, Maugeri U, Budzyn DM, Mroz E, Flak E, et al. Early wheezing phenotypes and severity of respiratory illness in very early childhood: Study on intrauterine exposure to fine particle matter. Environ Int. 2009;35:877–884. doi: 10.1016/j.envint.2009.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Owings MF, Lawrence L. Detailed diagnoses and procedures. National Hospital Discharge Survey. Vital. Health Stat. 1999;13:4–16. [PubMed] [Google Scholar]
- 5.Gergen PJ, Fowler JA, Maurer KR, et al. The burden of environmental tobacco smoke exposure on the respiratory health of children 2 months through 5 years of age in the United States: Third National Health and Nutrition Examination Survey 1988-1994. Pediatrics. 1998;101:1–6. doi: 10.1542/peds.101.2.e8. [DOI] [PubMed] [Google Scholar]
- 6.Patja K, Hakala S, Prattala R, Ojala K, Boldo E, Oberg M. Adult smoking as a proxy for environmental tobacco smoke exposure among children - Comparing the impact of the level of information in Estonia, Finland and Latvia. Prev. Med. 2009;49:240–244. doi: 10.1016/j.ypmed.2009.05.014. [DOI] [PubMed] [Google Scholar]
- 7.Keskinoglu P, Aksakoglu G. Pasif sigara içiciligin çocuklarda solunum sistemi uzerindeki etkileri. Turk. Arch. Ped. 2007;42:136–141. [Google Scholar]
- 8.Secondhand Smoke. [cited 2010 May 8]. Available from: http://www.cancer.gov/news-center/tip-sheet-secondhand-smoke .
- 9.Zahran SH, Zack MM, Vernon-Smiley EM, Hertz FM. Healthrelated quality of life and behaviors risky to health among adults aged 18-24 years in secondary or higher educationunited states 2003-2005. J. Adolescent. Health. 2007;41:389–397. doi: 10.1016/j.jadohealth.2007.05.011. [DOI] [PubMed] [Google Scholar]
- 10.Bildik HN, Bilgin E, Demirdogen E, Yildiz E, Aslan D, Yalcin S. Çocuklar sigara dumanindan pasif etkilenim açısından risk altında mı? Bir ilkogretim okulu deneyimi. Cocuk Sagligi Hast. Derg. 2008;51:147–152. [Google Scholar]
- 11.Ekerbiçer HC, Celik M, Güler E, DavutoSlu M, Kilinç M. Evaluating environmental tobacco smoke exposure in a group of Turkish primary school students and developing intervention methods for prevention. BMC Public Health. 2007;7:202. doi: 10.1186/1471-2458-7-202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Boyacı H, Duman C, Başyigit I, Ilgazli A, Yıldız F. İlkokul çocuklarında çevresel sigara dumanına maruziyetinin idrar kotinin duzeyi ile değerlendirilmesi. Tuberk Toraks. 2004;52:231–236. [PubMed] [Google Scholar]
- 13.Dybing E. Passive smoking, sudden infant death syndrome (SIDS) and childhood infections. Hum Exp Tox. 1999;18:202–205. doi: 10.1191/096032799678839914. [DOI] [PubMed] [Google Scholar]
- 14.Lenney W. The etiology of childhood asthma. Paediatr Child Health. 2009;19:257–260. [Google Scholar]
- 15.Vardavas CI, Athanasopoulos D, Balomenaki E, Niaounaki D, Linardakis MK, Kafatos AG. Smoking habits of Greek preschool children’s parents. BMC Public Health. 2007;7:112. doi: 10.1186/1471-2458-7-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pattenden S, et al. Parental smoking and children’s respiratory health: independent effects of prenatal and postnatal exposure. Tob Control. 2006;15:294–301. doi: 10.1136/tc.2005.015065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Farideh S, Mojgan P. Smoking practices and risk awareness in parents regarding passive smoke exposure of their preschool children: A cross-sectional study in Tehran. IJMS. 2008;62:228–235. [PubMed] [Google Scholar]
- 18.Wipfli H, Avila-Tang E, Navas-Acien A, Sungroul-Kim Onicescu G, Yuan J, et al. Secondhand Smoke Exposure of Women and Children: Evidence from 31 Countries. Am. J. Public Health. 2008;98:672–679. doi: 10.2105/AJPH.2007.126631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.The GTSS, Collaborative Group. A cross-country comparison of exposure to secondhand smoke among youth. Tob. Control. 2006;15(suppl 2):114–19. doi: 10.1136/tc.2006.015685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cornelius MD, Goldschmidt L, Dempsey DA. Environmental tobacco exposure in low-income 6-year-olds: Parent report and urine cotinine measures. Nicotine Tob. Res. 2003;5:333–339. doi: 10.1080/1462220031000094141. [DOI] [PubMed] [Google Scholar]
- 21.Winickoff JP, Berkowitz AB, Brooks K, Tanski SE, Geller A, Thomson C, et al. State-of-the-art interventions for office-based parental tobacco control. Pediatrics. 2005;115:750–760. doi: 10.1542/peds.2004-1055. [DOI] [PubMed] [Google Scholar]
- 22.Gerald LB, Gerald JK, Gibson L, Patel K, Zhang S, McClure LA. Changes in Environmental Tobacco Smoke Exposure and Asthma Morbidity Among Urban School Children. CHEST. 2009;135:911–916. doi: 10.1378/chest.08-1869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rantakallio P. Relationship of maternal smoking to morbidity and mortality of the child up to the age of five. Acta Paediatr. Scand. 1978;67:621–631. doi: 10.1111/j.1651-2227.1978.tb17813.x. [DOI] [PubMed] [Google Scholar]
- 24.Gilmour MI, Jaakkola MS, London SJ, Nel AE, Rogers CA. How exposure to environmental tobacco smoke, outdoor air pollutants and increased pollen burdens influences the incidence of asthma. Environ Health Perspect. 2006;114:627–33. doi: 10.1289/ehp.8380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tanaka K, Miyake Y, Arakawa M, Sasaki S, Ohya Y. Prevalence of Asthma and Wheeze in Relation to Passive Smoking in Japanese Children. Ann Epidemiol. 2007;17:1004–1010. doi: 10.1016/j.annepidem.2007.07.108. [DOI] [PubMed] [Google Scholar]


