Abstract
We report a case of intrathoracic malignant peripheral nerve sheath tumor in a 65-year old woman revealed after a few-month history of progressive dyspnea, appetite and body mass loss. The chest magnetic resonance (MR) examination revealed the presence of a large tumor occupying the mediastinum and a major portion of the right hemithorax. The diagnostic tumor sample was obtained by parasternal biopsy in local anesthesia. The surgical resection of the tumor could not be performed due to its excessive size, intrathoracic involvement and bad respiratory reserves of a patient. The chemotherapy and irradiation were performed as palliative measures. The lethal outcome appeared 10 months after the diagnosis was established.
Keywords: malignant peripheral nerve sheath tumor, mediastinum, magnetic resonance imaging
CASE REPORT
The patient was a 65-year old woman, a non-smoker, who was developing the disease gradually, over a couple of months, exhibiting the symptoms of difficult breathing, dyspnea on exertion, appetite and weight loss. For the last 10 years she was suffering from chronic obstructive pulmonary disease (COPD). The chest X-ray revealed a large homogeneous opacity, almost entirely occupying the right hemithorax with a consequent displacement of the mediastinal structures to the left (Figure 1).
FIGURE 1.

Chest X-ray revealed a large homogeneous opacity almost entirely occupying the right hemithorax and displacing the mediastinal structures to the left.
The chest magnetic resonance (MR) examination confirmed the presence of an intrathoracic tumor, solid in structure, involving the mediastinum, measuring 17x17x20 cm. The tumor occupied the mediastinal space involving almost completely the right hemithorax, from the prevertebral fascia to the anterior chest wall, reaching the upper thoracic aperture. The tumor also encircled and deformed the lumen of the trachea and large blood vessels. The bone structures remained intact (Figure 2).
FIGURE 2.
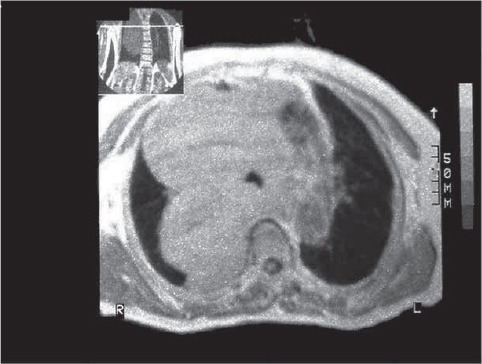
The chest MRI revealed the presence of huge thoracic tumor occupying the right hemithorax. The tumor also encircled and deformed the lumen of the trachea and large blood vessels.
Gas analyses of the arterial blood confirmed the presence of respiratory insufficiency: arterial pressure of oxygen (pO2) 7.12 kPa, arterial pressure of carbon dioxide (pCO2) 6.13 kPa, arterial oxygen saturation 89.5%, pH 7.45. Pulmonary function test revealed a combined (obstructive-restrictive) ventilation disorder: vital capacity (VC) 1.23 L (46%), forced expiratory volume in first second (FEV1) 1.04 L (49%).
Fine-needle aspiration biopsy of the tumor provided a sample involved by malignant cells, but the tumor type could not be determined, so the tumor biopsy sampling was obtained. Parasternal approach to the tumor in a local anesthesia provided a tumor tissue sample composed of a mixed matrix (Figure 3a) and occasionally settled oval and spindle shaped cells with hypechromatic and moderately pleomorphic nuclei (Figure 3b). The blood vessels were thickened and hyalinized (Figure 3c). The tumor infiltrated the antracotic pigmented alveolar lung tissue (Figure 3d). On the basis of the histological evaluation, the diagnosis of malignant infiltrative pulmonary peripheral nerve sheath tumor was finally established. As the surgical resection of the tumor could not be performed due to its excessive size, intrathoracic involvement and bad respiratory reserves of a patient, single course chemotherapy with Ifosphamide and Uromitexane was administered, accompanied by a split-course palliative irradiation therapy in dose of 40 Gy, because of tumor-induced compression of the mediastinal structures. A lethal outcome occurred 10 months after the diagnosis had been established.
FIGURE 3.
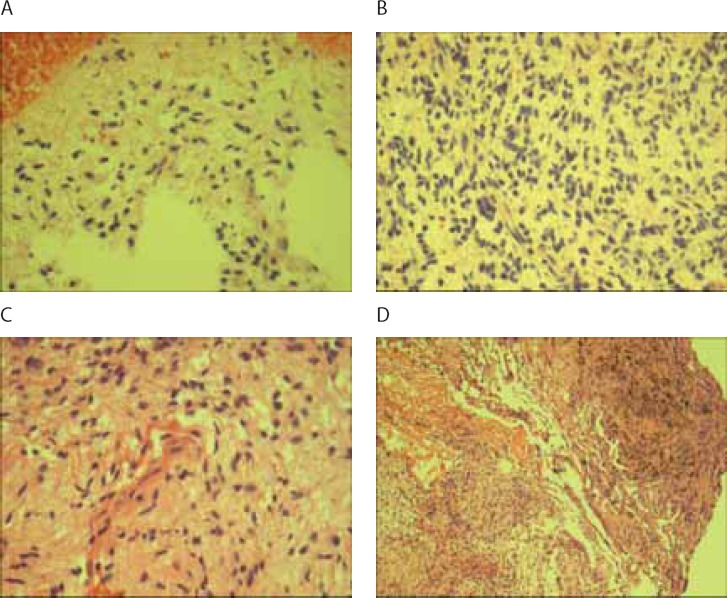
Mixed matrix (A) and occasionally settled oval and spindle shaped cells with hypechromatic and moderately pleomorphic nuclei (B). The blood vessels were thickened and hyalinized (C). The tumor infiltrated the antracotic pigmented alveolar lung tissue (D).
DISCUSSION
Neurogenic tumors make about 10-20% of all mediastinal tumors. These tumors may develop from peripheral nerves, nerve sheaths or from sympathetic ganglions [1]. They are most commonly localized in the posterior mediastinum [1], originating in most cases from the intercostals nerves [2]. Formerly, neurogenic malignant tumors were classified under different names (malignant schwannoma, neurogenic sarcoma or neurofibrosarcoma) and today they are generally designated by the term malignant peripheral nerve sheath tumors (MPNST) [1]. Both sexes are almost equally affected with these tumors, although in some studies the slight predominance of the affected females was noted [3]. They are commonly revealed in the 30-50 years age group [2]. The subjects suffering from neurofibromatosis I (NF1) have a greater risk of MPNST. These tumor occur in about 2-5% of NF1 patient compared with an incidence of 0.001% in the general population [4]. They most frequently affect the extremities, but may also affect other areas, predominantly head, neck, pelvis and retroperitoneum [3, 5], but it rarely develops in the thoracic cavity[5]. MPNST usually cause no symptoms [1]. Due to compression of the intercostal nerve or large airways, some patients may develop pain or dyspnea, or some other respiratory symptoms, like cough [1].Our patient had a severe dyspnea due to tumor-induced compression on the trachea and large airways. When MPNST involve deep tissue nerves, it can hardly be directly observed, so the early diagnosis is difficult [5]. MPNST is therefore usually detected in its advanced stage, when it has already reached a considerable size [5]. The method of choice for the treatment of MPNST is an extensive and total surgical resection [1-3, 5]. In patients with unresectable tumor chemotherapy and radiotherapy are modality of treatment [2]. MPNST unfortunately belong to the group of chemo and irradiation resistant tumor [3]. A curative chemotherapy regimen for MPNST has not been recommended yet [1], so chemotherapy is sometimes applied for palliation purposes [4].The efficacy of the new drugs such as anti-angiogenic agents and epidermal growth factor receptor antagonists is still being evaluated in the ongoing clinical trials [6].With the latest advances in molecular genetics, the target therapy for this tumor type is expected to be discovered [4].
DECLARATION OF INTEREST
We did not receive any financial support for this work and there is no conflict of interest.
REFERENCES
- 1.Lai RS, Lin SL, Hsu SS, Wu MT. Intrathoracic paraspinal malignant peripheral nerve sheath tumor. J Chin Med. Assoc. 2006;69:37–41. doi: 10.1016/S1726-4901(09)70109-1. [DOI] [PubMed] [Google Scholar]
- 2.Duwe BV, Sterman DH, Musani AI. Tumors of the Mediastinum. Chest. 2005;128:2893–2909. doi: 10.1378/chest.128.4.2893. [DOI] [PubMed] [Google Scholar]
- 3.Kar M, Deo SV, Shukla NK, Malık A, Datta Gupta S, Mohantı BK, Thulkar S. Malignant peripheral nerve sheath tumors (MPNST)Clinicopathological study and treatment outcome of twenty-four cases. World J Surg Oncol. 2006;4:55. doi: 10.1186/1477-7819-4-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ferner RE, Gutmann DH. International Consensus Statement on Malignant Peripheral Nerve Sheath Tumors in Neurofibromatosis. Cancer Res. 2002;62:1573–1577. [PubMed] [Google Scholar]
- 5.Shimizu J, Arano Y, Murata T, Ishikawa N, Yachi T, Nomura T, Minato H. A case of Intrathoracic giant malignant peripheral nerve sheath tumor in neurofibromatosis type I (von Recklinghausen’s disease) Ann Thorac Cardiovasc Surg. 2008;14:42–47. [PubMed] [Google Scholar]
- 6.Bernhard N, Morris SK, Taylor G, Oudjhane K, Baruchel S. Massive intrathoracic tumor in a relatively asymptomatic boy. Pediatr Ann. 2007;36:632–635. doi: 10.3928/0090-4481-20071001-05. [DOI] [PubMed] [Google Scholar]


