Abstract
Regulatory T cells (Treg) function in the prevention of excessive inflammation and maintenance of immunological homeostasis. However, these cells may also interfere with resolution of infections or with immune reactions following vaccination. Effects of Treg on vaccine responses are nowadays investigated, but the impact of vaccination on Treg homeostasis is still largely unknown. This may be a relevant safety aspect, since loss of tolerance through reduced Treg may trigger autoimmunity.
In exploratory clinical trials, healthy adults were vaccinated with an influenza subunit vaccine plus or minus the adjuvant MF59®, an adjuvanted hepatitis B subunit vaccine or a live attenuated yellow fever vaccine. Frequencies and phenotypes of resting (rTreg) and activated (aTreg) subpopulations of circulating CD4+ Treg were determined and compared to placebo immunization.
Vaccination with influenza vaccines did not result in significant changes in Treg frequencies and phenotypes. Vaccination with the hepatitis B vaccine led to slightly increased frequencies of both rTreg and aTreg subpopulations and a decrease in expression of functionality marker CD39 on aTreg. The live attenuated vaccine resulted in a decrease in rTreg frequency, and an increase in expression of activation marker CD25 on both subpopulations, possibly indicating a conversion from resting to migratory aTreg due to vaccine virus replication.
To study the more local effects of vaccination on Treg in lymphoid organs, we immunized mice and analyzed the CD4+ Treg frequency and phenotype in draining lymph nodes and spleen. Vaccination resulted in a transient local decrease in Treg frequency in lymph nodes, followed by a systemic Treg increase in the spleen.
Taken together, we showed that vaccination with vaccines with an already established safe profile have only minimal impact on frequencies and characteristics of Treg over time. These findings may serve as a bench-mark of inter-individual variation of Treg frequencies and phenotypes following vaccination.
Introduction
The immune system is trained to protect the host against a broad variety of pathogenic threats. When properly activated, a successful response to infection results in protection against the disease. However, to prevent excessive inflammation due to immune activation, the response needs to be tightly controlled to maintain and regain immunological homeostasis [1]. One of the mechanisms by which the body is equipped to do so, is via the negative control function of regulatory T cells (Treg) and improperly functioning Treg can result in severely uncontrolled immune reactions with autoimmunity and even death as result [2–4]. In addition to their role in prevention of autoimmunity, Treg were found to be imperative in the protection of the body from damage during (viral) infections. Several studies have shown that during infections the balance between functional Treg and effector T cells (Teff) is essential, as Treg depletion resulted in exacerbation of the disease, immune pathology and a delay in viral clearance [5–7]. On the other hand, Treg were also found to interfere in resolution of viral infections, e.g. in mouse models of hepatitis B virus (HBV) infection where their depletion led to more active, virus-specific T cells and improved viral clearance [8,9]. Thus, Treg regulation of immune responses can prevent autoimmunity and excessive tissue damage, but this process potentially allows persistent infections as well and therefore, the correct outcome of Treg dampening is vital [7,10].
Apart from infections, Treg may also interfere with immune reactions following vaccination. Dampening of the response to vaccines, which are usually mimics or derivatives of infectious agents, can potentially result in lower vaccine efficacy as was shown in anti-tumor vaccinations [11,12]. For this reason, the effect of Treg on vaccine responses is nowadays studied and several new strategies are explored to improve vaccine effectiveness by temporarily depleting or inhibiting Treg [13,14]. However, it has become more and more evident that the interaction between Treg and Teff during infection and vaccination is complex and pathogen-specific. Thus depletion of Treg might not be a straightforward solution to improve vaccine responses [10].
Not only knowledge on the effect of Treg on vaccine responses is essential, but also the other way around, namely the effect of vaccination on Treg requires attention. Because íf vaccination would significantly affect Treg frequency or function, this may result in uncontrolled (auto-)immune responses and thus be a relevant safety risk of vaccination. Therefore, we studied the effect of vaccinations on human CD4+ Treg responses, using a panel of four commonly used antiviral vaccines: a trivalent influenza vaccine (TIV) with and without the addition of adjuvant MF59® (Fluad® or Agrippal®), a HBV subunit vaccine (Engerix-B®) and a live attenuated yellow fever vaccine (Stamaril®). We analyzed peripheral blood mononuclear cells (PBMC) obtained from healthy volunteers that had been vaccinated in the context of broader study trials (BIOVACSAFE; [15]). At several days post vaccination (dpv), the frequency and phenotype of CD4+ Treg subpopulations in peripheral blood was examined by flow cytometry. For the analysis of local effects of the influenza and hepatitis B vaccines on Treg, we vaccinated mice and analyzed the CD4+ CD25+ Foxp3+ Treg frequency and phenotype in draining lymph nodes and spleen at several days post vaccination.
Here, we show that vaccination with commonly used, human anti-viral vaccines minimally impacts the frequency and characteristics of Treg over time in both men and mice, but that the effects are distinct for the different vaccines analyzed.
Materials and methods
Human inpatient study design
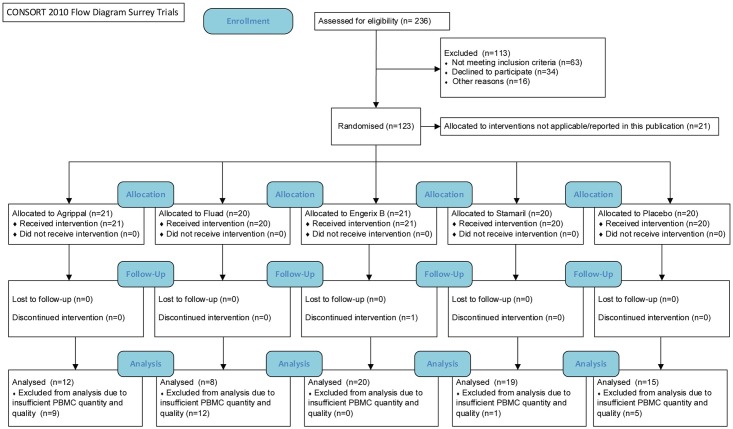
Three partial-blind (participant and laboratory), randomised, placebo-controlled exploratory studies (clinicaltrials.gov; NCT01765413, NCT01771354 and NCT01771367; protocols in S1–S3 Text and [15]) were conducted at the Surrey Clinical Research Centre, University of Surrey, Guildford, UK (as part of the BIOVACSAFE consortium-funded clinical study protocols) after approval of procedures by London-Surrey Borders Research Ethics Committee (REC References: 12LO/1871, 12/LO/1899, 13/LO/0044). The studies were undertaken in accordance with the Declaration of Helsinki and good clinical practices. Healthy participants (male and female) ranging from 18 to 45 years of age (characteristics in Table 1) were recruited into the studies after written informed consent. See CONSORT diagram and checklist (Fig 1 and S4 Text, respectively). Participants remained in the Centre from 1 day before vaccination until 5 days post vaccination for daily monitoring. After day 5, several outpatient follow-up visits took place.
Table 1. Summary of participant characteristics and pre-vaccination Treg values.
| Parameter | Influenza vaccine | Hepatitis B vaccine | Yellow fever vaccine |
|---|---|---|---|
| N participants | |||
| Placebo | 3 | 4 | 8 |
| Vaccine | 12 (Agrippal®) | 20 | 19 |
| Vaccine | 8 (Fluad®) | ||
| Age a | |||
| Placebo | 33 ± 2.65 | 30 ± 3.63 | 29 ± 2.00 |
| Vaccine | 27 ± 2.06 (Agrippal®) | 32 ± 1.47 | 30 ± 1.73 |
| Vaccine | 28 ± 2.05 (Fluad®) | ||
| Sex (M/F) a | |||
| Placebo | 1/2 | 2/2 | 5/3 |
| Vaccine | 3/9 (Agrippal®) | 17/3 | 12/7 |
| Vaccine | 4/4 (Fluad®) | ||
| Baseline frequency (%) a, b | |||
| CD4+CD45RA+FoxP3+ (rTreg) | 1.02 ± 0.09 | 4.04 ± 0.41 | 3.01 ± 0.21 |
| CD4+CD45RA-FoxP3++ (aTreg) | 0.99 ± 0.10 | 2.32 ± 0.21 | 2.44 ± 0.18 |
| Baseline frequency (%) within rTreg a, b | |||
| CD25 | 17.4 ± 1.1 | 13.5 ± 2.2 | 7.0 ± 0.9 |
| CD39 | 23.0 ± 2.7 | 25.2 ± 2.0 | 16.1 ± 0.9 |
| CD31 | n.d. | 85.8 ± 1.6 | 82.8 ± 1.3 |
| HLA-DR | n.d. | 52.5 ± 3.9 | 53.6 ± 1.5 |
| CCR4 | n.d. | 51.8 ± 4.0 | 50.9 ± 1.9 |
| CCR7 | 72.3 ± 3.5 | 63.5 ± 4.5 | 59.4 ± 2.1 |
| Baseline frequency (%) within aTreg a, b | |||
| CD25 | 58.0 ± 1.5 | 49.9 ± 2.7 | 51.5 ± 1.7 |
| CD39 | 67.1 ± 5.5 | 61.3 ± 5.6 | 66.3 ± 5.2 |
| CD31 | n.d. | 17.8 ± 3.7 | 15.3 ± 1.4 |
| HLA-DR | n.d. | 47.5 ± 3.5 | 43.5 ± 2.2 |
| CCR4 | n.d. | 76.7 ± 2.5 | 87.7 ± 1.1 |
| CCR7 | 41.2 ± 2.5 | 23.3 ± 3.2 | 19.3 ± 1.6 |
a mean ± SEM
b for influenza and yellow fever vaccines baseline is day 0, for hepatitis B vaccine baseline is day 168
n.d. = not determined
Fig 1. CONSORT flow diagram.
Influenza
Participants, assumed to be previously primed with hemagglutinin via vaccination or natural infection, received either a single 0.5 ml dose of a non-adjuvanted TIV (Agrippal®, Novartis Vaccines), a MF59®-adjuvanted TIV (Fluad®, Novartis Vaccines) or placebo (saline). Both vaccines contained the recommended composition for the 2012/2013 northern hemisphere influenza season (as described in [16]). Vaccine or placebo was administered intramuscularly (i.m., m. deltoideus) and PBMC samples were collected just before vaccination (day 0) and at days 1, 3, 5, 14 and 21 after vaccination. PBMC were purified and cryopreserved until further processing.
Hepatitis B
Participants seronegative for anti-hepatitis B antibodies were vaccinated i.m. (m. deltoideus) with either 1 ml doses of an alum-adjuvanted hepatitis B vaccine (Engerix-B® containing 20 μg hepatitis B surface antigen, GlaxoSmithKline) or placebo (saline). Vaccine or placebo doses were administered at days 0, 28 and 168 and PBMC samples were collected just before vaccination (day 168) and at day 1, 3 and 14 (days 169, 171 and 182) after dose 3. PBMC were purified and cryopreserved until further processing.
Yellow fever
Participants seronegative for anti-yellow fever antibodies were vaccinated subcutaneously (s.c., deltoid region) with a single 0.5 ml dose of a live attenuated yellow fever vaccine (Stamaril® containing not less than 1000 IU, Sanofi Pasteur) or placebo (saline). Blood samples were collected just before vaccination (day 0) and at days 1, 5, 7 and 14 after vaccination. PBMC were purified and cryopreserved until further processing.
Cell thawing
Vials containing frozen PBMC were quickly thawed in a 37°C water bath and cold RPMI medium (Gibco, Thermo Fisher Scientific, Landsmeer, The Netherlands) containing 5% NHS (Merck Millipore, Amsterdam, The Netherlands) was added dropwise to the cell suspension. The cells were washed twice with RPMI medium (5% NHS) and subsequently resuspended in PBS supplemented with 2% FBS (Lonza, Breda, The Netherlands) for flow cytometric staining.
Animals
Ethical statement
All animal experiments were performed in strict accordance to the Dutch Animal Experimentation Act and EU directives 86/609/CEE and 2010/63/EU related to the protection of vertebrate animals used for experimental and other scientific purposes. The experimental protocols were approved by the Committee on Animal Experiments of the University of Utrecht (DEC2012.II.08.114) and performed in the Central Laboratory Animal Research Facility of the University of Utrecht, which has AAALAC (Association for Assessment and Accreditation of Laboratory Animal care) accreditation.
Mice
CB6F1 mice (female; 6–10 weeks) were obtained from Charles River Laboratories and were housed at the Central Laboratory Animal Research Facility of the University of Utrecht, The Netherlands. Mice were kept under standard conditions and received water and food ad libitum.
Animal study design
Mice were randomly divided in control or treatment groups and at day 0, mice were injected i.m. (m. quadriceps) with 50 μl adjuvant/vaccine in PBS. Complete Freund’s Adjuvant (CFA, 0.5 mg/ml; Difco, New Jersey, USA) was prepared by mixing with equal volumes of PBS. Lipopolysaccharide (LPS; E. coli 0127:B8 L4516, Sigma-Aldrich, Zwijndrecht, The Netherlands) was injected as 0.5 mg/ml solution in 50 μl PBS. The influenza immunogens (TIV, a kind gift from Novartis Vaccines) consisted of 1.5 μg purified hemagglutinin and neuraminidase of each of the three influenza strains present in the Novartis Flu-vaccines as recommended for the 2012/2013 northern hemisphere influenza season (as described in [16]) in 50 μl PBS (TIV−) or in 25 μl PBS mixed with an equal volume of adjuvant MF59® (Novartis Vaccines; TIV+). Hepatitis B immunization was performed with an injection of 50 μL of Engerix-B® (20 μg/mL hepatitis B surface antigen, a kind gift from GlaxoSmithKline). The vaccine doses for mice equaled 1/10th of a human vaccine dose. Mock-injected animals received 50 μl PBS.
All animals were monitored on a daily basis the first 2 days post immunization and from thereon weekly. No signs of pain or other distress were observed. At day 3, 7, 14 and 21 post vaccination animals were humanely euthanized using a carbon dioxide chamber and draining lymph nodes (dLN, lnn. inguinales) and spleen were removed and kept on ice in IMDM medium (Gibco, Thermo Fisher Scientific) supplemented with 2% FBS (Lonza) for further processing.
Single cell suspensions
Single cell suspensions of draining lymph nodes and spleens were prepared using a 70 μm nylon mesh (BD Bioscience, New Jersey, USA). Erythrocytes were depleted from the splenic single cell suspension by incubation in ACK-lysis buffer (150 mM NH4Cl and 1 mM NaHCO3, pH 7.4) for 5 min at ice. Cells were resuspended in PBS supplemented with 2% FBS (Lonza) for flow cytometric staining.
Flow cytometric analysis
For analysis of the human samples, all antibodies were purchased from Miltenyi Biotec (Leiden, The Netherlands), unless stated otherwise. Cells were surface-labeled with mouse-anti-human monoclonal antibodies CD4-APC (M-T466, IgG1), CD25-FITC (M-A251, IgG1, BD Biosciences), CD31-BV510 (WM59, IgG1, BD Biosciences), CD39-PE (MZ18-23C8, IgG1), CD45RA-PerCP (T6D11, IgG2b), HLA-DR-FITC (AC122, IgG2a), rat-anti-human monoclonal antibody CCR7-BV510 (3D12, IgG2a, BD Biosciences) and recombinant human monoclonal antibody CCR4-PE (REA279, IgG1). Intracellular Foxp3 staining (mouse-anti-human, 236A/E7, IgG1, eFluor450-labeled) was performed with a Foxp3 staining kit as instructed (eBioscience, Vienna, Austria).
Based on the surface expression of CD45RA and intranuclear expression of Foxp3, two phenotypically and functionally distinct Treg subsets within the CD4+ T cell population could be distinguished (as shown by [17]): resting/naïve regulatory T cells (rTreg) were defined as CD4+ CD45RA+ Foxp3+ and activated/effector regulatory T cells (aTreg) as CD4+ CD45RA- Foxp3++. This gating strategy allowed us to exclude the activated non-suppressive effector T cells and analyze marker expression specifically within the Treg subsets. Natural Treg are defined as stable suppressive cells with a completely demethylated region in the FoxP3 gene. Within this population, resting/naïve Treg appear to be suppressive, but once activated can convert to activated/effector Treg with higher suppressive capacity [18]. The mean percentage of the respective human cell types and cell surface marker expression at day 0 is indicated in Table 1 and the used gating strategy is shown in S1 Fig.
For analysis of murine single cell suspensions, cells were stained with the monoclonal rat-anti-mouse antibodies CD4-V500 (RM4-5, IgG2a, BD Biosciences), CD25-PerCPCy5.5 (PC61.5, IgG1, eBioscience) and Armenian-hamster anti-mouse CD69-APC (H1.2F3, IgG, eBioscience). Intracellular Foxp3 staining (rat-anti-mouse, FJK-16s, IgG2a, eFluor450-labeled) was performed with a Foxp3 staining kit as instructed (eBioscience). Murine Treg were defined as CD4+ CD25+ Foxp3+ T cells.
Flow cytometry samples were measured on a Canto II (BD Biosciences) and analyzed using FlowJo software version 7.6.5 (Miltenyi Biotec).
Statistical analysis
Per time point, a delta percentage of the Treg frequency was calculated and all data are represented as mean delta ± SEM. For the human data, the delta was determined as the percentage of Treg at a specific time point subtracted by the percentage at day 0 for the same donor (= % Treg dayx—% Treg day0). In the case of the Engerix-B® trial, day0 = day168, the moment just before the third immunisation. Differences between 2 groups were determined with an unpaired, two-tailed Mann-Whitney test. Differences between 3 groups were determined with the Kruskal-Wallis test.
For mice, the delta was determined as the percentage Treg at a specific time point subtracted by the mean percentage of the mock-injected animals at that time point (= % Treg treatment dayx—average % Treg PBS dayx). Differences between 2 groups were determined with an unpaired two-tailed student’s t-test with Welch’s correction. Differences between 3 or more groups were determined with a one-way ANOVA (two-tailed) with Dunnett’s multiple comparison test.
Statistical analysis was performed using Prism 6 (GraphPad software). P < 0.05 was considered significant.
Results
Treg responses following vaccination in humans
To test whether vaccination leads to changes in the circulating Treg population, healthy individuals were i.m. or s.c. injected with a non-adjuvanted TIV (Agrippal®), a MF59®-adjuvanted TIV (Fluad®), an alum-adjuvanted hepatitis B vaccine (Engerix-B®), a live attenuated yellow fever vaccine (Stamaril®) or placebo. Treg frequency and characteristics were monitored right before and at different time points after vaccination.
Influenza
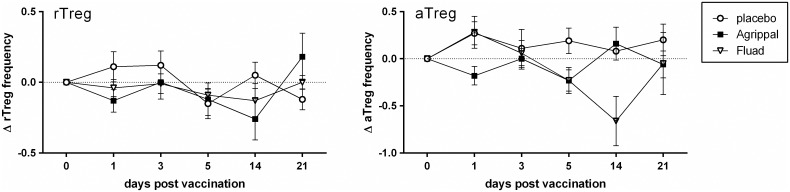
After vaccination with Agrippal® and Fluad®, we observed a small, but non-significant decrease in rTreg frequency shortly after vaccination (day 1) and also two weeks later (day 14) compared with placebo (Fig 2). During the first 5 dpv with Agrippal®, the aTreg frequency was slightly lower compared to placebo injection and equal to pre-vaccination values again around 14 dpv. Fluad® vaccination led to a decrease in aTreg frequencies at 5 and 14 dpv, though this did not reach statistical significance (Fig 2).
Fig 2. Effect of vaccination of humans with subunit influenza vaccines on Treg frequency.
At day 0, healthy adults were i.m. vaccinated with a non-adjuvanted (Agrippal®) or MF59®-adjuvanted (Fluad®) trivalent influenza subunit vaccine or injected with a placebo. At day 1, 3, 5, 14 and 21 post vaccination changes in Treg frequency were determined. The delta Treg percentage per time point was determined per donor (= % Treg dayx—% Treg day0). Mean (± SEM) delta percentage of the frequency of rTreg (left) and aTreg (right) in the blood at the different time points after vaccination with Agrippal® (n = 12), Fluad® (n = 8, day 14 n = 2) or placebo (n = 6). Means were statistically compared with a Kruskal-Wallis test.
To further dissect the characteristics within the Treg subpopulations, we analyzed the expression of several markers related to Treg functionality and migration (Table 1). After vaccination with Agrippal® and Fluad®, CD25 expression was lower (trend) on both rTreg (Figure A in S2 Fig) and aTreg (Figure B in S2 Fig) during the first 5 dpv compared to placebo injection. This was in contrast with the expression of CD39 and CCR7 on the rTreg subset, which was increased during this period (Figure A in S2 Fig). Compared with the placebo-injected group, vaccination with the influenza vaccines did not result in remarkable changes in the percentage of CD39+ or CCR7+ aTreg (Figure B in S2 Fig).
Taken together, vaccination with a non-adjuvanted or MF59®-adjuvanted subunit influenza vaccine only led to minor changes in rTreg and aTreg frequencies and characteristics, most of these shortly after vaccination.
Hepatitis B
As different vaccination strategies may result in different responses in the Treg population, we tested another frequently used subunit vaccine, the hepatitis B vaccine Engerix-B®, for its effect on Treg. This immunization requires a three-dose schedule to induce a protective antibody titer. Since antibody responses became only significantly measurable after the third dose, we decided to focus on changes in Treg frequency after this dose (day 168).
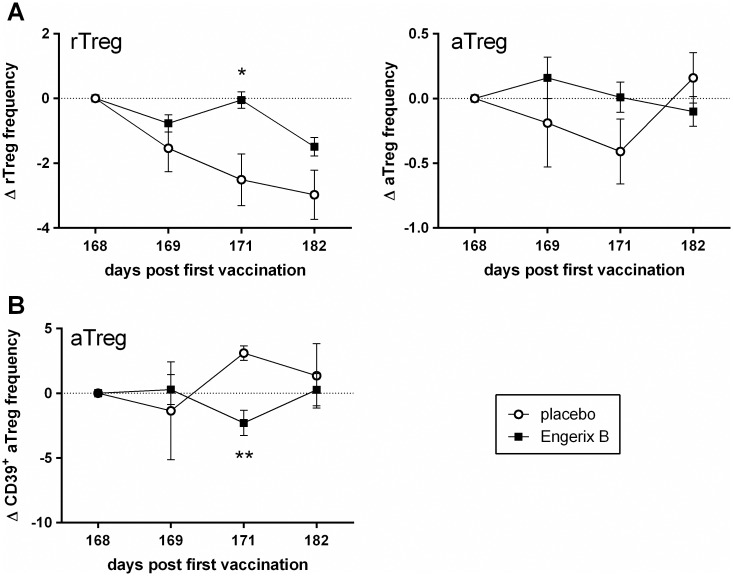
Vaccination with Engerix-B® led to an initial decrease in rTreg frequency, followed by a significant increase 3 dpv (day 171) compared with control participants. Hereafter, the frequency decreased again but it remained higher after Engerix-B® vaccination than placebo injection (Fig 3A). In contrast to rTreg, the frequency of the aTreg population increased the first day after Engerix-B® vaccination but was not statistically different from placebo (Fig 3A). In general, in the placebo group we observed a decrease in Treg frequency (both rTreg and aTreg).
Fig 3. Effect of vaccination of humans with a subunit hepatitis B vaccine on Treg frequency and characteristics.
At day 0, day 28 and day 168, healthy adults were i.m. vaccinated with Engerix-B® or injected with a placebo. At day 1, 3, and 14 after the third immunization dose (day 169, 171 and 182) changes in Treg frequency and phenotype were determined. The delta Treg percentage per time point was determined per donor (= % Treg dayx—% Treg day168). (A) Mean (± SEM) delta percentage of the frequency of rTreg (left) and aTreg (right) in the blood at the different time points after the third dose of Engerix-B® (n = 20) or placebo (n = 4). (B) Mean (± SEM) delta percentage of CD39 expression on aTreg after vaccination. Means were statistically compared with an unpaired, two-tailed Mann-Whitney test (* p < 0.05, ** p < 0.01, relative to placebo at the same time point).
Effect of Engerix-B® vaccination on Treg phenotype was most obvious in the aTreg population. In this population, expression of CD25 was first increased compared to placebo (day 169; trend), but then decreased again (day 171; Figure B in S3 Fig). Furthermore, CD31 appeared to be upregulated after vaccination (Figure B in S3 Fig), whereas CD39 (Fig 3B; significant) and HLA-DR (Figure B in S3 Fig; trend) both decreased during the first days after vaccination.
With respect to the rTreg population, no significant differences in surface marker expression between vaccinated and placebo-injected participants were observed (Figure A in S3 Fig). Nevertheless, an increase in CCR7 expression on rTreg was observed on the first day after vaccination compared to placebo which was followed by a decreased CCR7 expression (Figure A in S3 Fig; trend). A similar, though less pronounced effect of Engerix-B® was observed for CCR7 expression on aTreg (Figure B in S3 Fig).
Overall, hepatitis B immunization with a three-dose schedule of Engerix-B® resulted in significant increases in rTreg frequency as well as in significant changes in aTreg CD39 expression.
Yellow fever
Since live vaccines mimic a natural infection more closely than subunit vaccines, they may have a more pronounced effect on Treg. We therefore determined the frequency and surface marker expression on resting and activated Treg in yellow fever-naïve individuals before and in the first two weeks after vaccination with a live attenuated vaccine (Stamaril®).
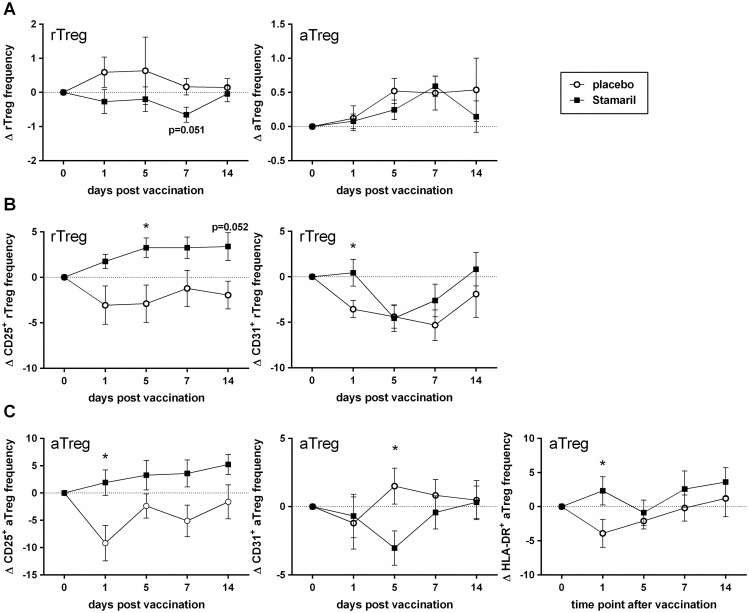
Compared to placebo injection, yellow fever vaccination led to a decrease in rTreg frequencies, which returned to the pre-vaccination values 14 dpv (Fig 4A). The aTreg showed an opposite trend, with an increase until 7 dpv and a return to the pre-vaccination values around 14 dpv (Fig 4A). The vaccine-induced changes in Treg frequency coincided with a significant increase in the expression of CD25 on rTreg as well as on aTreg (Fig 4B and 4C). Furthermore, HLA-DR expression on aTreg and CD31 expression on rTreg was significantly higher after Stamaril® vaccination compared to placebo injection (Fig 4B and 4C), but CD31 expression on aTreg significantly dipped at 5 dpv (Fig 4C). A (small) dip in frequency at day 5 was also observed for expression of HLA-DR and CD31 on rTreg and aTreg and for CCR4 and CCR7 on rTreg (Fig 4B and 4C and Figure A and B in S4 Fig).
Fig 4. Effect of vaccination of humans with a live attenuated yellow fever vaccine on Treg frequency and characteristics.
At day 0, healthy adults were s.c. vaccinated with Stamaril® or injected with a placebo. At day 1, 5, 7 and 14 post vaccination changes in Treg frequency and phenotype were determined. The delta Treg percentage per time point was determined per donor (= % Treg dayx—% Treg day0). (A) Mean (± SEM) delta percentage of the frequency of rTreg (left) and aTreg (right) in the blood at the different time points after vaccination with Stamaril® (n = 19) or placebo (n = 8). (B) Mean (± SEM) delta percentage of CD25 and CD31 expression on rTreg after vaccination. (C) Mean (± SEM) delta percentage of CD25, CD31 and HLA-DR expression on aTreg after vaccination. Means were statistically compared with an unpaired, two-tailed Mann-Whitney test (* p < 0.05 relative to placebo at the same time point).
At 14 dpv, when the frequency of rTreg in the peripheral blood had returned to normal, expression of CD39, CCR4 and CCR7 on the rTreg was increased in the vaccinated group compared to the placebo group (Figure A in S4 Fig). Vaccination with Stamaril® did not affect CCR4 or CCR7 expression on aTreg (Figure B in S4 Fig).
Taken together, our results revealed that administration of a live attenuated yellow fever vaccine induced changes in Treg frequencies and activation over time.
Treg responses following vaccination in mice
Since we could not determine the local effects of vaccination in humans, we analyzed the effects of anti-viral vaccination on CD4+ CD25+ Foxp3+ Treg in mice. For that purpose, mice were injected (i.m.) with the subunit vaccines TIV−, TIV+ and Engerix-B®. LPS, known to affect Treg, was included as positive control, as was the strong immunogenic adjuvant CFA [19,20].
Both in the dLN and in the spleen, LPS injection induced an increase in Treg frequency that was most evident at 3 and 7 dpv (Fig 5A and 5B). Injection of CFA, and, to a lesser extent, TIV+, TIV−and Engerix-B® resulted in a decrease in Treg frequency in the dLN at 3 dpv (Fig 5C), which was accompanied by a decrease in the expression of activation marker CD69 on Treg (S5 Fig). However, subsequently, from 7 to 14 dpv the Treg frequency in dLN after vaccination returned to levels similar or even higher than after mock injection. A systemic effect of immunization could be observed at 7 dpv, when the Treg frequency in the spleen was (significantly) increased for CFA and the three vaccines compared to mock-injected animals (Fig 5D). This was followed by the re-establishment of original Treg frequencies.
Fig 5. Effect of vaccination on local and systemic Treg frequency in mice.
At day 0, mice were i.m. injected with LPS, CFA or with one of the vaccines (TIV+, TIV- and Engerix-B®). Mock-injected animals received PBS. At day 3, 7, 14 and 21 post vaccination changes in Treg frequency were determined. The delta Treg percentage per time point was determined by comparing the treatment with the mean of PBS (= % Treg treatment dayx—average % Treg PBS dayx). The mean percentage Treg in PBS-injected mice was 10.9 ± 1.4% (dLN) and 12.0 ± 1.5% (spleen). N = 3–7 mice per group. (A-D) Mean (± SEM) delta percentage of Treg (CD4+ CD25+ Foxp3+) frequency at the different time points after vaccination were analyzed in dLN (A and C) and spleen (B and D) after LPS injection (A and B) and CFA or vaccine injection (C and D). Differences between PBS and LPS (A and B) were determined with an unpaired two-tailed student’s t-test with Welch’s correction. Differences between PBS and vaccines (C and D) were determined with a one-way ANOVA followed by Dunnett’s multiple comparisons test (* p < 0.05, ** p < 0.01, *** p < 0.001 relative to PBS at the same time point). TIV+: TIV supplemented with MF59® adjuvant; TIV-: TIV only; ENG: Engerix-B®
Thus, vaccination of mice resulted locally in an early, transient decrease in Treg frequency and activation, subsequently followed by a systemic Treg increase.
Discussion
In the current study, we have determined the effect of different anti-viral vaccinations on Treg responses. To the best of our knowledge, the present placebo-controlled study is the first in reporting this effect on the kinetics of frequency and characteristics of Treg subpopulations in healthy individuals.
We showed that vaccination of healthy individuals with a non-adjuvanted (Agrippal®) or MF59®-adjuvanted (Fluad®) influenza vaccine resulted only in minor changes in rTreg and aTreg frequencies, not significantly different from each other nor from placebo (Fig 2). Others have reported that vaccination with a different non-adjuvanted influenza vaccine also did not result in significant Treg frequency changes in healthy individuals, although significant increases were found in vaccinated rheumatoid arthritis patients in the first month following vaccination [21]. In contrast to vaccination, infection with an influenza virus was shown to increase Treg frequencies or absolute numbers in human peripheral blood and influenza A virus infection of mice induced a viral-specific Treg response locally as well as systemically that preceded the Teff response [22–25]. This shows that the influenza vaccines used in the current study have a much smaller effect on Treg than natural infections have.
Vaccination with another anti-viral subunit vaccine, Engerix-B®, did result in significant changes in Treg frequency. Compared to placebo, we found a significant increase in rTreg frequency at 3 dpv (day 171) after an initial decrease at 1 dpv (day 169) (Fig 3A). Other studies reported that in most cases hepatitis B vaccination or chronic HBV infection increased Treg frequencies in peripheral blood, potentially impairing vaccine effectiveness or viral clearance and reducing the response to treatment [8,26–31]. These studies, however, did not analyze frequency and marker expression within the different Treg subpopulations, except for the study from Mathew and colleagues [26]. This study found a negative correlation between the rTreg population and HBV-specific titres, although this was only found in hemodialysis patients and not in the healthy cohort. Nevertheless, this indicates that changes in Treg subpopulations are (at least in part) responsible for insufficiently protective immune responses following HBV vaccination, mainly in individuals with immune-related disorders. Of possible interest in this respect, studies have hypothesized relationships between HBV vaccination and autoimmunity (reviewed by Perricone and colleagues [32]).
The most obvious change in the aTreg population after Engerix-B® vaccination was a dip in CD39 expression at 3 dpv (day 171; Fig 3B). This finding may indicate a difference in Treg functionality or an efflux of CD39+ effector/memory-like Treg, as CD39 expression positively correlates with Foxp3 levels and is involved in the immune suppression during HBV infection [33–36]. Loss of activated cells could also explain the decrease in CD39+ Treg, as these effector cells are prone to apoptosis [18]. This, however, will need further investigation.
We also determined the effect of a live attenuated yellow fever vaccine on rTreg and aTreg. Our results show an activation of rTreg with potential conversion to aTreg. This is demonstrated by a significant increase of CD25 expression on rTreg (Fig 4B) and a decrease in frequency of this subpopulation (Fig 4A). Blom and colleagues [37] also found an increase in Treg activation after yellow fever vaccination and another study from Martins and colleagues [38] observed a decrease in Treg frequency, though both studies looked in a differently defined Treg population. Possibly, replication of the vaccine virus activated the rTreg that subsequently converted to aTreg with a potentially increased functionality (based on a trend towards higher CD39 expression, Figure B in S4 Fig) [18]. This indicates that the effects on Treg after vaccination with a live attenuated virus resemble more closely a natural infection than do the subunit vaccines.
Remarkably, all vaccines showed a trend of increased CCR7 expression on rTreg (S2, S3 and S4 Figs). This increase might be a common feature of vaccinations indicative of an influx of naïve (CD45RA+ CCR7+) rTreg that migrate between secondary lymphoid organs and peripheral blood [39,40]. Together with an increased expression of CCR4, especially after yellow fever vaccination (Figure A in S4 Fig), this would indicate that naïve rTreg that entered the peripheral blood were preparing for migration towards and interaction with activated antigen-presenting cells [38,41].
Phenotypic characterization of Treg after vaccination is a first step to analyze the effect of vaccination on Treg and functional assays would be of value in this work. However, we had to limit our analysis to phenotypic characterization for several reasons. In general, the % Treg in blood is low and ex vivo expansion of Treg to enhance the yield of Treg per donor was no option since Treg can change both phenotypically and functionally by culturing (personal experience and [42]). Furthermore, because of the set-up of this study, participants gave blood with a high frequency and thus were the drawn blood samples too small to yield sufficient Treg for such assays.
Local effects of vaccination are difficult to determine in humans and we therefore assessed this in mice. When i.m. injecting LPS, we observed transient local and systemic increases in Treg frequency (Fig 5A and 5B). This corresponds with the tuned suppression model: upon pathogenic encounter (and thus presence of TLR ligands), Teff expand and produce interleukin-2, which in turn induces Treg expansion [19]. Pathogenic clearance allows for suppression of Teff by the expanded Treg and while interleukin-2 levels go down, so do the (relative) Treg numbers [1,19].
In contrast to LPS injection, immunization with CFA, and to a lesser extent vaccination with the three subunit vaccines, led to a local dip in Treg frequencies in the dLN at 3 dpv, which was followed by a systemic increase in the spleen at 7 dpv (Fig 5C and 5D). This early local decrease in Treg frequency probably does not represent an actual decrease in Treg number, but rather is the result of a vaccination-induced influx of other cells (e.g. Teff, or neutrophils/monocytes) in the dLN [43,44]. Indeed, when we considered actual cell numbers in the dLN, we found an increase in total numbers of cells in the dLN at 3 and 7 dpv (Figure A in S6 Fig), corresponding to (small) increases in numbers of CD4+ T cells and also CD4+ CD25+ Treg (Figure B and C in S6 Fig). These local (and systemic) increases in Treg numbers roughly correspond with Treg responses after infection, e.g. sub-lethal influenza virus infection induces increases in Treg numbers in the dLN and spleen 5 days post infection [25].
Noteworthy, the systemic changes in Treg frequency found in mice were not identical to the human data. This may be caused by the fact that the human systemic Treg frequency was determined in blood and that of mice in the spleen or caused by interspecies differences in Treg definitions.
Concluding remarks
Although vaccines are usually regarded as mimics of infection, the present study has shown that inactivated (subunit) vaccines have only a minor effect on Treg frequencies, even in the presence of an adjuvant. The safe and widely used live attenuated vaccine closer resembled an infection with a more similar effect on frequency, activation and migration of the Treg. It therefore appears that Treg frequencies and phenotypes can fluctuate to a certain extent without causing a safety concern. However, to what extent vaccines also change Treg suppressive capacity and their characteristics will require further investigation, preferably in humans.
Supporting information
Representative flow cytometry plots of a placebo-injected individual to demonstrate gating strategy. This example belongs to a participant from the placebo group of the Stamaril trial (day0) and is representative for the overall gating. (A) In the fixed lymphocyte cell population, CD4+ T cells are selected and within this population rTreg (CD45RA+Foxp3+) and aTreg (CD45RA-Foxp3++) are defined. (B) Gating strategy of phenotypic marker expression on rTreg and aTreg for the markers CD25, CD39, CD31 (panel 1) and HLA-DR, CCR4 and CCR7 (panel 2). Gates were set on the CD45RA+Foxp3- non-Treg population and were subsequently placed on the rTreg and aTreg cell populations to determine the expression of these markers.
(TIF)
At day 0, healthy adults were i.m. vaccinated with a non-adjuvanted (Agrippal®) or MF59®-adjuvanted (Fluad®) trivalent influenza subunit vaccine or injected with a placebo. At day 1, 3, 5, 14 and 21 post vaccination changes in Treg frequency and phenotype were determined. The delta Treg percentage per time point was determined per donor (= % Treg dayx—% Treg day0). (A) Mean (± SEM) delta percentage of CD25, CD39 and CCR7 expression on rTreg after vaccination (top to bottom). (B) Mean (± SEM) delta percentage of CD25, CD39 and CCR7 expression on aTreg after vaccination (top to bottom). Means were statistically compared with a Kruskal-Wallis test.
(TIF)
At day 0, day 28 and day 168, healthy adults were i.m. vaccinated with Engerix-B® or injected with a placebo. At day 1, 3, and 14 after the third immunization dose (day 169, 171 and 182) changes in Treg frequency and phenotype were determined. The delta Treg percentage per time point was determined per donor (= % Treg dayx—% Treg day168). (A) Mean (± SEM) delta percentage of CD25, CD39, CD31, HLA-DR, CCR4 and CCR7 expression on rTreg after vaccination. (B) Mean (± SEM) delta percentage of CD25, CD31, HLA-DR, CCR4 and CCR7 expression on aTreg after vaccination. Means were statistically compared with an upaired, two-tailed Mann-Whitney test.
(TIF)
At day 0, healthy adults were s.c. vaccinated with Stamaril® or injected with a placebo. At day 1, 5, 7 and 14 post vaccination changes in Treg frequency and phenotype were determined. The delta Treg percentage per time point was determined per donor (= % Treg dayx—% Treg day0). (A) Mean (± SEM) delta percentage of CD39, HLA-DR, CCR4 and CCR7 expression on rTreg after vaccination. (B) Mean (± SEM) delta percentage of CD39, CCR4 and CCR7 expression on aTreg after vaccination. Means were statistically compared with an unpaired, two-tailed Mann-Whitney test.
(TIF)
At day 0, mice were i.m. injected with CFA or with one of the vaccines (TIV+, TIV- and Engerix-B®). Mock-injected animals received PBS. At day 3, 7, 14 and 21 post vaccination changes in CD69 expression on Treg were determined in the dLN. The delta CD69 percentage per time point was determined by comparing the treatment with the mean of PBS (= % CD69 treatment dayx—average %CD69 PBS dayx). The mean percentage CD69 in PBS-injected mice was 27.6 ± 4.5%. Mean (± SEM) delta percentage are indicated. N = 3–7 mice per group. Differences were determined with a one-way ANOVA followed by Dunnett’s multiple comparisons test (* p < 0.05, ** p < 0.01 relative to placebo at the same time point). TIV+: TIV supplemented with MF59® adjuvant; TIV-: TIV only; ENG: Engerix-B®.
(TIF)
At day 0, mice were i.m. injected with LPS, CFA or with one of the vaccines (TIV+, TIV- and Engerix-B®). Mock-injected animals received PBS. At day 3, 7, 14 and 21 post vaccination changes in numbers of (A) total cells, (B) CD4+ T cells and (C) Treg in the dLN were determined. The delta value per time point was determined by comparing the treatment with the mean of PBS (= number of cells (treatment) dayx—average number of cells (PBS) dayx). The mean number of cells in PBS-injected mice was 7.3x105 ± 3.7x105 (total cell numbers), 3.0x105 ± 1.6x105 (CD4+ T cells) and 3.3x105 ± 1.9x105 (Treg). Mean (± SEM) delta cell numbers are indicated. N = 3–7 mice per group. TIV+: TIV supplemented with MF59® adjuvant; TIV-: TIV only; ENG: Engerix-B®.
(TIF)
(PDF)
(PDF)
(PDF)
(DOC)
Abbreviations
- aTreg
activated regulatory T cell(s)
- CFA
Complete Freund’s Adjuvant
- dLN
draining lymph node(s)
- dpv
days post vaccination
- FBS
fetal bovine serum
- HBV
hepatitis B virus
- i.m.
intramuscular(ly)
- LPS
lipopolysaccharide
- NHS
normal human serum
- PBMC
peripheral blood mononuclear cell(s)
- rTreg
resting regulatory T cell(s)
- s.c.
subcutaneous(ly)
- Teff
effector T cell(s)
- TIV
trivalent influenza vaccine
- Treg
regulatory T cell(s)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was part of the BioVacSafe project. The BioVacSafe project has received support from the Innovative Medicines Initiative Joint Undertaking under grant agreement n° 115308, resources of which are composed of financial contribution from the European Union's Seventh Framework Programme (FP7/2007-2013) and EFPIA companies’ in kind contribution.
References
- 1.Liston A, Gray DHD. Homeostatic control of regulatory T cell diversity. Nat Rev Immunol. 2014;14: 154–165. doi: 10.1038/nri3605 [DOI] [PubMed] [Google Scholar]
- 2.Bacchetta R, Barzaghi F, Roncarolo M-. From IPEX syndrome to FOXP3 mutation: A lesson on immune dysregulation. Ann New York Acad Sci. 2016. doi: 10.1111/nyas.13011 [DOI] [PubMed] [Google Scholar]
- 3.Ramsdell F, Ziegler SF. FOXP3 and scurfy: How it all began. Nat Rev Immunol. 2014;14: 343–349. doi: 10.1038/nri3650 [DOI] [PubMed] [Google Scholar]
- 4.Sakaguchi S, Ono M, Setoguchi R, Yagi H, Hori S, Fehervari Z, et al. Foxp3+CD25+CD4+ natural regulatory T cells in dominant self-tolerance and autoimmune disease. Immunol Rev. 2006;212: 8–27. doi: 10.1111/j.0105-2896.2006.00427.x [DOI] [PubMed] [Google Scholar]
- 5.Oliphant S, Lines JL, Hollifield ML, Garvy BA. Regulatory T cells are critical for clearing influenza a virus in neonatal mice. Viral Immunol. 2015;28: 580–589. doi: 10.1089/vim.2015.0039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mangodt TC, Van Herck MA, Nullens S, Ramet J, De Dooy JJ, Jorens PG, et al. The role of Th17 and Treg responses in the pathogenesis of RSV infection. Pediatr Res. 2015;78: 483–491. doi: 10.1038/pr.2015.143 [DOI] [PubMed] [Google Scholar]
- 7.Rowe JH, Ertelt JM, Way SS. Foxp3 + regulatory T cells, immune stimulation and host defence against infection. Immunology. 2012;136: 1–10. doi: 10.1111/j.1365-2567.2011.03551.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dietze KK, Schimmer S, Kretzmer F, Wang J, Lin Y, Huang X, et al. Characterization of the Treg response in the hepatitis B virus hydrodynamic injection mouse model. PLoS ONE. 2016;11 doi: 10.1371/journal.pone.0151717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stross L, Günther J, Gasteiger G, Asen T, Graf S, Aichler M, et al. Foxp3+ regulatory T cells protect the liver from immune damage and compromise virus control during acute experimental hepatitis B virus infection in mice. Hepatology. 2012;56: 873–883. doi: 10.1002/hep.25765 [DOI] [PubMed] [Google Scholar]
- 10.Berod L, Puttur F, Huehn J, Sparwasser T. Tregs in infection and vaccinology: Heroes or traitors? Microb Biotechnol. 2012;5: 260–269. doi: 10.1111/j.1751-7915.2011.00299.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ndure J, Flanagan KL. Targeting regulatory T cells to improve vaccine immunogenicity in early life. Front Microbiol. 2014;5 doi: 10.3389/fmicb.2014.00477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nishikawa H, Sakaguchi S. Regulatory T cells in cancer immunotherapy. Curr Opin Immunol. 2014;27: 1–7. doi: 10.1016/j.coi.2013.12.005 [DOI] [PubMed] [Google Scholar]
- 13.Bayry J. Regulatory T cells as adjuvant target for enhancing the viral disease vaccine efficacy. VirusDisease. 2014;25: 18–25. doi: 10.1007/s13337-013-0187-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mills KH. Designer adjuvants for enhancing the efficacy of infectious disease and cancer vaccines based on suppression of regulatory T cell induction. Immunol Lett. 2009;122: 108–111. doi: 10.1016/j.imlet.2008.11.007 [DOI] [PubMed] [Google Scholar]
- 15.Lewis DJM, Lythgoe MP. Application of "systems Vaccinology" to Evaluate Inflammation and Reactogenicity of Adjuvanted Preventative Vaccines. J Immunol Res. 2015;2015 doi: 10.1155/2015/909406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Spensieri F, Siena E, Borgogni E, Zedda L, Cantisani R, Chiappini N, et al. Early rise of blood T follicular helper cell subsets and baseline immunity as predictors of persisting late functional antibody responses to vaccination in humans. PLoS ONE. 2016;11 doi: 10.1371/journal.pone.0157066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Miyara M, Yoshioka Y, Kitoh A, Shima T, Wing K, Niwa A, et al. Functional Delineation and Differentiation Dynamics of Human CD4+ T Cells Expressing the FoxP3 Transcription Factor. Immunity. 2009;30: 899–911. doi: 10.1016/j.immuni.2009.03.019 [DOI] [PubMed] [Google Scholar]
- 18.Sakaguchi S, Miyara M, Costantino CM, Hafler DA. FOXP3 + regulatory T cells in the human immune system. Nat Rev Immunol. 2010;10: 490–500. doi: 10.1038/nri2785 [DOI] [PubMed] [Google Scholar]
- 19.Walker LSK. Regulatory T cells overturned: The effectors fight back. Immunology. 2009;126: 466–474. doi: 10.1111/j.1365-2567.2009.03053.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Billiau A, Matthys P. Modes of action of Freund's adjuvants in experimental models of autoimmune diseases. J Leukocyte Biol. 2001;70: 849–860. [PubMed] [Google Scholar]
- 21.Salemi S, Picchianti-Diamanti A, Germano V, Donatelli I, Di Martino A, Facchini M, et al. Influenza vaccine administration in rheumatoid arthritis patients under treatment with TNFa blockers: Safety and immunogenicity. Clin Immunol. 2010;134: 113–120. doi: 10.1016/j.clim.2009.09.014 [DOI] [PubMed] [Google Scholar]
- 22.Guo X, Chen Y, Li X, Kong H, Yang S, Ye B, et al. Dynamic variations in the peripheral blood lymphocyte subgroups of patients with 2009 pandemic H1N1 swine-origin influenza A virus infection. Virol J. 2011;8 doi: 10.1186/1743-422X-8-215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Huang Y, Zhu W, Zeng X, Li S, Li X, Lu C. Innate and adaptive immune responses in patients with pandemic influenza A(H1N1)pdm09. Arch Virol. 2013;158: 2267–2272. doi: 10.1007/s00705-013-1692-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Giamarellos-Bourboulis EJ, Raftogiannis M, Antonopoulou A, Baziaka F, Koutoukas P, Savva A, et al. Effect of the novel influenza a (H1N1) virus in the human immune system. PLoS ONE. 2009;4 doi: 10.1371/journal.pone.0008393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Betts RJ, Prabhu N, Ho AWS, Lew FC, Hutchinson PE, Rotzschke O, et al. Influenza A virus infection results in a robust, antigen-responsive, and widely disseminated foxp3 + regulatory T cell response. J Virol. 2012;86: 2817–2825. doi: 10.1128/JVI.05685-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mathew RO, Mason DL, Song R, Tryniszewski T, Kennedy JS. Role of T-regulatory cells in the response to hepatitis B vaccine in hemodialysis patients. Hemodial Int. 2016;20: 242–252. doi: 10.1111/hdi.12326 [DOI] [PubMed] [Google Scholar]
- 27.Li J, Shi J, Ren W, Wu W, Chen Z. Regulatory role of CD4+CD25+Foxp3+ regulatory T cells on IL-17-secreting T cells in chronic hepatitis B patients. Dig Dis Sci. 2014;59: 1475–1483. doi: 10.1007/s10620-013-3022-1 [DOI] [PubMed] [Google Scholar]
- 28.Aalaei-Andabili SH, Alavian SM. Regulatory T cells are the most important determinant factor of hepatitis B infection prognosis: A systematic review and meta-analysis. Vaccine. 2012;30: 5595–5602. doi: 10.1016/j.vaccine.2012.06.063 [DOI] [PubMed] [Google Scholar]
- 29.El-Badawy O, Sayed D, Badary MS, Abd-Alrahman ME, El-Feky MA, Thabit AG. Relations of regulatory T cells with hepatitis markers in chronic hepatitis B virus infection. Hum Immunol. 2012;73: 335–341. doi: 10.1016/j.humimm.2012.01.014 [DOI] [PubMed] [Google Scholar]
- 30.Li J, Tan D, Liu H, Li K. CD4 + CD25 + FoxP3 + T regulatory cells in subjects responsive or unresponsive to hepatitis B vaccination. J Cent South Univ Med Sci. 2011;36: 1046–1051. doi: 10.3969/j.issn.1672-7347.2011.11.003 [DOI] [PubMed] [Google Scholar]
- 31.Miroux C, Vausselin T, Delhem N. Regulatory T cells in HBV and HCV liver diseases: Implication of regulatory T lymphocytes in the control of immune response. Expert Opin Biol Ther. 2010;10: 1563–1572. doi: 10.1517/14712598.2010.529125 [DOI] [PubMed] [Google Scholar]
- 32.Perricone C, Colafrancesco S, Mazor RD, Soriano A, Agmon-Levin N, Shoenfeld Y. Autoimmune/inflammatory syndrome induced by adjuvants (ASIA) 2013: Unveiling the pathogenic, clinical and diagnostic aspects. J Autoimmun. 2013;47: 1–16. doi: 10.1016/j.jaut.2013.10.004 [DOI] [PubMed] [Google Scholar]
- 33.Dwyer KM, Hanidziar D, Putheti P, Hill PA, Pommey S, McRae JL, et al. Expression of CD39 by human peripheral blood CD4+CD25 + T cells denotes a regulatory memory phenotype. Am J Transplant. 2010;10: 2410–2420. doi: 10.1111/j.1600-6143.2010.03291.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Deaglio S, Dwyer KM, Gao W, Friedman D, Usheva A, Erat A, et al. Adenosine generation catalyzed by CD39 and CD73 expressed on regulatory T cells mediates immune suppression. J Exp Med. 2007;204: 1257–1265. doi: 10.1084/jem.20062512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Borsellino G, Kleinewietfeld M, Di Mitri D, Sternjak A, Diamantini A, Giometto R, et al. Expression of ectonucleotidase CD39 by Foxp3+ Treg cells: Hydrolysis of extracellular ATP and immune suppression. Blood. 2007;110: 1225–1232. doi: 10.1182/blood-2006-12-064527 [DOI] [PubMed] [Google Scholar]
- 36.Tang Y, Jiang L, Zheng Y, Ni B, Wu Y. Expression of CD39 on FoxP3 + T regulatory cells correlates with progression of HBV infection. BMC Immunol. 2012;13 doi: 10.1186/1471-2172-13-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Blom K, Braun M, Ivarsson MA, Gonzalez VD, Falconer K, Moll M, et al. Temporal dynamics of the primary human T cell response to yellow fever virus 17D as it matures from an effector- to a memory-type response. J Immunol. 2013;190: 2150–2158. doi: 10.4049/jimmunol.1202234 [DOI] [PubMed] [Google Scholar]
- 38.Martins MÂ, Silva ML, Marciano APV, Peruhype-Magalhães V, Eloi-Santos SM, Ribeiro JGL, et al. Activation/modulation of adaptive immunity emerges simultaneously after 17DD yellow fever first-time vaccination: Is this the key to prevent severe adverse reactions following immunization? Clin Exp Immunol. 2007;148: 90–100. doi: 10.1111/j.1365-2249.2006.03317.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Valmori D, Merlo A, Souleimanian NE, Hesdorffer CS, Ayyoub M. A peripheral circulating compartment of natural naive CD4+ Tregs. J Clin Invest. 2005;115: 1953–1962. doi: 10.1172/JCI23963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sallusto F, Lenig D, Förster R, Lipp M, Lanzavecchia A. Two subsets of memory T lymphocytes with distinct homing potentials and effector functions. Nature. 1999;401: 708–712. doi: 10.1038/44385 [DOI] [PubMed] [Google Scholar]
- 41.Iellem A, Mariani M, Lang R, Recalde H, Panina-Bordignon P, Sinigaglia F, et al. Unique chemotactic response profile and specific expression of chemokine receptors CCR4 and CCR8 by CD4+CD25+ regulatory T cells. J Exp Med. 2001;194: 847–853. doi: 10.1084/jem.194.6.847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Marek N, Bieniaszewska M, Krzystyniak A, Juscinska J, Mysliwska J, Witkowski P, et al. The time is crucial for ex vivo expansion of t regulatory cells for therapy. Cell Transplant. 2011;20: 1747–1758. doi: 10.3727/096368911X566217 [DOI] [PubMed] [Google Scholar]
- 43.Hopf S, Garner-Spitzer E, Hofer M, Kundi M, Wiedermann U. Comparable immune responsiveness but increased reactogenicity after subcutaneous versus intramuscular administration of tick borne encephalitis (TBE) vaccine. Vaccine. 2016;34: 2027–2034. doi: 10.1016/j.vaccine.2015.12.057 [DOI] [PubMed] [Google Scholar]
- 44.Leliefeld PHC, Koenderman L, Pillay J. How neutrophils shape adaptive immune responses. Front Immunol. 2015;6 doi: 10.3389/fimmu.2015.00471 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Representative flow cytometry plots of a placebo-injected individual to demonstrate gating strategy. This example belongs to a participant from the placebo group of the Stamaril trial (day0) and is representative for the overall gating. (A) In the fixed lymphocyte cell population, CD4+ T cells are selected and within this population rTreg (CD45RA+Foxp3+) and aTreg (CD45RA-Foxp3++) are defined. (B) Gating strategy of phenotypic marker expression on rTreg and aTreg for the markers CD25, CD39, CD31 (panel 1) and HLA-DR, CCR4 and CCR7 (panel 2). Gates were set on the CD45RA+Foxp3- non-Treg population and were subsequently placed on the rTreg and aTreg cell populations to determine the expression of these markers.
(TIF)
At day 0, healthy adults were i.m. vaccinated with a non-adjuvanted (Agrippal®) or MF59®-adjuvanted (Fluad®) trivalent influenza subunit vaccine or injected with a placebo. At day 1, 3, 5, 14 and 21 post vaccination changes in Treg frequency and phenotype were determined. The delta Treg percentage per time point was determined per donor (= % Treg dayx—% Treg day0). (A) Mean (± SEM) delta percentage of CD25, CD39 and CCR7 expression on rTreg after vaccination (top to bottom). (B) Mean (± SEM) delta percentage of CD25, CD39 and CCR7 expression on aTreg after vaccination (top to bottom). Means were statistically compared with a Kruskal-Wallis test.
(TIF)
At day 0, day 28 and day 168, healthy adults were i.m. vaccinated with Engerix-B® or injected with a placebo. At day 1, 3, and 14 after the third immunization dose (day 169, 171 and 182) changes in Treg frequency and phenotype were determined. The delta Treg percentage per time point was determined per donor (= % Treg dayx—% Treg day168). (A) Mean (± SEM) delta percentage of CD25, CD39, CD31, HLA-DR, CCR4 and CCR7 expression on rTreg after vaccination. (B) Mean (± SEM) delta percentage of CD25, CD31, HLA-DR, CCR4 and CCR7 expression on aTreg after vaccination. Means were statistically compared with an upaired, two-tailed Mann-Whitney test.
(TIF)
At day 0, healthy adults were s.c. vaccinated with Stamaril® or injected with a placebo. At day 1, 5, 7 and 14 post vaccination changes in Treg frequency and phenotype were determined. The delta Treg percentage per time point was determined per donor (= % Treg dayx—% Treg day0). (A) Mean (± SEM) delta percentage of CD39, HLA-DR, CCR4 and CCR7 expression on rTreg after vaccination. (B) Mean (± SEM) delta percentage of CD39, CCR4 and CCR7 expression on aTreg after vaccination. Means were statistically compared with an unpaired, two-tailed Mann-Whitney test.
(TIF)
At day 0, mice were i.m. injected with CFA or with one of the vaccines (TIV+, TIV- and Engerix-B®). Mock-injected animals received PBS. At day 3, 7, 14 and 21 post vaccination changes in CD69 expression on Treg were determined in the dLN. The delta CD69 percentage per time point was determined by comparing the treatment with the mean of PBS (= % CD69 treatment dayx—average %CD69 PBS dayx). The mean percentage CD69 in PBS-injected mice was 27.6 ± 4.5%. Mean (± SEM) delta percentage are indicated. N = 3–7 mice per group. Differences were determined with a one-way ANOVA followed by Dunnett’s multiple comparisons test (* p < 0.05, ** p < 0.01 relative to placebo at the same time point). TIV+: TIV supplemented with MF59® adjuvant; TIV-: TIV only; ENG: Engerix-B®.
(TIF)
At day 0, mice were i.m. injected with LPS, CFA or with one of the vaccines (TIV+, TIV- and Engerix-B®). Mock-injected animals received PBS. At day 3, 7, 14 and 21 post vaccination changes in numbers of (A) total cells, (B) CD4+ T cells and (C) Treg in the dLN were determined. The delta value per time point was determined by comparing the treatment with the mean of PBS (= number of cells (treatment) dayx—average number of cells (PBS) dayx). The mean number of cells in PBS-injected mice was 7.3x105 ± 3.7x105 (total cell numbers), 3.0x105 ± 1.6x105 (CD4+ T cells) and 3.3x105 ± 1.9x105 (Treg). Mean (± SEM) delta cell numbers are indicated. N = 3–7 mice per group. TIV+: TIV supplemented with MF59® adjuvant; TIV-: TIV only; ENG: Engerix-B®.
(TIF)
(PDF)
(PDF)
(PDF)
(DOC)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.