Abstract
Corticotropin releasing hormone (CRH) produced by the hypothalamus initiates the hypothalamic-pituitary-adrenal (HPA) axis, which regulates the body’s stress response. CRH levels typically are undetectable in human plasma, but during pregnancy the primate placenta synthesizes and releases large amounts of CRH into both maternal and fetal circulations. Notably, placental CRH synthesis increases in response to maternal stress signals. There is evidence that human fetal exposure to high concentrations of placental CRH is associated with behavioral consequences during infancy and into childhood, however the direct effects on of the peptide on the human brain are unknown. In this study, we used a rodent model to test the plausibility that CRH has direct effects on the developing cortex. Because chronic exposure to CRH reduces dendritic branching in hippocampal neurons, we tested the hypothesis that exposure to CRH would provoke impoverishment of dendritic trees in cortical neurons. This might be reflected in humans as cortical thinning. We grew developing cortical neurons in primary cultures in the presence of graded concentrations of CRH. We then employed Sholl analyses to measure dendritic branching and total dendritic length of treated cells. A seven-day exposure to increasing levels of CRH led to a significant, dose-dependent impoverishment of the branching of pyramidal-like cortical neurons. These results are consistent with the hypothesis that, rather than merely being a marker of prenatal stress, CRH directly decreases dendritic branching. Because dendrites comprise a large portion of cortical volume these findings might underlie reduced cortical thickness and could contribute to the behavioral consequences observed in children exposed to high levels of CRH in utero.
Introduction
Corticotropin-releasing hormone (CRH), a hypothalamic, 41-amino acid neuropeptide, has a major role in regulating pituitary–adrenal function and biological responses to stress [1–6]. The expression of CRH in stress-sensitive hypothalamic neurons commences during fetal life [7–9], and the peptide contributes to the regulation of the response to stress throughout life. In addition to expression and function within the hypothalamus, CRH is expressed in select brain regions [10,11], and CRH receptors are distributed throughout the brain [12,13]. During stress, the peptide is released locally within the amygdala [14], hippocampus [15], and cortex [16], and contributes to the diverse effects of stress on brain functions, including memory and anxiety. Thus, during acute stress, CRH enhances memory through actions in the amygdala [14] and hippocampus [17]. However, exposure to high levels of CRH, or a chronic exposure to lower levels may have adverse effects throughout life, because the peptide reduces the number of neuronal synapses by disrupting the structure of dendritic spines [18,19]. During aging, CRH may also contribute to the pathology associated with dementia, including Alzheimer’s Disease [20,21]. Developing neurons are particularly sensitive to CRH. Indeed, exposure to nanomolar levels of the peptide results in neuronal hyper-excitability [22], increased risk for seizures, and even neuronal death [23,24].
There is experimental information about the role of brain-derived CRH during development; however, there is little known about the potential role of placental-derived, maternal CRH on brain maturation in the developing fetus. Rodent placenta does not seem to synthesize CRH. In contrast, during the course of human pregnancy the placenta expresses CRH as early as the seventh week of gestation [25]. This results in an exponential (20- to 40-fold) increase in CRH levels in maternal and fetal circulation over the course of human gestation. Placental CRH (pCRH) is identical to hypothalamic CRH, and it is believed that CRH contributes to organization of the fetal nervous system, regulates fetal maturation [26], and influences the timing of birth [27,28]. In the human, maternal signals of stress (e.g. increased cortisol) is associated with augmented synthesis of pCRH that is released into both maternal and fetal compartments.
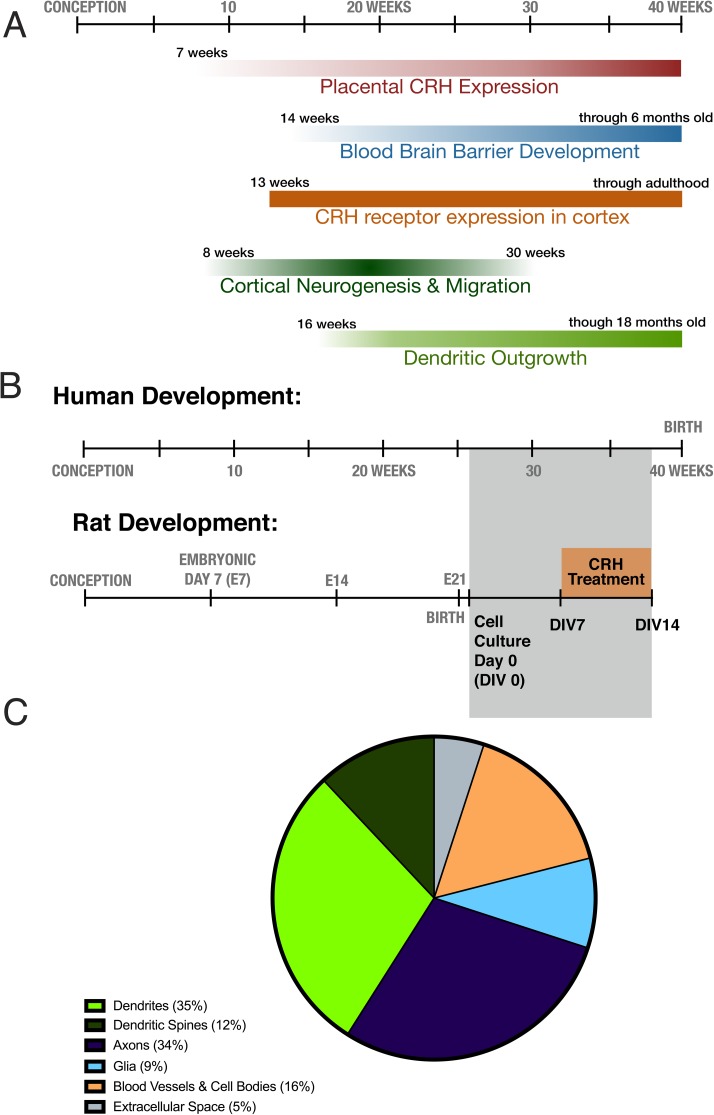
An association has been found between fetal exposure to elevated level of CRH and childhood outcomes. For example, increased pCRH exposure has been correlated with internalizing symptoms in children [29,30], but how CRH promotes these outcomes is unclear. The peptide might mainly function via influencing glucocorticoids and other mediators; alternatively, CRH may directly influence the development and maturation of brain cells, including neurons. This question is important: in addition to mechanistic understanding of human brain development, it may open therapeutic opportunities. Here, we query if, in addition to being a marker of prenatal stress, CRH exposure during periods of cortical neuronal development and growth might directly stunt the dendritic trees of rodent cortical neurons (Fig 1A). Using an in vitro model, we find a deleterious, dose-dependent effect of CRH on the development of cortical neurons, at a developmental period approximating human developmental stages when pCRH levels are maximal (Fig 1B). CRH led to poor development of dendritic trees, which constitute ~45% of cortical volume [31] (Fig 1C) and are essential for anchoring excitatory synapses, the basis of normal neuronal function. Thus, CRH-mediated mal-development of vital cortical structures may contribute to the mechanisms by which prenatal adversity may influence human neuropsychiatric outcome.
Fig 1. The relative timing and cortical volume impacts of CRH on dendritic growth in the fetus.
A) The relative timing of placental CRH expression, blood brain barrier development, cortical CRH expression, and cortical neurogenesis, migration and dendritic outgrowth in human gestation [25,32–34]. B) Relative human and rat cortical neuronal development. The relative timing of the cell culture experiment and treatment with CRH is indicated by the grey and orange boxes, respectively. C) Contribution of different cell types and structures to cortical volume. Based on data from Braitenberg & Schüz (1998).
Methods
All animal experiments conformed to National Institutes of Health guidelines and were approved by the Institutional Animal Care and Use Committee of the University of California-Irvine.
The detailed protocol has been listed for independent citation at protocols.io [35].
Primary cortical neuron cultures
Timed-pregnant Sprague-Dawley rat dams gave birth in the University of California-Irvine vivarium. Three independent experiments were conducted: Cortical neuron cultures were prepared within 36 hours after birth (P0-P1) from pups of either sex as previously described [36,37]. Briefly, motor cortices were dissected and incubated in dissection solution (137 mM NaCl, 5.4 mM KCl, 0.17 mM Na2PO4, 0.22 mM KH2PO4, 33.3 mM D-glucose, and 43.8 mM sucrose in 9.9 mM HEPES pH = 7.4) with 10 U/mL papain (Worthington, Lakewood, NJ). After removal of papain, cells were triturated and plated at a density of 400–600 cell/mm2 on 12 mm coverslips (Thermo Fisher, Houston, TX) pre-coated with poly-D-lysine (Sigma, St. Louis, MO). Cultures were initially maintained in Basal Medium Eagle (BME) with fetal bovine serum, sodium pyruvate, and L-alanyl-L-glutamine (GlutaMAX; Invitrogen, Grand Island, NY) at 36°C and 5% CO2. After 2 hours, half the culture medium was replaced with Neurobasal Medium (Invitrogen) pre-conditioned for 24 hours over 1-3-week-old glial cell culture (conditioned medium), and then half of the conditioned medium was refreshed after 2 more hours. Cultures were treated with 1μM arabinoside-cytosine (Sigma) on day in vitro 3 (DIV3) to inhibit glial proliferation and refreshed twice a week with conditioned medium.
Corticotropin Releasing Hormone (CRH) (Bachem, King of Prussia, PA) was added to the medium on the 7th day in vitro (DIV7) and refreshed on DIV10. Neurons were exposed for a total of one week to levels of CRH at 0.01, 0.1, 1, 10, or 100 nM. Cultured neurons were fixed using fresh 4% paraformaldehyde (PFA) on DIV14.
Immunocytochemistry (ICC) for MAP2
Neurons were washed in 0.1 M phosphate buffer (PB) for 1 minute and then fixed with ice-cold 4% paraformaldehyde in 0.1M PB pH = 7.4 for 1 hour. They were then washed quickly in phosphate-buffered saline + Triton-X (PBS-T) and treated with a blocking buffer (3% NGS, 1% BSA, 0.3% Triton-X in 0.01 M PBS, pH = 7.4) for 30 minutes. Coverslips were treated with mouse anti-MAP2 antibody (Sigma) diluted 1:10,000 in 0.3% Triton-X in 0.01 M PBS at 4°C for 48 hours. Finally, they were washed 3 times in PBS-T (5 minutes/wash) and then incubated in AlexaFluor488 goat anti-mouse IgG conjugate at a concentration of 1:400 (Invitrogen, Grand Island, NY) in 0.3% PBS-T with 1% BSA at room temperature for 2 hours. After washing for 5 minutes in PBS-T 3 more times, neurons were processed for confocal imaging with aqueous mounting medium (Gel-Mount; Biomeda, Foster City, CA) to protect against photo-bleaching.
Systematic imaging and analysis of dendritic length and arborization (Sholl analysis)
All coverslips were assessed and quantified without knowledge of treatment group. Each experiment included 12 coverslips per treatment group, and neurons were sampled equally from each coverslip for imaging. To objectively select neurons, each coverslip was imaged at lower resolution in four locations: a 1mm x 1mm square was 90° apart from each other and exactly 1 mm from the cover slip edge. These locations were selected in advance to obviate the potential confounder of high density of neurons and confluence of processes. All neurons with cell bodies within each 1mm x 1mm region and touching at least two neighboring neurons were imaged using confocal microscopy, Zeiss LSM 510 (Oberkochen, Germany). Images were taken using a 20x objective with 2x digital zoom. Overlapping images were stitched together using Fiji ImageJ (U.S. NIH, Bethesda, MD, USA) [38]. To limit the analyses to pyramidal-like neurons, somata were traced and fit to an ellipse, and the major and minor axes of the ellipse were measured. Neurons with a minor axis/major axis ratio of <0.5 were considered presumed interneurons and excluded from analysis. Dendrites of all remaining neurons that could be differentiated from the dendrites of neighboring neurons were manually traced and analyzed using the Simple Neurite Tracer plug-in [39]. Final n per group were 0 nM = 35; 0.1 nM = 24; 1.0 nM = 26, 10 nM = 30; 100 nM = 21. For total dendritic branching, two outliers in the 10 nM group (n = 30) were excluded using ROUT outlier method, with a false discovery rate of 5% [40]. No other group had outliers.
Results
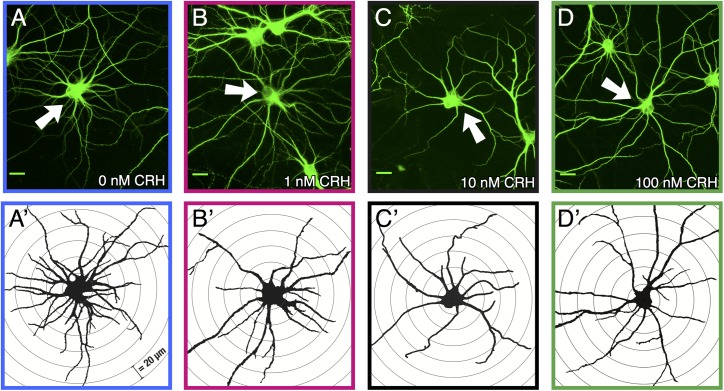
These experiments were designed to probe the plausibility of a direct causal role of CRH in mediating the effects of prenatal exposure to high levels of placental CRH on neuronal arborization and maturation that contributes to behavioral outcomes [29]. To this end, we used rat primary cortical cell culture, an in vitro model of neuronal development. Primary cell culture allows for the detailed analysis of neuronal dendrites from a neonatal rat, analogous, in terms of cortical development, to the 3rd trimester in humans [41]. Neurons were exposed to chronic levels of CRH at 0.01, 0.1, 1, 10, and 100 nM for 7 days of treatment. Fig 2A–2D depicts representative neurons and Fig 2A’–2D’ are Sholl drawings of the same neurons (concentric circles at 20 μm distances). Sholl drawings are used measure dendritic branching, comparing the number of dendrites at varying distances from the soma.
Fig 2. Images of cortical neurons treated with varying levels of CRH.
A-D: 40x images of representative neurons exposed to 0, 1, 10, 100 nM CRH respectively. Scale bar is 20 μm. A’-D’: Traces of the same cells in A-D and concentric Sholl circles spaced 20 μm apart.
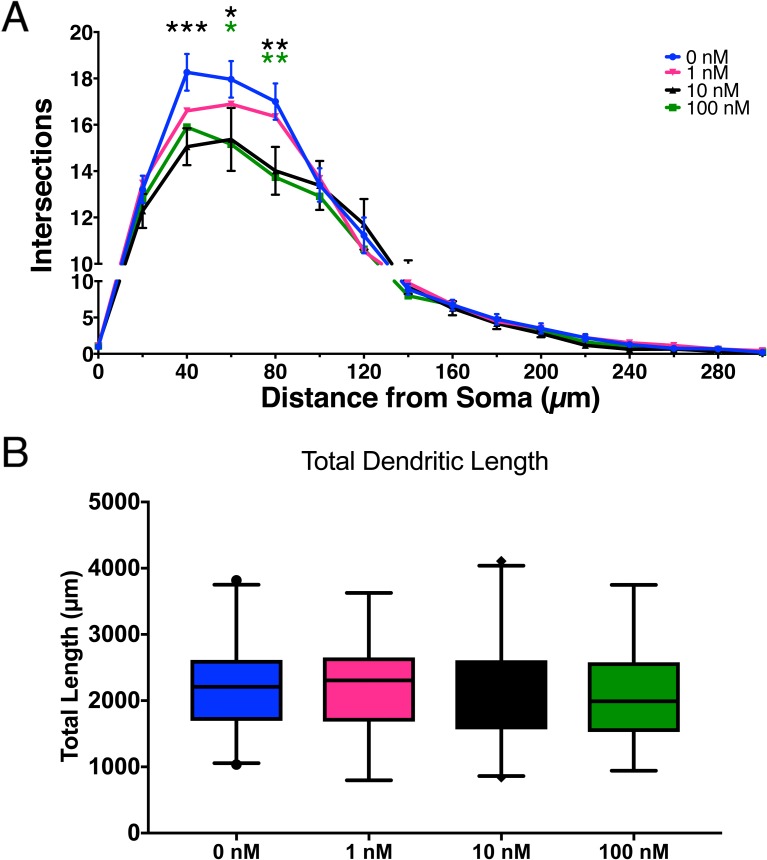
Chronic exposure to CRH led to a reduction in the dendritic branching of pyramidal-like neurons (Fig 3A). The effect was maximal at 40–80 μm from the soma (two-way ANOVA, Bonferroni correction for multiple comparisons, P<0.05). A dose effect was apparent at low concentrations but was not seen above 10 nM concentrations. Total dendritic branch length was also analyzed, but there were no significant differences found between treatment groups (Fig 3B) (one-way ANOVA, Bonferroni correction for multiple comparisons, p = 0.68). Dendritic branching is one of the components that drive dendritic length. Our data suggest that high levels of CRH likely inhibit the branching points of dendrites, probably by eliminating synaptic connections from other neurons, analogous to the known effects of the peptide [18]. Linear growth of dendrites and branches is not affected, and likely mitigates the overall effects on dendritic length
Fig 3. CRH exposure of developing cortical neurons influences dendritic branching, but not total dendritic length.
A) Sholl analysis reveals the dose-dependent effects comparing varying levels of CRH. Significant decreases were found at 40 μm from the soma (10 nM, p = 0. 0006), 60 μm (10 nM, p = 0.009; 100 nM p = 0.014), and 80 μm (10 nM, p = 0.0017, 100 nM, p = 0025). Error bars represent SEM. B) Total combined dendritic length was not different between groups. (Error bars represent SEM. B) Total combined dendritic length was not different between groups Error bars represent 2.5–97.5 percentiles on box and whisker plots. For both figures, 0.01 nM and 0.1 nM had no significant effects and are not shown.
Discussion
The principal findings of this paper are (1) cortical neurons at the developmental stage roughly concordant with late human gestation are sensitive to CRH; (2) CRH influences dendritic branching in a dose-dependent manner. Importantly, these effects are observed at CRH levels estimated to be present in the adult stressed brain [42].
Cortical pyramidal neurons are exposed to both local CRH, expressed in cortical interneurons [43] and potentially to CRH from other brain regions and circulating blood. Levels of CRH are low to undetectable in human blood, except during pregnancy when the human placenta produces large amounts of pCRH and releases it into both maternal and fetal circulation [44–46]. CRH produced by the placenta travels into the umbilical vein and enters fetal blood, and may thus reach the developing fetus [47]. Fetal plasma CRH levels throughout gestation are correlated with maternal plasma levels [48], stimulating the fetal pituitary to synthesize adrenocorticotropic hormone (ACTH) and drive fetal adrenal cortisol synthesis [47]. Once CRH enters the fetal circulation, it can also cross the blood brain barrier [33]. Thus, CRH has the potential to directly influence developing cortical neurons in the fetus.
Both the primate [49] and murine [12,13] cortex widely express CRH receptors, and those receptors can be found in fetal human neural stem/progenitor cells and in differentiated cortical neurons as early as 13 gestational week [32]. CRH at levels studied here has been found to directly influence the development of hippocampal neurons, including dendritic differentiation [18,50]. Although placental CRH is poised to influence cortical neurons as well, the direct effect of CRH on the structural development of cortical neurons had not been studied previously either in vivo or in vitro. The current study found that exposure to CRH directly reduces dendritic branching of pyramidal-like cortical neurons, indicating that the levels of this maternal stress hormone during fetal development likely mechanistically regulate the structure of the cortex.
In the current study, cortical neurons were exposed to chronic CRH at varying levels. There is little direct information about levels of CRH that bathe the developing human cortex. In the human cohort that our team has studied, we found maternal blood levels of placental CRH can reach as high as 3000 pg/mL (0.6 nM) [51], which approaches the levels that decreased dendritic branching. In our experiment, cortical neurons were only exposed to CRH for 7 days in vitro, while human fetal cortical neurons are exposed for months, allowing for more significant impacts. Additionally, CRH can cross even the developed blood brain barrier and may accumulate in fetal brain [33]. Finally, fetal cortical neurons are also exposed to endogenous CRH that is produced within fetal brain and has combined effects with placental CRH [52].
Here, the adverse actions of CRH on cortical neurons were only observed at higher levels tested. This is important, because all fetuses are exposed to pCRH as a normal part of gestation. The dose-dependent actions of CRH indicate that adverse cortical neuronal maturation will be limited to fetuses exposed to relatively high levels of pCRH.
Several negative effects of high levels of CRH on the developing brain have been demonstrated in rodents. The peptide increases neuronal excitability [22], promoting seizures and even neuronal death at high levels [23]. Whereas existing work has shown adverse actions of the peptide in hippocampus [22,50] and amygdala [22,53], this is the first report of untoward actions of CRH on the developing cortex. It is interesting to note that direct effects of CRH on the developing organism are found throughout evolution (1). For example, CRH is expressed in the Western spadefoot toad, which lays its eggs in pools of desert rainwater. If tadpoles detect that the conditions for normal development are unfavorable (e.g. rapid evaporation of the pool), CRH accumulates in the hypothalamus, promoting metamorphosis and escape from imminent peril. Notably, here, too there are adverse effects of high levels of CRH: tadpoles that survive by accelerating their development are smaller than average at emergence as toads and have reduced capacity to forage for food and to mate (2,3).
Placental CRH production increases in response to maternal signals of stress which is associated with maternal glucocorticoid (cortisol) production. In the hypothalamus, glucocorticoids inhibit CRH transcription providing a negative feedback during stress. Surprisingly, in the placenta, cortisol promotes production and release of pCRH [54], constituting a ‘positive feedback’ system. Thus, relatively high levels of cortisol and of CRH may both be present in the stressed pregnant mother [25,55], and steroids and pCRH can act synergistically to change neuronal structure [56]. The current work reveals for the first time that CRH alone suffices to alter neuronal development by stunting dendritic branching. Namely, the peptide is not merely a marker of stress or other conditions influencing fetal neuronal maturation via CRH-independent mechanisms. These effects of the peptide are important, because neuronal dendritic arbors form the bulk of cortical volume [31,57]; thus, changes in dendrites are likely to be reflected as measurable changes in cortical structure and function. Taken together, these data indicate that direct actions of CRH on cortical neuron maturation may provide a novel mechanism by which prenatal maternal signals have a lifelong effect on the neuropsychiatric outcome of her child.
Supporting information
(XLSX)
Acknowledgments
Supported by National Institute of Health awards P50 MH096889 (TZB, LMG, EPD), Eunice Kennedy Shriver National Institute of Child Health and Human Development through HD51852 and HD28413 (CAS); HD50662 and HD065823 (EPD); HD40967 (LMG), National Institute of Neurological Disorders and Stroke through NS41298 (CAS), T32 NS045540 (TZB/MMC), NS28912 (TZB), National Institute of General Medical Sciences through T32GM08620 (MMC). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The assistance of Claudia Buss and Mariann Howland is gratefully acknowledged.
Data Availability
All relevant data are within the paper and Supporting Information files.
Funding Statement
Supported by National Institute of Health awards P50 MH096889 (TZB, LMG, EPD). Eunice Kennedy Shriver National Institute of Child Health and Human Development through HD51852 and HD28413 (CAS); HD50662 and HD065823 (EPD); HD40967 (LMG), National Institute of Neurological Disorders and Stroke through NS41298 (CAS) T32 NS045540 (TZB/MMC), NS28912 (TZB). National Institute of General Medical Sciences through T32GM08620 (MMC). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Vale W, Spiess J, Rivier C, Rivier J. Characterization of a 41-residue ovine hypothalamic peptide that stimulates secretion of corticotropin and beta-endorphin. Science (80-). 1981. September 18;213(4514):1394–7. [DOI] [PubMed] [Google Scholar]
- 2.Bale TL, Vale WW. CRF AND CRF R ECEPTORS: Role in Stress Responsivity and Other Behaviors. Annu Rev Pharmacol Toxicol. 2004. February 10;44(1):525–57. [DOI] [PubMed] [Google Scholar]
- 3.Herman JP, McKlveen JM, Ghosal S, Kopp B, Wulsin A, Makinson R, et al. Regulation of the Hypothalamic-Pituitary-Adrenocortical Stress Response In: Comprehensive Physiology. Hoboken, NJ, USA: John Wiley & Sons, Inc.; 2016. p. 603–21. doi: 10.1002/cphy.c150015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Deussing J, Chen A, Dedic N. The CRF family of neuropeptides and their receptors—mediators of the central stress response. Curr Mol Pharmacol. 2017. March 2;10(999):1–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Regev L, Baram TZ. Corticotropin releasing factor in neuroplasticity. Front Neuroendocrinol. 2014. April;35(2):171–9. doi: 10.1016/j.yfrne.2013.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Joëls M, Baram TZ. The neuro-symphony of stress. Nat Rev Neurosci. 2009. April 2;10(6):459–66. doi: 10.1038/nrn2632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Keegan CE, Herman JP, Karolyi IJ, O’Shea KS, Camper SA, Seasholtz AF. Differential expression of corticotropin-releasing hormone in developing mouse embryos and adult brain. Endocrinology. 1994. June;134(6):2547–55. doi: 10.1210/endo.134.6.8194481 [DOI] [PubMed] [Google Scholar]
- 8.Baram TZ, Lerner SP. Ontogeny of corticotropin releasing hormone gene expression in rat hypothalamus—comparison with somatostatin. Int J Dev Neurosci. 1991;9(5):473–8. [DOI] [PubMed] [Google Scholar]
- 9.Grino M, Young WS, Burgunder JM. Ontogeny of expression of the corticotropin-releasing factor gene in the hypothalamic paraventricular nucleus and of the proopiomelanocortin gene in rat pituitary. Endocrinology. 1989. January;124(1):60–8. doi: 10.1210/endo-124-1-60 [DOI] [PubMed] [Google Scholar]
- 10.Swanson LW, Sawchenko PE, Rivier J, Vale WW. Organization of ovine corticotropin-releasing factor immunoreactive cells and fibers in the rat brain: an immunohistochemical study. Neuroendocrinology. 1983;36(3):165–86. [DOI] [PubMed] [Google Scholar]
- 11.Korosi A, Baram TZ. The central corticotropin releasing factor system during development and adulthood. Eur J Pharmacol. 2008. April 7;583(2–3):204–14. doi: 10.1016/j.ejphar.2007.11.066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Van Pett K, Viau V, Bittencourt JC, Chan RKW, Li HY, Arias C, et al. Distribution of mRNAs encoding CRF receptors in brain and pituitary of bat and mouse. J Comp Neurol. 2000. December 11;428(August):191–212. [DOI] [PubMed] [Google Scholar]
- 13.Chen Y, Brunson KL, Müller MB, Cariaga W, Baram TZ. Immunocytochemical distribution of corticotropin-releasing hormone receptor type-1 (CRF(1))-like immunoreactivity in the mouse brain: light microscopy analysis using an antibody directed against the C-terminus. J Comp Neurol. 2000. May 8;420(3):305–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Roozendaal B, Brunson KL, Holloway BL, McGaugh JL, Baram TZ. Involvement of stress-released corticotropin-releasing hormone in the basolateral amygdala in regulating memory consolidation. Proc Natl Acad Sci U S A. 2002. October 15;99(21):13908–13. doi: 10.1073/pnas.212504599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen Y, Andres AL, Frotscher M, Baram TZ. Tuning synaptic transmission in the hippocampus by stress: the CRH system. Front Cell Neurosci. 2012. January;6(April):13 doi: 10.3389/fncel.2012.00013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Behan DP, Heinrichs SC, Troncoso JC, Liu XJ, Kawas CH, Ling N, et al. Displacement of corticotropin releasing factor from its binding protein as a possible treatment for Alzheimer’s disease. Nature. 1995. November 16;378(6554):284–7. doi: 10.1038/378284a0 [DOI] [PubMed] [Google Scholar]
- 17.Gunn BG, Cox CD, Chen Y, Frotscher M, Gall CM, Baram TZ, et al. The endogenous stress hormone CRH modulates excitatory transmission and network physiology in hippocampus. Cereb Cortex. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen Y, Dubé CM, Rice CJ, Baram TZ. Rapid loss of dendritic spines after stress involves derangement of spine dynamics by corticotropin-releasing hormone. J Neurosci. 2008;28:2903–11. doi: 10.1523/JNEUROSCI.0225-08.2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Maras PM, Baram TZ. Sculpting the hippocampus from within: stress, spines, and CRH. Trends Neurosci. 2012. May;35(5):315–24. doi: 10.1016/j.tins.2012.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang C, Kuo C-C, Moghadam SH, Monte L, Campbell SN, Rice KC, et al. Corticotropin-releasing factor receptor-1 antagonism mitigates beta amyloid pathology and cognitive and synaptic deficits in a mouse model of Alzheimer’s disease. Alzheimers Dement. 2016. May;12(5):527–37. doi: 10.1016/j.jalz.2015.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rissman RA, Staup MA, Lee AR, Justice NJ, Rice KC, Vale W, et al. Corticotropin-releasing factor receptor-dependent effects of repeated stress on tau phosphorylation, solubility, and aggregation. Proc Natl Acad Sci U S A. 2012. April 17;109(16):6277–82. doi: 10.1073/pnas.1203140109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baram TZ, Hatalski CG. Neuropeptide-mediated excitability: a key triggering mechanism for seizure generation in the developing brain. Trends Neurosci. 1998. November;21(11):471–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Baram TZ, Ribak CE. Peptide-induced infant status epilepticus causes neuronal death and synaptic reorganization. Neuroreport. 1995. January 26;6(2):277–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brunson KL, Eghbal-Ahmadi M, Bender R, Chen Y, Baram TZ. Long-term, progressive hippocampal cell loss and dysfunction induced by early-life administration of corticotropin-releasing hormone reproduce the effects of early-life stress. Proc Natl Acad Sci U S A. 2001. July 17;98(15):8856–61. doi: 10.1073/pnas.151224898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Karteris E, Grammatopoulos DK, Randeva HS, Hillhouse EW. The role of corticotropin-releasing hormone receptors in placenta and fetal membranes during human pregnancy. Mol Genet Metab. 2001. April;72(4):287–96. doi: 10.1006/mgme.2001.3159 [DOI] [PubMed] [Google Scholar]
- 26.Class QA, Buss C, Davis EP, Gierczak M, Pattillo C, Chicz-DeMet A, et al. Low levels of corticotropin-releasing hormone during early pregnancy are associated with precocious maturation of the human fetus. Dev Neurosci. 2008;30(6):419–26. doi: 10.1159/000191213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Smith R, Nicholson RC. Corticotrophin releasing hormone and the timing of birth. Front Biosci. 2007. January 1;12:912–8. [DOI] [PubMed] [Google Scholar]
- 28.McLean M, Bisits A, Davies J, Woods R, Lowry P, Smith R. A placental clock controlling the length of human pregnancy. Nat Med. 1995. May;1(5):460–3. [DOI] [PubMed] [Google Scholar]
- 29.Howland MA, Sandman CA, Glynn LM, Crippen C, Davis EP. Fetal exposure to placental corticotropin-releasing hormone is associated with child self-reported internalizing symptoms. Psychoneuroendocrinology. 2016;67:10–7. doi: 10.1016/j.psyneuen.2016.01.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Davis EP, Glynn LM, Schetter CD, Hobel C, Chicz-Demet A, Sandman CA, et al. Corticotropin-releasing hormone during pregnancy is associated with infant temperament. Dev Neurosci. 2005. January;27(5):299–305. doi: 10.1159/000086709 [DOI] [PubMed] [Google Scholar]
- 31.Braitenberg V, Schüz A. Cortex: Statistics and Geometry of Neuronal Connectivity. Berlin, Heidelberg: Springer Verlag; 1998. [Google Scholar]
- 32.Koutmani Y, Politis PK, Elkouris M, Agrogiannis G, Kemerli M, Patsouris E, et al. Corticotropin-releasing hormone exerts direct effects on neuronal progenitor cells: implications for neuroprotection. Mol Psychiatry. 2013. March;18(3):300–7. doi: 10.1038/mp.2012.198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kastin AJ, Akerstrom V. Differential interactions of urocortin/corticotropin-releasing hormone peptides with the blood-brain barrier. Neuroendocrinology. 2002. June;75(6):367–74. [DOI] [PubMed] [Google Scholar]
- 34.Sandman CA, Wadhwa P, Glynn L, Chicz-Demet A, Porto M, Garite TJ. Corticotrophin-releasing hormone and fetal responses in human pregnancy. Ann N Y Acad Sci. 1999. January;897:66–75. [DOI] [PubMed] [Google Scholar]
- 35.Curran M, Baram TZ. Protocol for Primary Neuronal Culture & CRH Treatment. protocols.io. https://protocols.io/view/primary-neuronal-culture-crh-treatment-h2kb8cwdx.doi.org/10.17504/protocols.io.h2kb8cw
- 36.Noam Y, Zha Q, Phan L, Wu RL, Chetkovich DM, Wadman WJ, et al. Trafficking and surface expression of hyperpolarization-activated cyclic nucleotide-gated channels in hippocampal neurons. J Biol Chem. 2010. May 7;285(19):14724–36. doi: 10.1074/jbc.M109.070391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Andres AL, Regev L, Phi L, Seese RR, Chen Y, Gall CM, et al. NMDA receptor activation and calpain contribute to disruption of dendritic spines by the stress neuropeptide CRH. J Neurosci. 2013. October 23;33(43):16945–60. doi: 10.1523/JNEUROSCI.1445-13.2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Preibisch S, Saalfeld S, Tomancak P. Globally optimal stitching of tiled 3D microscopic image acquisitions. Bioinforma. 2009. June 1;25(11):1463–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Longair MH, Baker DA, Armstrong JD. Simple Neurite Tracer: open source software for reconstruction, visualization and analysis of neuronal processes. Bioinformatics. 2011. September 1;27(17):2453–4. doi: 10.1093/bioinformatics/btr390 [DOI] [PubMed] [Google Scholar]
- 40.Motulsky HJ, Brown RE, Barnett V, Lewis T, Hampel F, Ronchetti E, et al. Detecting outliers when fitting data with nonlinear regression–a new method based on robust nonlinear regression and the false discovery rate. BMC Bioinformatics. 2006;7(1):123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Avishai-Eliner S, Brunson KL, Sandman C a, Baram TZ. Stressed-out, or in (utero)? Trends Neurosci. 2002. October;25(10):518–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Khan S, Milot M, Lecompte-Collin J, Plamondon H. Time-dependent changes in CRH concentrations and release in discrete brain regions following global ischemia: effects of MK-801 pretreatment. Brain Res. 2004. July;1016(1):48–57. doi: 10.1016/j.brainres.2004.04.062 [DOI] [PubMed] [Google Scholar]
- 43.Yan XX, Toth Z, Schultz L, Ribak CE, Baram TZ. Corticotropin-releasing hormone (CRH)-containing neurons in the immature rat hippocampal formation: light and electron microscopic features and colocalization with glutamate decarboxylase and parvalbumin. Hippocampus. 1998;8(3):231–43. doi: 10.1002/(SICI)1098-1063(1998)8:3<231::AID-HIPO6>3.0.CO;2-M [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Goland RS, Wardlaw SL, Stark RI, Brown LS, Frantz AG. High levels of corticotropin-releasing hormone immunoactivity in maternal and fetal plasma during pregnancy. J Clin Endocrinol Metab. 1986. November 1;63(5):1199–203. doi: 10.1210/jcem-63-5-1199 [DOI] [PubMed] [Google Scholar]
- 45.Robinson BG, Arbiser JL, Emanuel RL, Majzoub J a. Species-specific placental corticotropin releasing hormone messenger RNA and peptide expression. Mol Cell Endocrinol. 1989;62:337–41. [DOI] [PubMed] [Google Scholar]
- 46.Frim DM, Robinson BG, Smas CM, Division E, Hospital W. Hormone Messenger RNA in Human Placenta. 1988;82(July):287–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Smith R. Parturition. N Engl J Med. 2007. January 18;356(3):271–83. doi: 10.1056/NEJMra061360 [DOI] [PubMed] [Google Scholar]
- 48.Gitau R, Fisk NM, Glover V. Human fetal and maternal corticotrophin releasing hormone responses to acute stress. Arch Dis Child Fetal Neonatal Ed. 2004. January;89(1):F29–32. doi: 10.1136/fn.89.1.F29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kostich W a., Grzanna R, Lu NZ, Largent BL. Immunohistochemical visualization of corticotropin-releasing factor type 1 (CRF1) receptors in monkey brain. J Comp Neurol. 2004;478(December):111–25. doi: 10.1002/cne.20271 [DOI] [PubMed] [Google Scholar]
- 50.Chen Y, Bender RA, Brunson KL, Pomper JK, Grigoriadis DE, Wurst W, et al. Modulation of dendritic differentiation by corticotropin-releasing factor in the developing hippocampus. Proc Natl Acad Sci U S A. 2004. November 2;101(44):15782–7. doi: 10.1073/pnas.0403975101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sandman C a., Glynn L, Schetter CD, Wadhwa P, Garite T, Chicz-DeMet A, et al. Elevated maternal cortisol early in pregnancy predicts third trimester levels of placental corticotropin releasing hormone (CRH): Priming the placental clock. Peptides. 2006. June;27(6):1457–63. doi: 10.1016/j.peptides.2005.10.002 [DOI] [PubMed] [Google Scholar]
- 52.Gayle DA. Maternal LPS induces cytokines in the amniotic fluid and corticotropin releasing hormone in the fetal rat brain. AJP Regul Integr Comp Physiol. 2004. January 29;286(6):R1024–9. [DOI] [PubMed] [Google Scholar]
- 53.Baram TZ, Hirsch E, Snead OC, Schultz L. Corticotropin-releasing hormone-induced seizures in infant rats originate in the amygdala. Ann Neurol. 1992. May;31(5):488–94. doi: 10.1002/ana.410310505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Robinson BG, Emanuel RL, Frim DM, Majzoub J a. Glucocorticoid stimulates expression of corticotropin-releasing hormone gene in human placenta. Proc Natl Acad Sci U S A. 1988;85(July):5244–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dörr HG, Heller A, Versmold HT, Sippell WG, Herrmann M, Bidlingmaier F, et al. Longitudinal study of progestins, mineralocorticoids, and glucocorticoids throughout human pregnancy. J Clin Endocrinol Metab. 1989. May;68(5):863–8. doi: 10.1210/jcem-68-5-863 [DOI] [PubMed] [Google Scholar]
- 56.Chen Y, Molet J, Lauterborn JC, Trieu BH, Bolton JL, Patterson KP, et al. Converging, Synergistic Actions of Multiple Stress Hormones Mediate Enduring Memory Impairments after Acute Simultaneous Stresses. J Neurosci. 2016;36(44). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Paus T. Brain Development In: Lerner RM, Steinberg L, editors. Handbook of Adolescent Psychology. Hoboken, NJ, USA: John Wiley & Sons, Inc.; 2009. p. 95–115. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(XLSX)
Data Availability Statement
All relevant data are within the paper and Supporting Information files.